Abstract
Background
Hemovigilance is an organized system of surveillance throughout the transfusion chain intended to evaluate information in order to prevent the appearance or recurrence of adverse reactions related to the use of blood products.
Objective
The aims of this study were to assess the late reporting of incidents related to possible seroconversion in respect to age, marital status and ethnical background, annual variations in late reporting, the number of reports opened and closed, seroconversion of donors and transfusions of blood products within the window period.
Methods
This retrospective, descriptive study used data on blood donations in the blood bank in Uberaba during the period from 2004 to 2011. Some socio-epidemiological characteristics of the donors and serology test results of donors and recipients were analyzed in respect to the late reporting of incidents related to possible seroconversion. The Chi-square test, odds ratio and a regression model were used for statistical analysis.
Results
From 2004 to 2011, the blood bank in Uberaba collected 117,857 blood bags, 284 (0.24%) of which were investigated for late reported incidents. The profile of the donors was less than 29 years old, unmarried and non-Whites. Differences in age (p-value < 0.0001), marital status (p-value = 0.0002) and ethnical background (p-value < 0.0001) were found to be statistically significant. There was no statistical difference between men and women (0.24% and 0.23% respectively; p-value = 0.951). The number of late reported incidents increased until 2008 followed by a downward trend until 2011. There were twelve cases of seroconversion in subsequent donations (seven human immunodeficiency virus, four hepatitis B and one hepatitis C) with proven human immunodeficiency virus infection after screening of only one recipient.
Conclusion
The twelve cases of seroconversion in donors with subsequent infection proven in one recipient underscores the importance of this tool to increase transfusion safety.
Keywords: Blood safety; Serology; Blood donors; Blood transfusion/adverse effects; Communicable diseases/transmission; Quality assurance, health care; Retrospective studies
Introduction
Hemovigilance is an organized system of surveillance throughout the transfusion chain intended to evaluate information in order to prevent the appearance or recurrence of adverse reactions related to the use of blood products.
The hemovigilance system evaluates the processes involved in the transfusion chain and was proposed in order to monitor and create corrective actions for any non-conformity(1).
Delayed transfusion incidents are those that occur more than 24 hours after transfusion. Examples include delayed hemolytic reactions and infections such as hepatitis C (HCV), hepatitis B (HBV), Human immunodeficiency virus (HIV), Human T-lymphotropic virus (HTLV), Chagas disease, syphilis and malaria(2).
The investigation model adopted in Brazil, according to Resolution RDC 153 - Hemovigilance Program Manual for delayed infectious incidents is named "Look Back"; it starts tracing contaminated blood products from the seropositive donor and follows them to the transfusion thereby identifying the recipients of the blood products(3,4). This manual was updated in June 2011 with the aim of correcting shortcomings found in previous versions.
The main objectives of the hemovigilance system are to make blood transfusions safer, more effective and more efficient, to demonstrate the safety of the existing transfusion system to the population, to present the risks and benefits of this therapy and to demonstrate that the problems are well known and effectively addressed in an attempt to increase blood safety(5).
The first cases of the transmission of Treponema pallidum and Trypanosoma cruzi via transfusion were reported in the 1940s. The Australia antigen was discovered in 1968 and it started to be used in the serological screening of blood donors in 1971. International blood banks started to screen for HIV in 1985 and for HTLV and HCV in1989 and 1990, respectively. In Brazil screening began a little later (HIV in1986and both HTLV and HCV in 1993)(6). A recent study reported that the transmission of HIV and HCV through blood transfusions in Canada today is approximately one in one million blood transfusions. This shows that, despite the low risk of transmission via blood transfusions, infections still occur(7).
The ethical aspects of hemovigilance are beneficial to patient safety and to provide information on health as a preventive measure in possible cases of contact. The ethical aspects take into account benefits related to avoiding malpractice, recklessness and negligence, blood donor awareness and providing information to both doctors and patients(8).
The first work on hemovigilance was carried out in France in 1991. Subsequently, other European countries adopted this procedure in an attempt to improve transfusion safety starting from collection and continuing to the transfusion itself(9).
