Abstract
Purpose
The aim of this study was to compare total knee arthroplasty (TKA) procedures between different countries with regard to epidemiological data and surgical technique by reference to the worldwide arthroplasty registers.
Methods
A systematic search was carried out using the EFORT website to identify the relevant arthroplasty registers. We extracted data with respect to the number of implanted TKAs, patients’ age distribution, procedure types, and revision rates. After identification of 28 national arthroplasty registers, 11 offered sufficient data regarding the above mentioned parameters and were therefore included in the final analysis.
Results
A large variation was found in the annual number of primary TKA implantations per inhabitant with a reported range from 30 to 199 per 100,000 (mean 106). The fixation method varied strongly between the different registers as well, e.g. 90 % of totally cemented TKAs in Sweden, England and Wales, Slovakia, and New Zealand versus 54 % cemented fixation in Australia. Another significant difference between included countries was observed with respect to the use of patellar resurfacing in TKA. Whilst the Danish knee arthroplasty register reports a percentage of 72 % using a patellar button in TKA the register from Norway reports only a minority of 2 %.
Conclusions
The comparison of arthroplasty registers revealed large differences regarding the annual number of primary TKAs per inhabitant and primary TKA procedure types. These variations may be explained by several factors such as patient demographics (prevalence of osteoarthritis) and national conditions such as healthcare systems (insurance status), number or availability of performing surgeons, medical facilities and surgeon-dependent factors such as definition of indications, education, tradition and experience.
Introduction
The development of joint arthroplasty in the 1970s promoted the establishment of projects for documentation purposes leading to the establishment of arthroplasty registers [1, 2]. The arthroplasty records developed from institutional and later multicentred databases up to regional and national arthroplasty registries [1, 3]. The Swedish knee arthroplasty register was the first national register of its vein, followed by registers from more and more countries [4].
National joint arthroplasty registries facilitate an exchange of experiences concerning new materials and surgical methods, which is beneficial for the evaluation of efficacy and detection of failures and disadvantages as early as possible. Furthermore, national registers play an important role in the comparative analysis of implant performance, the detection of revision rates following total joint arthroplasty, and identification of patients for the purpose of follow-ups and recalls [5–10]. This allows a continuous, evidence-based adaptation of implant-choice and surgical technique to achieve improved results.
By now, there are several national registries from a large part of the European countries and furthermore from the United States, Canada, Australia, and New Zealand. These national registers should give an important overview on incidence, practice, and outcome of primary total joint arthroplasty and revision procedures [11–14]. However, no systematic comparisons with a focus on the surgical technique of total knee arthroplasty (TKA) using international arthroplasty registers have been published so far as we know. The actual epidemiology and precise description of procedure type and surgical technique of TKA is of interest and well worth being described in detail.
The aim of this study was therefore the comparison of primary total knee arthroplasty procedures between different countries concerning epidemiological data and surgical technique as well as revision rates by the use of worldwide knee arthroplasty registers.
Materials and methods
The EFORT Website for European Arthroplasty Registers was used to identify the existing worldwide registers included in our study [15]. In addition, we performed a free-hand search using the terms “(arthroplasty register) OR (knee arthroplasty register)” via Google. This method was described in previous studies of our group [16, 17].
These registers were searched to find the annual report from 2010 or, if not available, from 2009 or the most recent documented time period. We extracted data with respect to the number of implanted TKAs, the patients’ age distribution, procedure types, and revision rates. These parameters were analysed for each arthroplasty register in duplicate using a qualitative content analysis of the text and compared against one another. Disagreement was resolved by discussion or, if necessary, by the decision of the senior author according to the PRISMA criteria published by the CONSORT group [18, 19].
All except two countries presented their data in the form of an annual report for each year separately, whereas the others reported summarised data, mostly from the year of establishment of their arthroplasty registers until the most recent documented time period. Time periods of the number, age distribution, and procedure type included recording over a one-year period except for the registers of Australia, New Zealand and Spain (Catalonia), where data was reported for long time periods. Registers used different classifications with respect to age distribution and were pooled, if applicable.
Primary total knee arthroplasty procedures were differentiated into types of procedures including total replacement with or without patellar resurfacing and unicompartmental procedures as well as into method of fixation including cemented, cementless, hybrid (cemented tibial and cementless femoral component), and reverse hybrid primary knee arthroplasties (cemented femoral component and cementless tibial component). In most registers, hybrid and reversed hybrid fixation procedures were not reported separately. Hybrid and reversed hybrid TKAs were therefore subsumed under “hybrid fixation” in our study.
