Abstract
Objectives
To describe the informal care network of U.S. veterans referred to home and community-based services (Homemaker Home Health services, H/HHA, or Home-Based Primary Care, HBPC) at the Durham Veterans Affairs Medical Center (VAMC), including: quantity and types of tasks provided and desired content for caregiver training programs.
Methods
All primary care patients referred to H/HHA or HBPC during the preceding 3 months were sent questionnaires in May 2007. Additionally, caregivers were sent questionnaires if a patient gave permission. Descriptive statistics and chi-squared tests were performed.
Results
On average, patients received 5.6 hours of VA care and 47 hours of informal care per week. 26% of patients (38% of patients with caregiver proxy respondents) and 59% of caregivers indicated the caregiver would be interested in participating in a training program by phone or on-site. Significant barriers to participation existed. The most common barriers were: transportation; no time due to caregiving or work demands; caregiver's own health limitations; and no need.
Conclusions
Caregiver training needs to be tailored to overcome barriers to participate. Overcoming these barriers may be possible through in-home phone or internet training outside traditional business hours, and by tailoring training to accommodate limiting health problems among caregivers.
Keywords: Informal care, caregiver training programs, VA patients, frail elderly
Introduction
With the rapid growth of the elderly population in the United States, especially those 85 and older, an increasing number of individuals will experience a loss of independence. Although institutionalized long-term care may be an option, many elders prefer to stay at home. Remaining at home often requires support, which may be provided by formal programs (e.g., home health agencies) or informal caregivers (e.g., spouses or adult children who provide unpaid assistance). Informal caregivers of elderly adults often experience stress, economic hardship, and burnout, which increases the elderly adult's risk of nursing home admission1-3,4. Thus, an important policy issue is how to provide support to informal caregivers so that elderly adults can remain home—generally the preferred and less expensive alternative to institutionalized long-term care (LTC)5.
Issues surrounding informal caregivers have become important in the Veterans Health Administration (VHA). Through the passage of the United States Millennium Healthcare and Benefits Act 6, the VHA is committed to providing high-quality long-term care to U.S. veterans in the least restrictive setting possible—the patient's home. When considering the projected increase in the number of frail elderly veterans and the high cost of long-term care (LTC), this commitment is expected to create an enormous financial burden on the VHA. The Millennium Act greatly expanded home and community-based services (VA-HCBS), including Homemaker Home Health Services (H/HHA) which offers assistance with bathing, transferring, and other daily personal care, and Home-Based Primary Care (HBPC), which provides interdisciplinary longitudinal primary care to veterans with advanced chronic disease through home visits from a physician-led team of primary care providers.7
VA-HCBS often complement services provided by informal caregivers to help maintain veterans at home. However, to effectively provide care, informal caregivers may benefit from skills training programs. Developing such programs is challenging for three reasons: (1) we do not whether informal caregivers perceive a need for training programs; (2) even if they desire such programs, we do not know the areas in which caregivers desire training; and (3) most research on informal caregivers study spouses of elders with dementia;7 however, veterans requiring VA-HCBS have complex and heterogeneous conditions and needs 8 that may differ from dementia.
This study describes the informal and formal care infrastructure among veterans and the perceived need for caregiver training among veterans and caregivers for a patient cohort referred to VA-HCBS. Through this study, we will learn about the need, feasibility and desired content of caregiver programs to support caregivers of frail veterans with chronic disease.
Methods
The study was conducted at a large academically-affiliated Veterans Affairs Medical Center (VAMC) in Durham North Carolina, The United States. We worked with Department of Social Work and the HBPC program to identify all primary care patients referred to or receiving VA-HCBS between January and March, 2007 (N=212). After pilot testing the survey on 7 patients, we mailed questionnaires to patients in May 2007. The survey included a request to provide contact information for the family member or friend who helped the most in the home. We mailed separate questionnaires to these informal caregivers. For both patients and caregivers, we sent follow-up reminder postcards if they had not responded within two and four weeks. Incentives of $10.00 were given to patients and caregivers upon completion of the survey. Survey instruments are available upon request. This study was approved by the Durham VAMC and the Duke Medical Center Institutional Review Boards.
