Abstract
Purpose
The restoration, and fixation, of normal pelvic anatomy after a windswept type injury can be a difficult endeavor and our purpose is to describe a method to accomplish this.
Methods
A stepwise and sequential technique was utilized to effectively reduce and stabilize this injury pattern. By first closing down the open disruption posteriorly and fixing with a partially threaded SI screw, a stable platform was created upon which to work from and subsequently distract and reduce the contralateral side via an anterior internal fixator (seven), external fixator (one), or plate (one). This was followed by a fully threaded SI screw in the compression side of the sacral fracture to hold the distraction. Nine consecutive patients with LC3 (61-B3.2) were included in the study with an average FU of 15 months.
Results
The Keshishyan deformity index revealed an initial mean deformity of 0.0456 which was corrected to 0.0170 (postop) and 0.0181 at latest follow up. This entailed an average correction of 62 % at the latest follow up. The follow-up group was significantly different from pre-op (p = 0.0040), but not post-op (p = 0.6833). Furthermore, post-op was significantly different from pre-op (p = 0.0089).
Conclusion
This is an effective method of correcting and maintaining reduction until healing for this relatively rare and difficult-to-treat injury pattern.
Introduction
The treatment of pelvic ring injuries requires appropriate reduction and stable fixation [1]. Various reduction manoeuvres and stabilization techniques exist based on the particular injury pattern. In a recent study, lateral compression type injuries were the most common, accounting for 77 % of all patterns [2]. Of these, lateral compression type three (LC3) (61-B3.2) fractures accounted for 5.9 % of all injuries. In other studies, this pattern was present in 1–14 % [3, 4] of cases. This injury is also known as the windswept deformity and it is described as a lateral compression type injury on one side (61-B2.2) and an anterior posterior compression injury (61-B1) on the contralateral side. By definition the windswept pelvis has vertical stability, but lacks rotational stability.
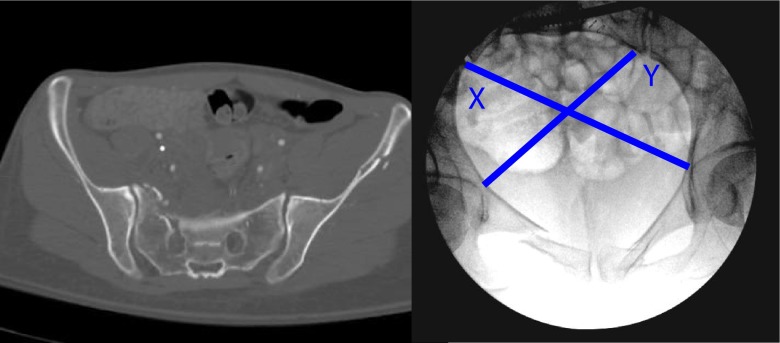
The diagnosis is made on plain radiographs and can be confirmed on CT scan for the posterior injury (Fig. 1). Occasionally the injury may be misdiagnosed as a one-sided lateral compression injury and the true nature of the injury becomes apparent after an attempt at distraction shows displacement of the presumed uninjured SI joint.
Fig. 1.
Patient 5 classic CT scan and inlet view X-ray of a windswept pelvic injury. X = 130.2, Y = 111, deformity index = Abs(X-Y)/(X + Y) = 0.0796
Even in light of surgical treatment, these injuries are still likely to have “persistent impairment" [5]. Restoration and fixation of the pelvic ring is important but unlike treating an isolated unilateral injury, there is no uninjured side that can be used as a stable reference point. An external rotation reduction on one hemi-pelvis to correct that deformity will likely exacerbate the contralateral internal rotation deformity, and vice versa.
To effectively reduce the pelvic shape and hold the reduction, a stepwise treatment pattern was developed to reestablish the pelvic ring in an LC3 (61-B3.2) pattern. To our knowledge, there are no reported descriptions of treating a windswept pelvis in this fashion. The purpose of this study to describe the technique and report its effectiveness.
