Abstract
Purpose
The authors made a retrospective analysis of three triage situations of war wounded in Chad and Rwanda in which mass casualties overwhelmed available medical facilities.
Methods
The triage classification is based on the waiting period for surgery. The categories are: extreme, first, second and third emergencies, expectant, walking wounded.
Results
In Chad, 23 wounded adults were received in 24 hours, and 19 were operated up on within 48 hours. In Rwanda 1, 94 wounded were received in two hours, of whom 68 were operated upon, 23 on the first day. In Rwanda 2, 59 wounded were received in 12 hours, treatment of extreme and first emergencies required 48 hours, while second and third emergencies were treated during the three following days.
Conclusions
These episodes were very different when considering the setting, the number of casualties, the type of wounds, the logistical and medical difficulties. The authors report the difficulties faced and the lessons learned.
“Il faut toujours commencer par le plus douloureusement blessé sans avoir égard aux rangs et aux distinctions.” You must always begin with those who are most seriously wounded without regard to rank or other distinction. Baron Larrey (1766–1842), surgeon to Napoléon’s Imperial Guard [1]
Keywords: Triage, Mass casualties, War, Waiting period
Introduction
The concept of triage is essential in the management of soldiers’ and civilians’ wounds in war or in natural disasters. Triage is used when the medical care system is overloaded, meaning there are more people who need care than there are available resources to care for them. It allows the rational utilisation of resources in order to benefit the greatest number.
The French definition is “draw or choose, after examination.” Triage is a process of sorting the casualties according to the severity of injury and the prioritisation of treatment.
The need to sort war casualties rose dramatically in the 19th century during the Napoleonic wars. Dominique Jean Larrey was the first to organise triage in the field [1, 2]. He also described the echelons of care that characterise modern military surgery.
The French army medical service is frequently engaged in treating servicemen or civilians injured in armed conflict or natural disasters. Our surgical teams have experience from many military and humanitarian missions. Many times in recent years, field surgical teams have used triage to the benefit of French soldiers and combatants from other countries (2004 Ivory Coast; 2008 Kosovo; 2008 and 2012 Afghanistan; 2013 Mali).
The authors, with a Forward Surgical Team (FST) had to cope with three episodes of triage of war wounded in 1994 in Chad and Rwanda. This article reports the difficulties faced and the lessons learned.
Materials and methods
This is a retrospective analysis of the management of three mass casualties in Chad and Rwanda in 1994. FST of the French Medical Corps is a small facility (Table 1). The first mission was to support the French Armed Forces and provide the initial medical support abroad for all military and/or humanitarian operations. The wounded were not supposed to stay in the FST. In the three reported experiences the unit had no ability to evacuate the wounded.
Table 1.
Composition of a forward surgical team
| Forward Surgical Team (FST) of the French armed forces military medical service | |
|---|---|
| Category | Description |
| Mission | 1. Treat wounded and after stabilisation quickly evacuate them to the rear |
| 2. Treat wounded civilians in humanitarian operation | |
| Composition | Three physicians (one general surgeon, one orthopaedic surgeon, one anaesthetist) |
| Five nurses (two anaesthetists, one operating room, one for the ward) | |
| Four corpsmen | |
| Infrastructure | Two tents: one operating room and one 12 bedroom |
| Equipment | Equipment for the treatment of all surgical emergencies (abdominal, thoracic, neurosurgical and orthopaedic) |
| Treatment capacity | Operational within one hour of arriving at location. |
| Ten to 12 procedures/day | |
| Theoretical triage capacity: 100 wounded per day | |
| Limits of independence | Capable of working independently in 48 h |
| Basic supplies | 48 h (including water, food, gas for generating set, drugs, surgical material) |
| 30 red packed cells units, resupplied every three weeks X-ray equipment, laboratory | |
| Shipping size | 5137 kg, 30 m3 |
Triage system
The French classification is based on one criterion only—the waiting period for surgery. Classifications are reported in Table 2. The third column shows a few examples of the wounded for each category.
