Abstract
Purpose
Fractures of the pubic rami due to low energy trauma are common in the elderly, with an incidence of 26 per 100,000 people per year in those aged more than 60 years. The purpose of this study was to evaluate the clinical application of this minimally invasive technique in patients with pubic ramus fractures combined with a sacroiliac joint complex injury, including its feasibility, merits, and limitations.
Methods
Fifteen patients with pubic ramus fractures combined with sacroiliac joint injury were treated with the minimally invasive technique from June 2008 until April 2012. The quality of fracture reduction was evaluated according to the Matta standard.
Results
Fourteen cases were excellent (93.3 %), and one case was good (6.7 %). The fracture lines were healed 12 weeks after the surgery. The 15 patients had follow-up visits between four to 50 months (mean, 22.47 months). All patients returned to their pre-injury jobs and lifestyles. One patient suffered a deep vein thrombosis during the peri-operative period. A filter was placed in the patient before the surgery and was removed six weeks later. There was no thrombus found at the follow-up visits of this patient.
Conclusion
The minimally invasive technique in patients with pubic ramus fractures combined with a sacroiliac joint complex injury provided satisfactory efficacy.
Introduction
Fractures of the pubic rami due to low energy trauma are common in the elderly, with an incidence of 26 per 100,000 people per year in those aged more than 60 years [1, 2]. Pubic ramus fractures combined with a sacroiliac joint complex injury is a pelvic fracture, its incidence is increasing due to the development of civilization and transportation [3]. Because pubic ramus fractures combined with a sacroiliac joint complex injury involves both anterior and posterior rings and is usually caused by pelvic crush injuries, it is an unstable pelvic fracture [4], and surgical fixation is often required to treat this type of injury [5].
Common methods used to treat this type of pelvic fracture involving an unstable or partially unstable posterior ring include long cancellous bone screw fixation, plate internal fixation, and external fixator fixation to reset and stabilize the anterior ring [6, 7]. Some clinicians use the screw-rod system and one or two cancellous bone screw fixations to treat sacroiliac joint injuries [8–10]. We tried to improve the fixation methods to reduce patients’ trauma from surgery while obtaining a satisfactory fixation. We used the minimally invasive plate osteosynthesis (MIPO) technique [11] to treat anterior ring fracture (pubic ramus fracture), and posterior ring injury (sacroiliac joint fracture or dislocation) was treated either with or without single-screw percutaneous fixation. The purpose of this study was to evaluate the clinical application of this minimally invasive technique in patients with pubic ramus fractures combined with a sacroiliac joint complex injury, including its feasibility, merits, and limitations.
Materials and methods
Patients
Fifteen patients with pubic ramus fractures combined with a sacroiliac joint injury were treated with the minimally invasive technique from June 2008 until April 2012 in our hospital. Patients who were not suitable for the surgery within three weeks after the date of their injuries were excluded. The patients included nine men and six women who ranged in age from 17 to 58 years. The average age of the patients was 36.2 years. The causes of injury included eight traffic accidents, five falls, one crush injury, and one injury by a heavy falling object. The types of associated injuries included one chest injury, two urinary tract injuries, six upper limb fractures, two lower extremity fractures, one lumbar fracture, and two acetabular fractures. There were 13 cases of unilateral pubic ramus fracture combined with a sacroiliac joint complex injury, and two cases of bilateral pubic ramus fracture combined with a sacroiliac joint complex injury. According to the Tile classification system [12], there were ten B-type cases, including two B1.1-type cases (both combined with ipsilateral acetabular fracture), one B1.2-type case, four B2.1-type cases, one B2.2-type case, and two B2.3-type cases. There were five cases of the C type, including one C1.2-type case and four C1.3-type cases (Table 1). The institutional review board approved the study protocol, and all patients provided written informed consent.
Table 1.
