Abstract
Purpose
The purpose of this study was to assess the effects of operative and non-operative treatment on clavicle fractures.
Method
Relevant clinical trials on the operative and non-operative treatment for clavicle fractures were retrieved through searching the databases MEDLINE, Embase, OVID and the Cochrane Central Register of Controlled Trials up to December 2011. The quality of the included studies was assessed by two authors. A meta-analysis was carried out on homogeneous studies. Five studies involving 633 clavicle fractures were included.
Results
The differences in nonunion [risk ratio (RR) 0.12, 95 % confidence interval (CI) 0.05–0.29], malunion (RR 0.11, 95 % CI 0.04–0.29) and neurological complications (RR 0.45, 95 % CI 0.25–0.81) were statistically significant between operative and non-operative treatment. There was no statistically significant difference in delayed union (RR 0.78, 95 % CI 0.31–1.95).
Conclusion
Operative treatment is better than non-operative treatment, but decisions should be made in accordance with specific conditions for clinical application.
Introduction
Clavicle fractures are frequent injuries, representing 2.6–10 % of fractures in adults [1, 2], of which midshaft fractures are the most common, accounting for approximately 81 % of all clavicle fractures [2]. Traditionally, clavicular fracture is treated non-operatively with a figure-of-eight bandage or broad arm sling [3]. Non-operative treatment is easily accepted by undemanding patients and patients who do not tolerate surgery well as it offers the advantages of minimal trauma, easy procedure and low cost. However, outcomes of non-operative treatment are not always excellent [4, 5]. Some specific subsets of patients are reported to be at a high risk for nonunion, shoulder dysfunction or residual pain after non-surgical management [6]. Therefore, operative treatment is playing an increasingly important role in the clinical setting, mainly using compression plating or intramedullary nail fixation [7–10].
A number of studies have assessed the effectiveness of operative versus non-operative treatment for clavicle fractures in different populations; however, the results are inconsistent and inconclusive because of the small sample size in most of the studies [11–13]. Meta-analysis was first proposed by Beecher in 1955 and named by Glass in 1976. It is defined as a statistical method for systematically combining the results of multiple independent studies (controversial or even conflicting studies) and analysing a large data set to allow definite conclusions, offering great help for scientific research and practice decisions [14]. Therefore, this report retrieved randomised controlled trials or clinical controlled trials of operative and non-operative treatment for clavicle fracture over nearly 20 years and meta-analysis was performed to provide a basis for the preferred therapies for clavicle fracture in clinical practice.
Materials and methods
Literature search
The databases PubMed, MEDLINE, EMBASE and the Cochrane Central Register of Controlled Trials (CCTR) were searched for all articles on operative and non-operative treatment for clavicle fracture with the following search terms: (clavicle) AND (fractures) AND (‘randomised controlled trial’ OR ‘controlled clinical trial’) where the search date was December 2011. We also retrieved the relevant articles with Google Scholar.
Inclusion and exclusion criteria
Abstracts of all citations and retrieved studies were reviewed. Studies meeting the following criteria were included: (1) original literature published at home and abroad; (2) randomised clinical trial (RCT) or controlled clinical trial (CCT) design; (3) having definite study time; (4) having definite sample size; (5) providing definite pathological diagnostic criteria; (6) the therapeutic methods are operative treatment (plating or intramedullary nailing) and non-operative treatment (arm sling or bandage); (7) the method of data collection is scientific and correct; and (8) comparison of Constant score (CS) scores, disabilities of the arm, shoulder and hand (DASH) scores, nonunion, delayed union or neurological complications.
Studies were excluded if one of the following existed: (1) providing undefined sample and control source, non-therapeutic clinical studies, animal experiments, non-original studies and undefined grouping; (2) providing undefined pathological diagnostic criteria; (3) patients without clavicle fracture due to trauma; (4) no control design; (5) the method of data collection is not scientific and the method of data analysis is incorrect or not provided; (6) no therapeutic outcome; and (7) review literature, repeated reports and retrospective studies.