Table 2.
Triage categories
| Category | Time to surgery | Example |
|---|---|---|
| EU/Extreme emergency | Immediate resuscitation and/or intervention | Massive haemorrhage |
| Respiratory distress | ||
| U1/First emergency | 6 h | Abdomen |
| Limbs (tourniquet, major wounds) | ||
| Head (neurological signs) | ||
| Burns > 15 % | ||
| U2/Second emergency | 18 h (or more) | Limbs |
| U3/Third emergency | Head | |
| Facial wounds, ophthalmology | ||
| Chest | ||
| Eclopés/Walking wounded | No surgery | |
| Potential emergency | No surgery. Constant reassessment and updating | Multiple small wounds of the trunk : penetration? |
| U4/Expectant | No surgery |
Environmental constraints
Chad, January 1994
Since 1986, one FST has been based in N’djamena to provide surgical support for the French troops and for French citizens and foreigners. The FST took care of Chadian soldiers and some Chadian civilian people. In this case the FST was not housed in tents but in a building with two well equipped operating rooms, X-ray equipment and laboratory. There were also a large number of ancillary personnel. In addition to the FST there were regimental medical officers, one chemist, laboratory technicians, and nurses. There were also some Chadian employees, who were very useful as translators. N’djamena FST was rather more a small MASH than a simple FST. The organisation of triage was well planned in this hospital because mass casualties of Chadian soldiers had been received once or twice a year.
Rwanda, July 1994
The same FST was sent to Rwanda in June 1994 with the French troops during the “Operation Turquoise”. Its goal was to try to stop the massacre of Tutsis people. The FST was based in Goma, a city on the border between Rwanda and Zaire. The FST’s organisation was basic. The FST was planned for the emergency surgical treatment of French soldiers before an early evacuation to France. Because of an unexpected flood of refugees to Goma, the FST had to take care of the civilian population as well. More than 500 patients were received within two months. We performed more than 300 surgical procedures and coped with two mass casualty situations.
Results
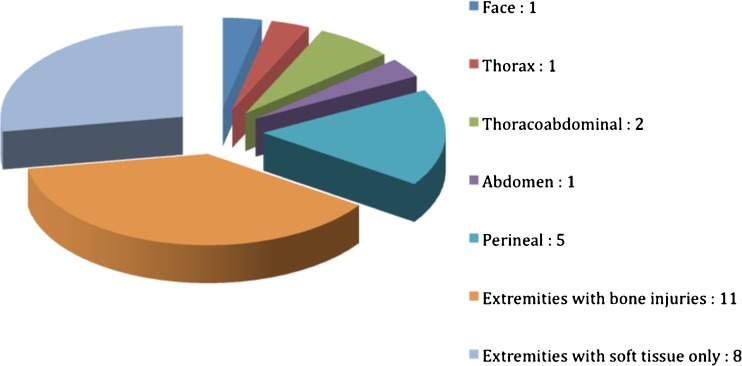
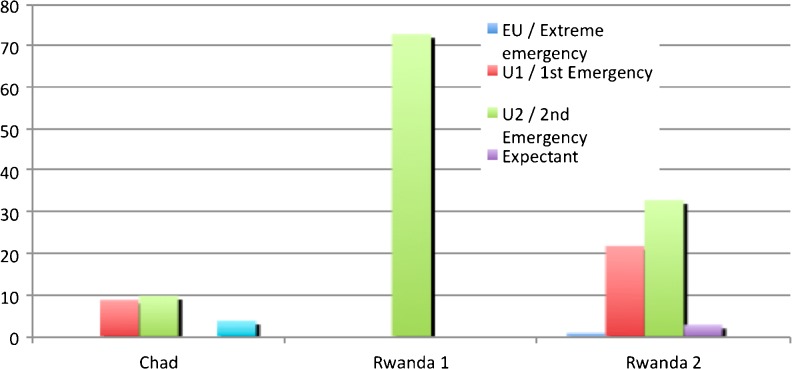
Mass casualties in Chad (Fig. 1). Twenty three wounded were received within 24 hours. All were male adults. They sustained 21 gunshot wounds and two blunt traumas. Categorisation was nine U1, ten U2 and four ambulatories (Fig. 2). Nineteen wounded were operated upon within 48 hours. The priority of treatment was first the face wounds, second the thoracabdominal wound, and third abdominal and perineal wounds. There was no mortality.