The patients’ characteristics
| Gender | Age (years) | Type of pelvic fracture | Mechanism of injury | Concomitant Injuries | Perioperative anticoagulation | Time from injury to surgery (days) | Surgical manoeuver | Duration of unilateral MIPO | Duration of sacral screw fixation | Blood loss (ml) | Blood transfusion (ml) | Autologous transfusion (ml) | Reduction for fracture |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Men | 58 | B2.3 | Fall injury | Fracture of the distal segment of the left humerus | No | 10 | MIPO | 45 | – | 150 | 400 | 50 | Excellent |
| Women | 25 | B1.1 | Traffic injury | Left anterior column acetabular fracture | No | 13 | MIPO + sacral screw fixation | 80 | 15 | 160 | 400 | 150 | Excellent |
| Women | 27 | B2.2 | Traffic injury | No | No | 15 | MIPO + sacral screw fixation | 56 | 14 | 160 | 0 | 50 | Excellent |
| Men | 49 | C1.3 | Traffic injury | Left ulna fracture | No | 6 | MIPO + sacral screw fixation | 92 | 18 | 200 | 0 | 121 | Excellent |
| Men | 38 | B2.3 | Traffic injury | No | No | 7 | MIPO + sacral screw fixation | 41 | 9 | 200 | 0 | 100 | Excellent |
| Women | 17 | C1.2 | Fall injury | No | No | 10 | Double MIPO + sacral screw fixation | 78 | 14 | 160 | 400 | 100 | Fair |
| Women | 24 | C1.3 | Traffic injury | No | No | 13 | Double MIPO + sacral screw fixation | 92 | 21 | 170 | 0 | 150 | Excellent |
| Men | 58 | C1.3 | Fall injury | L1 compression fracture and Right olecranon fracture | No | 4 | MIPO + sacral screw fixation | 80 | 15 | 200 | 0 | 80 | Excellent |
| Men | 31 | B1.1 | Traffic injury | Incomplete transverse fracture of the left acetabulum | Yes | 4 | MIPO + sacral screw fixation | 77 | 8 | 220 | 0 | 120 | Excellent |
| Women | 36 | B1.2 | Traffic injury | Left humerus fracture Multiple rib fractures | No | 20 | MIPO + sacral screw fixation | 102 | 23 | 190 | 0 | 78 | Excellent |
| Men | 46 | C1.3 | Fall injury | Calcaneal fractures (both left and right), right distal radius fracture, and urinary tract injury | No | 7 | MIPO + sacral screw fixation | 60 | 15 | 160 | 0 | 0 | Excellent |
| Men | 26 | B2.1 | Fall injury | Right intertrochanteric fracture, right radius fractures, and urinary tract injury | No | 6 | MIPO | 45 | – | 200 | 1000 | 0 | Excellent |
| Men | 32 | B2.1 | Crush injury | No | No | 5 | MIPO + sacral screw fixation | 56 | 14 | 170 | 0 | 70 | Excellent |
| Women | 41 | B2.1 | Traffic injury | No | No | 4 | MIPO + sacral screw fixation | 48 | 12 | 180 | 0 | 0 | Excellent |
| Men | 35 | B2.1 | Heavy objects falling | No | No | 6 | MIPO | 65 | – | 90 | 0 | 0 | Excellent |
MIPO minimally invasive plate osteosynthesis
Preoperative assessment
All patients underwent preoperative X-ray (Fig. 1a) and three-dimensional pelvic CT scans (Fig. 1b). The following three characteristics were clarified: (a) whether patients had other pelvic fractures and injuries, such as pubic symphysis separation, pubic fracture near the pubic symphysis, or iliac wing fractures, (b) whether patients had acetabular fractures, since acetabular fractures which could not be stabilized by the MIPO technique were excluded from the study; and (c) understanding of the status of sacroiliac joint complex injuries. The patients who had a large separation of the sacroiliac joint or an associated fracture that could not be satisfactorily fixed by sacral screw after preoperative traction and assessment were excluded from the study.