Data extraction
All data were extracted independently by two authors according to the inclusion criteria listed above. Disagreements were resolved by discussion between the two reviewers. The following characteristics were collected from each study: the first author, year of publication, source, experiment design, sample size, sample characteristics, treatment outcome and others.
Statistical analysis
The statistical analysis was conducted using Review Manager 5.0 software. Continuous data were expressed as standardised mean differences (SMD) and 95 % confidence intervals (CI). Dichotomous data were presented as risk ratios (RR) with 95 % CI. P ≤ 0.05 was considered statistically significant. Heterogeneity was assessed with the χ2-based Q testing. If there was significant heterogeneity (P < 0.1), we selected a random effects model to pool the data. If not, a fixed effects model was used.
Results
Literature characteristics
A total of 37 studies related to the effects of operative and non-operative treatment of clavicle fracture and the complications were retrieved after the preliminary screening; eight of the 37 studies were incorporated into the study [15–22]. The basic characteristics of these studies such as the authors, publication year, journal, study type, the number of patients, therapeutic method and follow-up time are summarised in Table 1. There were five RCT [16, 18, 20–22] and three CCT [15, 17, 19]. The number of patients ranged from 53 to 132 (Table 1).
Table 1.
Basic situation and quality assessment of the studies
| Literature | Journal | Type | Patients (n) | Follow-up (n) | Follow-up time | Operative group | Non-operative group |
|---|---|---|---|---|---|---|---|
| Böhme (2011) [15] | Z Orthop Unfall | CCT | 120 | 96 | 8 months | Plating/elastic intramedullary nail | Bandage fixation |
| COTS (2007) [16] | J Bone Joint Surg | RCT | 132 | 111 | 1 year | Plating | Arm sling |
| Jubel (2005) [17] | Unfallchirurg | CCT | 53 | 53 | 6 months | Elastic intramedullary nail | Bandage fixation |
| Judd (2009) [18] | Am J Orthop | RCT | 57 | 50 | 1 year | Elastic intramedullary nail | Arm sling |
| Kulshrestha (2011) [19] | J Orthop Trauma | CCT | 73 | 68 | 18 months | Plating | Arm sling |
| Smekal (2009) [20] | J Orthop Trauma | RCT | 68 | 60 | 2 years | Elastic intramedullary nail | Arm sling |
| Smith (2001) [21] | 68th AM of AAOS | RCT | 100 | 65 | 18.5 months | Plating | Arm sling |
| Virtanen (2010) [22] | 75th AM of AAOS | RCT | 60 | 51 | 1 year | Plating | Arm sling |
COTS Canadian Orthopaedic Trauma Society, AM of AAOS Annual Meeting of the American Academy of Orthopaedic Surgeons
Comparison of the CS and DASH scores between operative and non-operative treatment for clavicle fracture
Five studies [15–17, 20, 22] reported the CS scores after the treatment of clavicle fracture and the results showed that the CS scores of the operative group were higher than those of the non-operative group. Four studies [16, 17, 20, 22] reported the DASH scores and the DASH scores of the operative group were shown to be lower than those of the non-operative group. We did not compare the statistical difference due to a lack of information on standard deviation.. The definite scores are shown in Table 2.
Table 2.