Fig. 1.
Distribution of injuries in Chad
Fig. 2.
Categorisation in the three triage situations in Chad
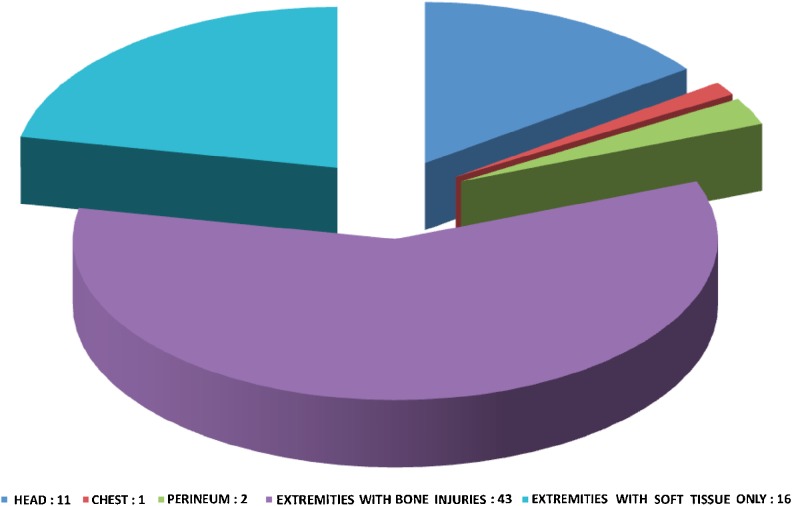
The first instance of mass casualties in Rwanda (Fig. 3) occurred when thousands of refugees fled from the massacres. The most severely injured were brought to the FST by helicopter. Ninety-four wounded were received within two hours. Survivors were seen days or weeks after wounding. Thirty percent were children and 20 % were women. Seventy percent sustained machete wounds and 30 % gunshot wounds.
Fig. 3.
Distribution of injuries during the first episode in Rwanda
Triage was performed during the night in front of the tents. Identification of the wounded was a difficult task. Most of them did not speak French and we did not have translators. Some children were too young to communicate with and were frightened without their parents. For registration we had to write a number on the forehead or the wrist of the patient.
Sixty eight out of 94 were operated upon. The delay between wounding and arrival was so long that we did not face any extreme or first level emergencies. All wounded were classified as second level emergencies (Fig. 2). Twenty-three patients were operated upon within the first day. Priority was given to head wounds because we feared cranio-cerebral injuries. Then we treated perineal injuries and finally limb wounds. Many of these injuries were infected with early gangrene. When children and adults presented with similar injuries, children were treated first.