Results
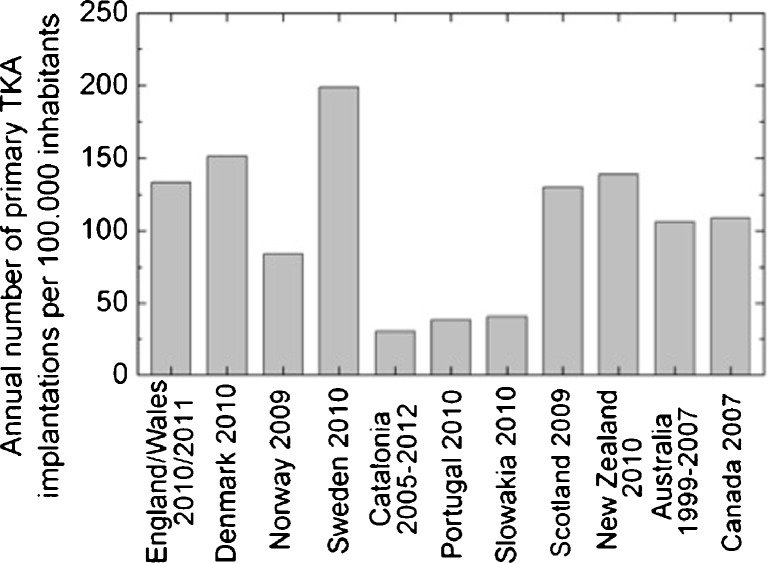
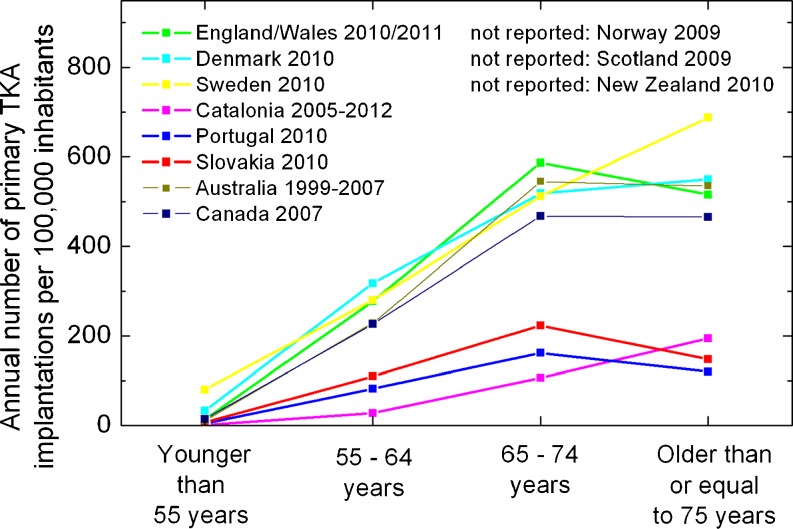
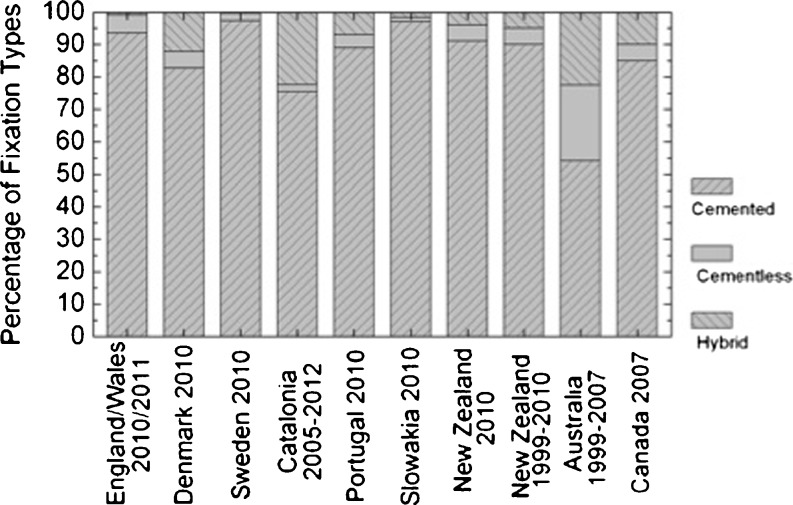
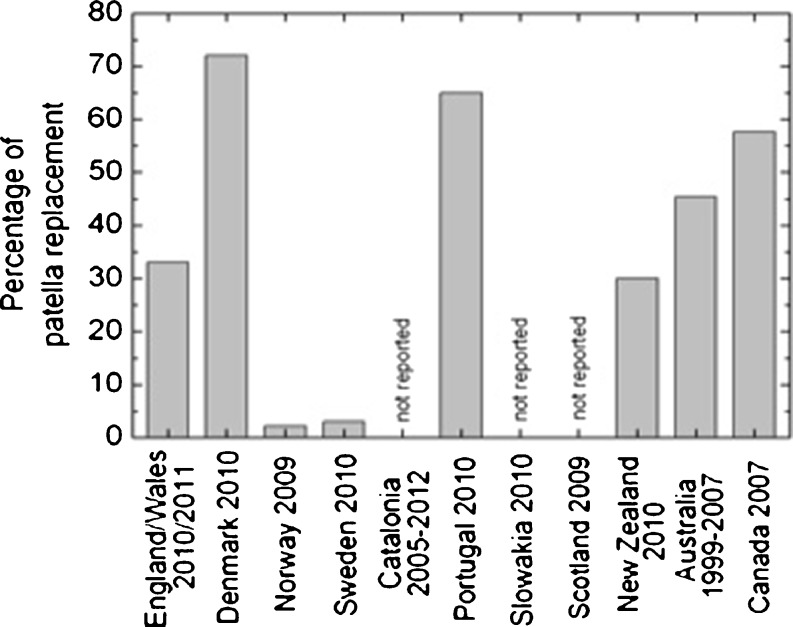
After initial identification of 28 national or regional arthroplasty registers, 11 (England & Wales, Denmark, Norway, Sweden, Catalonia, Portugal, Slovakia, Scotland, New Zealand, Australia, and Canada) offered sufficient data and were included in the final analysis. Eight of the included registers are national registers and the Scottish, English and Catalan arthroplasty registers operate on a regional basis. A large variation was found in the annual number of primary TKA implantations per inhabitant with a reported range from 30 to 199 per 100,000 (mean 106) as shown in Fig. 1. Figure 2 shows the distribution of annual primary TKA implantations according to age groups. The fixation method varied strongly between the different registers as well, e.g. 90 % of totally cemented TKAs in Sweden, England and Wales, Slovakia and New Zealand versus 54 % cemented fixation in Australia as illustrated in Fig. 3. Another significant difference between included countries was observed with respect to the use of patellar resurfacing in TKA. Whilst the Danish knee arthroplasty register reports a percentage of 72 % using a patellar button in TKA the register from Norway reports only a minority of 2 % (Fig. 4). Revision rates after TKA varied from 4.4 to 12.5 % (mean 8.02 %) as illustrated in Table 1.
Fig. 1.
Reported number of annual primary total knee arthroplasty (TKA) implantations per inhabitant in different worldwide arthroplasty registers
Fig. 2.
