Abstract
Purpose
The purpose of this study was to compare the causes and characteristics of reoperations after different primary operations for lumbar disc herniation (LDH).
Methods
Out of a series of 5,280 patients who underwent operations for LDH between 2001 and 2012, 207 patients (135 male and 72 female, mean age 47.7 years) underwent primary and revision operations, which were included in this study. The following clinical parameters were retrospectively assessed: the primary surgical methods, the intervals between primary and revision operations, and surgical findings in the revisions.
Results
In total, 232 lumbar discs underwent reoperations. One hundred and nineteen reoperations were performed after microendoscopic discectomy (MED group), 68 after percutaneous endoscopic lumbar discectomy (PELD group) and 45 after open disc surgery (open group). The locations of revision operations had priority over those of primary surgery, with a moderate correlation (kappa coefficient = 0.533). A total of 46.6 % of reoperations were performed within 0.5 years after primary surgery, and 35.3 % were performed between one and five years. Real recurrent herniation (homolateral herniations at the same level) was significantly more common than other reoperative surgical findings (70.6 % in PELD group, 47.1 % in MED group, 37.8 % in open group). The overall mean interval until revision surgery was 18.9 months (8.1 months in the PELD group vs. 19.7 months in the MED group vs. 33.1 months in the open group, p < 0.01).
Conclusions
For LDH, real recurrent herniation was the most common cause of reoperations, and more reoperations for real recurrent herniations and shorter intervals were found after minimally invasive endoscopic discectomy than after open disc surgery.
Introduction
Lumbar disc herniation (LDH) is the most common disorder of the lumbar spine, and it is occasionally treated surgically. Highly successful results have been obtained with lumbar disc surgery, but 2.8–24 % of patients undergo reoperations after their primary surgery [1–7]. The most common cause of lumbar disc reoperation has been reported to be reherniation [5, 7–9], which includes real recurrent herniation [7] (homolateral herniation at the same level), contralateral herniation at the same disc level and new herniation at another level. The following discectomy-related conditions can also occasionally give rise to revision surgery: scar, adhesive arachnoiditis, infection, epidural haematoma, pseudomeningocele, and other complications [1, 7, 10, 11]. These herniations and conditions in revision surgery are related to primary surgical methods.
Recently, minimally invasive surgery has been widely applied to treat LDH, including microendoscopic discectomy (MED), percutaneous endoscopic lumbar discectomy (PELD), and other similar techniques [12]. Despite improvement in surgical techniques, recurrences and reoperations cannot always be prevented [5, 13]. Some studies have reported differences in reoperation rates after different primary surgical methods [6, 14–18], but to our knowledge, no comparative studies of the causes and characteristics of different surgical methods, especially including MED and PELD, have been published. In our study, we retrospectively investigated 207 patients who had undergone primary lumbar disc surgery and subsequent reoperation. We sought to compare the causes and characteristics of different surgical methods.
Methods
Study population
This study was a retrospective, cross-sectional study using data from the Military Hospital Information Registry Database, gathered from June 2001 to June 2012. All of the medical records were anonymous, and no patient information was extracted except for research purposes. The procedure was approved by the Ethics Committee of The Third Military Medical University. Out of a series of 5,280 patients who were surgically treated for LDH in our department, 207 patients underwent primary and revision operations between June 1, 2001 and June 1, 2012 and were included in this study. The 207 patients’ medical records and imaging studies (X-ray, computed tomography scan, or magnetic resonance imaging) before the primary procedures and reoperations were retrospectively evaluated. The following clinical parameters were assessed: age, sex, history of smoking, alcohol use, concurrent disease, intervals between the primary and revision operations, surgical methods, and level and side of each operation. The imaging studies and reoperative surgical findings were also assessed, including real recurrent herniations, contralateral herniations at the same disc level, new herniations at another level, scar or adhesive arachnoiditis, and other complications, such as cerebrospinal fluid leakage, haematoma, and infection. Based on the reoperative surgical findings, real recurrent herniations in this study indicated that these revision operations were performed at the previously operative site and side [7, 8, 19].