Measures
Patient
Formal care
We asked patients whether they received home health aide services, home health care, or HBPC.
Primary informal caregiver
The veteran was asked who cared for them the most (i.e., family member, friend, unpaid person); where the primary caregiver lived; and the number of unpaid caregivers helping him or her. Patients who reported not receiving any informal care assistance were coded as not having an informal caregiver.
Hours of informal and formal care received
We asked: (1) “In a usual week, how many days per week do you receive VA (non-VA, informal care) services in your home?” and (2)“On the days that you receive VA (non-VA, informal care) services, about how much time per day does an aide (informal caregiver) help you?” From these questions, we calculated the average hours per week that a patient received VA HCBS, non-VA HCBS, and informal care. A patient may have received non-VA services if they wanted to receive additional services in the home or if they did not qualify for VA services (due to their military disability eligibility or budget limitations). Non-VA HCBS may be paid for out-of-pocket or by other government programs (e.g. Medicare or Medicaid).
Care tasks from informal or formal caregivers
Veterans were asked to identify all tasks their caregiver(s) or providers helped with because of their medical problems.
Unmet need for care
We asked veterans to estimate the hours per week they received VA-HCBS and the how much more time per week they needed VA-HCBS.”
Desired content of a caregiver training program
We asked veterans to select areas for training (complete list on bottom of Table 4) that they thought would be useful to their primary caregiver or other caregivers to learn about in programs held by the VA. We also asked whether they thought their caregiver would be able to participate in a one-hour monthly on-site training program or a one-hour weekly phone training program. They were asked to provide reasons their caregiver would not be able to participate.
Table 4. Top five types of training that would be useful to your primary caregiver/you in a training session held by the VA, by type of respondent.
| Rank of categories | Patient with no caregiver help filling out survey | Patient with help from caregiver filling out survey | Caregiver Report from caregiver survey |
|---|---|---|---|
| (N=42) | (N=47) | (N=17) | |
| (% number of observations) | |||
| 1. | Adapting The home Environment (36.2%; n=15) | When and how to ask for more help (52.4%;n=25) | Organizing preventive care for patient (58.8%;n=10) |
| 2. | When and How to Ask for more help (31.9%;n=13) | Getting respite2 Services or other Services for patient (47.6%;n=22) | When and3 How to Ask for more Help (47.1%;n=8) |
| 3. | Coping with1 Caregiving (27.6%;n=12) | Coping with2 Caregiving (47.6%;n=22) | Taking care3 Yourself as caregiver (47.1%;n=8) |
| 4. | Taking care of1 Yourself as caregiver (27.6%;n=12) | Taking care of Yourself as caregiver (45.2%;n=21) | Coping with4 Caregiving (41.2%;n=7) |
| 5. | More about patient's1 Disease and what to Expect next (27.6%=n=12) | More about patient's disease and what to Expect next (40.5%;n=19) | Getting respite4 Service or other Service for patient (41.2%;n=7) |
| Identifying when1 To call a doctor (27.6%;n=12) | |||
| None of them | 19.1%; n=8 | 7.1%;n=3 | 0%; n=0 |
Data source: The patient survey (data column 1,2) and caregiver survey (data column 3) Note: The full list of items was managing medication; safe transferring; safe bathing; how to help change patient's diet; identifying when to call a doctor; adapting the home environment; coping with caregiving; taking care of yourself as a caregiver; when and how to ask for more help; organizing preventive care for the veteran; getting respite services and/or other services for your patient; dealing with incontinence; more about patient's disease and what to expect next; how to communicate better with patient and/or medical providers; how to help patients with pain management; other (please explain). 1. Ranks no different from each other. 2. Ranks no different from each other. 3. Ranks no different from each other. The n in parentheses was rounded to the nearest whole number.
