Abstract
Background
Laparoscopic surgery for common bile duct stones varies procedurally from a transcystic approach to laparoscopic choledochotomy (LC) with or without biliary drainage. However, LC is a difficult procedure with higher documented morbidity than the transcystic approach. We retrospectively investigated risk factors for adverse outcomes of LC.
Methods
We used logistic regression models to assess 4 categories of adverse outcomes: overall, complications, conversion to open operation and failed surgical clearance. We calculated the area under the receiver operating characteristic curve to evaluate diagnostic accuracy.
Results
We included 201 patients who underwent LC in our analysis. Adverse outcomes occurred in 48 (23.9%) patients, complications occurred in 43 (21.4%), retained stones were observed in 8 (4%), and conversion to laparotomy occurred in 7 (3.5%). Multivariate analysis showed that total bilirubin (BIL) and the presence of medical risk factors (MRFs) were significant predictors of adverse outcomes and complications. We calculated the probability of adverse outcomes (p) using the following formula: logit(p) = 0.977 (MRFs) + 0.014 (BIL) − 2.919. p = EXP (logit(p)) ÷ [1+EXP (logit(p))]. According to their logit(p), all patients were divided into a low-risk group (logit(p) ≤ −1.32, n = 130) and a high-risk group (logit(p) > −1.32, n = 71). Patients in the low-risk group had about a 1 in 10 chance (12 of 130) of adverse outcomes developing. Of the 71 patients in the high-risk group, 36 (50.7%) experienced adverse outcomes.
Conclusion
High BIL and the presence of MRFs could predict adverse outcomes in patients undergoing LC.
Abstract
Contexte
La chirurgie laparoscopique pour extraction de calculs biliaires logés dans le cholédoque diffère sur le plan technique de la cholédochotomie laparoscopique (CL) par approche transcystique avec ou sans drain biliaire. Toutefois, la CL est une intervention délicate, qui s’accompagne d’un taux de morbidité documenté plus élevé comparativement à l’extraction transcystique. Nous avons analysé rétrospectivement les facteurs de risque à l’égard d’une issue négative de la CL.
Méthodes
Nous avons utilisé des modèles de régression logistique pour évaluer 4 catégories d'issue négative : issue négative globale, complications, conversion vers une chirurgie ouverte et échec de l’extraction chirurgicale. Nous avons calculé l'aire sous la courbe de la fonction d’efficacité du récepteur pour évaluer la précision diagnostique.
Résultats
Nous avons inclus dans notre analyse 201 patients soumis à une CL. Une issue négative est survenue chez 48 patients (23,9 %), des complications chez 43 (21,4 %), la persistance des calculs chez 8 (4 %) et la conversion vers la laparotomie chez 7 (3,5 %). L’analyse multivariée a montré que la bilirubine totale (BIL) et la présence de facteurs de risque médicaux (FRM) étaient des prédicteurs significatifs d’une issue négative et de complications. Nous avons calculé la probabilité de survenue d’une issue négative (p) à l’aide de la formule suivante : logit(p) = 0,977 (FRM) + 0,014 (BIL) − 2,919. p = EXP (logit(p)) ÷ [1 + EXP (logit(p))]. En fonction de leur valeur logit(p), tous les patients ont été répartis entre un groupe à faible risque (logit(p) = ≤ −1,32, n = 130) et un groupe à risque élevé (logit(p) > −1,32, n = 71). Les patients du groupe à faible risque présentaient 1 chance sur 10 (12 sur 130) d’issue défavorable. Parmi les 71 patients du groupe à risque élevé, 36 (50,7 %) ont présenté une issue défavorable.
Conclusion
Un taux de BIL élevé et la présence de FRM pourraient prédire l’issue négative chez des patients soumis à une CL.
With the advent of laparoscopic cholecystectomy, when the presence of common bile duct (CBD) stones are suspected during the preoperative period, endoscopists can perform an endoscopic retrograde cholangiopancreatography (ERCP) with stone extraction before the surgeon performs a laparoscopic cholecystectomy. This approach is practical, but it requires the intervention of 2 teams: surgical and endoscopic. In addition, ERCP is associated with substantial morbidity and mortality,1,2 and adds costs to the procedure. For this reason, there is growing acceptance that in experienced hands laparoscopic bile duct exploration is more efficient than, and at least as safe as, endoscopic sphincterotomy in patients with CBD stones who are fit enough for general anesthesia and cholecystectomy. A meta-analysis of 5 randomized controlled trials3 and recent clinical guidelines4 have endorsed this opinion.