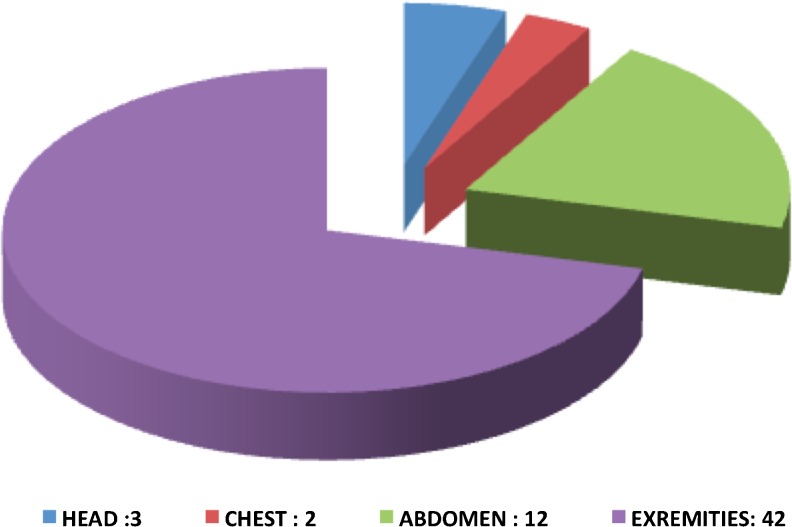
The second instance of mass casualties in Rwanda (Fig. 4) occurred ten days later where one million refugees were settled around the airport near the FST. They were targeted by mortar attacks. Fifty nine wounded were received within 12 hours. Thirty percent were children, 70 % sustained fragment wounds and 30 % gunshot wounds.
Fig. 4.
Distribution of injuries during the second episode in Rwanda
Triage was performed in daylight, most logistical problems had been solved after the first triage, and translators were available. Categorisation was such that there was one extreme emergency (cardiac wound in a French officer) and three patients were classified “expectant” (severe cranio-cerebral wounds and coma). Nearly 50 % were classified extreme emergency or first emergency. The choice of priorities of treatment had to be made for patients classified in the same category. We therefore treated abdominal wounds before patients with seriously damaged limbs.
Treatment of extreme and first emergency required 48 hours of continuous work. Second and third level emergencies were treated during the three following days. Some of them were operated upon more than 20 hours after wounding, when they should have been treated within six hours according to category. Thirteen patients died: three expectants, three while waiting for surgery (one hip joint wound, two upper limbs with severe injuries) and seven after surgery (one head, four abdominal with associated injuries including three children, two severe upper limb).
During the postoperative course we were forced to keep these refugees in the FST because of the same lack of social organisation and the impossibility of early evacuation. A major cholera epidemic worsened the situation. Thousands of refugees died from cholera. More than 150 patients stayed under our tents and about 20 suffered from cholera but only one died.
Discussion
These three episodes were very different when considering the setting, the number of casualties and the types of wounds. The logistical and medical difficulties were also different, but they both shared the complete inability to transfer wounded to a higher level of medical care.
A situation in which the number of casualties overwhelms the medical resources is uncommon. For management of many casualties we can distinguish two different situations. First is multiple casualties, where the number does not exceed available medical resources. In this case, the triage permits every patient the appropriate medical treatment without delay. Triage delivers “the right patient to the right place at the right time” [3]. Second is mass casualties that overwhelm available medical facilities. Some patients simply cannot be treated in a timely manner. The goal of triage is to ensure the best possible chance of survival for the largest number of people. Triage imposes a process which delivers “the greatest good for the greatest number” [4] or “the best for the most” and not “everything for everyone” [5].
Triage in Chad could be viewed as “easy”. This was a well organised and trained facility where medical staffing was adequate, equipment was sufficient, and the social context was good. Families could help feed and provide the patients’ nursing. The triage was easy because there were a relatively small number of casualties and the flow of victims did not exceed capacity in any single day. Finally, because of a long delay, the most severely injured died before arrival, making decisions about the remaining priorities easy.
During the first mass casualty situation in Rwanda medical problems were limited because of the very long delay before arrival. Logistical problems were serious. Indeed major difficulties have to be expected when a small surgical facility is coping with mass casualties over such a short period of time. The organisation of the reception centre was difficult, e.g. for registration, identification and translation with patients, especially for civilians and children. This has been reported by several authors [6]. It is even more difficult when refugees are without relatives to help them, when there is no possibility of evacuation. Furthermore in overcrowded tents the monitoring of patients is very difficult.