Health
Patients were asked what medical problems caused them to need extra help in their home from a list of the 12 conditions that were most prevalent among all VA H/HHA recipients in 2002-20038. In addition, patients were asked their self-rated health status (1=excellent, 5=poor), their height and weight, and a 2-item depression screen.9
Demographics
Patients reported their age, marital status, number of household members, ethnicity, race, education, work status, household income, and supplemental health insurance.
Caregiver
Prior training
We asked whether caregivers ever received caregiver training, and if yes, what types of tasks and who provided the training.
Interest in participating in training
Caregivers were asked to identify which of 17 topics they thought would be useful for them to learn more about. They could also suggest other topics. We asked them about their willingness to participate in training sessions through either monthly programs at the Durham VAMC or one-hour weekly telephone calls.
Confidence
Caregivers were asked about their confidence (not at all, somewhat or very) regarding: (1) taking care of their patient's physical needs; (2) taking care of their patient's emotional needs; (3) identifying services for their patient; and (4) coping with the stress of being a caregiver. This variable was dichotomized as not at all vs. somewhat or very confident.
Unmet need
Caregivers were asked whether, when considering all care provided by VA (non-VA) HCBS providers, it was enough to take care of the patient's needs. If not, they were asked how many more hours a week of VA (non-VA) HCBS they would need.
Health and Demographics
Caregivers were asked about their self-rated health status (1=excellent, 5=poor), height and weight, the 2-item depression screen, age, marital status, number of household members, ethnicity, race, education, work status, income, and health insurance.
Statistical Analysis
We present descriptive statistics of patients and caregivers and the informal and formal care infrastructure. We also present the caregiver data on perceived need for training, barriers to training, and caregiver confidence. We then present the items that patients and caregivers identified as being useful in training sessions and report common barriers to training.
Results
Of 212 patients who were mailed surveys, five were returned with addresses that could not be reconciled. Of the remaining 207 patients, 89 (43%) returned completed surveys; 42 patients provided their primary caregiver's contact information, 17 of whom (40%) returned completed surveys. Notably, 58% of patients reported receiving help completing the questionnaire, generally from the informal caregiver (52%). Thus, for half of the patients, responses may have been influenced by the informal caregivers.
Patient Survey Results
Demographics
Patient mean age was approximately 74.6 years; approximately half were married; 28% were African-American; 65% completed high school; and more than half had annual incomes below $30,000 (Table 1). Approximately 89% reported having an informal caregiver, usually the spouse or adult child (Table 1).
Table 1. Patient and Caregiver Demographics (N=89; N=17).
| Variable description | PATIENTS (N=89) | CAREGIVERS (N=17) |
|---|---|---|