Laparoscopic surgery for CBD stones can be divided into several procedural variations: a transcystic approach, and laparoscopic choledochotomy (LC) with or without biliary drainage. The transcystic approach has been reported to be applicable in up to 93% of patients (mean 71%) with a success rate of 74%–98%.5 However, LC is still a difficult procedure with higher documented morbidity than the transcystic approach.6 Surprisingly, there is relatively little information on the results of LC alone, as most series continue to pool the results of the 2 approaches.5,7,8
To the best of our knowledge, only 1 published study has specifically evaluated the predictors relating to poor outcomes after laparoscopic bile duct exploration.8 However, in that report, they also pool the results of laparoscopic transductal, transcystic and radiological exploration. In Asian reports, the success rates of transcystic exploration are much lower than those in Western reports.9,10 However, to our knowledge, there is no published analysis focusing on predictors of adverse outcomes after LC alone. Therefore, the purpose of the present retrospective study was to investigate the results and to evaluate the risk factors for adverse outcomes after LC for the management of CBD stones in a large series of consecutive patients.
Methods
The study included patients who underwent LC performed by or under the direct supervision of an experienced laparoscopic surgeon (X.M. Hong) at Yinzhou Second Hospital between April 2004 and April 2011. Data were collected immediately after the operation. All patients were routinely assessed 6 weeks after discharge or rereferred if complications occurred after this period. This study complied with the guidelines established by the Ethics Committee of our hospital and the Declaration of Helsinki.
Operative technique
All patients underwent transabdominal ultrasonography and liver function tests. Patients with severe acute suppurative cholangitis or severe acute pancreatitis requiring immediate biliary drainage were scheduled to undergo emergency ERCP. Patients with CBD stones identified by ultrasonography or computed tomography proceeded straight to ERCP or LC. Equivocal cases (cholangitis, pancreatitis, current elevated liver function tests, CBD dilatation ≥ 8 mm on ultrasound) underwent magnetic resonance cholangiopancreatography (MRCP), and the results were used to select patients for subsequent ERCP or LC. Only patients with confirmed CBD stones and a CBD diameter of 8 mm or greater were selected for LC. Patients with a CBD diameter of less than 8 mm at ultrasound or MRCP and other patients deemed unfit for general anesthesia were scheduled to undergo ERCP. However, for patients with a CBD diameter of 8 mm or greater, there was still no standard protocol for patient selection in our institute.
We performed LC basically in the same way as open exploration. After preparing the anterior wall of the CBD, we used scissors to make a longitudinal incision in the CBD long enough to accommodate the stone intact. All stones visible at LC could be extracted with atraumatic forceps. Stones located in the lower part of the CBD could be pushed through choledochotomy by pressure on the CBD wall with blunt forceps or flushed through the choledochotomy with saline irrigation. The remaining stones were extracted with baskets and balloons under choledochoscopic guidance. Presenting cases of impacted biliary tract stones at the papilla level, obstructing the access of the basket, were managed with fragmentation achieved by holmium laser lithotripsy. In this procedure, the transducer was introduced through the choledochoscope and placed under direct visualization immediately over the stone, which was then broken into small fragments and collected in the basket or flushed out.
We used choledochoscopy for a postexploratory check of the bile ducts in all patients to ensure complete clearance of the biliary system. We considered clearance of the distal CBD to be complete only when the choledochoscope was passed into the duodenum through the ampulla of Vater. This was done carefully, avoiding undue manipulation of the ampulla.
We then assessed the CBD to decide on the method of closure. Whenever there was a concern of residual debris, extensive inflammation in the CBD or manipulation of the ampulla, we preferred closure over a drainage tube through a T-tube, or an endoscopic nasobiliary drainage (ENBD) tube. If the CBD was completely cleared, there was no debris or sludge in the CBD, and the papilla of Vater had no evidence of stenosis, the choledochotomy was primarily closed without biliary drainage. Subhepatic drainage was routinely positioned through the lateral subcostal port in all patients (Figs. 1–3).