Hemovigilance is a relatively new procedure in the world, initially implemented in France in 1993 and then in the United Kingdom(10,11). In Brazil, hemovigilance started in 2004 following the norms of resolution DRC 153-3. The idea of the current work came about due to the lack of studies in Brazil about hemovigilance. Thus, this study aims to analyze the epidemiological profile of donors involved in the delayed reporting of contaminated donations according to age, gender, marital status and ethnic background, annual variations in late reporting, the number of reports opened and closed, seroconversion of donors and transfusions of blood products within the window period.
Methods
This retrospective, descriptive study used data from the database of Fundação Hemominas on blood donors of the Hemocentro Regional de Uberaba (HRU) during the period from 2004 to 2011. Two groups of individuals were investigated: donors (with positive serology identified by screening) and the recipients of these blood products. Absolute numbers and percentages were calculated for some socio-epidemiological characteristics of the first group: gender, age (< 29 vs. > 29 years old), ethnical background (White vs. Non-White) and marital status (married vs. unmarried vs. others). Moreover, the positivity of serology testing for HIV, HBC, HCV, Syphilis and HTLV was investigated for both groups.
The data were submitted to an analysis of absolute frequencies and percentages and organized into graphs and tables. The Chi-square test was applied and the Odds Ratio calculated to investigate any associations between the characteristics of interest. The trend of the late reporting of incidents was verified using a stepwise regression model during the period from 2004 to 2011. The level of significance for all tests was set at 5%. The data were evaluated using the GraphPad InStat 3.0 statistical program.
Results
The blood center collected 117,857 blood bags in the period from 2004 to 2011; 284 (0.24%) were discarded due to the late reporting process. The pattern of late reporting of incidents was statistically similar between men and women (0.24% and 0.23%, respectively; p-value = 0.951); there was a higher percentage of under 29-year olds than over 29-year olds (0.32% and 0.17%, respectively: p-value < 0.0001); the chance of being seropositive in the under 29-year age group was 1.85 times higher than in the over 29-year age group [95% confidence interval (95% CI): 1.47-2.35]; the occurrence was significantly higher (p-value = 0.0002) among single (0.35%) compared to married individuals (0.21%) with this occurrence being 1.63 times higher (95% CI: 1.27-2.10). There was also a significant difference (p-value < 0.0001) comparing the non-White Group (0.32%) with the White Group (0.19%) with the chance of being seropositive in the non-White Group being 1.65 times higher than in the White Group (95% CI: 1.31-2.09) (Table 1).
Table 1.
Distribution of donations at the Hemocentro Regional de Uberaba initially considered safe but with subsequent reporting of incidents in the period from 2004 to 20011: stratified by gender, age, marital status and ethnical background
| Epidemiological characteristics | Total donations | Safe donations | Hemovigilance | ||||||
| n | n | n | % | OR | 95% CI | χ2 | p-value | ||
| Total donations | 117,857 | 117,573 | 284 | ||||||
| Gender | |||||||||
| Female | 33,808 | 33,728 | 99.76 | 81 | 0.24 | - | - | - | - |
| Male | 84,048 | 83,845 | 99.76 | 203 | 0.24 | 1.01 | (0.78-1.30) | 0.004 | 0.951 |
| Age | |||||||||
| 18 to 29 years | 50,034 | 49,870 | 99.67 | 164 | 0.33 | 1.85 | (1.47-2.35) | 26.63 | 0.0000* |
| > 29 years | 67,823 | 67,703 | 99.82 | 120 | 0.18 | - | - | - | - |
| Marital status | |||||||||
| Married | 52,509 | 52,396 | 99.78 | 113 | 0.22 | - | - | - | - |
| Single | 37,664 | 37,532 | 99.65 | 132 | 0.35 | 1.63 | (1.27-2.10) | 14.32 | 0.0002* |
| Ethnical background | |||||||||
| White | 79,116 | 78,959 | 67.20 | 157 | 0.19 | - | - | - | - |
| Non-white | 38,741 | 38,614 | 32.80 | 127 | 0.32 | 1.65 | (1.31-2.09) | 17.57 | 0.0000* |
OR: Odds Ratio; 95% CI: 95% confidence interval; x2: Chi-square Test; *: Significant difference; Note: there were 27,684 cases that were not classified as single or married