Second mass casualty situation in Rwanda. The logistic problems were solved or improved after the first mass casualties incident. The medical problems were very different. Sorting was very difficult because of the high rate of seriously wounded, e.g. near 50 % were classified EU or U1 (the anticipated rate during a standard conflict is about 30 %) [7]. The treatment of those patients only required 48 hours. Some of them were operated upon more than 20 hours after wounding, when they should have been treated within six hours according to the category. The perioperative mortality rate was high (22 %).
In the Red Cross classification, the priority seems to be given to abdominal wounds [8, 9]. In the NATO classification stable patients with abdominal wounds seem to be treated after the major limbs wounds. In our experience the abdominal wounds were treated before the limbs wounds. But in Rwanda some patients with major limbs wounds died before surgery. We believe that some of them should have been operated upon before the patients with abdominal wounds. The large mortality in patients suffering from upper extremity major injury is probably due to associated pulmonary blast with pulmonary and/or myocardial contusion. Some patients died while waiting for surgery and some others after surgery. One can wonder whether triage was judicious. If we had operated earlier on those who died before surgery or if we had decided not to operate on some of those who died after surgery, maybe we could have saved one or two more wounded.
We would like to highlight three points: logistic, medical and ethics. In the ICRC hospitals it is generally agreed that triage is declared when seven (or more) patients arrive simultaneously [8]. For an FSU as soon as the number of casualties exceeds ten wounded, triage becomes very difficult to organise. To identify the civilian casualties without ID is very hard. The translator’s role is very important. Operating records should also be classified in real time. Every team member should know in advance his proper place and task during a mass casualty situation. The decisions of the triage officer must be accepted without discussion. During conflict involving a civilian population, secondary evacuation is usually impossible. We would like to underline a very important point. Without evacuation triage and treatment can be different and surgical procedures must allow for simple postoperative monitoring.
There are a variety of defined triage systems used. It is inherently difficult to investigate and compare disaster protocols by using an evidence-based approach [10]. There is no definitive data on which disaster triage technique would save the largest number of victims. Each organisation has its own variation. In every system three main categories are proposed—first, patients to operate upon; second, patients not to operate upon because they do not need surgical treatment; and third, patients not to operate upon because they are too seriously injured and they are unlikely to survive. The important points are that the categorisation should be perfectly understood by every member of the team and members of the team should be regularly taught and trained about the classification used.
Triage is a medical task that requires moral responsibility. The triage officer needs internal stability and external authority [11, 12]. In the past he was the most experienced surgeon. Nowadays the triage officer is the anaesthetist–intensivist [13]. However, we must consider that both are complementary. The surgeon probably better evaluates the length of the surgical procedure. The anaesthetist–intensivist has a better expertise in resuscitation. Application of effective and accurate triage is a team-based multidisciplinary activity.
These three aspects of triage bring us to a discussion of two key ethical problems, i.e. the notion of expectant and the neutrality of the choice. It is very hard to think of “expectant”, whereby two types of wounded may be classified into this category. The first variety is not difficult to classify as they are the extremely wounded patients. However, it is very hard to classify the second group, which comprises patients who might be saved after prolonged surgical treatment and major resuscitation.
Could we sort patients using only medical criteria? According to Dominique Larrey [1] and the Geneva convention [14] one should triage regardless of nationality, race, sex, religion, rank, etc. The only criteria used for triage should be the medical status. A classification using criteria other than medical principles is a violation of human rights [11]. However, wounded children in a war mass casualties situation are uncommon for military teams. For civilian patients in the same category we believe that priority must be given to children, because they are weaker. If we sort children we could classify some of them as “expectant”. But such a decision seems to be very difficult, or even impossible. However because of the high postoperative mortality of children with abdominal wounds and associated lesions we think that some of them should have been classified “expectant”. It is absolutely necessary that each member of the medical team thinks about this particular category beforehand.
Conclusion
For the majority of surgeons, triage is an abstract concept. They never have to use it in their daily practice. Triage in war or disaster conditions is a complex process with no direct civilian medical equivalent. Each medical unit must be prepared to participate in a realistic triage practice.
