Abstract
Purpose
This study was conducted to examine the risk factors for recurrent dislocation after total hip arthroplasty (THA) and test the hypothesis that late dislocations are associated with recurrence.
Methods
A total of 1,250 hips in 1,017 patients were retrospectively reviewed. All operations were performed through the posterolateral approach with posterior soft tissue repair. An early or late dislocation was defined as a dislocation occurring before or after one year postoperatively, respectively.
Results
Dislocation occurred in 36 hips (2.9 %) and 20 of them experienced recurrence. Recurrent dislocations were observed in ten out of 25 hips (40.0 %) with early dislocation; however, ten out of 11 hips (90.9 %) with late dislocation experienced recurrence (p = 0.0046). Multivariate analysis revealed that late dislocation was significantly associated with recurrence with odds ratio of 5.94 per year. Seven in 20 hips with recurrent dislocation required surgical treatment.
Conclusion
Late dislocation significantly contributed to the development of recurrent dislocations.
Introduction
Dislocation is one of the most frequent complications after total hip arthroplasty (THA) with an incidence from 1 % to 9 % [1–6]. Reported risk factors for dislocation include patient variables such as age, sex, avascular necrosis of the femoral head, inflammatory arthritis, and previous revision; surgery-related factors such as the posterior approach and implant malposition; and implant-related factors such as head size and modularity [4, 6–9]. The majority of dislocations can be managed conservatively; however, multiple dislocations cause substantial disability in the daily life of patients and frequently need surgical interventions. Instability or dislocation was reported to be the most common cause of revision surgery in the United States in 2005 and 2006 [10].
Dislocation is likely to occur early in the first few postoperative months. More than half of dislocations have been shown to occur by 12 months after surgery [11]; however, as implants are expected to survive for a longer period of time, an increase in the frequency of late dislocations is a growing concern. Woo and Morrey have shown that the dislocation rate after five years was 0.19 % in 1982, but increased to 0.84 % by 2002 in the same group of patients [2, 12]. They also reported that patients with later dislocation tended to require surgical management.
In our study, we tested the hypothesis that late dislocation is more likely to be associated with recurrent dislocation and examined the risk factors for recurrent dislocation in more than 1,000 patients from various backgrounds.
Materials and methods
Patients
This study was approved by the institutional review board. Between 1998 and 2011, a total of 1,283 hips in 1,050 patients underwent THA including revision THA. Among them, ten hips in ten patients were excluded from this study because of death unrelated to THA. Twenty-three hips in 23 patients were excluded as they were lost to follow-up within one year. The remaining 1,250 hips in 1,017 patients were included in this study (Table 1). The mean patient age at surgery was 63.1 years old and the mean duration of follow-up was 56.1 months. The details of indications for THA are shown in Table 1. The hips that underwent revision were classified as revision regardless of the primary diagnosis. Prior to THA, 88 hips had corrective osteotomy such as proximal valgus osteotomy or periacetabular osteotomy.
Table 1.
Patient characteristics
| Characteristic | Value, mean ± SD (range) | |
|---|---|---|
| Age at THA (years old) | 63.1 ± 11.0 (16–92) | |
| Height (cm) | 152.5 ± 8.39 (124–180) | |
| Body weight (kg) | 55.0 ± 10.9 (27.5–100) | |
| BMI (kg/m2) | 23.5 ± 3.71 (14.1–45.2) | |
| Follow-up period (months) | 56.1 ± 39.6 (12–162) | |
| Gender (hips) | Male | 218 |
| Female | 1032 | |
| Diagnosis (hips) | OA | 944 |
| RA | 49 | |
| ONFH | 99 | |
| Revision | 158 | |
THA total hip arthroplasty, SD standard deviation, BMI body mass index, OA osteoarthritis, RA rheumatoid arthritis, ONFH idiopathic osteonecrosis of femoral head
All THAs were performed using the posterolateral approach and a posterior soft tissue repair was performed according to the methods by Pellicci et al. [5]. All patients were followed prospectively. Visits were scheduled to our clinic for examination two months, six months, and one year after THA and yearly thereafter. When patients could not visit the clinic, they were called and asked about the presence or absence of dislocation.
Implants
Two cementless stems, PerFix or PerFix-910 (Kyocera, Osaka, Japan), were mainly used. PerFix-910 stem has a thinner neck diameter and a greater head–neck ratio (HNR) compared to PerFix. When a 32-mm head was used, HNR of PerFix and PerFix-910 were 2.6 and 3.0, respectively. PerFix stem was used in 360 hips by the year 2004 including 40 hips for revision, and PerFix-910 was used in 753 hips thereafter including 21 hips for revision. Versys cementless stem (Zimmer, Warsaw, IN) was used in 35 hips. Various other stems were used in a small number hips, including SROM (Depuy, Warsaw, IN) in 12 hips and Cannulock (Nakashima Medical, Okayama, Japan) in five hips, etc. Cementless acetabular cups were used in all primary THA including AMS cup (Kyocera) in 1,057 hips and TM cup (Zimmer) in 35 hips. Various cups were also used for the revision THA including AMS cup in 30 hips, Duraloc (Depuy) in seven hips, Trilogy (Zimmer) in 22 hips, etc.
Head size was changed depending on the periods and cup size; 22 mm in 208 hips, 26 mm in 812 hips, 28 mm in 43 hips, and 32 mm in 187 hips. All the polyethylene liners used had the elevated portion of 15 degrees.