CS and DASH scores
| Literature | CS scores | DASH scores | ||
|---|---|---|---|---|
| Operative group | Non-operative group | Operative group | Non-operative group | |
| Böhme (2011) [15] | 94 | 90 | NA | NA |
| COTS (2007) [16] | 96.1 | 90.8 | 5.2 | 13 |
| Jubel (2005) [17] | 98 | 90 | 2 | 10 |
| Judd (2009) [18] | NA | NA | NA | NA |
| Kulshrestha (2011) [19] | NA | NA | NA | NA |
| Smekal (2009) [20] | 97.9 | 93.7 | 0.5 | 3 |
| Smith (2001) [21] | NA | NA | NA | NA |
| Virtanen (2010) [22] | 86.5 | 86.1 | 4.3 | 7.1 |
COTS Canadian Orthopaedic Trauma Society
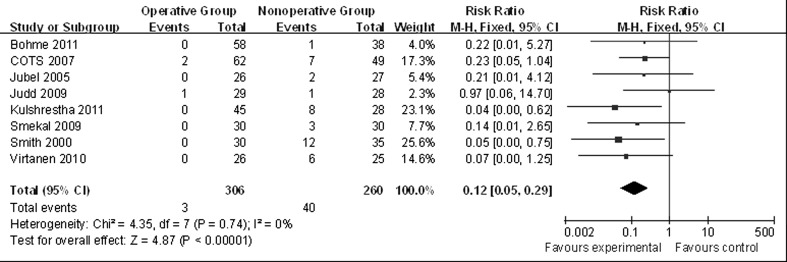
Comparison of the nonunion rate between operative and non-operative treatment for clavicle fracture
Eight RCT or CCT [15–22] reported the nonunion rate after operative and non-operative treatment of clavicle fracture in which 306 patients were included in the operative treatment group and 260 patients were included in the non-operative treatment group. No heterogeneity was observed between the studies (P = 0.74, I2 = 0 %); therefore, a fixed effect model was used. The result of meta-analysis showed that there was a statistical difference in the nonunion rate between operative and non-operative treatment for clavicle fracture (RR 0.12, 95 % CI 0.05–0.29). Operative treatment could significantly reduce the nonunion rate (Fig. 1).
Fig. 1.
Comparison of the nonunion rate after operative and non-operative treatment for clavicle fracture
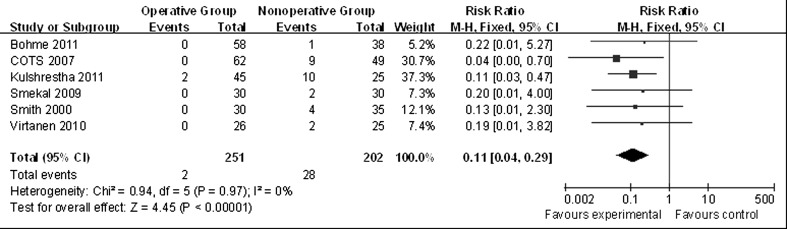
Comparison of the malunion rate between operative and non-operative treatment for clavicle fracture
Six RCT or CCT [15, 16, 19–22] reported the malunion rate after operative and non-operative treatment for clavicle fracture in which 251 patients were included in the operative treatment group and 202 patients were included in the non-operative treatment group. Heterogeneity was also not observed between the studies (P = 0.97, I2 = 0 %). The result of meta-analysis showed there was a significant difference in malunion rate between operative and non-operative treatment for clavicle fracture (RR 0.11, 95 % CI 0.04–0.29), indicating operative treatment reduces the malunion rate (Fig. 2).
Fig. 2.
Comparison of the malunion rate after operative and non-operative treatment for clavicle fracture
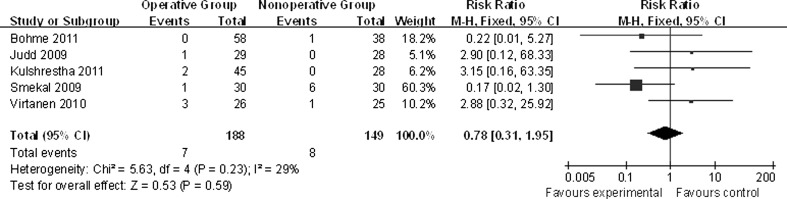
Comparison of the delayed union rate between operative and non-operative treatment for clavicle fracture
There were five RCT or CCT [15, 18–20, 22] which had been performed to study the delayed union rate after operative and non-operative treatment of clavicle fracture. A total of 337 patients were studied, including 188 patients receiving operative treatment and 149 patients receiving non-operative treatment. No heterogeneity was present between the studies (P = 0.23, I2 = 29 %). The result of meta-analysis showed that there was no statistical difference in the delayed union rate between operative and non-operative treatment for clavicle fracture (RR 0.78, 95 % CI 0.31–1.95), indicating operative treatment did not reduce the delayed union rate (Fig. 3).