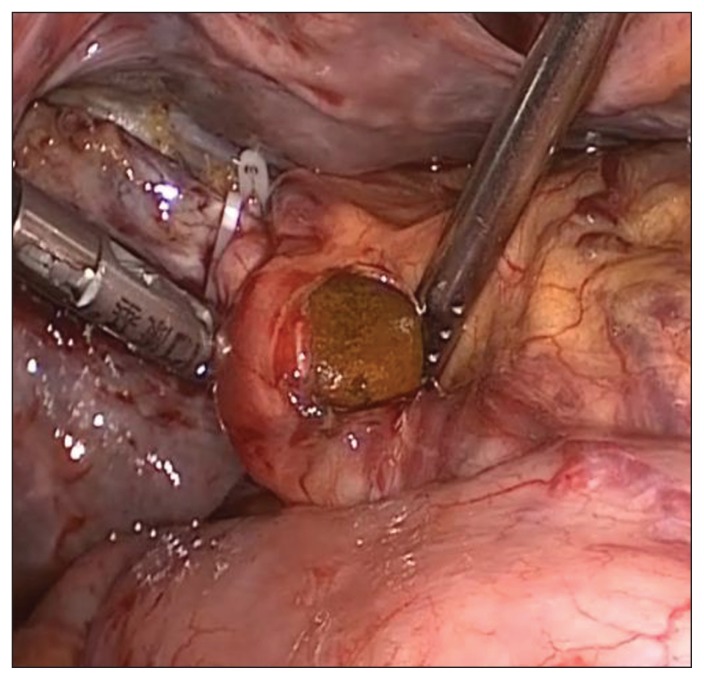
Fig. 1.
Retrieval of a common bile duct stone.
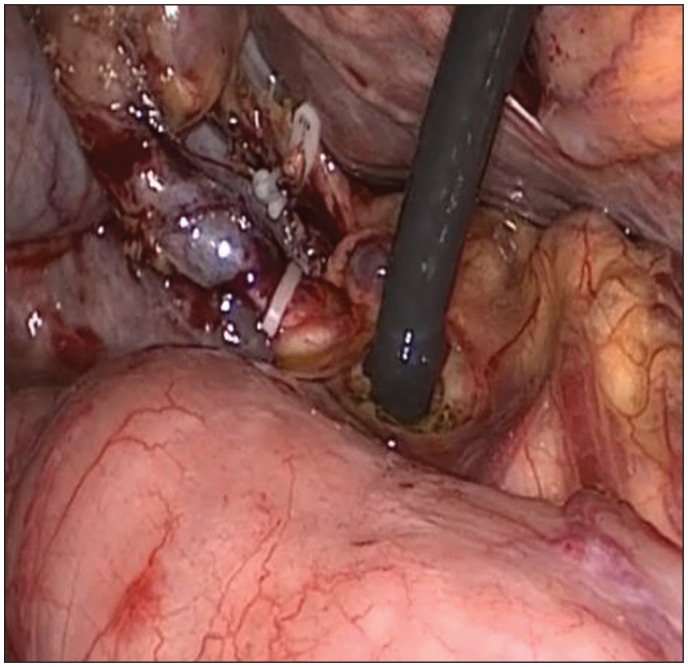
Fig. 3.
Laparoscopic placement of the T-tube with endosuturing techniques.
Data collection
The following variables were documented for each case: age, sex, American Society of Anesthesiologists (ASA) grade, acute biliary-related affections, preoperative ERCP, previous upper abdominal surgery, white cell count, serum total bilirubin (BIL), serum alkaline phosphatase (ALP), serum alanine transferase (ALT), albumin, creatinine, medical risk factors (MRFs), preoperative CBD diameter, number of stones (> 3 or ≤ 3) and presence of biliary sludge. We defined MRFs as any cardiovascular or respiratory condition requiring long-term drug therapy, diabetes mellitus requiring oral hypoglycemic agents or insulin, any medical condition requiring long-term steroids, cirrhosis, uremia and any major psychiatric disorder (psychosis or dementia) or central nervous system disturbance (hemiplegia, multiple sclerosis). We divided patients into 2 groups (≥ 1 MRFs v. no MRFs) without any attempt at weighting.