Methods
Surgical technique
The patient is stabilized according to ATLS protocols under the direction of our General Surgery Trauma team. Orthopaedic treatment may consist of a binder or an initial external fixator if required. Once the patient is stable and ready for definitive fixation, we use a flat-top OSI table and single fluoroscopic machine. The presence of an experienced X-ray technician who can repeatedly position the c-arm in the lateral, inlet, outlet, outlet/obturator oblique and inlet obturator oblique can save much time.
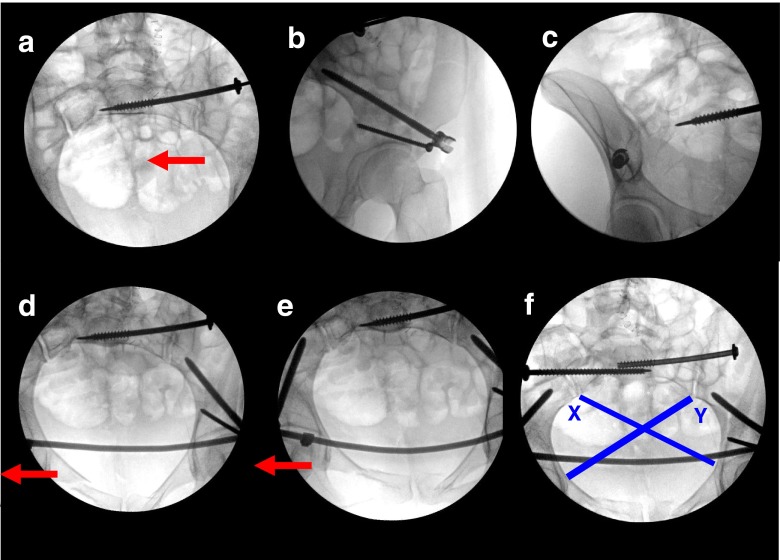
Attention is first turned to the open book side of the injury (usually an anterior sacroiliac diastasis). This is reduced and stabilized with a partially threaded iliosacral screw using standard technique [6]. The reduction is gauged on the inlet view of the image intensifier and if further reduction is needed another iliosacral screw can be considered, or if warranted an open reduction and plating to restore the normal anatomy. This is the key portion of the procedure as it effectively creates a stable platform upon which to build from that is anatomically reduced (Fig. 2a). This fixation now establishes a reduced and stable hemi pelvis and the reduction and fixation of the remaining ring performed from this point.
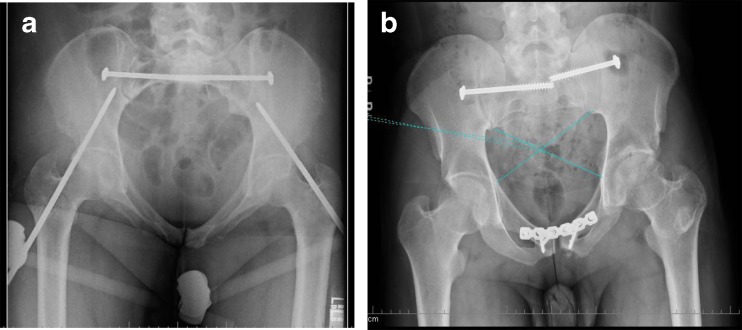
Fig. 2.
Patient 5. Sequential fixation technique. a SI screw closes the left SI joint. b,c,d Application of anterior internal fixator. e Distraction of anterior pelvis and posterior right sacral fracture against fixed left SI joint. f Left fully threaded right SI screw to hold sacral fracture. X = 153.0 Y = 156.6, DI =0.0116
Next, correction of the internally-rotated contralateral hemipelvis is performed. This can be accomplished in a variety of ways, i.e. external fixator, anterior internal fixator [7] or plate (Fig. 2b,c,d). Utilizing the stable fixed side, the opposite internal rotation is reduced, by taking advantage of the fixed angle construct of the anterior device. The laterally compressed injury, either the anterior sacrum, SI joint or iliac wing, is subsequently distracted back and reduced to a more anatomic position (Fig. 2d,e,f). With the anterior fixation locked, the posterior injury is then stabilized with a fully-threaded iliosacral screw (sacral fracture), or a plate ±AIIS-PSIS screw for iliac wing fracture. This reduction is verified on the inlet view of the image intensifier (Fig. 2f).