Fig. 3.
Comparison of the delayed union rate after operative and non-operative treatment for clavicle fracture
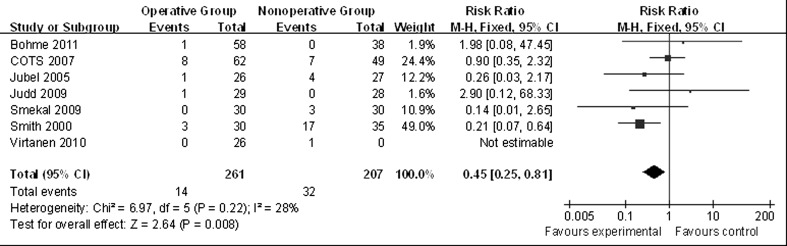
Comparison of the neurological complication rate
There were seven RCT or CCT [15–18, 20–22] which had been performed to study the neurological complication rate after operative and non-operative treatment for clavicle fracture. A total of 468 patients were studied, including 261 patients receiving operative treatment and 207 patients receiving non-operative treatment. No heterogeneity was present between the studies (P = 0.23, I2 = 28 %). The result of meta-analysis showed there was also no statistical difference in the neurological complication rate between operative and non-operative treatment of clavicle fracture (RR 0.45, 95 % CI 0.25–0.80) (Fig. 4).
Fig. 4.
Comparison of the neurological complication rate after operative and non-operative treatment for clavicle fracture
Discussion
Some systematic reviews on clavicle fracture treatment have been reported in previous studies. For example, Zlowodzki et al. [23] showed that the nonunion rate can reach 4 % by operative treatment and 6 % by non-operative treatment. However, this study only included three RCT containing a cohort study due to the limitation of methodology. Only one of the three RCT studied the effect of different operations on clavicle fracture. Lenza et al. [24] investigated three reports of non-operative treatment of middle third clavicle fractures, but the three reports could not analyse the effect of different operations on clavicle fracture. This meta-analysis included five RCT and three CCT published between 2000 and 2011. This meta-analysis analysed the nonunion, malunion, delayed union and neurological complication rate after operative and non-operative treatment for clavicle fracture. The results showed that there were statistical differences in the nonunion, malunion and neurological complication rates between operative and non-operative treatment, suggesting operative treatment could decrease the incidence rate of these adverse events. Operative treatment did not reduce the delayed union rate in our study.
These meta-analysis results should be cautiously interpreted because there are still some limitations to this study. (1) Although this meta-analysis was performed based on unbiased data, the bias must exist because of the differences in the concerned populations and regions in the studies. By collecting all papers about clavicle fracture using multiple languages, we believe that the results of the study are suitable for almost all populations. (2) Since the deficiency of the original data such as CS scores and the standard deviation of DASH scores, the CS scores and DASH scores only could be described. A statistical analysis could not be performed. (3) We did not analyse the effect of treatments on clavicle fracture according to different ages and sexes on account of the limitation of the studies included, which may affect the result of this meta-analysis. (4) Our study may also be influenced by the lack of final effect of the treatments on patients because of the delayed follow-up, the loss to follow-up and the increasing number of patients who dropped out of the studies. (5) Meta-analysis is a retrospective research tool that is subject to methodological deficiencies. Therefore, larger and well-designed studies are needed to confirm our results.
Conclusions
Operative treatment reduces the nonunion, malunion and neurological complication rates of clavicle fractures, but does not affect the delayed union rate. For clinical application, we should make decisions in accordance with specific conditions. In order to avoid the risk of adverse events, operative treatment is a better therapeutic method if it is matched to the individual patient.