Theoretically the medical team of a forward surgical team knows the principles of the triage. However, we have been surprised by the number of casualties and the resulting logistics problems, by the issues of prioritisation, by the presence of a large number of children and by the issue of when to apply the expectant category.
Battlefield surgery, because it sometimes deals with mass wounded, requires a replacement of “individual ethics” with the ethics of doing “the greatest good for the greatest number” [4].
Acknowledgments
Conflict of interest
The authors declare that they have no conflict of interest.
The views expressed are solely those the authors and do not necessary reflect the official policy or position of the French army medical service.
References
- 1.Larrey DJ (1984) Mémoires et campagnes du baron Larrey. Campagnes de Saxe et de Prusse. Première réédition, Remanences Editions, Paris, p 4
- 2.Blair JSG. Famous figures: James Dominique, First Baron Larrey. J R Army Med Corps. 2005;151:207–208. doi: 10.1136/jramc-151-03-13. [DOI] [PubMed] [Google Scholar]
- 3.Morris JA, Jr, Auerbach PS, Marshall GA, et al. The trauma score as a triage tool in the prehospital setting. JAMA. 1986;256(10):319–325. doi: 10.1001/jama.1986.03380100093027. [DOI] [PubMed] [Google Scholar]
- 4.Burris DG, Fitz-Harris JB, Holcomb JB, et al. Emergency war surgery. Washington DC: US Government Printing Office; 2004. [Google Scholar]
- 5.Giannou C, Baldan M (2009) War surgery working with limited resources in armed conflict and other situations of violence, vol 1, chap 9. Hospital triage of mass casualties. International Committee of the Red Cross, March 2009
- 6.Burkle FM, Jr, Newland C, Orebaugh S, Blood CG. Emergency medicine in the Persian Gulf War-Part 2. Triage : methodology and lessons learned. Ann Emerg Med. 1994;23(4):748–754. doi: 10.1016/S0196-0644(94)70310-8. [DOI] [PubMed] [Google Scholar]
- 7.Houdelette P. Le triage de blessés de guerre en chirurgie de guerre et en situation d’exception. J Chir (Paris) 1996;133(8):363–712. [PubMed] [Google Scholar]
- 8.Coupland RM, Parker PJ, Gray RC. Triage of war wounded: the experience of the International Committee of the Red Cross. Injury. 1992;23(8):507–510. doi: 10.1016/0020-1383(92)90146-J. [DOI] [PubMed] [Google Scholar]
- 9.Coupland RM. Epidemiological approach to surgical management of the casualties of war. BMJ. 1994;308(6945):1693–1697. doi: 10.1136/bmj.308.6945.1693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Cone DC, Serra J, Burns K, MacMillan DS, Kurland L, Van Gelder C. Pilot test of the SALT Mass Casualty Triage System. Prehosp Emerg Care. 2009;13(4):536–540. doi: 10.1080/10903120802706252. [DOI] [PubMed] [Google Scholar]
- 11.Domres B, Koch M, Manger A, Becker HD. Ethics and triage. Prehosp Disaster Med. 2001;16(1):53–58. doi: 10.1017/s1049023x00025590. [DOI] [PubMed] [Google Scholar]
- 12.Frykberg ER. Triage: principles and practice. Scand J Surg. 2005;94:272–278. doi: 10.1177/145749690509400405. [DOI] [PubMed] [Google Scholar]
- 13.Adu-Gyamfi Y. The Gulf War: the experience of a department of anesthesiology in the management of Scud missile casualties. Prehosp Disaster Med. 1997;12(2):109–113. [PubMed] [Google Scholar]
- 14.International Red Cross (1995) Convention (IV) Relative to the Protection of Civilian Persons in Time of War. Geneva, 12 August 1949. Part II. General protection of populations against certain consequences of war. Art. 13. International Humanitarian Law—Treaties & Documents. International Committee of the Red Cross, Geneva, ref 0173, p 245