| Mean/(Std.Dev. or number of observations) | ||
| Age | 74.6 (12.0) | 66.63 (10.7) |
| Marital Status | ||
| Married | 52.8% (47) | 88.2% (15) |
| Single | 37.1% (33) | 11.8% (11) |
| Divorced | 12.4% (11) | 5.9% (1) |
| Widowed | 19.1% (17) | 5.9% (1) |
| Never married | 5.6% (5) | 00.0% (0) |
| Missing status | 10% (9) | 00.0% (0) |
| Race | ||
| Black | 28.1% (25) | 05.9% (1) |
| Other | 2.2% (2) | 11.8% (2) |
| White | 61.8% (55) | 48.8% (8) |
| Missing race | 7.9% (7) | 27.1% (5) |
| Number in household | 1.69 (4.26) | 1.25 (.577) |
| Completed high school | 65.2% (58) | 88.2% (15) |
| Household Income pre-tax | ||
| Less than $10,000 | 6.7% (6) | 0.0 (0) |
| $10,000-$19,999 | 28.1% (25) | 0.0 (0) |
| $20,000-$29,999 | 20.3% (18) | 5.9% (1) |
| $30,000-$39,999 | 15.6% (14) | 35.3% (6) |
| $40,000-$49,999 | 3.1% (3) | 00.0% (0) |
| $50,000-$59,999 | 10.9% (10) | 17.6% (16) |
| $60,000-$79,999 | 9.4% (8) | 17.6% (16) |
| $80,000 or more | 3.1% (3) | 5.9% (5) |
| Health | ||
| Self-rated health (1=exc, 5=poor) | 4.0 (1.0) | 2.9 (.81) |
| Depressive symptoms (2 items “yes”) | 29% (26) | 23.5% (21) |
| Health insurance other than VA | ||
| Medicare | 65.1% (58) | 52.9% (9) |
| Medicaid | 6.7% (6) | 0% (0) |
| Private/HMO | 19.1% (17) | 52.9% (9) |
| Long-term Care Insurance | 2.2% (2) | 11.8% (2) |
| Relationship to caregiver (among 89% of sample receiving informal care) | ||
| Spouse | 52.8% (47) | |
| Daughter | 12.4% (11) | |
| Sons | 9.0% (8) | |
| Friend | 4.5% (4) | |
| Sibling | 3.4% (3) | |
| Parent | 2.2% (2) | |
| Other (relative, unknown) | 15.7% (14) | |
| Coresiding with caregiver | 60.7% (54) | |
| Coresiding w/non-spouse caregiver | 40.5% (36) | |
Data source: The patient survey (data column 1) and caregiver survey (data column 2)
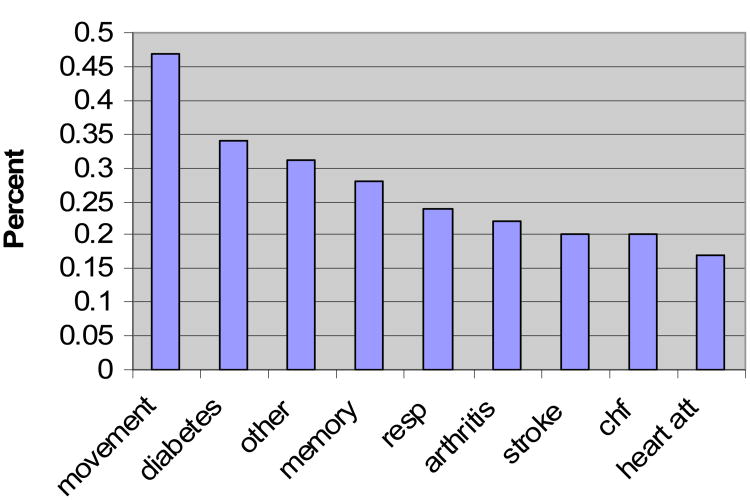
Health
Patients reported multiple limitations and chronic illnesses for which they needed extra help, including movement problems (47%), diabetes (34%), and memory problems (28%) (see Figure 1). On average the respondents had 2.74 problems or illnesses (of 13) requiring them to need help (see note on Figure 1 for full list). Additionally, patients reported needing help with 3.6 (of 7) activities of daily living (ADLs) and 3.9 (of 6) instrumental activities of daily living (IADLs). Nearly 30% of patients screened positive for probable depression. Sixty-four percent of patients reported being unable to drive to the doctor, 57.3% could not do housework and nearly 50% could not get around outside without help (Table 2). Nearly half (46%) needed help with medication management.
Figure 1. Common Conditions for Patients in the Sample.
Data source: The patient survey
X-axis legend: Movement=movement problems; diabetes=type 1 or type 2 diabetes; other=compilation of conditions written in by respondent; memory=memory problems; resp=respiratory problems; arthritis=any type of arthritis; stroke=stroke or transient ischemic attack; chf=congestive heart failure; heart att=heart attack.
Note: The 13 response options were: stroke; respiratory problems (such as COPD or asthma); cancer; heart failure; heart attack diabetes; arthritis; hip or knee replacement; amputation; cirrhosis/liver damage; movement problems; memory problems; and other (please explain).