Acknowledgments
This study was supported by National Natural Science Foundation of China (No. 81200964 and No. 31171069); Military Twelfth Five Key Projects (No.BWS11J038); Foundation of State Key Laboratory of Trauma, Burns and Combined Injuries (No.SKLKF201113)
Conflict of interest
The authors declare that they have no conflict of interest.
Footnotes
Guo-dong Liu and Song-lin Tong contributed equally to the study.
Contributor Information
Shan Ou, Phone: +86-13983051093, FAX: +86-23-68818654, Email: euromountainou@hotmail.com.
Jian-wen Gu, Email: 769419161@qq.com.
References
- 1.Robinson C. Fractures of the clavicle in the adult. Epidemiology and classification. J Bone Joint Surg Br. 1998;80(3):476–484. doi: 10.1302/0301-620X.80B3.8079. [DOI] [PubMed] [Google Scholar]
- 2.Postacchini F, Gumina S, De Santis P, Albo F. Epidemiology of clavicle fractures. J Shoulder Elbow Surg. 2002;11(5):452–456. doi: 10.1067/mse.2002.126613. [DOI] [PubMed] [Google Scholar]
- 3.Postacchini R, Gumina S, Farsetti P, Postacchini F. Long-term results of conservative management of midshaft clavicle fracture. Int Orthop. 2010;34(5):731–736. doi: 10.1007/s00264-009-0850-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Nowak J, Holgersson M, Larsson S. Can we predict long-term sequelae after fractures of the clavicle based on initial findings? A prospective study with nine to ten years of follow-up. J Shoulder Elbow Surg. 2004;13(5):479–486. doi: 10.1016/j.jse.2004.01.026. [DOI] [PubMed] [Google Scholar]
- 5.Robinson CM, Court-Brown CM, McQueen MM, Wakefield AE. Estimating the risk of nonunion following nonoperative treatment of a clavicular fracture. J Bone Joint Surg Am. 2004;86(7):1359–1365. doi: 10.2106/00004623-200407000-00002. [DOI] [PubMed] [Google Scholar]
- 6.van der Meijden OA, Gaskill TR, Millett PJ. Treatment of clavicle fractures: current concepts review. J Shoulder Elbow Surg. 2011;21(3):423–429. doi: 10.1016/j.jse.2011.08.053. [DOI] [PubMed] [Google Scholar]
- 7.McKee M, Seiler J, Jupiter J. The application of the limited contact dynamic compression plate in the upper extremity: an analysis of 114 consecutive cases. Injury. 1995;26(10):661–666. doi: 10.1016/0020-1383(95)00148-4. [DOI] [PubMed] [Google Scholar]
- 8.Poigenfürst J, Rappold G, Fischer W. Plating of fresh clavicular fractures: results of 122 operations. Injury. 1992;23(4):237–241. doi: 10.1016/S0020-1383(05)80006-3. [DOI] [PubMed] [Google Scholar]
- 9.Mueller M, Burger C, Florczyk A, Striepens N, Rangger C. Elastic stable intramedullary nailing of midclavicular fractures in adults: 32 patients followed for 1–5 years. Acta Orthop. 2007;78(3):421–423. doi: 10.1080/17453670710014013. [DOI] [PubMed] [Google Scholar]
- 10.Eden L, Doht S, Frey SP, Ziegler D, Stoyhe J, Fehske K, Blunk T, Meffert RH. Biomechanical comparison of the Locking Compression superior anterior clavicle plate with seven and ten hole reconstruction plates in midshaft clavicle fracture stabilisation. Int Orthop. 2012;36(12):2537–2543. doi: 10.1007/s00264-012-1671-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rokito AS, Zuckerman JD, Shaari JM, Eisenberg DP, Cuomo F, Gallagher MA. A comparison of nonoperative and operative treatment of type II distal clavicle fractures. Bull Hosp Jt Dis. 2002;61(1–2):32–39. [PubMed] [Google Scholar]