Surgical techniques
Open disc surgery was performed according to the modified Love’s procedure, and the aggressive discectomy described by Cauchoix et al. [20] was performed. The extruded disc material was removed as much as possible, without curetting the endplates. MED was performed as Foley and Smith described [21] using the METRx system (Medtronic Sofamor Danek, Memphis, TN, USA). PELD was performed as Yeung [22] and Hoogland et al. [23] described, using an endoscopic spine system (Joimax GmbH, Karlsruhe, Germany). The limited discectomy described by Spengler [24] was used in MED and PELD surgeries, with only extruded fragments, and any loose pieces in the disc space being removed.
Statistical analysis
Statistical analysis was performed using SPSS software, version 19.0. The chi-square test was used to analyse the frequency data regarding the intervals and surgical findings of reoperations. For values of interval durations, 95 % confidence intervals and independent samples t-tests were performed. Results were considered to be statistically significant if the p-value was less than 0.05. The correlations between surgical levels and sides of the primary and revised operations were represented by kappa coefficients.
Results
In total, 207 patients (135 male and 72 female patients) underwent primary lumbar disc operations and subsequent reoperations. At the primary surgery, open disc surgery was performed in 36 patients, MED in 108 patients, and PELD in 63 patients. The mean age at the time of primary surgery was 47.7 years (range 18–89 years). Nineteen cases (9.2 %) were complicated with hypertension, 12 cases (5.8 %) were complicated with diabetes, 19 cases (9.2 %) had a history of smoking, and seven cases (3.4 %) had a history of high alcohol consumption. No statistically significant differences in age or sex distribution were found among the three groups. Of the primary operations, 185 cases had only one disc excised, 20 cases had two excised, and two cases had three excised. In total, 233 discs were excised in the primary operations.
In overall reoperations, 232 lumbar discs were treated. One hundred and twenty (51.7 %) disc reoperations were performed at the L4/5 level and 100 (43.1 %) at the L5/S1 level. Based on the reoperative surgical findings, 127 (54.7 %) discs were treated for real recurrent herniations, 52 (22.4 %) for new herniations and 30 (12.9 %) for contralateral herniations. The other 23 discs were treated to manage other conditions, including scar or adhesive arachnoiditis (n = 8), infection (n = 7), haematoma (n = 6), and cerebrospinal fluid leakage (n = 2). The relationships of the surgical levels and sides between the primary and revised operations are shown in Table 1. The locations of the revision operations had priority over those of the primary surgery, with a moderate correlation (kappa coefficient = 0.533). The reoperative surgical findings, according to the primary operations and the intervals between the two operations, are shown in Table 2. Among the 232 disc reoperations, 108 (46.6 %) reoperations were performed within 0.5 years after primary surgery and 82 (35.3 %) at one to five years. A total of 90.1 % (209/232) of reoperations were performed for reherniations (including real recurrent herniations, contralateral herniations, and new herniations), and these reoperations were performed during every interval period after primary surgery. Approximately half (49.6 %, 63/127) of the revision operations for real recurrent herniations were performed within 0.5 years after primary surgery. Reoperations for scar or adhesive arachnoiditis were performed, on average, within five years after the primary surgery. Most of the other reoperations for infection, haematoma or cerebrospinal fluid leakage were performed within 0.5 years after primary surgery.
Table 1.
Relationships of surgical levels and sides between primary and revision surgeries
| Primary surgery | Revision surgery | Total | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| L2/3 | L3/4 | L4/5 | L5/S1 | |||||||
| L | R | L | R | L | R | L | R | |||
| L2/3 | L | 0 | ||||||||
| R | 1 | 1 | ||||||||
| L3/4 | L | 1 | 1 | 2 | ||||||
| R | 2 | 1 | 3 | 1 | 7 | |||||
| L4/5 | L | 1 | 1 | 2 | 1 | 39 | 12 | 8 | 7 | 71 |
| R | 3 | 9 | 44 | 3 | 9 | 68 | ||||
| L5/S1 | L | 4 | 39 | 2 | 45 | |||||
| R | 2 | 5 | 7 | 24 | 38 | |||||
| Total | 2 | 1 | 3 | 6 | 56 | 64 | 58 | 42 | 232 | |
Bold type indicates the number of discs treated on the same side of the same level
R right, L left
Table 2.