Table 2. Assistance needed and assistance received by patient from informal caregiver or home health aide, Patient survey. (N=89).
| Description of Task | Percent (n) Need help With… | Percent (n) Cannot do Without help… | Percent (n) Caregiver Helps with… | Percent (n) Home Health Aide Helps With… |
|---|---|---|---|---|
| ADL Tasks | ||||
| Getting around inside your home | 30.3% (27) | 25.8% (23) | 44.9% (40) | 29.2% (26) |
| Getting around outside your home | 27.0% (24) | 49.4% (44) | 55.1% (49) | 21.3% (19) |
| Eating | 23.6% (21) | 10.1% (9) | 43.8% (39) | 16.9% (15) |
| Getting in or out of bed | 25.8% (23) | 18.0% (16) | 34.8% (31) | 13.5% (12) |
| Getting dressed | 34.8% (31) | 21.3% (19) | 40.4% (36) | 22.5% (20) |
| Bathing | 28.1% (25) | 32.6% (29) | 40.4% (36) | 31.5% (28) |
| Getting on/off the toilet | 16.9% | 15.7% | 22.5% | 15.7% |
| IADL Tasks | ||||
| Managing your money or paying bills | 22.5% (20) | 40.4% (36) | 58.4% (52) | 6.7% (6) |
| Making telephone calls | 15.7% (14) | 23.6% (21) | 42.7% (38) | 7.9% (7) |
| Doing housework | 23.6% (21) | 57.3% (51) | 62.9% (56) | 16.9% (15) |
| Washing laundry | 23.6% (21) | 53.9% (48) | 58.4% (52) | 19.1% (17) |
| Shopping for your groceries | 27.0% (24) | 51.7% (46) | 68.5% (61) | 12.4% (11) |
| Preparing meals | 24.7% (22) | 48.3% (43) | 65.1% (58) | 18.0% (16) |
| Medical care tasks | ||||
| Driving to doctor or clinic | 16.9% (15) | 64.0% (57) | 62.9% (56) | 12.4% (11) |
| Filling your pill box for the week | 16.9% (15) | 46.1% (41) | 49.4% (44) | 12.4% (11) |
| Helping you take medicine | 28.1% (25) | 21.3% (21) | 48.0% (43) | 10.1% (9) |
| Managing side-effects from medication | 28.1% (25) | 24.7% (22) | 49.3% (44) | 12.4% (11) |
| Changing your bandages | 27.0% (24) | 27.0% (24) | 47.9% (43) | 18.0% (16) |
| Deciding whether to call a doctor | 23.6% (21) | 30.3% (27) | 51.7% (46) | 16.9% (15) |
| Average number of ADL tasks | 1.9 | 1.7 | 2.8 | 1.5 |
| Average number of IADL tasks | 1.4 | 2.8 | 3.6 | 0.8 |
| Average number of medical care tasks | 1.4 | 2.1 | 2.9 | 0.8 |
| Total number of tasks | 4.6 | 6.6 | 9.3 | 3.5 |
Data source: The patient survey (N=89)
Pathways and Infrastructure of HCBS
The most common ways to be referred to VA-HCBS (either H/HHA or HBPC) were either during a hospitalization (37%) or a doctor's visit (33.7%). Of the 89 patients referred, 68.5% received VA-HCBS (Table 3) and 28.1% received non-VA HCBS. Fewer than 5% received HCBS from non-VA sources only, whereas 23.6% of the sample received both VA and non-VA HCBS. The majority of patients had both VA-provided HCBS and informal care in the home (65.2%). 6.7% of patients reported having neither informal nor formal care in the home. Only 2.2% of respondents with VA-HCBS reported not having an informal caregiver. Respondents received VA–HCBS an average of 5.6 hours per week. For the 27 patients who received non-VA HCBS, the amount of services was 23.4 hours per week.