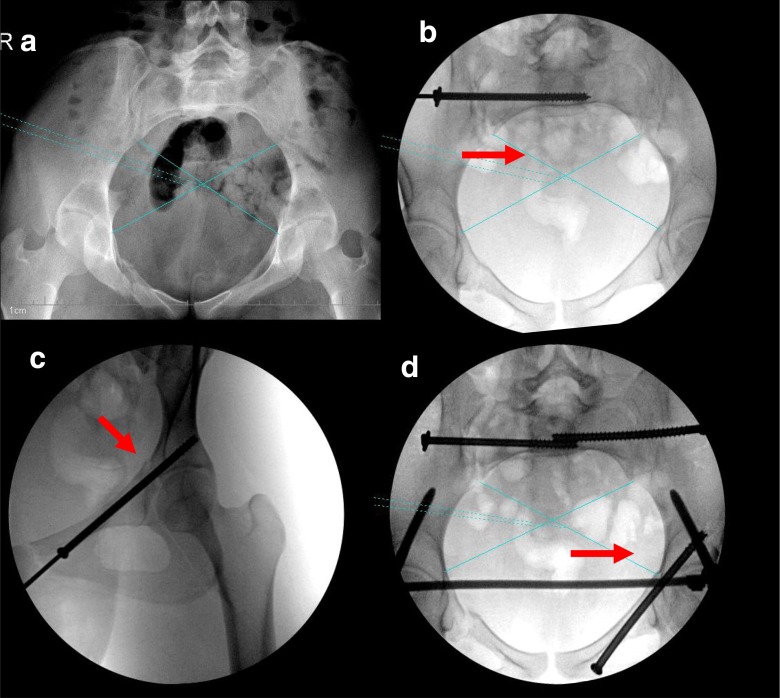
In certain situations where there are high rami fractures that involve the acetabulum, care must be taken to prevent distraction through the joint and an anterior column screw may be used prior to distraction (Fig. 3).
Fig. 3.
Patient 9. a Pre-operative X = 141.8 Y = 158.7 with high left ramus fracture intra-articular. b Right SI screw closes SI joint. c Anterior column screw protects acetabulum. d Anterior internal fixator distracts left sacral fracture and fixed with fully threaded SI screw, X = 157.4, Y = 165.0, DI 0.0235
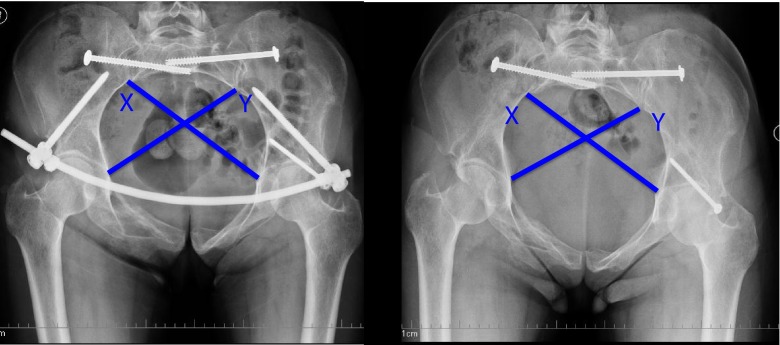
This technique was prospectively performed on nine consecutive patients with displaced windswept pelvic fractures (LC3) 61-B3.2 from 2008 to 2012. There were four men and five women with a mean age of 39 years (range 17–63) with an average follow up of 15 months (eight–31) months. All were treated with the above technique which included reduction of the open book portion of the posterior injury accomplished with a partially threaded iliosacral screw or open reduction and plating. This was then followed by either an anterior internal fixator (InFix seven) [7], external fixator (one) or a plate (one) (Figs. 4 and 5). We then placed a fully threaded iliosacral screw on the compression side of the injury to hold the reduction (sacral fracture). The anterior internal fixators were removed at 12–16 weeks [7], the external fixator at six weeks and the plate remained.