Note: there were 27,684 cases that were not classified as single or married
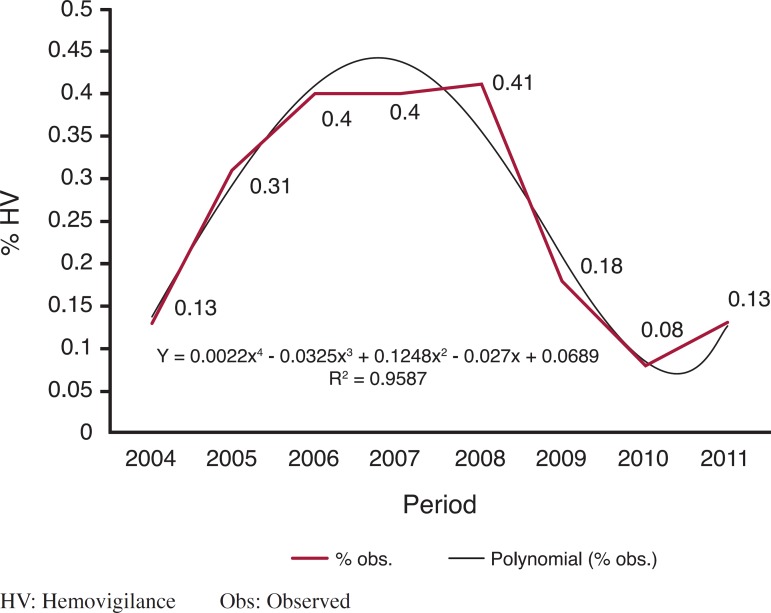
As to the annual variation in the late reporting of incidents over the eight years studied, the mean prevalence observed was 0.24%, with the highest percentage in 2008 (0.41%) and the lowest in 2010 (0.08%). By regression analysis it was observed that the degree 4 polynomial model (y = 0.0022x4 - 0.0325x3 + 0.1248x2 - 0.027x + 0.0689) explains 95.87% (r² = 0.9587) of the pattern of late reporting of incidents (Figure 1).
Figure 1.
Percentage of late reporting of incidents at the Hemocentro Regional de Uberaba from 2004 to 2011
There were 284 late reported incidents during the study period. Of these 131 (46.12%) were due to suspected positive serology for HIV, 88 (30.98%) for hepatitis B, 52 (18.30%) for hepatitis C, eight (2.81%) for HTLV and one (0.35%) for Syphilis. However 251 cases were closed because the confirmatory test was seronegative and 21 because the donors did not return for tests after three requests. Seropositivity was confirmed for 12 donations during the four years of the study; seven with positive serology for HIV, four for hepatitis B and one for hepatitis C. Four recipients were located and submitted to serological tests but without proven seroconversion after a mean time of two years. Two donations were discarded due to lipemic serum, two recipients were requested to attend a consultation but did not show up, two recipients died and two recipients of late reported incidents still did not return to perform confirmatory tests. Additionally, in one case of proven contamination by HIV, a second recipient died before being traced (Table 2).
Table 2.
Number of donations with seropositivity for HIV, HBV and HCV and possible contamination of recipients in the Hemocentro Regional de Uberaba - Hemominas from 2004 to 2011
| Donation | ||||||
| Date | no. | Seropositivity | Possible seroconversion | Recipient | Outcome | |
| 11/01/2005 | 624978 | HIV | 16/09/2004 | ESC | seronegative | |
| 29/03/2005 | 1935 | HIV | 22/11/2004 | OOB/ALA | seronegative | |
| 14/02/2007 | 636809 | HBV | 28/06/2006 | IRC | seronegative | |
| 19/06/2007 | 641251 | HIV | 02/01/2007 | DMS | did not return | |
| 06/12/2007 | 626136 | HIV | 14/08/2007 | VGS | seronegative | |
| 15/12/2008 | 648347 | HBV | 13/08/2008 | discarded | ||
| 24/06/2009 | 648991 | HBV | 08/02/2009 | HHA | did not return | |
| 16/06/2011 | 635321 | HCV | 07/02/2011 | discarded | ||
| 20/07/2011 | 47571 | HIV | 24/02/2011 | GBD/MAS | seropositive/ death | |
| 30/11/2011 | 651794 | HIV | 17/04/2011 | RLG/SCA | tracking | |
| 15/11/2011 | 633419 | HIV | 08/06/2011 | MGFO | death | |
| 23/11/2011 | 614141 | HBV | 19/07/2011 | industry/MPC/DSM/UPA | tracking | |
| Total | 12 | 16 | ||||
Discussion
The profile of blood donors who were involved in the late reported incidents at the HRU in the period from 2004 to 2011 was younger than 29 years old, single and non-White. A statistically similar pattern was found between genders. These results suggest that these individuals (under 29 years old, single and non-Whites) should be the target of educational programs to increase their awareness about the act of donation; this might help reduce the chance of infections via transfusions, the number of discarded bags and improve the effectiveness of the method. However we cannot fail to point out that despite having found a statistically significant difference for this population, awareness programs must be extended to all donors, regardless of profile. The results of this study are similar to those found in São José do Rio Preto and in Pelotas, both in 2008 where the vast majority of donors with seropositive results were young and single but also men(12,13). A study in Rio de Janeiro in 2008 found the highest rate of seropositive results for HIV in male donors and in over 30-year olds(14>). The findings of this study are similar to those found in a previous study by the same group on the occurrence of blood donations seropositive for HIV in HRU in the period 1995 to 2006 with 177,246 donations and 119 with positive serology for HIV; the proportions were significantly higher for single and for younger donors(15).