Table 3. The home care network among VA patients referred to H/HHA or HBPC (N=89).
| Formal Home Care | Informal Care | ||||||
|---|---|---|---|---|---|---|---|
|
|
|
||||||
| Types of services | Any | VA | HBPC | H/HHA | VA-D/K | Non-VA | Any |
| Percent (number of subjects rounded to nearest whole number) | |||||||
| Any formal care | 83.2% (74) | ||||||
| Any VA | 68.5% (61) | ||||||
| HBPC | 40.4% (36) | ||||||
| H/HHA | 20.2% (18) | 33.7% (30) | |||||
| D/K which | 0.0% (0) | 0.0% (0) | 14.6% (13) | ||||
| Any Non-VA | 23.6% (21) | 12.4% (11) | 11.0% (10) | 6.7% (6) | 28.1% (25) | ||
| Any Informal Care | 78.7% (70) | 65.2% (58) | 40.4% (36) | 33.7% (30) | 12.4% (11) | 27.0% (24) | 88.8% (79) |
Data source: The patient survey
Notes: Any formal care indicates VA home and community-based services (HCBS) or non-VA HCBS by any payer source.
HBPC = VA Home-Based Primary Care
H/HHA= VA Homemaker Home Health Aide Services
D/K = Do not know
Non-VA = Non-VA provided home health care, which could be paid for by the patient or caregiver or through some other governmental home health care benefit such as through Medicaid or Medicare
Perceived unmet need for formal home care
Of the patients who received VA-HCBS (N=48), 66% felt that the services received were enough to address their medical needs. For the remainder, they reported needing 8 additional weekly hours.
Intensity of Informal Care
Informal care intensity was much higher than formal care. Patients reported receiving informal care a mean of 4.9 days per week for a mean of 7.5 hours per day (or an average of 47 hours per week).
Perceived Need for Training
Patients reported that the training that would be most useful to their primary caregivers was adapting the home environment, learning to ask for more help, coping with caregiving, and taking care of themselves (Table 4). Of note, more patients without a proxy caregiver respondent than patients with a proxy caregiver respondent reported that none of the items would be useful (19% vs. 7%. p=.098).
Overall, 27.7% of patients reported that their caregivers would be able to participate in training: 21.3% for monthly training programs at the VA and 25.8% weekly phone training. Because nearly half of patients had their primary caregiver help them fill out the survey, we examined whether perceived need for training differed by having a caregiver proxy respondent. Among the 42 patients with caregiver proxy respondents, 38.1% reported that their caregiver would be able to take part in training (28.6% by phone versus 31.0% at the VA).
The main barriers of on-site training reported by patients were: transportation or distance (13.5%); caregiver's bad health (7.9%); caregiver's work demands (4.5%); and lack of need (4.5%). The main barriers for phone training included: lack of time (12.4%); lack of need (6.7%); caregiver's own health problems (5.6%); and caregiver's work demands (4.5%).
Caregiver Survey Results
Demographics
Caregivers who responded to the caregiver survey (N=17) were an average of 9 years younger than the patients (Table 1). Caregivers reported better health, although 23.5% screened positive for probable depression10.
Caregiver perceived need for training
Approximately half of caregivers reported that they had received training about how to help their veteran, generally related to clinical care tasks, such as wound care, blood sugar readings, or catheter care. The proportion of caregivers who reported that they would be interested in participating in a caregiver training program of either format was 58.8%: 47% were interested in phone-based programs and 29.4% were interested in training at the VA. The top ranked barriers for on-site training were: transportation (25%); lack of need or interest (18.8%); and lack of time (12.5%). For phone training, the most common barriers were lack of need (18.8%); time (6.3%); and patient would interrupt (6.3%). The most appealing training sessions were organizing preventive care for veterans, supporting self-care, and coping with caregiving (Table 4). Also important to caregivers was learning how to get more services for the veteran. Caregivers' interest in training was markedly different from patients
Caregiver confidence
Only 6% of caregivers reported being not at all confident in coping with the stress of being a caregiver and 12% reported being not at all confident they could take care of the veteran's physical needs. A higher proportion, 35%, felt not at all confident that they could find out about services for the veteran and 41% felt not at all confident that they could take care of their veteran's emotional needs.