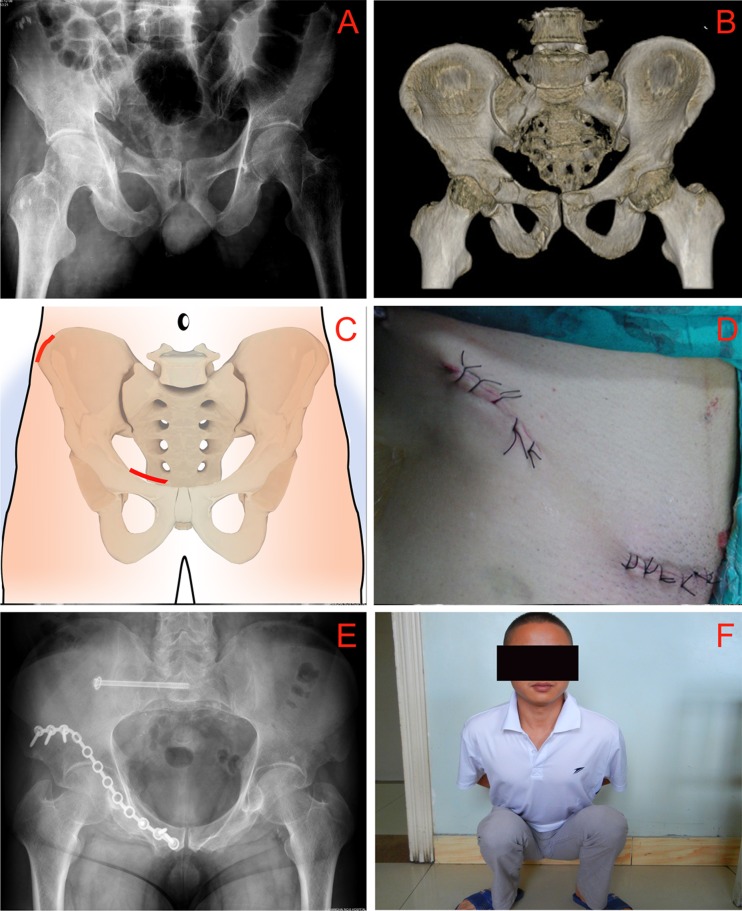
Fig. 1.
Male patient, age 38, with a pelvic B23 fracture caused by a traffic accident. Preoperative X-ray image (a), horizontal CT scanning image (b), surgical incisions of MIPO fixation of pubic ramus fracture (c, d), postoperative pelvic X-ray image (e), and the patient’s functional diagram (f) were performed 24 months after the injury
The patients who met the exclusion criteria described above could not be treated with the MIPO technique combined with sacral screw fixation used in this study, or had to be treated in combination with other fixation methods; therefore, the surgical procedure time and blood loss during surgery could not be accurately estimated. All of the patients underwent ipsilateral bone traction therapy.
Surgical technique
MIPO technique for anterior ring fracture (pubic ramus fracture) fixation
First, anterior pelvic ring fixation was performed with the patients in a supine position. A 5–6-cm incision was made at approximately 2 cm above the pubic ramus along the line from near the pubic symphysis to the pubic ramus (Fig. 1c, d, marked with a thick line in the area of the pubic rami). The incision passed through the skin and subcutaneous fat to reach the external oblique aponeurosis. The edges of the incision were separated by pushing the flesh upward and downward with gauze to expose the pyramidal muscle (i.e., the end of the rectus abdominis muscle) interiorly and the spermatic cord or round ligament exteriorly. The ligaments and periosteum of the superior pubic ramus were exposed by stripping the spermatic cord to the superiomedial side. The pubic rami were exposed by cutting and removing the ligaments on the surface of the pubis along the vertical axis. This exposed area was the inside window of the ilioinguinal approach. Based on the location of the fracture line displayed on the preoperative X-ray image, the pyramidal muscle may have also been partially excised. The associated periosteum and other soft tissues were also stripped. The edges of the incision were separated with retractors to reach the lower edge of the front of the acetabulum. Then, the superior pubic ramus was repositioned with reduction clamps and temporarily fixed with Kirschner needles. The entry position of the needle was selected to avoid the location where the steel plate would be placed.