Reoperative surgical findings according to their primary operations and the intervals between the first and the second operations
| Surgical findings | Open (n = 45) | MED (n = 119) | PELD (n = 68) | Total (n = 232) | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| I | II | III | IV | I | II | III | IV | I | II | III | IV | I | II | III | IV | |
| Real recurrent herniations | 2 | 2 | 11 | 2 | 24 | 8 | 24 | 5 | 37 | 2 | 9 | 1 | 63 | 12 | 44 | 8 |
| New herniations | 1 | 1 | 10 | 2 | 9 | 3 | 10 | 3 | 11 | 2 | 21 | 4 | 22 | 5 | ||
| Contralateral herniations | 5 | 2 | 5 | 5 | 7 | 2 | 2 | 1 | 1 | 7 | 6 | 13 | 4 | |||
| Scar or adhesive arachnoiditis | 1 | 1 | 1 | 2 | 1 | 2 | 3 | 2 | 3 | |||||||
| Infection | 1 | 4 | 2 | 6 | 1 | |||||||||||
| Haematoma | 2 | 4 | 6 | |||||||||||||
| Cerebrospinal fluid leakage | 1 | 1 | 2 | |||||||||||||
| Total | 7 | 5 | 27 | 6 | 49 | 17 | 43 | 10 | 52 | 3 | 12 | 1 | 108 | 25 | 82 | 17 |
Open open disc surgery, MED microendoscopic discectomy, PELD percutaneous endoscopic lumbar discectomy
I, II, III, IV Intervals between the first and the second operations
I <0.5 years; II 0.5–1 year; III 1–5 years, IV 5–9 years
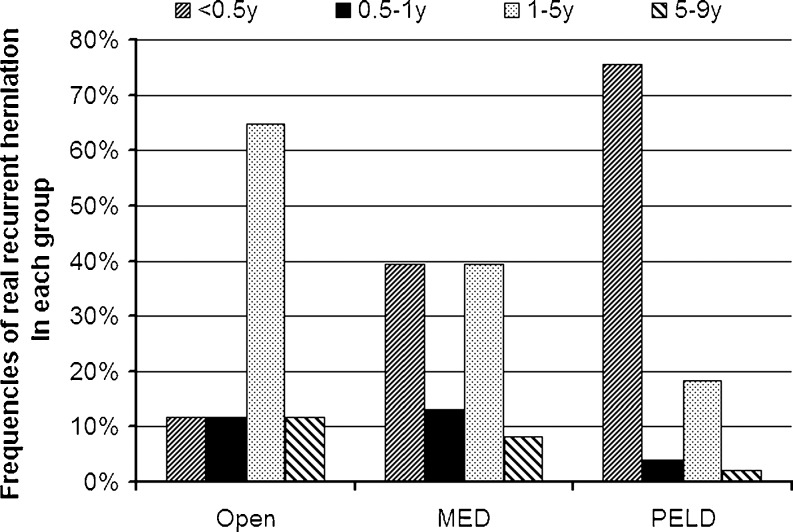
Based on the primary surgical methods of these 232 disc reoperations, 119 reoperations were performed after MED (MED group), 68 were performed after PELD (PELD group), and 45 were performed after open disc surgery (open group). In each group, real recurrent herniation was the most common reoperative surgical finding (p <0.001). More real recurrent herniations occurred in the PELD group than in the MED group (70.6 % vs. 47.1 %, p <0.001) or in the open group (70.6 % vs. 37.8 %, p <0.001). More real recurrent herniations occurred in the MED group than in the open group but with no statistically significant difference (47.1 % vs. 37.8 %, p = 0.123). Thus, real recurrent herniations were more frequently found in reoperations after minimally invasive endoscopic discectomy (the PELD group and MED group) than in reoperations after open disc surgery (55.6 % vs. 37.8 %, p = 0.011). In the PELD group, no reoperations were performed for scar, haematoma or cerebrospinal fluid leakage. Two infections occurred in the PELD group during the early period when we performed the technique. The distributions of reoperative surgical findings across different intervals are shown in Fig. 1.
Fig. 1.