The following adverse outcomes were identified as being suitable for investigation.
Complications: postoperative complications were stratified using a validated classification system developed by Dindo and colleagues (the Clavien system).11 This system stratifies complications into 5 grades: any deviation from the normal postoperative course (grade I), those requiring certain pharmacological interventions (grade II), those requiring surgical intervention (grade III), life-threatening complications (grade IV) and death (grade V). We sought predictors of relatively severe, Clavien grade II–V, complications.
Conversion to an open operation.
Failed surgical clearance, which we defined as failure to clear the bile duct of stones at operation, requiring subsequent intervention.
Statistical analysis
Quantitative variables are expressed as means and standard deviations (SD). Categorical variables are presented as values and percentages. We assessed potentially relevant risk factors by univariate analysis with the χ2 statistic in the case of categorical variables and using simple logistic regression in the case of continuous variables. A significance level of p < 0.05 was used to identify factors on univariate analysis to enter into multivariate models. On multivariate analysis, we considered results to be significant at p < 0.05. We used the Hosmer–Lemeshow test to assess goodness of fit. The area under the receiver operating characteristic curve was calculated to evaluate diagnostic accuracy. We conducted all statistical analyses using SPSS version 13.0 for Windows (SPSS Inc.).
Results
During a period of 7 years, 201 patients with a confirmed diagnosis of CBD stones were treated with LC. The patient demographic and clinical characteristics are shown in Table 1. In all, there were 52 (25.9%) men and 149 (74.1%) women with a mean age of 57 (range 16–80) years. Of these, 192 (95.5%) patients had ASA I and II grade disease, and 9 (4.5%) had ASA III and IV grade disease. Twenty-two (10.9%) patients had undergone previous abdominal surgery. Nine patients had a history of cholecystectomy. Sixty-three procedures were carried out in the first 3 years and 138 in the latter 4 years of the study. A total of 149 patients were managed with a T-tube, 36 were managed with an ENBD tube, and 16 had a primary closure of the CBD. Of the 201 patients who underwent LC, adverse outcomes occurred in 48 (23.9%; Table 2). Clavien grade II–V complications occurred in 43 (21.4%) patients: grade II in 24 (11.9%), grade III in 21 (10.4%) and grade IV in 2 (1.0%). There was 1 death (grade V) for a mortality of 0.5%; it occurred in a 70-year-old patient with acute pancreatitis and jaundice who had failed clearance at previous ERCP and died from biliary peritonitis, sepsis and multiorgan failure after emergency surgery. Retained CBD stones were observed in 8 (4%) patients. The residual stones were removed through the T-tube tract by choledochoscopy in 6 of these 8 patients. The remaining 2 patients underwent postoperative ERCP. Conversion to laparotomy occurred in 7 (3.5%) cases owing to choledochojejunostomy in 3 patients with a markedly dilated CBD and distal biliary stricture harboring multiple stones, impacted stones in 1 patient, and severe acute cholecystitis or difficult access to CBD in 3 patients. Some patients had more than 1 adverse outcome.
Table 1.
Demographic and clinical characteristics of patients who underwent laparoscopic choledochotomy
| Characteristic | Mean (SD) [range]* |
|---|---|
| Age, yr | 56.9 (12.7) [16–80] |
| Sex, no. (%) male | 52 (25.9) |
| Acute biliary-related affections, no. (%) | 63 (31.3) |
| Preoperative ERCP, no. (%)† | 58 (28.9) |
| Previous upper abdominal surgery, no. (%) | 22 (10.9) |
| Presence of medical risk factors, no. (%) | 89 (44.3) |
| White blood cell count, × 109/L | 9.3 (5.2) [3.2–26.7] |
| Serum creatinine, μmol/L | 62.7 (15.0) [34–100] |
| Serum total bilirubin, μmol/L | 79.0 (84.9) [9.1–368.4] |
| Serum alkaline phosphatase, IU/L | 385.8 (394.9) [47–2107] |
| Serum alanine transferase, IU/L | 142.8 (152.9) [12–776] |
| Serum albumin, g/L | 40.7 (4.7) [30–49] |
| ASA grade (I or II), no. (%) | 192 (95.5) |
| Preoperative CBD diameter, mm | 16.5 (4.8) [8–32] |
| More than 3 stones, no. (%) | 104 (51.7) |
| Presence of biliary sludge, no. (%) | 50 (24.9) |
ASA = American Society of Anaesthesiology; CBD = common bile duct; ERCP = endoscopic retrograde cholangiopancreatography; SD = standard deviation.