- 12.Vander Have KL, Perdue AM, Caird MS, Farley FA. Operative versus nonoperative treatment of midshaft clavicle fractures in adolescents. J Pediatr Orthop. 2010;30(4):307–312. doi: 10.1097/BPO.0b013e3181db3227. [DOI] [PubMed] [Google Scholar]
- 13.Virtanen KJ, Malmivaara AO, Remes VM, Paavola MP. Operative and nonoperative treatment of clavicle fractures in adults. Acta Orthop. 2012;83(1):65–73. doi: 10.3109/17453674.2011.652884. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Deeks JJ, Altman DG, Bradburn MJ (2008) Statistical methods for examining heterogeneity and combining results from several studies in meta-analysis. Systematic reviews in health care: meta-analysis in context, 2nd edn. BMJ Publishing Group, London, pp 285–312
- 15.Böhme J, Bonk A, Bacher G, Wilharm A, Hoffmann R, Josten C. Current treatment concepts for mid-shaft fractures of the clavicle-results of a prospective multicentre study. Z Orthop Unfall. 2011;149(1):68–76. doi: 10.1055/s-0030-1250334. [DOI] [PubMed] [Google Scholar]
- 16.Canadian Orthopaedic Trauma Society Nonoperative treatment compared with plate fixation of displaced midshaft clavicular fractures. A multicenter, randomized clinical trial. J Bone Joint Surg Am. 2007;89:1–10. doi: 10.2106/JBJS.F.00020. [DOI] [PubMed] [Google Scholar]
- 17.Jubel A, Andermahr J, Prokop A, Lee J, Schiffer G, Rehm K. Treatment of mid-clavicular fractures in adults. Early results after rucksack bandage or elastic stable intramedullary nailing. Unfallchirurg. 2005;108(9):707–714. doi: 10.1007/s00113-005-0970-8. [DOI] [PubMed] [Google Scholar]
- 18.Judd DB, Pallis MP, Smith E, Bottoni CR. Acute operative stabilization versus nonoperative management of clavicle fractures. Am J Orthop (Belle Mead NJ) 2009;38(7):341–345. [PubMed] [Google Scholar]
- 19.Kulshrestha V, Roy T, Audige L. Operative versus nonoperative management of displaced midshaft clavicle fractures: a prospective cohort study. J Orthop Trauma. 2011;25(1):31–38. doi: 10.1097/BOT.0b013e3181d8290e. [DOI] [PubMed] [Google Scholar]
- 20.Smekal V, Irenberger A, Struve P, Wambacher M, Krappinger D, Kralinger FS. Elastic stable intramedullary nailing versus nonoperative treatment of displaced midshaft clavicular fractures-a randomized, controlled, clinical trial. J Orthop Trauma. 2009;23(2):106–112. doi: 10.1097/BOT.0b013e318190cf88. [DOI] [PubMed] [Google Scholar]
- 21.Smith C, Rudd J, Crosby L (2001) Results of operative versus non-operative treatment for 100 % displaced mid-shaft clavicle fractures: a prospective randomized trial. In: Proceedings from the 68th Annual Meeting of the American Academy of Orthopaedic Surgeons
- 22.Virtanen KJ, Paavola MP, Remes VM, Pajarinen J, Savolainen V, Bjorkenheim, JM (2010) Nonoperative versus operative treatment of midshaft clavicle fractures: a randomized controlled trial. The 75th Annual Meeting of the American Academy of Orthopaedic Surgeons, 9–12: 65–73
- 23.Zlowodzki M, Zelle BA, Cole PA, Jeray K, McKee MD. Treatment of acute midshaft clavicle fractures: systematic review of 2144 fractures: on behalf of the Evidence-Based Orthopaedic Trauma Working Group. J Orthop Trauma. 2005;19(7):504–507. doi: 10.1097/01.bot.0000172287.44278.ef. [DOI] [PubMed] [Google Scholar]
- 24.Lenza M, Belloti JC, Andriolo RB, Gomes Dos Santos JB, Faloppa F (2009) Conservative interventions for treating middle third clavicle fractures in adolescents and adults. Cochrane Database Syst Rev 2:CD007121 [DOI] [PubMed]