Fig. 4.
Patient 4. a At three months post operation, the fracture is stable and the anterior apparatus is removed. b At one year post operation the pelvis has healed and maintained its symmetry. Deformity index =0.016
Fig. 5.
Alternatively a plate (patient 5) or an external fixator (patient 7) can be used to accomplish the same result
For the nine patients, deformity indices were generated in the method described by Keshishyan et al. [8] (deformity index = absolute value (X-Y)/(X + Y); Fig. 1) at three points: before surgery, after surgery and at final follow-up. As this is a ratio, we also calculated the percent correction for each individual case and the average correction. The perfect deformity index would be zero and so correction was calculated as (pre-operative deformity index – post operative deformity index)/pre-operative deformity index multiplied by 100 to give a percentage of correction. Our hypothesis was that the technique employed for repair of the windswept pelvic fracture would systematically result in a demonstrable improvement from pre-operative obliquity to post-operative correction, without significant loss of correction at follow-up measurement. To test the null hypothesis of no difference between the groups of measurements, within-subject comparisons were performed using repeated measures ANOVA, and the associated sphericity assumption was examined using Mauchly’s test, both with alpha of 0.05; Huyhn-Feldt univariate correction was to be preferred in case of departure. Contrast operations were included to illustrate differences between each group of measurements. Analysis was done using SAS 9.3 (SAS Institute Inc., Cary, NC).
Results
All patients healed without incident. The mean deformity index was calculated to be 0.0456 ± .0242 (pre-operative), 0.0170 ± 0.14 (post operative), and 0.0181 ± .014 at latest follow up (Table 1). The mean correction of deformity was 62 % ± 26 % at latest follow up. Patients ambulated on average 12.3 weeks after the surgery. There was one complication, an infection and wound dehiscence one month postoperatively requiring implant removal which led to no sequelae at last follow up at 15 months (exfix). Anterior and posterior injuries are described in Table 2.
Table 1.
Deformity indexᅟ
| Patient | Preop deformity index | Postop deformity index | Latest FU deformity index | Final percent correction |
|---|---|---|---|---|
| 1 | 0.036505 | 0.028289 | 0.021129 | 42 % |
| 2 | 0.03231 | 0.006711 | 0.006711 | 79 % |
| 3 | 0.06087 | 0.04668 | 0.0466 | 23 % |
| 4 | 0.079602 | 0.011628 | 0.01623 | 80 % |
| 5 | 0.0271 | 0.010753 | 0.0183 | 33 % |
| 6 | 0.012389 | 0.004664 | 0.000336 | 97 % |
| 7 | 0.07891 | 0.017154 | 0.018012 | 77 % |
| 8 | 0.026376 | 0.003631 | 0.005243 | 80 % |
| 9 | 0.05624 | 0.023573 | 0.030629 | 46 % |
| Mean | 0.045589 | 0.0170 | 0.01813 | 62 % |
| STD | ±0.024203 | ±0.0139 | ±0.0141 | ±26 % |
Table 2.
Injuries
| Patient | Posterior injury R | Posterior injury L | Anterior injury |
|---|---|---|---|
| 1 | SI widening | Sacral fracture zone 1 | bilat rami fx L high |
| 2 | SI widening | Sacral fracture zone 1 | r rami fx, SP disrup, L acet fx |
| 3 | Sacral fracture zone 1 | SI widening | r rami fx SP disruption |
| 4 | Sacral fracture zone 1 | SI widening | bilat rami fx Low, L iliac fx |
| 5 | SI widening | Sacral fracture zone 1 | low rami fx |
| 6 | Sacral fracture zone 1 | SI widening | bilat rami fx low |
| 7 | Sacral fracture zone 2 | SI widening | r rami fx, |
| 8 | SI widening | Sacral fracture zone 1 | SP |
| 9 | SI widening | Sacral fracture zone 1 | r rami fx, L very high ramus acetab fx |
In the course of analysis, testing the sphericity assumption demonstrated significant departure, necessitating univariate correction; statistical significance was achieved at p = .0.0034. In comparing follow up to both pre-operative and post operative, the follow-up group was statistically significantly different from pre-op (p = 0.0040), but not post-op (p = .0.6833). Furthermore, post operative was significantly different from pre-operative (p = 0089).