Unless otherwise indicated.
Included acute pancreatitis, acute cholecystitis, acute cholangitis. More biliary-related complications may coexist in the same patient. Isolated jaundice, chronic cholecystitis, biliary colic pain and asymptomatic alteration of hepatic enzymes are not considered.
Table 2.
Adverse outcomes in 201 patients undergoing laparoscopic choledochotomy*
| Adverse outcome | No. (%) |
|---|---|
| Conversion to laparotomy | 7 (3.5) |
| Retained CBD stones | 8 (4.0) |
| Clavien grade V complication (death) | 1 (0.5) |
| Clavien grade IV complication | |
| Neurological ischemic stroke | 1 (0.5) |
| Left ventricular failure | 1 (0.5) |
| Clavien grade III complication | |
| Bile leak requiring ERCP or percutaneous drainage | 9 (4.5) |
| Pleural effusion requiring drainage | 5 (2.5) |
| Intra-abdominal collection requiring drainage | 5 (2.5) |
| Intra-abdominal bleeding requiring reoperation | 2 (1.0) |
| Clavien grade II complication | |
| Tachyarrhythmia | 7 (3.5) |
| Chest infection | 6 (3.0) |
| Cholangitis | 5 (2.5) |
| Urinary tract infection | 2 (1.0) |
| Infectious diarrhea | 2 (1.0) |
| Acute pancreatitis — de novo | 2 (1.0) |
CBD = common bile duct; ERCP = endoscopic retrograde cholangiopancreatography.
Some patients had more than 1 adverse outcome.
Predictors of adverse outcomes
The results of our analysis of risk factors for adverse outcomes are shown in Table 3. According to the data from univariate analysis, 7 variables — the presence of MRFs, BIL, number of stones, ALP, ALT, white cell count and acute biliary-related affections — were found to be significantly associated with adverse outcomes. Multivariate analysis showed that only 2 factors had independent significance in terms of predicting adverse outcomes: BIL and the presence of MRFs. We calculated the probability (p) of adverse outcomes using the following formula:
Table 3.
Risk factors for adverse outcomes after laparoscopic choledochotomy in the univariate and multivariate analysis*
| Risk factor | Patients with adverse outcomes n = 48 | All patients n = 201 | Univariate p value | Odds ratio (95% CI) |
|---|---|---|---|---|
| Significant in the multivariate analysis | ||||
| Presence of medical risk factors, no. (%) | 32 (66.7) | 89 (44.3) | < 0.001 | 2.66 (1.22–5.80) |
| Serum total bilirubin, mean (SD) μmol/L | 157.8 (117.1) | 79.0 (84.9) | < 0.001 | 1.01 (1.00–1.02) |
| Significant in the univariate analysis only | ||||
| More than 3 stones, no. (%) | 31 (64.6) | 104 (51.7) | 0.041 | |
| Serum alkaline phosphatase, mean (SD) IU/L | 546.9 (532.4) | 385.8 (394.9) | 0.002 | |
| White blood cell count, mean (SD) × 109/L | 11.8 (6.2) | 9.3 (5.2) | < 0.001 | |
| Serum alanine transferase, mean (SD) IU/L | 210.7 (174.7) | 142.8 (152.9) | 0.001 | |
| Acute biliary-related affections, no. (%) | 28 (58.3) | 63 (31.3) | < 0.001 | |
CI = confidence interval; SD = standard deviation.
Only risk factors that were significant (p < 0.05) in the univariate analysis were included in the multivariate analysis.