The reoperative surgical findings’ distribution across different intervals. Real recurrent herniation was the most common reoperative surgical finding in almost all of the time intervals. Reoperations for real recurrent herniations accounted for almost one third of reoperations in the open group, half in the MED and two thirds in the PELD group across each interval. Most of “others” were found within one year after primary operations. Other reoperative surgical findings, included scar or adhesive arachnoiditis, infection, haematoma, and cerebrospinal fluid leakage
The overall mean interval until revision surgery was 18.9 months (range, three days to 8.3 years) (Table 3). The mean intervals in the three groups met the following order: PELD < MED < open (8.1 months vs. 19.7 months vs. 33.1 months, p < 0.01). The mean interval until reoperation after minimally invasive endoscopic discectomy was shorter than that after open disc surgery (15.5 months vs. 33.1 months, p = 0.022). For each type of reherniation, the mean interval in the PELD group was always significantly shorter than that in the MED group and open group (p < 0.05). For real recurrent herniations and new herniations, the mean interval in the MED group was shorter than that in the open group but with no statistical significance (p > 0.05). For contralateral herniations, the mean interval in the MED group was significantly shorter than that in the open group (p = 0.031).
Table 3.
The interval durations (months) between the first and second operations
| Surgical findings | Open | MED | PELD | Total |
|---|---|---|---|---|
| Real recurrent herniations | 35.8 ± 25.6 | 21.1 ± 23.2 | 8.6 ± 17.3*# | 18.3 ± 23.3 |
| New herniations | 34.0 ± 22.7 | 21.8 ± 24.2 | 7.3 ± 15.1*# | 21.5 ± 23.6 |
| Contralateral herniations | 51.0 ± 24.4# | 24.4 ± 22.4 | 7.7 ± 5.7*# | 28.4 ± 25.1 |
| Other surgical findings | 7.0 ± 9.5 | 3.6 ± 5.7 | 1.7 ± 0.1 | 4.4 ± 6.9 |
| Total | 33.1 ± 25.8# | 19.7 ± 22.6 | 8.1 ± 16.1*# | 18.9 ± 23.2 |
Open open disc surgery, MED microendoscopic discectomy, PELD percutaneous endoscopic lumbar discectomy
*: p < 0.05, compared with the open group; #: p < 0.05, compare with the MED group
For overall reoperations, the distributions across different intervals are shown in Fig. 2. In the three groups, the percentages of reoperations within 0.5 years met the following order: PELD > MED > open (76.5 % vs. 41.2 % vs. 15.6 %, p < 0.01); the percentage of reoperations occurring at 1–5 years met the following order: open > MED > PELD (60.0 % vs. 36.1 % vs. 17.6 %, p < 0.01). For 127 real recurrent herniations, the distributions across different intervals are shown in Fig. 3. The distributions were similar to those for overall reoperations.
Fig. 2.
The time interval distribution in different primary operation groups. Different reoperation peaks occurred in different groups. In the open group, 60 % of reoperations were performed in the one- to five-year period. In the microendoscopic discectomy (MED) group, more reoperations were performed in the 0–0.5 year and one- to five-year periods than during other intervals. In the percutaneous endoscopic lumbar discectomy (PELD) group, 76.5 % of reoperations were performed within 0.5 years after primary surgery
Fig. 3.
The time interval distribution of real recurrent herniations in different primary operation groups. Different reoperation peaks occurred in different groups. In the open group, 64.7 % of reoperations were performed in the one- to five-year period. In the microendoscopic discectomy (MED) group, more reoperations were performed in the 0–0.5 year and one- to five-year periods than during other interval times. In the percutaneous endoscopic lumbar discectomy (PELD) group, 75.5 % of reoperations were performed within 0.5 years after primary surgery
Discussion
Lumbar discectomy is the most common surgical procedure performed for patients who are experiencing back and leg pain [25]. Despite the development of new surgical techniques and the reporting of successful outcomes in lumbar disc surgery, more than 10 % of patients develop long-term recurrent pain, which has been associated with substantial health care costs [26]. Reoperations are usually necessary, and the reoperation rate has been reported to range from 2.8 % to 24 % [1–7, 27, 28], depending on the type of primary surgical procedure. Osterman et al. [14] found that patients with one reoperation had a 25.1 % risk of further spinal surgery over the next ten years. Unfortunately, the precise mechanism of reoperation is still unclear [29]. The causes and characteristics of reoperations after different primary surgery were not specified in the population-based data. In this study, 207 patients underwent reoperations for LDH and were retrospectively reviewed. The reoperations were compared among three different primary surgery groups with the same age and sex distributions. Similar to the findings of many other researchers [7, 13, 30, 31], we found that reoperations were most frequently performed at the L4/5 level and next at the L5/S1 level, with 64.2 % of disc reoperations occurring in the same location as the primary surgery.