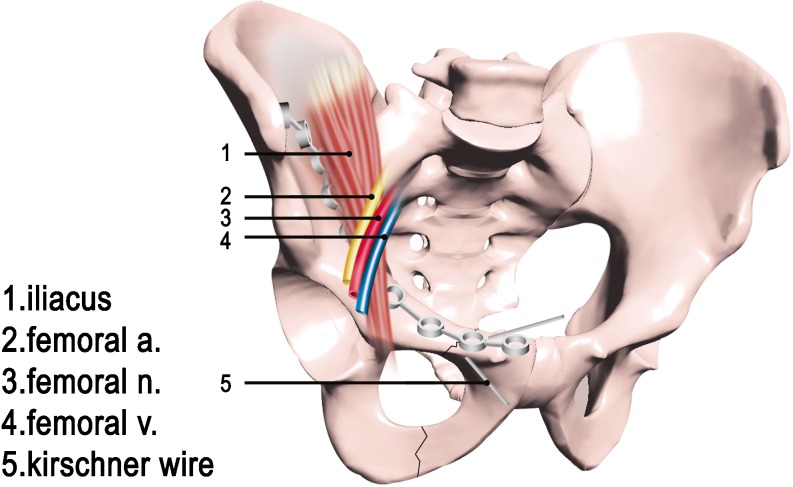
A 4–5-cm incision was made outward, starting from the anterior superior iliac spine along the iliac crest, and the tissues were dissociated from the inner table of the iliac crest (Fig. 2a, the edge area outside of the blue area). A surgical elevator was used to strip along the front edge of the acetabulum toward the superior pubic ramus to form a tunnel. The tunnel was then expanded to allow the steel plate to pass through. During the formation of the tunnel, the critical factor for avoiding vascular damage and unexpected bleeding was to ensure that the surgical elevator was placed underneath the periosteum (Fig. 3).
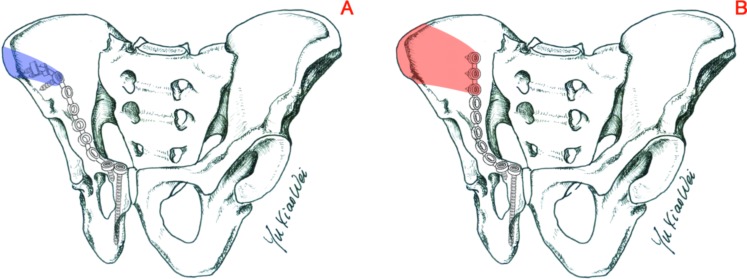
Fig. 2.
Schematic diagrams of minimally invasive plate osteosynthesis (MIPO) fixation of pubic ramus fracture (a) and of traditional steel plate fixation of pubic ramus fracture (b). The blue shaded area represents the exposed area required in the iliac wing in MIPO fixation, and the red shaded area represents the exposed area required in the iliac wing in traditional fixation
Fig. 3.
Diagram for insertion of the shaped steel plate in minimally invasive plate osteosynthesis (MIPO) fixation
After the reposition was satisfactorily confirmed by X-ray, a reconstruction plate with ten to 12 holes (universal reconstruction ribbon, DePuy Orthopaedics, Inc., USA) was shaped and placed through the “tunnel” on top of the pubic rami aligned from the acetabular anterior wall to the bottom of the anterior superior iliac crest, with two or three screws fixated at both ends of the steel plate (Figs. 1e and 2a).
Minimally invasive technique for sacroiliac complex fixation
After the anterior ring was fixed, the pelvis was tested with the squeeze-separation technique. The dynamic activity of the anteroposterior pelvis, pelvic outlet, and pelvic inlet were observed with a C-arm machine to examine whether the sacral joint remained shifted or dislocated. If the sacroiliac joint was restored without a significant displacement, the surgery was complete. If there was a large separation, the decision was made to fix the sacroiliac complex with screws.
The patient remained in a supine position. The sacroiliac joint was reset by traction under the condition of hip flexion. After the repositioning was satisfactorily confirmed, one or two pieces of 2.0-cm Kirschner needles were nailed in the sacrum from the outside of the iliac through the skin for temporary fixation. The depth of the Kirschner needle insertion into the sacrum should not exceed 2 cm to prevent possible nerve damage, but it should be deep enough to maintain the reset status for convenient operation of the sacroiliac screws in the future. The entry point of the guide pin for the sacroiliac screws was determined based on the S1 pedicle morphology from the preoperative CT image. According to the Tile guide, the safe zone of nail placement is the middle position between the two points. After a guide pin was drilled in and the position was satisfactorily confirmed with a C-arm machine, a semi-threaded hollow screw was placed (a 6.5-mm diameter cannulated cancellous screw with a 22-mm thread length, DePuy Orthopaedics, Inc., USA). The requirement for extra pressure on the sacroiliac screw was determined by whether the sacroiliac joint was separated. The location of the screw was further confirmed from the outlet, inlet, and lateral side of the pelvis. When the location of the screw was satisfactorily confirmed, the surgery was complete. For this group of patients, we used single-screw fixation.