The presence of 1 or more MRFs was expressed as 1, and the absence of MRFs was expressed as zero; BIL was expressed in μmol/L. The Hosmer–Lemeshow goodness of fit test indicated satisfactory fit (p > 0.05). The area under the receiver operating characteristic curve was 0.812. A cut-off value of logit p = −1.32 was selected with a sensitivity and specificity of 75.0% and 77.1%, respectively. According to their logit(p), all patients were divided into a low-risk group (logit(p) ≤ −1.32, n = 130) and a high-risk group (logit(p) > −1.32, n = 71). Patients in the low-risk group had about a 1 in 10 chance (12 of 130) of adverse outcomes developing. Of these 71 patients in the high-risk group, 36 (50.7%) experienced adverse outcomes.
Predictors of Clavien grade II–V complications
We analyzed risk factors for Clavien grade II–V complications. According to the data from univariate analysis, 7 variables — the presence of MRFs, BIL, number of stones, ALP, ALT, white cell count and acute biliary-related affections — were significantly associated with complications. Multivariate analysis showed that BIL and the presence of MRFs had independent significance in terms of predicting complications. We calculated the probability (p) of complications using the following formula:
Predictors of other adverse outcomes
Owing to the small numbers of patients who had retained CBD stones or whose operations were converted to laparotomy, a similar analysis was not possible for this group.
The influence of the learning curve
The first 3 years of the series, referred to as the learning curve period, was not associated with the occurrence of adverse outcomes, complications, conversion to laparotomy and retained CBD stones (all p > 0.05). Adverse outcomes occurred in 13 of 63 (20.6%) patients during this period compared with 35 of 138 (25.4%) patients afterwards.
Discussion
We examined the incidence of and the risk factors associated with adverse outcomes after LC for the management of CBD stones. We selected this procedure because there are only a few series that report the results of LC, and because LC is still a difficult procedure with higher documented morbidity than the transcystic approach.6 Most series continue to pool the results of transcystic and transductal approaches, and many have a relatively low proportion of LC. For example, Tinoco and colleagues7 recently reported 481 laparoscopic CBD explorations, of which 69 were formal choledochotomy, and Riciardi and colleagues12 reported 76 transductal procedures out of 346 explorations.5,7,8,12
In the present study, postoperative adverse outcomes occurred in 23.9% of patients. In this group, Clavien grade II–V complications occurred in 21.4% of patients, retained CBD stones were observed in 4%, and conversion to laparotomy occurred in 3.5%. These outcomes are relatively similar to those observed in other studies.5,6,8,10,13
According to the data from multivariate analysis, the serum BIL and the presence of MRFs were significantly associated with adverse outcomes. The presence of toxic substances, such as BIL and bile salts, impaired liver function, and altered nutritional status due to obstructive jaundice have been characterized as factors for the development of complications, including acute renal failure, cardiovascular depression, hemorrhage from vitamin K deficiency and septicaemia.14,15 An obstructed biliary tree is likely to be infected and, as a consequence, there will be a higher incidence of severe chronic cholecystitis found at operation, necessitating conversion.8 In addition, patients with higher BIL were more likely to undergo an emergency operation, and an emergency operation was a risk factor for poor outcomes.16 As a result, BIL was one of the risk factors for adverse outcomes. Morbidity was significantly higher in patients with severe comorbidities who may not have been able to tolerate longer procedures than in those without comorbidities, whereas patient age had no influence on morbidity.5 The findings of the present investigation also showed that having MRFs was associated with increased postoperative complications. According to these risk factors, patients could be divided into a low-risk group and a high-risk group. The implications of these findings are as follows:
For patients without MRFs and a BIL of 114.2 μmol/L or lower, LC is a safe and advantageous procedure and can result in low rates of adverse outcomes. If patients with 1 or more MRFs and a BIL of 44.4 μmol/L or lower, LC is also recommended if the surgeons have the skill and facilities required for the procedure.
