Abstract
We report here on a rare case of BCR-ABL1-negative atypical chronic myeloid leukemia with a t(9;22)(p24;q11.2)translocation and a BCR-JAK2 fusion gene, with resistance to the tyrosine kinase inhibitors imatinib and dasatinib.At two years of follow-up, the patient showed no hematologic response and was submitted to an allogeneic bonemarrow transplantation. Fifty-three days after the procedure, he died due to acute graft-versus-host disease. This BCR-JAK2 fusion gene has so far been found in only five patients in the whole world, with three clinical presentations: myeloproliferative neoplasm, acute lymphoblastic leukemia and acute myeloid leukemia.
Keywords: Leukemia, myeloid, chronic, atypical, BCR-ABL negative; Myelodysplastic-myeloproliferative diseases; Proto-oncogene proteins c-bcr
Introduction
Chronic Myeloid Leukemia (CML) is the best described disease resulting from the t(9;22)(q34,q11.2). This chromosomal rearrangement leads to the well-known BCR-ABL fusion that promotes tyrosine kinase activity. Other oncogenic BCR fusions have also been found, such as platelet-derived growth factor receptor-alpha gene (PDGFRA) (4q12)(1)and fibroblast growth factor receptor 1 (FGFR1) (8p12)(2,3), which cause myeloproliferative disorders (MD).
The janus kinase 2 (JAK2) gene is one of the four members of the JAK gene family. The JAK2 V617F mutation which results from a G->T transversion at nucleotide 1849 in exon 14 of the JAK2 gene resulting in the substitution of valine by phenylalanine at codon 617, is associated with MD and is a major diagnostic criterion for primary myelofibrosis, polycythemia vera and essential thrombocythemia(4). A great number of chromosomal translocations involving the JAK2 locus have been described.
We report here on an extremely rare case of atypical CML that was found to be breakpoint cluster region (BCR)-Abelson (ABL) 1 (BCR-ABL1) -negative, due to the BCR-JAK2 fusion resulting from a t(9;22)(p24,q11.2) translocation. To the best of our knowledge, this is the first case reported in Brazil and the sixth in the world.
Case Report
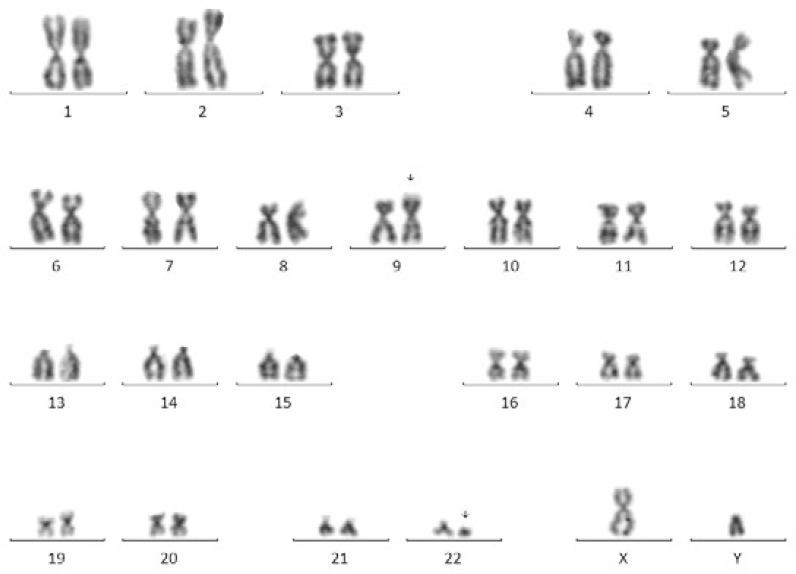
In April 2010, a 54-year-old male patient presented with fatigue, abdominal pain and splenomegaly. A blood count revealed leukocytosis (93.38 x 109/L) with a predominance of neutrophils and a shift to the left. Hypercellular bone marrow with granulocytic and erythroid dysplasia was described. Conventional cytogenetic analysis was performed and a 46,XY,t(9;22) (p24;q11.2) karyotype was found in 90% of the metaphases examined (Figure 1) In view of the clinical picture, the result was interpreted as indicative of the presence of a BCR-ABL1 fusion gene, but this was not detected by reverse transcription polymerase chain reaction (RT-PCR). The presence of a BCR-ABL rearrangement was also ruled out by fluorescence in situ hybridization (FISH) using a BCR-ABL probe. In addition, no BCR/PDGFR FIP fusion gene or JAK2 V617F mutation were detected by RT-PCR. Therefore, the case was classified, according to the latest World Health Organization Classification, as BCR-ABL1-negative atypical CML.