Postoperative management
Antibiotics were administered for one to two days following surgery. Patients were not given traction and were allowed to freely move both lower extremities. A drainage tube was placed in the surgical cavity of the anterior pelvic ring. When the draining fluid was less than 20 mL/day, the tube was removed. The patients were allowed to sit two weeks after surgery, to walk with crutches after one month, and to walk normally three months after surgery.
Criteria for evaluation of the quality of fracture reduction
The quality of fracture reduction was evaluated according to the Matta standard [7] and described as follows: if the maximal distance of anteroposterior fracture displacement is less than 4 mm at the pelvic inlet and outlet, the quality is considered to be excellent; if the distance is 5–10 mm, the quality is good; if the distance is 11–20 mm, the quality is fair; and if the distance is more than 20 mm, the quality is poor.
Results
Patient characteristics
Among the 13 cases of unilateral pubic ramus fractures combined with a sacroiliac joint complex injury, three cases required only pubic ramus MIPO fixation, whereas ten patients underwent pubic ramus fixation combined with minimally invasive sacroiliac screw fixation. In the two cases of bilateral pubic ramus fracture combined with a sacroiliac complex injury, the patients underwent bilateral pubic ramus MIPO fixation combined with screw fixation on the unstable side of the sacroiliac joint.
The procedure times for pubic ramus MIPO fixation ranged from 41 to 102 min/side with an average of 67.8 min/side. The mean intraoperative blood loss was 174 mL/side (range, 90–220 ml/side). The mean procedure time for sacroiliac screw fixation was 14.83 min/side (range, 8–23 min/side). Because the fixation was a percutaneous procedure, the intraoperative blood loss was negligible.
There were only four patients who needed blood transfusion during the surgery. One of the patients suffered a right radial fracture and right femoral neck fracture; therefore, this patient underwent internal fixation for these two fractures in addition to the pelvic fixation during the surgery. This patient received 1,000 ml of non-autologous blood during the surgery. The other three patients each received blood transfusions of 400 ml.
No iatrogenic nerve injury occurred in this patient group, and no postoperative wound infections at the anterior pelvic ring occurred in these patients, including the patient with urinary tract injuries.
Status of fracture healing
The quality of fracture reduction of the 15 patients was evaluated according to the Matta criteria [7]. Fourteen cases were excellent (93.3 %), and one case was good (6.7 %). The fracture lines were healed 12 weeks after the surgery.
Functional evaluation
The 15 patients had follow-up visits for between four to 50 months (mean, 22.47 months). All patients returned to their pre-injury jobs and lifestyles. One patient suffered deep vein thrombosis during the peri-operative period. A filter was placed in the patient before the surgery and was removed six weeks later. There was no thrombus found at the follow-up visits of this patient. The internal fixation was removed from one female patient upon request because of her concern for impaired sexual activity and fertility. The sacroiliac screws were removed from one patient with sacrococcygeal complaints; however, the steel plate remained in the patient. The internal fixations remained in the rest of the patients.
Discussion
When the pelvis encounters violent forces that fracture both the anterior and posterior pelvic rings, pelvic instability and fracture shifts will occur [13]. This type of injury is a high-energy injury, which usually causes hemodynamic disorders and other injuries, such as visceral injury and nerve injury [5]. Delayed fixation of the pubic fracture combined with an unstable or partially unstable posterior pelvic ring will aggravate the primary injuries and will detrimentally affect patient care [14]. Therefore, pelvic stability should be restored as early as the patient’s condition allows [15].