For patients without MRFs and a BIL higher than 114.2 μmol/L, or patients with 1 or more MRFs and a BIL higher than 44.4 μmol/L, medical treatment is preferred to lower the BIL. Laparoscopic choledochotomy is still a good choice for patients who respond to the medical treatment, especially those whose gallbladder is left in situ, and for young patients with preservation of the biliary sphincter. In this series, previous ERCP was not found to be a predictor of adverse outcomes. These data are similar to those reported by other authors.8,17,18 For patients who fail to respond to medical treatment, biliary drainage (ENBD or stenting) or stone extraction, is therefore indicated. Whether further endoscopy or LC should be adopted will largely depend on local availability of surgical and endoscopic skills.
We found that the learning curve period was not associated with the occurrence of adverse outcomes. These findings may be explained in part by the fact that the presence of more MRFs and higher BIL were found in the latter period. We found MRFs in 20 of 63 (31.7%) patients in the early period compared with 69 of 138 (50%) afterwards (p = 0.016). The mean (SD) BIL was 64.6 (80.6) μmol/L in the early period compared with 85.6 (86.2) μmol/L afterwards, although the differences were not significant.
Limitations
The principal limitation of this study was its nonrandomized and retrospective nature, with a selection bias in LC. Our study was conducted in only 1 medical centre, which may limit the generalizability of our results. Even so, the data from our current study could provide the support for future prospective and randomized investigation.
Conclusion
Laparoscopic choledochotomy is a safe and effective treatment in most cases of CBD stones. The incidence of adverse outcomes is low, but a high BIL and the presence of MRFs do not favour the success of the procedure.
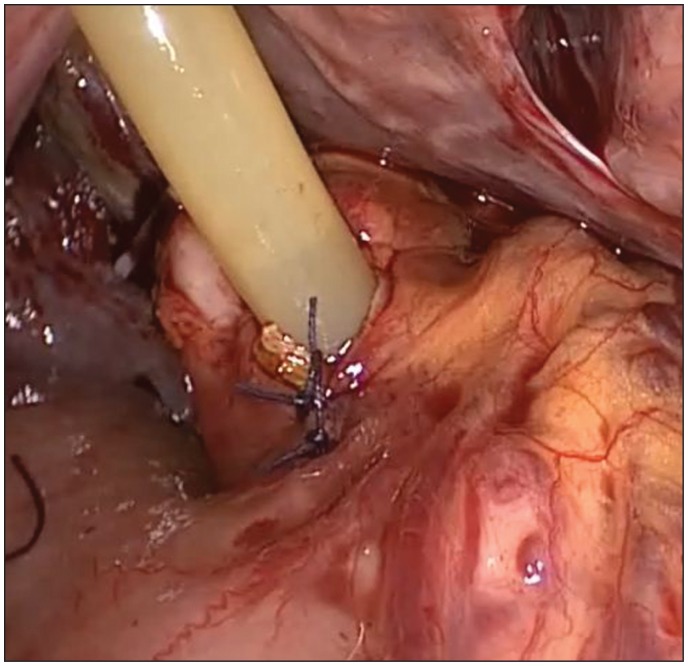
Fig. 2.
Choledochoscope inserted through choledochotomy incision.
Acknowledgments
We would like to thank the other members of the Department of Surgery in taking care of the patients.
Footnotes
Competing interests: None declared.
Contributors: X. Ye and X. Hong designed the study and reviewed the article. X. Teng and K. Xie acquired the data, which X. Ye, X. Hong and K. Ni analyzed. X. Ye, K. Ni, X. Teng and K. Xie wrote the article. All authors approved its publication.