Distribution of annual primary total knee arthroplasty (TKA) implantations in worldwide arthroplasty registers according to different age groups
Fig. 3.
Fixation method (totally cemented, cementless, or hybrid fixation) of primary total knee arthroplasty (TKA) presented in worldwide arthroplasty registers
Fig. 4.
Percentage of patella replacement for primary total knee arthroplasty (TKA) in different worldwide arthroplasty registers
Table 1.
Number (and percentage) of annual revision rates of primary total knee arthroplasty (TKA) reported in worldwide arthroplasty register datasets
| Arthroplasty registers | Absolute and (relative) revisions |
|---|---|
| England/Wales 2010/2011 | 5109 (6.6 %) |
| Denmark 2010 | 1092 (12.5 %) |
| Norway 2009 | 435 (9.8 %) |
| Sweden 2000–2009 | 4835 (3.7 %) |
| Catalonia 2005–2012 | 1602 (8.6 %) |
| Portugal 2010 | 291 (7 %) |
| Slovakia 2010 | 97 (4.4 %) |
| Scotland 2009 | 567 (8.2 %) |
| New Zealand 2010 | 425 (6.9 %) |
| New Zealand 1999–2010 | 4158 (8 %) |
| Australia 1999–2007 | 17717 (10.7 %) |
| Canada 2007 | 1075 (6.3 %) |
Discussion
The aim of this study was the comparison of primary total knee arthroplasty (TKA) procedures between different countries concerning epidemiological data and surgical technique as well as revision rates through the use of worldwide knee arthroplasty registers.
Worldwide arthroplasty registers are essential to analyse single surgical devices and pooled analyses have successfully served as guidelines in the past [16, 17]. However, in order to compare register datasets from different countries a comparable minimal dataset is essential [20]. Our study is a pooled analysis of worldwide knee register data to evaluate application and surgical technique.