The degree of fixation intensity needed to mechanically stabilize a fractured pelvis has been the focus of domestic and international researchers’ discussion. The approaches for fixing the anterior pelvic ring (pubic ramus fracture) include cancellous bone screw fixation, steel plate fixation, built-in external fixator fixation, and external fixator fixation. It is generally accepted that steel plate fixation provides better stability than do other fixation approaches, and it is considered a better fixation method. In traditional anterior ring plate fixation, one end of the steel plate is fixated to the pubic ramus on one side of pubic symphysis, and the other end of the plate is fixated to the arcuate line. We improved the technique of this type of steel plate fixation. We first moved the end of the steel plate which is fixated to the medial border of the pelvis (outside of the arcuate line) to the iliac wing (below the anterior superior iliac spine); thus, we only need 2 or 3 screws to fix the steel plate to both ends of the fracture to obtain a satisfactory fixation. We used a single piece of cancellous bone screw instead of two pieces for the posterior ring injury (sacroiliac joint). All of these improvements contributed to a certain degree of decreased stability of the fixation system. However, we did not observe fracture shift or nonunion in any of the patients based on the analysis of postoperative radiographs and fracture healing assessments at the patients’ follow-up clinical visits. Therefore, we believe that the effective stability of our improved approach sufficiently meets the requirements for postoperative care and patient recovery.
Considering the surgical trauma, we believe that the second guiding principle for treating this type of injury should be keeping the surgery fast and minimally invasive to avoid secondary damage from the surgery. Traditional steel plate fixation of the anterior ring and two-screw fixation of the sacroiliac joint certainly have mechanical advantages; however, unstable pelvic fractures are frequently accompanied by hemodynamic disorders and other complications. Among clinical cases of pubic ramus fracture combined with sacroiliac joint injury in our study, 40 % of patients (6/15) suffered other associated injuries, including one patient who had deep vein thrombosis during the peri-operative period. Therefore, the treatment strategy for this type of injury should be different from the treatment for acetabular fractures, which usually require an anatomical reduction and a strong fixation. Notably, in the two cases with combined acetabular fractures in this study, because the fracture occurred at the anterior column, the MIPO technique used in this study repaired the pubic ramus fracture and simultaneously provided strong fixation for the acetabular fracture. We modified the fixation position of the steel plate on the iliac side (Fig. 2a), which greatly reduced the exposed area required for surgery (Fig. 2a, blue shaded area) compared with that required by traditional fixation (Fig. 2b, red shaded area). The modification described above greatly decreased the trauma and procedure time of the surgery and simplified the surgical procedure. The mean procedure time (67.8 min) and intraoperative blood loss (174 ml) associated with the minimally invasive technique for pelvic fixation used in our study were significantly less than those reported in the literature. We believe that the reduced intraoperative blood loss was attributed to the reduction in operative trauma resulting from our modifications of the MIPO technique. Only four patients required blood transfusion during surgery. In addition, we used an autotransfusion of red blood cells during surgery. We believe that autotransfusion was not the major factor because three out of the 15 patients did not need the autotransfusion procedure.
To reduce and prevent fracture-induced complications, we first used the percutaneous technique for fixing the steel plate to improve the anterior ring (pubic rami) fixation. Our method differs from the reported method [16]. We first stripped the blood vessels and nerves underneath the pubic ramus periosteum and then placed the steel plate through the tunnel (Fig. 3). The inferior epigastric artery and the communication branch of the obturator artery often pass along the pectineal ligament behind the supra-pubic branch which was 6 cm away from the pubic symphysis. This communication branch is close to the pubic rami and therefore is easily injured during surgery. During the surgical procedures, subperiosteal dissection may avoid injury of this communication branch. In our series, no such injury was noted. Therefore, this approach could greatly reduce damage to the blood vessels and nerves. According to the reported method [16], a steel plate was placed subcutaneously and on top of blood vessels. Although this method could also reduce secondary damage to the blood vessels and nerves, it causes the patient discomfort because the steel plate is placed directly under the skin and is palpable (although in the report, they did not receive such complaints from patients); therefore, the authors also believed that the steel plate should be removed after a relatively short period. Moreover, in this fixation method, the steel plate is not tightly attached to the fracture, and the force arm is large; therefore, the fixation is unstable, and there is the possibility of micro-movement in the fracture, which affects fracture healing [17–21]. We treated the 15 patients with pubic ramus MIPO fixation, and with one exception, all of the patients denied discomfort and lived a normal life. One female patient had the steel plate removed due to her concern about the effects of the steel plate on her sexual activities and fertility. Furthermore, there was no surgery-associated complication of blood vessel and nerve damage. Follow-up visits demonstrated that the fractures healed in a short time (12 weeks) in all of the cases, thereby confirming that this method is safe and reliable.