References
- 1.Morino M, Baracchi F, Miglietta C, et al. Preoperative endoscopic sphincterotomy versus laparoendoscopic rendezvous in patients with gallbladder and bile duct stones. Ann Surg. 2006;244:889–93. doi: 10.1097/01.sla.0000246913.74870.fc. discussion 93–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Vandervoort J, Soetikno RM, Tham TC, et al. Risk factors for complications after performance of ERCP. Gastrointest Endosc. 2002;56:652–6. doi: 10.1067/mge.2002.129086. [DOI] [PubMed] [Google Scholar]
- 3.Martin DJ, Vernon DR, Toouli J. Surgical versus endoscopic treatment of bile duct stones. Cochrane Database Syst Rev. 2006:CD003327. doi: 10.1002/14651858.CD003327.pub2. [DOI] [PubMed] [Google Scholar]
- 4.Williams EJ, Green J, Beckingham I, et al. Guidelines on the management of common bile duct stones (CBDS) Gut. 2008;57:1004–21. doi: 10.1136/gut.2007.121657. [DOI] [PubMed] [Google Scholar]
- 5.Berthou J, Dron B, Charbonneau P, et al. Evaluation of laparoscopic treatment of common bile duct stones in a prospective series of 505 patients: indications and results. Surg Endosc. 2007;21:1970–4. doi: 10.1007/s00464-007-9387-5. [DOI] [PubMed] [Google Scholar]
- 6.Thompson MH, Tranter SE. All-comers policy for laparoscopic exploration of the common bile duct. Br J Surg. 2002;89:1608–12. doi: 10.1046/j.1365-2168.2002.02298.x. [DOI] [PubMed] [Google Scholar]
- 7.Tinoco R, Tinoco A, El-Kadre L, et al. Laparoscopic common bile duct exploration. Ann Surg. 2008;247:674–9. doi: 10.1097/SLA.0b013e3181612c85. [DOI] [PubMed] [Google Scholar]
- 8.Noble H, Whitley E, Norton S, et al. A study of preoperative factors associated with a poor outcome following laparoscopic bile duct exploration. Surg Endosc. 2011;25:130–9. doi: 10.1007/s00464-010-1146-3. [DOI] [PubMed] [Google Scholar]
- 9.Huang SM, Wu CW, Chau GY, et al. An alternative approach of choledocholithotomy via laparoscopic choledochotomy. Arch Surg. 1996;131:407–11. doi: 10.1001/archsurg.1996.01430160065012. [DOI] [PubMed] [Google Scholar]
- 10.Chander J, Vindal A, Lal P, et al. Laparoscopic management of CBD stones: an Indian experience. Surg Endosc. 2011;25:172–81. doi: 10.1007/s00464-010-1152-5. [DOI] [PubMed] [Google Scholar]
- 11.Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004;240:205–13. doi: 10.1097/01.sla.0000133083.54934.ae. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Riciardi R, Islam S, Canete JJ, et al. Effectiveness and long-term results of laparoscopic common bile duct exploration. Surg Endosc. 2003;17:19–22. doi: 10.1007/s00464-002-8925-4. [DOI] [PubMed] [Google Scholar]
- 13.Tokumura H, Umezawa A, Cao H, et al. Laparoscopic management of common bile duct stones: transcystic approach and choledochotomy. J Hepatobiliary Pancreat Surg. 2002;9:206–12. doi: 10.1007/s005340200020. [DOI] [PubMed] [Google Scholar]
- 14.van der Gaag NA, Kloek JJ, de Castro SM, et al. Preoperative biliary drainage in patients with obstructive jaundice: history and current status. J Gastrointest Surg. 2009;13:814–20. doi: 10.1007/s11605-008-0618-4. [DOI] [PubMed] [Google Scholar]
- 15.Wang Q, Gurusamy KS, Lin H, et al. Preoperative biliary drainage for obstructive jaundice. Cochrane Database Syst Rev. 2008:CD005444. doi: 10.1002/14651858.CD005444.pub2. [DOI] [PubMed] [Google Scholar]
- 16.Ingraham AM, Cohen ME, Bilimoria KY, et al. Comparison of 30-day outcomes after emergency general surgery procedures: potential for targeted improvement. Surgery. 2010;148:217–38. doi: 10.1016/j.surg.2010.05.009. [DOI] [PubMed] [Google Scholar]
- 17.Poole G, Waldron B, Shimi SM, et al. Laparoscopic common bile duct exploration after failed endoscopic stone extraction. Endoscopy. 1997;29:609–13. doi: 10.1055/s-2007-1004265. [DOI] [PubMed] [Google Scholar]
- 18.Karaliotas C, Sgourakis G, Goumas C, et al. Laparoscopic common bile duct exploration after failed endoscopic stone extraction. Surg Endosc. 2008;22:1826–31. doi: 10.1007/s00464-007-9708-8. [DOI] [PubMed] [Google Scholar]