In previous studies, more than half of lumbar disc reoperations occurred within one year after primary surgery [1, 5, 6, 10]. Recently, Kim et al. [6] reported on a nationwide cohort study of the reoperation rate after surgery for LDH. In their research, 46.0 % (1,187/2,578) of reoperations were performed within 0.5 years after primary surgery. Our results were similar, with 46.6 % of reoperations performed within 0.5 years. Little research has taken note of the differences in intervals of reoperations after different primary procedures. Kim et al. [13] researched 42 patients who underwent reoperations after PELD, and they reported that the mean symptom-free interval was 2.5 months (range, 0.5–27 months). In the research of Matsumoto et al. [5] on 37 recurrences after MED, the mean time interval between MED and recurrence was 16.6 months (range, 0.5–52 months), with 54.1 % (22/37) developing recurrence within one year after MED. In our study, the mean intervals until reoperation were 8.1 months after PELD and 19.7 months after MED. We found shorter intervals after minimally invasive endoscopic discectomy than after open disc surgery, but more research on clinical outcomes after primary surgery are needed to explain this outcome.
In this study, real recurrent herniation was the most common cause for lumbar disc reoperations. In the previous studies, the percentage of real recurrent herniation after lumbar disc reoperations was reported to be 40.9–75 % [4, 7, 10, 11]. In our study, 54.7 % (127/232) of reoperations were performed for real recurrent herniation, which was significantly more than other reoperative surgical findings in the three groups (p <0.001). In particular, more real recurrent herniation was found after minimally invasive endoscopic discectomy than after open disc surgery. We believe this finding has two causes. First, this condition could have been related to the primary surgical method. In open discectomy, it is convenient to make a thorough decompression and remove the hidden fragments under a wide view, while MED and PELD are performed under the endoscope with a bidimensional vision. Relatively less decompression is performed because the endoscope tube limits the scope of decompression instruments. Furthermore, it is difficult to remove hidden free fragments which are located beyond the endoscopic channel [5, 13, 32]. The residual or hidden fragments can lead to a higher incidence of recurrences, especially in the early period after primary discectomy. For the above reasons, Teli et al. [32] found that recurrent herniations were significantly more common after MED than after micro or open discectomy. The recurrence rate after limited discectomy was reported to be higher than that after aggressive discectomy [16]. With the limited discectomy, more real recurrent herniations occurred after minimally invasive endoscopic discectomy than after open disc surgery in our study. Second, this condition was correlated with the definition of real recurrent herniation in our study. By strict definition, patients with recurrent herniation always have a pain-free interval of at least six months between the primary surgery and the recurrence of symptoms [19]. However, no strict time interval has been required in the literature for the diagnosis of recurrent disc herniation [5, 7]. The more appropriate clinical definition is disc herniation at the previously operative site and side [7, 8, 19]. Based on this definition, homolateral herniations at the same level were designated as real recurrent herniations in this study, regardless of the time interval between the first and second operations. Within 0.5 years after primary surgery, the percentages of reoperations performed at the previously treated site and side were 75.5 % in the PELD group, 39.3 % in the MED group, and only 11.8 % in the open group. In our study, these reoperations were considered to be real recurrent herniations, which might have increased the percentage of real recurrent herniations after minimally invasive endoscopic discectomy. It should also be considered that many real recurrent herniations occurred within 0.5 years in the PELD group. A total of 35.1 % (13/37) of these reoperations were performed without a pain-free interval of at least one week. The authors believe that these primary PELD operations did not excise sufficient material, and residual nucleus pulposus caused reoperations within a short period of time. We suggest that the rate of reoperations could be reduced during the early period with excision of more herniation during primary PELD treatment. As Yong [33] reported, the key to success in transforaminal PELD was complete herniotomy after thorough release of the annular anchorage.