To reduce and prevent fracture-induced complications, we used single-screw fixation (which has been reported) to treat posterior ring injuries (sacroiliac joint complex). Compared with two-screw fixation, this posterior sacroiliac joint fixation technique greatly reduced surgery-associated trauma. It is safer to use a single screw in the safe zone of the upper posterior sacrum, although the safe zone can accommodate a two-sacroiliac screw fixation. The two-screw fixation method demands good technical skills from surgeons and requires continuous fluoroscopy, which increases the exposure time to X-rays for both surgeons and patients; in addition, the procedure time is greatly increased. We used single-screw fixation to reduce 50 % of the exposure time for fluoroscopy, and the screw could be directly placed. The single-screw fixation procedure could usually be finished within 10 minutes. The blood loss from this procedure was negligible. Upon follow-up, there was no radiographic abnormality in the sacroiliac joint complex or screw displacement in any of the patients.
In summary, the minimally invasive technique in patients with pubic ramus fractures combined with a sacroiliac joint complex injury provided satisfactory efficacy. However, the shortcoming of this study is that we used an analysis based on clinical cases to predict the stability of fixation methods. It is an indirect deduction and lacks direct support from biomechanical data. Moreover, our patients were told to gradually bear weight one to three months after surgery. It remains unknown whether this minimally invasive technique could provide patients with earlier ambulatory stability.
Acknowledgments
Conflict of interest
All authors declare that there are no conflicts of interest.
Footnotes
Xiaowei Yu and Mingjie Tang contributed equally to this study.
References
- 1.Hill RM, Robinson CM, Keating JF. Fractures of the pubic rami. Epidemiology and five-year survival. J Bone Joint Surg Br. 2011;83(8):1141–1144. doi: 10.1302/0301-620X.83B8.11709. [DOI] [PubMed] [Google Scholar]
- 2.Scheyerer MJ, Osterhoff G, Wehrle S, Wanner GA, Simmen HP, Werner CM. Detection of posterior pelvic injuries in fractures of the pubic rami. Injury. 2012;43(8):1326–1329. doi: 10.1016/j.injury.2012.05.016. [DOI] [PubMed] [Google Scholar]
- 3.Gao H, Luo CF, Hu CF, Zhang CQ, Zeng BF. Minimally invasive fluoro-navigation screw fixation for the treatment of pelvic ring injuries. Surg Innov. 2011;18(3):279–284. doi: 10.1177/1553350611399587. [DOI] [PubMed] [Google Scholar]
- 4.Starr AJ, Walter JC, Harris RW, Reinert CM, Jones AL. Percutaneous screw fixation of fractures of the iliac wing and fracture-dislocations of the sacro-iliac joint (OTA types 61-B2.2 and 61-B2.3, or Young-Burgess “lateral compression type II” pelvic fractures) J Orthop Trauma. 2002;16(2):116–123. doi: 10.1097/00005131-200202000-00008. [DOI] [PubMed] [Google Scholar]
- 5.Nicodemo A, Decaroli D, Pallavicini J, Sivieri R, Aprato A, Massè A. A treatment protocol for abdomino-pelvic injuries. J Orthop Traumatol. 2008;9(2):89–95. doi: 10.1007/s10195-008-0003-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ghanayem AJ, Wilber JH, Lieberman JM, Motta AO. The effect of laparotomy and external fixator stabilization on pelvic volume in an unstable pelvic injury. J Trauma. 1995;38(3):396–400. doi: 10.1097/00005373-199503000-00020. [DOI] [PubMed] [Google Scholar]
- 7.Matta JM. Indications for anterior fixation of pelvic fractures. Clin Orthop Relat Res. 1996;329:88–96. doi: 10.1097/00003086-199608000-00011. [DOI] [PubMed] [Google Scholar]