Discussion
Windswept injuries account for about 6 % of pelvic fractures [4] but may account for 15 % of operated pelvic injuries [9]. In the treatment of certain pelvic injuries, the nature of the pattern and the remaining stability can be used to effectively reduce and stabilize the ring. For example, in an APC2 injury (61-B1.1), the posterior ligament(s) remain intact with vertical stability maintained, and so a simple reduction of the diastasis reduces the deformity. With an LC2 injury (61-B2.2), various fixation techniques can be utilized, i.e. LC2 screw [10] or an external fixator [11], etc., with a common theme that there is inherent stability for support from the contralateral uninjured side. In the LC3 (61-B3.2) pattern the posterior ligaments are theoretically intact and can be used to aid in the reduction. The problem when treating this windswept deformity, is that there is no stable platform from which to build and this amounts to trying to hit a moving target. The main benefit of the described technique is that it allows for a logical approach to treating LC3 injuries. However, unless this fixation is done in a stepwise fashion, the ring will likely be fixed effectively in situ, usually resembling an oblique ovoid and not normal ring anatomy.
A weakness with this technique is that it largely relies on having stable posterior ligamentous structures, or effectively an injury pattern that is not vertically unstable. While this stepwise technique could be used in the treatment of completely unstable injuries (61-C), it would be somewhat more difficult, likely requiring an open reduction and possible augmented fixation, above what has been mentioned.
There are certain instances when care has to be taken when reducing these fractures due to anterior fractures which may involve the acetabulum or iliac wing in addition to a posterior sacral injury. Here the acetabular component or iliac wing fracture must be stabilized before distraction with an exfix, infix or anterior plate to restore the posterior anatomy or the more anterior injury would be deformed.
The method of Keshishyan et al. [8] was used to measure the deformity in these LC3 injuries but there is some difficulty in using this measurement and getting perfect inlet or AP views. For this study we used inlet views and in several instances had to use an intra-operative pre-operative pelvic X-ray as X-rays in the trauma bay are often of poor quality. The deformity index was used as our PACS system is not perfectly calibrated to give absolute numbers but based on a pixel system length that does not exactly correlate to centimeters. The use of the deformity index which is a ratio eliminated the variation that would be effected by this problem which occurs for all digital PACS systems.
The frequency of these fractures is as reported approximately 5 % of all pelvic fractures in large series and explains the limited number of cases in our study. However, we were able to show that the technique was able to improve deformity in our cases and requires very little extra than what is already available to orthopedic trauma surgeons.
The technique described was able to reduce and fix the asymmetry of the pelvis in these windswept injuries until they healed. We reject the null hypothesis of no difference between deformity indices; a real and lasting correction of pelvic obliquity was achieved using this technique for addressing the windswept pelvis. Post operative and follow-up did not vary significantly from one another, suggesting that the reductions are adequately stable after healing.
Conclusion
We believe this simple stepwise technique that has not been previously described in the literature is crucial in restoring the anatomy in these complex pelvic fractures.
Acknowledgments
Conflict of interest
The FDA has not approved the devices Infix used for the purposes described in this manuscript.The authors declare that they have no conflict of interest in the preparation of this publication. We also declare that Dr. Vaidya has received payment for lectures from AO Trauma and Synthes Trauma for teaching courses; Dr. Vaidya has received payments for consulting with Stryker Corporation for implant development; Dr. Vaidya is involved in developing an FDA approved product for Stryker Corporation which is not this fixator that is made from custom spinal implants; butwhich have no relation to this topic or its preparation.
This paper has been presented in parts at the following meetings: Michigan Orthopaedic Society Meeting 2012, Macinac Island, Michigan. This paper has not been published elsewhere nor has any of the data.