Figure 1.
Conventional cytogenetics showing 46,XY,t(9;22)(p24;q11.2)karyotype
The patient was treated with imatinib at a dose of 400 mg/day because of the involvement of the BCR gene. After three months of treatment, he presented weight loss, progressive splenomegaly and no hematologic response. His medication was changed to dasatinib (150 mg/day) plus hydroxyurea (3 g/day). In August 2011, given the absence of a hematologic response, the dasatinib treatment was discontinued.
Conventional karyotyping was performed again and the 46,XY,t(9;22)(p24;q11.2) karyotype was observed in all metaphases examined.
In October 2012, the patient had not achieved complete hematologic remission with hydroxyurea. However, in the meantime, his sister had been identified as an HLA-fully matched donor and he was presenting a 90% Karnofsky score. Thus, he was referred for an allogeneic bone marrow transplant. Fifty-three days after the transplantation he died due to acute graft-versus-host disease affecting his gastrointestinal tract and skin.
Discussion
The patient described here, presenting BCR-ABL1-negative atypical CML and a t(9;22)(p24;q11.2) translocation, was treated with the tyrosine kinase inhibitors imatinib and dasatinib but did not achieve any hematologic response. Of the five previously reported cases, three presented MD, one had acute myeloid leukemia and one acute lymphoblastic leukemia. Only one of them was treated with imatinib, and the patient could not be followed-up(8). Although the follow-up in two of the case reports was not described, it is important to observe that in the remaining cases the mortality rate was 66% (Table 1). The BCR-JAK2 fusion protein contains the coiled-coil dimerization domain of BCR and the protein tyrosine kinase domain (JH1) of JAK2. It was demonstrated by preclinical studies that BCR-JAK2 induces STAT5 activation and elicits BCRxL gene expression. These factors promote tumorigenic properties and lead to increased cell survival(10).
Tabela 1.
Characteristics of cases reported with the t(9;22)(p24;q11.2)
| Reference | Age | Gender | Translocation | Clinical presentation | Treatment | Follow-up |
| Griesing et al.(5) | 63 | F | t(9;22)(p24;q11.2) | MD | Hy; Cy; Mit | Death |
| Cirmena et al.(6) | 67 | F | t(9;22)(p24;q11) | AML | HD + allo BMT | Death |
| Lane et al (7) | 44 | M | t(9;22)(p24;q11.2) | MD | Not described | Not described |
| Elnaggar et al.(8) | 84 | M | t(9;22)(p24;q11.2) | MD | Hy; IM | Dropped out from follow up |
| Tirado et al.(9) | 14 | M | t(9;22)(p24;q11.2) | ALL | Polychemotherapy | Remission |
F: Female; M: Male; Hy: Hydroxyurea; Cy: Cytarabine; Mit: Mitoxantrone; HD: High dose chemotherapy; allo BMT: allogeneic Bone Marrow Transplantation; IM: imatinib; AML: Acute myeloid leukemia; MD: myeloproliferative disorder; ALL: Acute lymphoblastic leukemia
It was not possible to define which therapy would be best because tyrosine kinase inhibitors may not be effective against the BCR-JAK2 fusion. Some authors suggest that in these cases it is important to investigate the role of JAK2 inhibitors alone or in combination with chemotherapy(10). We decided to submit our patient to allogeneic bone marrow transplantation, taking into account the poor prognosis reported in previous cases, his good performance status and the presence of a sister who was an HLA-fully matched donor. Unfortunately, he died of acute graft-versus host disease of the gastrointestinal tract and skin, so the efficacy of this treatment strategy could not be determined.
Our case shows a rare t(9;22)(p24;q11.2) leading to a BCR/JAK2 fusion in a patient with MD. This finding explains the tumorigenic activity seen in preclinical studies.