A large variation was found regarding the annual number of primary TKA implantations across the countries. These variations may be explained by several factors including patient demographics (prevalence of joint disease) and national conditions such as healthcare systems (insurance status), availability of surgeons and medical facilities and surgeon-dependent factors such as definition of indications, education, tradition and experience [10].
While the mean age of patients was similar between the different registers, the more specific distributions varied widely, with Slovakia, England and Wales, Australia and Portugal reporting the majority of implantations in patients at 65–75 years of age and the countries Denmark, Sweden and Spain (Catalonia) reporting majority implantations in patients at 75 years of age or older.
All of the investigated registers have had a predominance of female patients with a proportion of women up to 73 % in Portugal and Spain (Catalonia).
We further observed differences with respect to the fixation method in TKA and the use of unicompartmental arthroplasties between the investigated registers. The fixation type varied from more than 90 % cemented fixation in Sweden, England and Wales, Slovakia and New Zealand to 54 % cemented fixation in Australia. The percentage of hybrid or reversed hybrid procedures varied between one and 23 % between different registers.
Data revealed a north–south expansion with more cemented arthroplasties in Scandinavian countries than southern countries, such as the authors' (Austria and Germany). However, there were short periods when even Swedish registers also reported a higher percentage of uncemented prostheses in the mid 1980s.
Pooled outcome of register data revealed no consensus between countries with respect to the use of patellar resurfacing. Whilst the Danish knee arthroplasty register [15] reports a percentage of 72 % using a patellar button in TKA in 2009 it was only 2 % in Norway according to the Norwegian arthroplasty register report in 2010 [15].
The Australian Joint Replacement Registry [15] has reported a 1.3 times higher proportion of TKAs without patellar resurfacing for revision surgery compared to TKAs using a patellar button in their annual report. However, it is unclear why there is such a big difference regarding the use of a patellar button between the countries mentioned [15]. Again, the Swedish register reported a higher proportion of resurfaced patellae in the mid 1980s with even a lower risk of revision in case of resurfaced TKA. However, this data is biased, because cases without patella buttons underwent secondary resurfacing in case of pain due to unknown causes and, nowadays, TKA in Sweden is mostly performed without patella buttons.
The annual percentage of unicompartimental knee arthroplasties varied between 1.5 % (Spain) and 15.5 % (Australia). Partial knee replacement includes a variety of procedures, such as unicondylar or femoropatellar replacement, as well as other partial resurfacings [14]. Exact numbers of all types of unicompartimental or resurfacing procedures were not given in most of the registers und therefore not conclusively reported in the results section.
This study has the following limitations. First, as for every meta-analysis, this study is dependent on the quality of the primary data included. Therefore, it is not clear whether the reported number of operations in the registers reflects the true number of primary procedures and revisions performed in every investigated country. Further limitations include the lack of standardisation of reporting age, gender distribution, the use of fixation techniques, or the number of revisions in the investigated arthroplasty registers. Next, only the Swedish register reports sufficient evidence on data compliance and we cannot tell how high the percentage of complete data reporting is in different registers. In addition, further issues are the completeness of reporting of the registers, difficulties in comparison of different registers due to region-specific differences in register datasets and a possible lack of knowledge of a minimal dataset [20].
We want to underline the significant benefit that this is the first study to analyse pooled incidence and application type of TKA using data from worldwide arthroplasty registers.
Conclusion
The comparison of worldwide arthroplasty registers showed a large variance regarding age distribution, annual number of procedures, implant techniques, and revision rates of TKAs. These international variations may be explained by several independent factors including patient demographics (prevalence of joint disease) as well as national conditions (insurance status) such as healthcare systems, number or availability of surgeons and medical facilities and surgeon-dependent factors such as definition of indications, education, tradition and experience.