In our study, the reoperation peaks and reoperation findings were different according to different primary procedures. These results could help surgeons make diagnoses when persistent pain or recurrence of symptoms occurs. Within 0.5 years after PELD, real recurrent herniation should be considered first when low back pain recurs. At 0.5 years after open disc surgery, scar and haematoma should not be ignored. These results should also be helpful with regard to setting follow-up schedules. Follow-up should occur more frequently within 0.5 years after PELD and MED. Furthermore, more visits or telephone calls can be made in the one- to five-year period after open disc surgery. One limitation of this study was the small number of reoperations after open disc surgery. As a large minimally invasive treatment centre for lumbar degenerative disease, more patients in this study underwent minimally invasive discectomy. Thus, the information for comparison should be considered with caution. However, as a retrospective study on 5,280 patients over 11 years, the comparisons of reoperations for LDH could provide some suggestions. We encourage large-sample prospective studies with long-term follow-up.
Conclusions
Most reoperations after lumbar disc discectomy presented during the 0–0.5 year and one- to five-year periods after primary surgery. The mean intervals in the three groups met the following order: PELD < MED < open (p < 0.01). For LDH, real recurrent herniation was the most common cause of reoperations, with more reoperations for real recurrent herniations and shorter intervals found after minimally invasive endoscopic discectomy than after open disc surgery.
Acknowledgments
This work was supported by the Key Project of Chinese Ministry of Health (no. 201002018) and the Foundation of the State Key Laboratory of Robotics (no. 2011-O01).
Conflict of interest
The authors declare that they have no conflict of interest.
Contributor Information
Hongwei Wang, Phone: +86-23-68755608, FAX: +86-23-68755608, Email: cplawhw@163.com.
Yue Zhou, Phone: +86-23-68755608, FAX: +86-23-68755608, Email: happyzhou@vip.163.com.
References
- 1.Fandino J, Botana C, Viladrich A, Gomez-Bueno J. Reoperation after lumbar disc surgery: results in 130 cases. Acta Neurochir (Wien) 1993;122(1–2):102–104. doi: 10.1007/BF01446994. [DOI] [PubMed] [Google Scholar]
- 2.Suk KS, Lee HM, Moon SH, Kim NH. Recurrent lumbar disc herniation: results of operative management. Spine (Phila Pa 1976) 2001;26(6):672–676. doi: 10.1097/00007632-200103150-00024. [DOI] [PubMed] [Google Scholar]
- 3.Atlas SJ, Keller RB, Chang Y, Deyo RA, Singer DE. Surgical and nonsurgical management of sciatica secondary to a lumbar disc herniation: five-year outcomes from the Maine Lumbar Spine Study. Spine (Phila Pa 1976) 2001;26(10):1179–1187. doi: 10.1097/00007632-200105150-00017. [DOI] [PubMed] [Google Scholar]
- 4.Hakkinen A, Kiviranta I, Neva MH, Kautiainen H, Ylinen J. Reoperations after first lumbar disc herniation surgery; a special interest on residives during a 5-year follow-up. BMC Musculoskelet Disord. 2007;9(8):2. doi: 10.1186/1471-2474-8-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Matsumoto M, Watanabe K, Hosogane N, Tsuji T, Ishii K, Nakamura M, Chiba K, Toyama Y. Recurrence of lumbar disc herniation after microendoscopic discectomy. J Neurol Surg A Cent Eur Neurosurg. 2012 doi: 10.1055/s-0032-1320031. [DOI] [PubMed] [Google Scholar]