Footnotes
Conflict-of-interest disclosure: The authors declare no competing financial interest
References
- 1.Baxter EJ, Hochhaus A, Bolufer P, Reiter A, Fernandez JM, Senent L, et al. The t(4;22)(q12;q11) in atypical chronic myeloid leukaemia fuses BCRto PDGFRA. Hum Mol Genet. 2002;11(12):1391–1397. doi: 10.1093/hmg/11.12.1391. [DOI] [PubMed] [Google Scholar]
- 2.Demiroglu A, Steer EJ, Heath C, Taylor K, Bentley M, Allen SL, et al. The t(8;22) in chronic myeloid leukemia fuses BCR to FGFR1: transforming activity and specific inhibition of FGFR1 fusion proteins. Blood. 2001;98(13):3778–3783. doi: 10.1182/blood.v98.13.3778. [DOI] [PubMed] [Google Scholar]
- 3.Fioretos T, Panagopoulos I, Lassen C, Swedin A, Billström R, Isaksson M, et al. Fusion of the BCR and the fibroblast growth factor receptor-1 (FGFR1) genes as a result of t(8;22)(p11;q11) in a myeloproliferative disorder: The first fusion gene involving BCR but not ABL. Genes Chromosomes Cancer. 2001;32(4):302–310. doi: 10.1002/gcc.1195. [DOI] [PubMed] [Google Scholar]
- 4.Thiele J, Kvasnicka HM, Orazi A, Tefferi A, Birgegard G. World Health Organization classification of tumours of haematopoietic and Lymphoid Tissues. Chronic myeloproliferative disorders treatment. 4. Lyon: International Agency for Research on Cancer Press; 2008. [Google Scholar]
- 5.Griesinger F, Hennig H, Hillmer F, Podleschny M, Steffens R, Pies A, et al. A BCR-JAK2 fusion gene as the result of a t(9;22)(p24;q11.2) translocation in a patient with a clinically typical chronic myeloid leukemia. Genes Chromosomes Cancer. 2005;44(3):329–333. doi: 10.1002/gcc.20235. [DOI] [PubMed] [Google Scholar]
- 6.Cirmena G, Aliano S, Fugazza G, Bruzzone R, Garuti A, Bocciardi R, et al. A BCR-JAK2 fusion gene as the result of a t(9;22)(p24;q11) in a patient with acute myeloid leukemia. Cancer Genet Cytogenet. 2008;183(2):105–108. doi: 10.1016/j.cancergencyto.2008.02.005. [DOI] [PubMed] [Google Scholar]
- 7.Lane SW, Fairbairn DJ, McCarthy C, Nandini A, Perry-Keene J, Kennedy GA. Leukaemia cutis in atypical chronic myeloid leukaemia with a t(9;22) (p24;q11.2) leading to BCR-JAK2 fusion. Br J Haematol. 2008;142(4):503. doi: 10.1111/j.1365-2141.2008.07164.x. [DOI] [PubMed] [Google Scholar]
- 8.Elnaggar MM, Agersborg S, Sahoo T, Girgin A, Ma W, Rakkhit R, et al. BCR- JAK2 fusion as a result of a translocation (9;22)(p24;q11.2) in a patient with CML-like myeloproliferative disease. Mol Cytogenet. 2012;5(1):23. doi: 10.1186/1755-8166-5-23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Tirado CA, Chen W, Huang LJ, Laborde C, Hiemenz MC, Valdez F, et al. Novel JAK2 rearrangement resulting from a t(9;22)(p24;q11.2) in B-acute lymphoblastic leukemia. Leuk Res. 2010;34(12):1674–1676. doi: 10.1016/j.leukres.2010.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cuesta-Domínguez Á, Ortega M, Ormazábal C, Santos-Roncero M, Galán-Díez M, Steegmann JL, et al. Transforming and tumorigenic activity of JAK2 by fusion to BCR: molecular mechanisms of action of a novel BCR-JAK2 tyrosine-kinase. PLoS One. 2012;7(2):e32451. doi: 10.1371/journal.pone.0032451. [DOI] [PMC free article] [PubMed] [Google Scholar]