References
- 1.Robertsson O. Knee arthroplasty registers. J Bone Joint Surg Br. 2007;89B:1–4. doi: 10.1302/0301-620X.89B1.18327. [DOI] [PubMed] [Google Scholar]
- 2.Charnley J. Low friction arthroplasty of the hip: theory and practice. Berlin: Springer; 1979. [Google Scholar]
- 3.Berry DJ, Kessler M, Morrey BF. Maintaining a hip registry for 25 years: Mayo clinic experience. Clin Orthop. 1997;344:618. doi: 10.1097/00003086-199711000-00007. [DOI] [PubMed] [Google Scholar]
- 4.Robertsson O, Lewold S, Knutson K, Lidgren L. The Swedish knee arthroplasty project. Acta Orthop Scand. 2007;71:7–18. doi: 10.1080/00016470052943829. [DOI] [PubMed] [Google Scholar]
- 5.Ranstam J, Robertsson O. Statistical analysis of arthroplasty register data. Acta Orthop. 2010;81(1):10–14. doi: 10.3109/17453671003587168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Robertsson O, Mendenhall S, Paxton EW, Inacio MCS, Graves S. Challenges in prosthesis classification. J Bone Joint Surg Am. 2011;93E:72–5. doi: 10.2106/JBJS.K.00990. [DOI] [PubMed] [Google Scholar]
- 7.Sadoghi P, Schröder C, Fottner A, Steinbrück A, Betz O, Müller PE, Jansson V, Hölzer A. Application and survival curve of total hip arthroplasties: a systematic comparative analysis using worldwide hip arthroplasty registers. Int Orthop. 2012;36(11):2197–203. doi: 10.1007/s00264-012-1614-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Labek G, Janda W, Agreiter M, Schuh R, Böhler N. Organisation, data evaluation, interpretation and effect of arthroplasty register data on the outcome in terms of revision rate in total hip arthroplasty. Int Orthop. 2011;35(2):157–163. doi: 10.1007/s00264-010-1131-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Labek G, Frischhut S, Schlichtherle R, Williams A, Thaler M. Outcome of the cementless Taperloc stem: a comprehensive literature review including arthroplasty register data. Acta Orthop. 2011;82(2):143–148. doi: 10.3109/17453674.2011.570668. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Labek G, Kovac S, Levasic V, Janda W, Zagra L. The outcome of the cementless tapered SL-Plus stem: an analysis of arthroplasty register data. Int Orthop. 2012;36(6):1149–1154. doi: 10.1007/s00264-011-1421-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Paxton EW, Furnes O, Namba RS, Inacio MCS, Fenstad AM, Havelin LI. Comparison of the Norwegian knee arthroplasty register and a United States Arthroplasty Registry. J Bone Joint Surg Am. 2011;93(3E):20–30. doi: 10.2106/JBJS.K.01045. [DOI] [PubMed] [Google Scholar]
- 12.Robertsson O, Bizjajeva S, Fenstad AM, Furnes O, Lidgren L, Mehnert F, Odgaard A, Pedersen AB, Havelin LI. Knee arthroplasty in Denmark, Norway and Sweden. Acta Orthop. 2010;81:82–89. doi: 10.3109/17453671003685442. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.W-Dahl A, Robertsson O, Lidgren L, Miller L, Davidson D, Graves S. Unicompartmental knee arthroplasty in patients aged less than 65. Acta Orthop. 2010;81:90–94. doi: 10.3109/17453671003587150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kurtz SM, Ong KL, Lau E, Widmer M, Maravic M, Gómez-Barrena E, de Fátima de Pina M, Manno V, Torre M, Walter WL, Steiger R, Geesink RGT, Peltola M, Röder C. International survey of primary and revision total knee replacement. Int Orthop. 2011;35:1783–1789. doi: 10.1007/s00264-011-1235-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.European Arthroplasty Register (2011) EAR European arthroplasty register. http://www.ear.efort.org. Accessed 22 September 2012
- 16.Sadoghi P, Liebensteiner M, Agreiter M, Leithner A, Böhler N, Labek G (2013) Revision surgery after total joint arthroplasty: a complication-based analysis using worldwide arthroplasty registers. J Arthroplasty doi:10.1016/j.arth.2013.01.012 [DOI] [PubMed]
- 17.Sadoghi P, Thaler M, Janda W, Hübl M, Leithner A, Labek G (2013) Comparative pooled survival and revision rate of Austin-Moore hip arthroplasty in published literature and arthroplasty register data. J Arthroplasty doi:10.1016/j.arth.2012.12.011 [DOI] [PubMed]
- 18.Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, Clarke M, Devereaux PJ, Kleijnen J, Moher D (2009) The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. PLoS Med 6(7):E [DOI] [PMC free article] [PubMed]
- 19.Moher D, Cook DJ, Eastwood S, Olkin I, Rennie D, Stroup DF. Improving the quality of reports of meta-analyses of randomised controlled trials: the QUOROM statement. Quality of reporting of meta-analyses. Lancet. 1999;354:1896–900. doi: 10.1016/S0140-6736(99)04149-5. [DOI] [PubMed] [Google Scholar]
- 20.Sadoghi P, Leithner A, Labek G (2013) Overcoming boundaries of worldwide joint arthroplasty registers: the European arthroplasty register minimal dataset. J Arthroplasty doi:10.1016/j.arth.2013.02.023 [DOI] [PubMed]