- 6.Kim CH, Chung CK, Park CS, Choi B, Kim MJ, Park BJ. Reoperation rate after surgery for lumbar herniated intervertebral disc disease: nation-wide cohort study. Spine (Phila Pa 1976) 2013;38(7):581–590. doi: 10.1097/BRS.0b013e318274f9a7. [DOI] [PubMed] [Google Scholar]
- 7.Aizawa T, Ozawa H, Kusakabe T, Nakamura T, Sekiguchi A, Takahashi A, Sasaji T, Tokunaga S, Chiba T, Morozumi N, Koizumi Y, Itoi E. Reoperation for recurrent lumbar disc herniation: a study over a 20-year period in a Japanese population. J Orthop Sci. 2012;17(2):107–113. doi: 10.1007/s00776-011-0184-6. [DOI] [PubMed] [Google Scholar]
- 8.Lee JK, Amorosa L, Cho SK, Weidenbaum M, Kim Y. Recurrent lumbar disk herniation. J Am Acad Orthop Surg. 2010;18(6):327–337. doi: 10.5435/00124635-201006000-00005. [DOI] [PubMed] [Google Scholar]
- 9.Chen Z, Zhao J, Liu A, Yuan J, Li Z. Surgical treatment of recurrent lumbar disc herniation by transforaminal lumbar interbody fusion. Int Orthop. 2009;33(1):197–201. doi: 10.1007/s00264-008-0531-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Kayaoglu CR, Calikoglu C, Binler S. Re-operation after lumbar disc surgery: results in 85 cases. J Int Med Res. 2003;31(4):318–323. doi: 10.1177/147323000303100410. [DOI] [PubMed] [Google Scholar]
- 11.Erbayraktar S, Acar F, Tekinsoy B, Acar U, Guner EM. Outcome analysis of reoperations after lumbar discectomies: a report of 22 patients. Kobe J Med Sci. 2002;48(1–2):33–41. [PubMed] [Google Scholar]
- 12.Zhu H, Zhou XZ, Cheng MH, Shen YX, Dong QR. The efficacy of coblation nucleoplasty for protrusion of lumbar intervertebral disc at a two-year follow-up. Int Orthop. 2011;35(11):1677–1682. doi: 10.1007/s00264-010-1196-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kim JM, Lee SH, Ahn Y, Yoon DH, Lee CD, Lim ST. Recurrence after successful percutaneous endoscopic lumbar discectomy. Minim Invasive Neurosurg. 2007;50(2):82–85. doi: 10.1055/s-2007-982504. [DOI] [PubMed] [Google Scholar]
- 14.Osterman H, Sund R, Seitsalo S, Keskimaki I. Risk of multiple reoperations after lumbar discectomy: a population-based study. Spine (Phila Pa 1976) 2003;28(6):621–627. doi: 10.1097/01.BRS.0000049908.15854.ED. [DOI] [PubMed] [Google Scholar]
- 15.Ruetten S, Komp M, Merk H, Godolias G. Full-endoscopic interlaminar and transforaminal lumbar discectomy versus conventional microsurgical technique: a prospective, randomized, controlled study. Spine (Phila Pa 1976) 2008;33(9):931–939. doi: 10.1097/BRS.0b013e31816c8af7. [DOI] [PubMed] [Google Scholar]
- 16.McGirt MJ, Ambrossi GL, Datoo G, Sciubba DM, Witham TF, Wolinsky JP, Gokaslan ZL, Bydon A. Recurrent disc herniation and long-term back pain after primary lumbar discectomy: review of outcomes reported for limited versus aggressive disc removal. Neurosurgery. 2009;64(2):338–344. doi: 10.1227/01.NEU.0000337574.58662.E2. [DOI] [PubMed] [Google Scholar]
- 17.Malter AD, McNeney B, Loeser JD, Deyo RA. 5-year reoperation rates after different types of lumbar spine surgery. Spine (Phila Pa 1976) 1998;23(7):814–820. doi: 10.1097/00007632-199804010-00015. [DOI] [PubMed] [Google Scholar]
- 18.Keskimaki I, Seitsalo S, Osterman H, Rissanen P. Reoperations after lumbar disc surgery: a population-based study of regional and interspecialty variations. Spine (Phila Pa 1976) 2000;25(12):1500–1508. doi: 10.1097/00007632-200006150-00008. [DOI] [PubMed] [Google Scholar]