- 8.Shuler TE, Boone DC, Gruen GS, Peitzman AB. Percutaneous iliosacral screw fixation: early treatment for unstable posterior pelvic ring disruptions. J Trauma. 1995;38(3):453–458. doi: 10.1097/00005373-199503000-00031. [DOI] [PubMed] [Google Scholar]
- 9.Templeman DC, Simpson T, Matta JM. Surgical management of pelvic ring injuries. Instr Course Lect. 2005;54:395–400. [PubMed] [Google Scholar]
- 10.Vaidya R, Colen R, Vigdorchik J, Tonnos F, Sethi A. Treatment of unstable pelvic ring injuries with an internal anterior fixator and posterior fixation: initial clinical series. J Orthop Trauma. 2012;26(1):1–8. doi: 10.1097/BOT.0b013e318233b8a7. [DOI] [PubMed] [Google Scholar]
- 11.Gökay NS, Bagatur AE. The results of minimally invasive percutaneous plate osteosynthesis (MIPPO) in distal and diaphyseal tibial fractures. Acta Orthop Traumatol Turc. 2012;46(4):243–249. doi: 10.3944/AOTT.2012.2836. [DOI] [PubMed] [Google Scholar]
- 12.Adams JE, Davis GG, Heidepriem RW, 3rd, Alonso JE, Alexander CB. Analysis of the incidence of pelvic trauma in fatal automobile accidents. Am J Forensic Med Pathol. 2002;23(2):132–136. doi: 10.1097/00000433-200206000-00004. [DOI] [PubMed] [Google Scholar]
- 13.Gabbe BJ, de Steiger R, Esser M, Bucknill A, Russ MK, Cameron PA. Predictors of mortality following severe pelvic ring fracture: results of a population-based study. Injury. 2011;42(10):985–991. doi: 10.1016/j.injury.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 14.Biffl WL, Smith WR, Moore EE, Gonzalez RJ, Morgan SJ, Hennessey T, Offner PJ, Ray CE, Jr, Franciose RJ, Burch JM. Evolution of a multidisciplinary clinical pathway for the management of unstable patients with pelvic fractures. Ann Surg. 2001;233(6):843–850. doi: 10.1097/00000658-200106000-00015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gruen GS, Leit ME, Gruen RJ, Peitzman AB. The acute management of hemodynamically unstable multiple trauma patients with pelvic ring fractures. J Trauma. 1994;36(5):706–711. doi: 10.1097/00005373-199405000-00019. [DOI] [PubMed] [Google Scholar]
- 16.Hiesterman TG, Hill BW, Cole PA. Surgical technique: a percutaneous method of subcutaneous fixation for the anterior pelvic ring: the pelvic bridge. Clin Orthop Relat Res. 2012;470(8):2116–2123. doi: 10.1007/s11999-012-2341-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Tosounidis T, Kanakaris N, Nikolaou V, Tan B, Giannoudis PV. Assessment of lateral compression type 1 pelvic ring injuries by intraoperative manipulation: which fracture pattern is unstable? Int Orthop. 2012;36(12):2553–2558. doi: 10.1007/s00264-012-1685-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kobbe P, Hockertz I, Sellei RM, Reilmann H, Hockertz T. Minimally invasive stabilisation of posterior pelvic-ring instabilities with a transiliac locked compression plate. Int Orthop. 2012;36(1):159–164. doi: 10.1007/s00264-011-1279-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Karadimas EJ, Nicolson T, Kakagia DD, Matthews SJ, Richards PJ, Giannoudis PV. Angiographic embolisation of pelvic ring injuries. Treatment algorithm and review of the literature. Int Orthop. 2011;35(9):1381–1390. doi: 10.1007/s00264-011-1271-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Hao T, Changwei Y, Qiulin Z. Treatment of posterior pelvic ring injuries with minimally invasive percutaneous plate osteosynthesis. Int Orthop. 2009;33(5):1435–1439. doi: 10.1007/s00264-009-0756-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Papakostidis C, Kanakaris NK, Kontakis G, Giannoudis PV. Pelvic ring disruptions: treatment modalities and analysis of outcomes. Int Orthop. 2009;33(2):329–338. doi: 10.1007/s00264-008-0555-6. [DOI] [PMC free article] [PubMed] [Google Scholar]