Contributor Information
Rahul Vaidya, Phone: +1-313-9667852, FAX: +1-313-9668400, Email: rahvaidya2012@gmail.com.
Bryant W. Oliphant, Phone: +1-313-9667852, FAX: +1-313-9668400, Email: gtwalkon@gmail.com
Ian Hudson, Phone: +1-313-9667852, FAX: 1-313-9668400, Email: Hudson1@msu.edu.
Mitch Herrema, Phone: +1-313-9667852, FAX: +1-313-9668400, Email: Herremam1@gmail.com.
David Knesek, Phone: +1-313-9667852, FAX: +1-313-9668400, Email: davidknesek@gmail.com.
Fred Tonnos, Phone: +1-313-9667852, FAX: +1-313-9668400, Email: tonnosfr@msu.edu.
References
- 1.Tile M. Pelvic ring fractures: should they be fixed? J Bone Joint Surg Br. 1988;70:1–12. doi: 10.1302/0301-620X.70B1.3276697. [DOI] [PubMed] [Google Scholar]
- 2.Manson T, O’Toole RV, Whitney A, Duggan B, Sciadini M, Nascone J. Young-Burgess classification of pelvic ring fractures: does it predict mortality, transfusion requirements, and non-orthopaedic injuries? J Orthop Trauma. 2010;24:603–609. doi: 10.1097/BOT.0b013e3181d3cb6b. [DOI] [PubMed] [Google Scholar]
- 3.Weaver MJ, Bruinsma W, Toney E, Dafford E, Vrahas MS. What are the patterns of injury and displacement seen in lateral compression pelvic fractures? Clin Orthop Relat Res. 2012;470(8):2104–2110. doi: 10.1007/s11999-012-2364-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Burgess AR, Eastridge BJ, Young JW, et al. Pelvic ring disruptions: effective classification system and treatment protocols. J Trauma. 1990;30:848–856. doi: 10.1097/00005373-199007000-00015. [DOI] [PubMed] [Google Scholar]
- 5.Hoffmann MF, Jones CB, Sietsema DL. Persistent impairment after surgically treated lateral compression pelvic injury. Clin Orthop Relat Res. 2012;470:2161–2172. doi: 10.1007/s11999-012-2247-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Routt ML, Nork SE, Mills WJ (2000) Percutaneous fixation of pelvic ring disruptions. Clin Orthop Relat Res 15–29 [DOI] [PubMed]
- 7.Vaidya R, Colen R, Vigdorchik J, Tonnos F, Sethi A. Treatment of unstable pelvic ring injuries with an internal anterior fixator and posterior fixation: initial clinical series. J Orthop Trauma. 2012;26:1–8. doi: 10.1097/BOT.0b013e318233b8a7. [DOI] [PubMed] [Google Scholar]
- 8.Keshishyan RA, Rozinov VM, Malakhov OA, et al. Pelvic polyfractures in children. Radiographic diagnosis and treatment. Clin Orthop Relat Res. 1995;32:28–33. [PubMed] [Google Scholar]
- 9.Vaidya R, Kubiak EN, Bergin PF, et al. Complications of anterior subcutaneous internal fixation for unstable pelvis fractures: a multicenter study. Clin Orthop Relat Res. 2012;470(8):2124–31. doi: 10.1007/s11999-011-2233-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Starr AJ, Walter JC, Harris RW, Reinert CM, Jones AL. Percutaneous screw fixation of fractures of the iliac wing and fracture-dislocations of the sacro-iliac joint (OTA Types 61-B2.2 and 61-B2.3, or Young-Burgess "lateral compression type II" pelvic fractures) J Orthop Trauma. 2002;16:116–123. doi: 10.1097/00005131-200202000-00008. [DOI] [PubMed] [Google Scholar]
- 11.Bellabarba C, Ricci WM, Bolhofner BR. Distraction external fixation in lateral compression pelvic fractures. J Orthop Trauma. 2000;14:475–482. doi: 10.1097/00005131-200009000-00003. [DOI] [PubMed] [Google Scholar]