Since 2003, the Brazilian legislation has made it compulsory to notify seroconversions of blood donors in blood centers around the country. However, studies are scarce and notifications about incidents are uncommon in Brazil.
The rate of late notifications observed in this study was similar to published findings. Thus, while values ranging from 0.09 to 1% were found in different studies(16,17), 0.24% of collected bags were discarded in the HRU as a result of hemovigilance. This low incidence can be attributed to the scarcity of studies in relation to the incidence of late notifications, the better socio-intellectual conditions of these donors compared to countries or regions that do not use this procedure, as well as better staff training in blood centers where hemovigilance is effective.
The current study demonstrates a decreasing trend in the percentage of late notifications from 2008 to 2011. Therefore, it seems reasonable to say that there is an improvement in the training of staff involved in the notification process of delayed adverse effects due to blood transfusions, and greater awareness and loyalty of donors. These data may also reflect an inadequate understanding of the recently implanted process by the professional team and the possible occurrence of failures in implementation at the start.
This study shows that twelve of the 284 donors involved in late notifications became seropositive for HIV, hepatitis B or hepatitis C; one case of transfusion-related HIV transmission was confirmed and it has been impossible to locate two cases of recipients from earlier donations until now. The contaminated patient had received packed red blood cells in a procedure four months prior to donor seroconversion being identified. This patient was 56 years old and was suffering from non-Hodgkin mantle-cell lymphoma. He was followed up in the service and died in May 2012 due to complications of the neoplastic disease and so did not evolve with acquired immune deficiency syndrome (AIDS). The recipient of concentrated platelets from the same donation died before being traced. These results show that, despite the advances of serologic tests and consequently the reduction in the immunological window, risks still exist. It is important to point out that blood transfusion is a therapy, and thus risks exist and so this procedure needs to be indicated carefully and only when needed. This work emphasizes the usefulness of hemovigilance in the control of transfusion-related late adverse events in an attempt to provide a safe service to the recipient with actions that allow preventive measures, early diagnosis and the establishment of effective treatment. Additionally it questions the need for increasingly sensitive screening tests with a high negative predictive value to decrease risk of the immunological window without sacrificing specificity. The Ministry of health determined that nucleic acid testing (NAT) for HIV and HCV must be implanted in blood banks throughout the country by January 2004(18); this was introduced to HRU in September 2011. While serological screening tests identify antibodies, they take time. Molecular biology methods, on the other hand, identify components of the virus, the nucleic acid, thus increase the sensitivity and specificity of testing. Studies have shown that with the new technique, the 'immunological window' is reduced from 22 to 10 days for HIV infections and from 90 to 15 days for HCV infections. Studies carried out in the HRU in 2008 and in a blood bank in São Paulo in 2004 also support the implementation of this method(19,20). A work published in 2011 also defends the use of increasingly sensitivity and specific serological screening methods in an attempt to increase transfusion safety(21).
Two review articles on this topic in 2008 and 2011 also support the implementation of hemovigilance in Brazil as it enables the evaluation of prospective and retrospective data, which is of fundamental importance to adapt preventive measures to the Brazilian reality(22,23).