Conclusions
We examined the need, feasibility and desired content of caregiver programs to support informal caregivers of frail U.S. veterans. Our sample included veterans with significant multimorbidity (mean of 2.74 problems requiring them to need help in the home) who were receiving or had been recently referred to H/HHA or HBPC. We found that these veterans received both formal and informal care, with average hours of informal care exceeding full-time employment per week (47 hours).
Given this heavy time burden, training programs for informal caregivers could have a large impact on patients and caregivers. However, whether or not caregivers would participate in training depended on who you asked. Only 26% of patients reported that their caregiver would participate in a training program (and 38% of patients with caregiver proxies). However, 58% of caregivers reported that they were interested in participating in training, especially by telephone. Notably, a sizable portion were not interested in participating, which may be explained by barriers such as transportation; lack of time; caregivers' own health problems; and no perceived need. The importance of caregiver health problems suggest that the caregiver's themselves may face health problems that may impede their ability to care for the patient.
Caregivers felt most confident about the physical care that they provided, but less secure about meeting patients' emotional needs and securing services for the patient. The types of training that held most interest overall to patients and caregivers were when and how to ask for more help, taking care of oneself, and coping. The most important area for training varied by respondent type. Thus, a training program that is tailored to incorporate the perceived needs of both patients and caregivers will likely be most effective because the participation of both the patient and the caregiver is critical for its success.
There are several limitations to our study. First, the study was conducted at a single VAMC, which limits generalizability. Second, the study was small. In particular, we only received responses from 17 caregivers, and caregivers who responded may not be representative of other caregivers of frail elders referred to VA-HCBS. Third, approximately half of the patients received help completing the survey from their primary informal caregiver. Thus, we cannot be certain whether and how patient responses were influenced by caregivers. In some instances, such as need for training, there were statistically significant differences in the results by whether or not a patient had help filling out the survey.
Maintaining frail patients in the location that they prefer is important to patient-centered care. Remaining at home is generally more desirable and less expensive. However, remaining at home often depends on informal caregivers11, 12. Training programs may be useful to maintain patients at home and obtain the best quality of care and outcomes. Understanding caregiver competencies and barriers is paramount to designing quality-enhancing training programs, because tailored interventions will maximize enrollment and impact. Overall, we found that caregiver training needs to be tailored to cover diverse patient and caregiver conditions and interests, and to overcome barriers to participate from time and transportation burdens, lack of interest, and frailty of the caregiver. The diverse barriers identified indicate that recruitment of caregivers of frail veterans with multiple conditions will be challenging. Possible solutions to these barriers include: (1) individual or group training by phone or some other media such as the internet so that caregivers will not have to leave the house; (2) offering sessions after business hours to accommodate work schedules among younger caregivers, and (3) tailoring the training to accommodate the high proportion of caregivers who have their own limiting health problems and who have limited confidence in how to meet the patients' emotional needs.
Our study focused on a system of care with minimal public support of informal caregivers and generous coverage for formal long-term care, the U.S. Veterans Health Care System. We know very little about the potential barriers to caregiver training in other systems, however, such as in countries with similarly generous formal long-term care benefits and generous supports for informal caregivers (e.g. Germany), or countries with limited publicly provided long-term care and no support to caregivers (e.g. emerging economy countries or developing countries). In the former, because there is a high level of administrative control, caregivers could be identified, queried, assessed, and trained through the formal long-term care system. Payments to caregivers from the state could even be tied to receipt of periodic training if desired. Among the latter type of countries, however, it could be a challenge to even identify informal caregivers. Yet caregiver training is likely even more imperative in these countries due to the lack of any viable long-term care alternative. More study is needed on how best to train informal caregiver programs in other health care systems, so that scarce resources and care recipient health can be optimized.