- 19.Swartz KR, Trost GR. Recurrent lumbar disc herniation. Neurosurg Focus. 2003;15(3):E10. doi: 10.3171/foc.2003.15.3.10. [DOI] [PubMed] [Google Scholar]
- 20.Cauchoix J, Ficat C, Girard B. Repeat surgery after disc excision. Spine (Phila Pa 1976) 1978;3(3):256–259. doi: 10.1097/00007632-197809000-00011. [DOI] [PubMed] [Google Scholar]
- 21.Foley KT, Smith MM. Microendoscopic discectomy. Tech Neurosurg. 1997;7(5):301–307. [Google Scholar]
- 22.Yeung AT, Tsou PM. Posterolateral endoscopic excision for lumbar disc herniation: surgical technique, outcome, and complications in 307 consecutive cases. Spine (Phila Pa 1976) 2002;27(7):722–731. doi: 10.1097/00007632-200204010-00009. [DOI] [PubMed] [Google Scholar]
- 23.Hoogland T, Schubert M, Miklitz B, Ramirez A. Transforaminal posterolateral endoscopic discectomy with or without the combination of a low-dose chymopapain: a prospective randomized study in 280 consecutive cases. Spine (Phila Pa 1976) 2006;31(24):E890–E897. doi: 10.1097/01.brs.0000245955.22358.3a. [DOI] [PubMed] [Google Scholar]
- 24.Spengler DM. Lumbar discectomy. Results with limited disc excision and selective foraminotomy. Spine (Phila Pa 1976) 1982;7(6):604–607. doi: 10.1097/00007632-198211000-00015. [DOI] [PubMed] [Google Scholar]
- 25.Deyo RA, Weinstein JN. Low back pain. N Engl J Med. 2001;344(5):363–370. doi: 10.1056/NEJM200102013440508. [DOI] [PubMed] [Google Scholar]
- 26.Ambrossi GL, McGirt MJ, Sciubba DM, Witham TF, Wolinsky JP, Gokaslan ZL, Long DM. Recurrent lumbar disc herniation after single-level lumbar discectomy: incidence and health care cost analysis. Neurosurgery. 2009;65(3):574–578. doi: 10.1227/01.NEU.0000350224.36213.F9. [DOI] [PubMed] [Google Scholar]
- 27.O’Sullivan MG, Connolly AE, Buckley TF. Recurrent lumbar disc protrusion. Br J Neurosurg. 1990;4(4):319–325. doi: 10.3109/02688699008992741. [DOI] [PubMed] [Google Scholar]
- 28.Cinotti G, Roysam GS, Eisenstein SM, Postacchini F. Ipsilateral recurrent lumbar disc herniation. A prospective, controlled study. J Bone Joint Surg Br. 1998;80(5):825–832. doi: 10.1302/0301-620X.80B5.8540. [DOI] [PubMed] [Google Scholar]
- 29.Wera GD, Marcus RE, Ghanayem AJ, Bohlman HH. Failure within one year following subtotal lumbar discectomy. J Bone Joint Surg Am. 2008;90(1):10–15. doi: 10.2106/JBJS.F.01569. [DOI] [PubMed] [Google Scholar]
- 30.Dai LY, Zhou Q, Yao WF, Shen L. Recurrent lumbar disc herniation after discectomy: outcome of repeat discectomy. Surg Neurol. 2005;64(3):226–231. doi: 10.1016/j.surneu.2004.11.003. [DOI] [PubMed] [Google Scholar]
- 31.Papadopoulos EC, Girardi FP, Sandhu HS, Sama AA, Parvataneni HK, O’Leary PF, Cammisa FJ. Outcome of revision discectomies following recurrent lumbar disc herniation. Spine (Phila Pa 1976) 2006;31(13):1473–1476. doi: 10.1097/01.brs.0000219872.43318.7a. [DOI] [PubMed] [Google Scholar]
- 32.Teli M, Lovi A, Brayda-Bruno M, Zagra A, Corriero A, Giudici F, Minoia L. Higher risk of dural tears and recurrent herniation with lumbar micro-endoscopic discectomy. Eur Spine J. 2010;19(3):443–450. doi: 10.1007/s00586-010-1290-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Ahn Y. Transforaminal percutaneous endoscopic lumbar discectomy: technical tips to prevent complications. Expert Rev Med Devices. 2012;9(4):361–366. doi: 10.1586/erd.12.23. [DOI] [PubMed] [Google Scholar]