Conclusion
This study has shown that under 29-year-old, single and non-White individuals predominated in the number of late notification cases of contaminated blood donations. It also identified a prevalence of 0.24% of donors as cases of late notifications with a growth in the number of cases between 2004 and 2008 followed by a downward trend until 2011. Moreover, the twelve confirmed cases of seroconversion and one contaminated recipient identified proves that late notification reporting has an impact on transfusion safety and helps to prevent the occurrence and recurrence of transfusion-related adverse effects. This demonstrates that, despite advances in serologic methods, risk linked to the immunological window is real, hence, more sensitive methods such as NAT with a lower negative predictive value but without the loss of specificity are necessary to reduce the risk of infectious disease transmission via blood transfusions. These data demonstrate the need to educate the community that donation is an act of citizenship which aims to save lives and not to transmit disease.
Acknowledgments
The authors wish to thank Heloíza das Graças de Sous and Marise Carvalho Silveira for help in the data collection, and Fapemig (Fundação de Amparo à Pesquisa do Estado de Minas Gerais) and the Fundação Hemominas for scientific initiation grants.
Footnotes
Conflict-of-interest disclosure: The authors declare no competing financial interest
References
- 1.Faber JC. Haemovigilance around the world. Vox Sang. 2002;83(Suppl 1):71–76. doi: 10.1111/j.1423-0410.2002.tb05271.x. [DOI] [PubMed] [Google Scholar]
- 2.United Kingdom. Departament of Health. Health Service Circular . Better Blood Transfusion: appropriate use of blood [Internet] England: UK Department of Health; 2005. [cited 2012 Jun 1]. [HSC 2002/009, 04 july 2002 ] Available from: http://www.transfusionguidelines.org/docs/pdfs/nbtc_bbt_hsc_02.pdf. [Google Scholar]
- 3.Brasil. Ministério da Saúde . Resolução RDC nº153, de 14 de junho de 2004. Determina o regulamento técnico para os procedimentos hemoterápicos, incluindo a coleta, o processamento, a testagem, o armazenamento, o transporte, o controle de qualidade e o uso humano de sangue, e seus componentes, obtidos do sangue venoso, do cordão umbilical, da placenta e da medula óssea [Internet] Brasília: MS; 2002. [cited 2010 Feb 2]. Available from: http://portal.saude.gov.br/portal/arquivos/pdf/resolucao_153_2004.pdf. [Google Scholar]
- 4.Fundação Centro de Hematologia e Hemoterapia de Minas Gerais-HEMOMNAS. Portaria PRE No. 128/2011 de 13 de junho de 2011. Aprova o Manual de Normas e Procedimentos de Hemovigilância de Incidentes transfusionais tardios infecciosos no âmbito da Fundação HEMOMINAS. Belo Horizonte: HEMOMINAS; 2011. [cited 2011 June 13]. Available from: http://www.jusbrasil.com.br/diarios/27674889/doemg-executivo-legislativo-14-06-2011-pg-42. [Google Scholar]
- 5.Callum JL, Merkley LL, Coovadia AS, Lima AP, Kaplan HS. Experience with the medical event reporting system for transfusion medicine (MERS-TM) at three hospitals. Transfus Apher Sci. 2004;31(2):133–143. doi: 10.1016/j.transci.2004.07.007. Comment in: Transfus Apher Sci. 2004;31(2):95-8. [DOI] [PubMed] [Google Scholar]
- 6.Kleinman SH, Busch MP. The risks of transfusion-transmitted infection: direct estimation and mathematical modeling. Baillieres Best Pract Res Clin Haematol. 2000;13(4):631–649. doi: 10.1053/beha.2000.0104. [DOI] [PubMed] [Google Scholar]
- 7.Callum JL, Lin Y, Lima A, Merkley L. Transitioning from 'blood' safety to 'transfusion' safety: addressing the single biggest risk of transfusion. ISBT Science Series. 2011;6(1):96–104. [Google Scholar]