Acknowledgments
This research was supported by the VA Health Services Research and Development Merit Review Program (MRP 05-311) and Career Development Program (Dr. Weinberger), and by the Trajectories on Aging Center, Duke School of Nursing (P20 NR007795-04, Clipp, PI). The study team appreciates excellent assistance administering and managing the survey from Linda C. Folsom, Katrina A. Long, and Michelle Mitchell, Duke School of Nursing. Courtney Van Houtven is extremely grateful to Elizabeth C. Clipp for her mentoring and inspiration. Any mistakes or errors remain the authors'.
Contributor Information
Courtney Harold Van Houtven, Email: courtney.vanhoutven@duke.edu.
Eugene Z. Oddone, Email: oddon001@mc.duke.edu.
Morris Weinberger, Email: mweinber@email.unc.edu.
References
- 1.Schulz R, O'Brien AT, Bookwala J, Fleissner K. Psychiatric and physical morbidity effects of dementia caregiving: prevalence, correlates, and causes. Gerontologist. 1995;35:771–91. doi: 10.1093/geront/35.6.771. [DOI] [PubMed] [Google Scholar]
- 2.Fast JE, Williamson DL, Keating NC. The hidden costs of informal elder care. Journal of Family and Economic Issues. 1999;20:301–326. [Google Scholar]
- 3.Jette AM, Tennstedt S, Crawford S. How does formal and informal community care affect nursing home use? Journals of Gerontology, Series B, Psychological Sciences and Social Sciences. 1995;50:S4–S12. doi: 10.1093/geronb/50b.1.s4. [DOI] [PubMed] [Google Scholar]
- 4.Van Houtven CH, Voils CV, Clipp E, Weinberger M. A conceptual model of informal caregiver skills training programs. Durham, NC: 2009. [Google Scholar]
- 5.Van Houtven CH, Norton EC. Informal Care and Medicare Expenditures:Testing for Heterogeneous Treatment Effects. Journal of Health Economics. 2008;27:134–156. doi: 10.1016/j.jhealeco.2007.03.002. [DOI] [PubMed] [Google Scholar]
- 6.D.o.V. Affairs, editor. Geriatric and extended care (GEC) referral. VHA DIRECTIVE 2004-059. Veterans Health Administration; Washington, DC: 2004. pp. 1–5. [Google Scholar]
- 7.Thorpe J, Sleath B, Kalinowski C, et al. Caregiver psychological distress as a barrier to vaccination for influenza among community-dwelling elderly with dementia. Medical Care. 2006;44:713–721. doi: 10.1097/01.mlr.0000215905.36968.76. [DOI] [PubMed] [Google Scholar]
- 8.Van Houtven CH, Jeffreys A, Coffman C. Home Health Care and Patterns of Subsequent VA and Medicare Health Care Utilization for Veterans. The Gerontologist. doi: 10.1093/geront/48.5.668. In Press. [DOI] [PubMed] [Google Scholar]
- 9.Spitzer RL, Kroenke K, Williams JB. Validation and utility of a self-report version of PRIME-MD: the PHQ primary care study. Primary Care Evaluation of Mental Disorders Patient Health Questionnaire. JAMA. 1999;282:1737–44. doi: 10.1001/jama.282.18.1737. [DOI] [PubMed] [Google Scholar]
- 10.Whooley MA, Avins AL, Miranda J, Browner WS. Case-finding instruments for depression. Two questions are as good as many. J Gen Intern Med. 1997;12:439–45. doi: 10.1046/j.1525-1497.1997.00076.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Mittelman MS, Haley WE, Clay OJ, Roth DL. Improving caregiver well-being delays nursing home placement of patients with Alzheimer disease. Neurology. 2006;67:1592–9. doi: 10.1212/01.wnl.0000242727.81172.91. [DOI] [PubMed] [Google Scholar]
- 12.Van Houtven CH, Norton EC. Informal Care and Elderly Health Care Use. Journal of Health Economics. 2004;23:1159–1180. doi: 10.1016/j.jhealeco.2004.04.008. [DOI] [PubMed] [Google Scholar]