- 8.Williamson LM, Lowe S, Love EM, Cohen H, Soldan K, McClelland DB, et al. Serious hazards of transfusion (SHOT) initiative: analysis of the first two annual reports. BMJ. 1999;319(7201):16–19. doi: 10.1136/bmj.319.7201.16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Salmi LR. Transfus Clin Biol. 6. Vol. 1. French: 1994. Epidemiological support in blood surveillance; pp. 421–424. [DOI] [PubMed] [Google Scholar]
- 10.Strengers PF, Heier HE. 4th European and 5th Regional Congress of International Society of Blood Transfusions. Venezia, Italy: Haemovigilance procedures in transfusion medicine; p. 953. 2 to 5 july 1995. [Google Scholar]
- 11.Hervé P, des Floris MF, Rebibo D, Morei P, Andreu G. Hemovigilance in France. Rev Bras Hematol Hemoter. 2000;22(3):368–373. [Google Scholar]
- 12.Vendramini-Foss M, Santos-Andreto AC, Mergulhão MB, Fachini RM, Ricci Jr O. Perfil de doadores inaptos soropositivos para HIV. Rev Bras Hematol Hemoter. 2008;30(Supl 4):374–374. [Abstract 979] [Google Scholar]
- 13.Nachtigal GC, Araújo AB, Loges LÂ, Michel JO, Duarte CR, Bareno FB. Avaliação do retorno de doadores não liberados na triagemsorológica do Hemopel [Abstract 969] Rev Bras Hematol Hemoter. 2008;30(Supl 4):370–370. [Google Scholar]
- 14.Dias KK, Ferreira PH, Brito S, Ferreira E, Silva S, Feitoza M, Martins M, et al. Perfil do doador de sangue HIV positivo do serviço de Hemoterapia do Inca-RJ. Rev Bras Hematol Hemoter. 2008;30(Supl 4):374–374. [Abstract 980] [Google Scholar]
- 15.Eustáquio JM, Lima GM, Martins RA, Souza HM, Martins PR. Ocorrência de doações de sangue com sorologia positiva para o vírus HIV no Hemocentro Regional de Uberaba (MG) - Fundação Hemominas no período de 1995 a 2006. Rev Patol Trop. 2009;38(2):73–81. [Google Scholar]
- 16.Pillonel J, Le Marrec N, Girault A, David D, Laperche S. Transfus Clin Biol. 3. Vol. 12. French: 2005. [Epidemiological surveillance of blood donors and residual risk of blood-borne infections in France, 2001 to 2003] pp. 239–246. [DOI] [PubMed] [Google Scholar]
- 17.Ludwig L, Zilly A. Reações transfusionais ligadas ao sistema ABO. NewsLab. 2007;84(1):102–112. [Google Scholar]
- 18.Brasil. Ministério da Saúde . Portaria no. 112/GM, em 29 de Janeiro de 2004. Dispõe sobre a implantação, no âmbito da Hemorrede Nacional, da realização dos testes de amplificação e detecção de ácidos nucléicos (NAT) para HIV e HCV [Internet] Brasília: MS; 2004. [[cited 10 August 2012]]. Available from: http://dtr2001.saude.gov.br/sas/PORTARIAS/Port2004/GM/GM-112.htm. [Google Scholar]
- 19.Garcia FB, Gomide GP, Pereira GA, Souza HM. Importância dos testes sorológicos de triagem e confirmatórios na detecção de doadores de sangue infectados pelo vírus da hepatite C. Rev Bras Hematol Hemoter. 2008;30(3):218–222. [Google Scholar]
- 20.Scuracchio PS, Poli MC, Lemos MM, Oliveira AG, Filho, Salles NA, Chamone DA, et al. Detection of HIV-1 infection in blood donors during the immunological window period using the nucleic acid-amplification technology. Transfus Med. 2007;17(3):200–4. doi: 10.1111/j.1365-3148.2007.00748.x. [DOI] [PubMed] [Google Scholar]
- 21.AuBuchon JP. Update on the status of pathogen inactivation methods. ISBT Science Series. 2011;(6):181–188. [Google Scholar]
- 22.Lopes MS, Proietti AB. HTLV-1/2 transfusional e hemovigilância: a contribuição dos estudos de look-back . Rev Bras Hematol Hemoter. 2008;30(3):229–240. [Google Scholar]
- 23.Nascimento F. Haemovigilance: a tool for quality improvement. ISBT Science Series. 2011;6(1):84–88. [Google Scholar]