Radiographic assessment
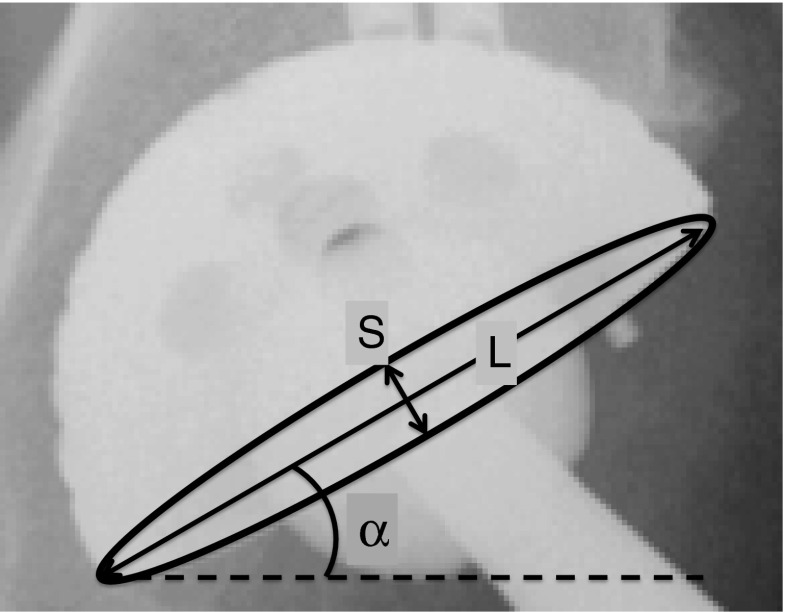
The cup inclination was measured as an abduction angle using the interteardrop line as the baseline. The cup anteversion was calculated using trigonometric function from anteroposterior radiographs following the method of McLaren et al. [13]. Briefly, the length of the major axis of the ellipse was defined as “L”, the minor axis was defined as “S”, and the anteversion was calculated as arcsine (S/L) (Fig. 1).
Fig. 1.
Measurement of cup inclination and anteversion. Using anteroposterior radiographs, the cup inclination is represented as α. The cup anteversion is calculated as arcsine (S/L). L length of the major ellipse axis, S length of the minor ellipse axis
Statistical Analyses
Examined factors that can influence dislocation included age, gender, BMI, indication of THA, direction of dislocation, timing of dislocation, neck geometry, and cup position (inclination and anteversion). A statistical analysis was performed for risk factors associated with hip dislocation using a univariate analysis and multivariate analysis (multivariable logistic regression) using JMP 8.0 software (SAS Institute, Cary, NC). In univariate analysis, qualitative data were compared using the χ2 test and quantitative data were compared with the Pearson test. In neck geometry, only PerFix and PerFix-910 were compared as there was a small number of other type stems used. For the same reason, the 28-mm diameter of the femoral head was omitted. In the multivariate analysis, the odds ratio and P values are presented. P values less than 0.05 were considered statistically significant.
Results
Overall incidence of dislocation and risk factors
Dislocation occurred in 36 hips (2.9 %). The mean time to dislocation after THA was 13.6 months (range, 0–78 months); within one year in 25 hips (69.4 %) and more than one year in 11 hips (30.5 %). The univariate analysis indicated four significant risk factors for dislocation; gender, primary diagnosis, neck geometry, and cup abduction angle. The incidence of dislocation in male was significantly higher than in females (5.5 % versus 2.3 %, p = 0.0109) (Table 2). Primary THA for OA resulted in a significantly lower incidence of dislocation; 1.2 % for OA, 8.2 % for RA, 9.1 % for ONFH, and 7.6 % for revision (P < 0.001). The use of PerFix-910 neck resulted in a significantly lower incidence of dislocation than PerFix (1.7 % versus 4.4 %, P = 0.0077). The average cup abduction in dislocated hips was significantly greater than that without dislocation (43.5° versus 40.6°, P = 0.0060). A multivariate analysis demonstrated that the primary diagnosis (P < 0.001), neck geometry (P = 0.0076), and the cup abduction angle (P = 0.0379) were significantly associated with dislocation (Table 3).
Table 2.
Risk factors for dislocation; univariate analysis of the factors for dislocation
| Factors | Dislocation (+) | Dislocation (−) | P value |
|---|---|---|---|
| Age (years old) | 65.7 ± 12.5 | 63.1 ± 10.9 | 0.1493 |
| Height (cm) | 154 ± 11.0 | 152.5 ± 8.30 | 0.2975 |
| Body weight (kg) | 56.4 ± 13.6 | 54.9 ± 10.8 | 0.4454 |
| BMI (kg/m2) | 23.7 ± 4.45 | 23.5 ± 3.69 | 0.7817 |
| Gender | Male: 5.50 % (12/218) | Male: 94.5 % (206/218) | 0.0109* |
| Female: 2.33 % (24/1031) | Female: 97.7 % (1007/1031) | ||
| Indication of THA | OA: 1.17 % (11/944) | OA: 98.8 % (933/944) | <0.0001* |
| RA: 8.16 % (4/49) | RA: 91.8 % (45/49) | ||
| ONFH: 9.09 % (9/99) | ONFH: 90.9 % (90/99) | ||
| Revision: 7.59 % (12/158) | Revision: 92.4 % (146/158) | ||
| Prior osteotomy | Prior osteotomy (−): 2.93 % (34/1162) | Prior osteotomy (−): 97.1 % (1128/1162) | 0.7239 |
| Prior osteotomy (+): 2.27 % (2/88) | Prior osteotomy (+): 97.7 % (86/88) | ||
| Diameters of femoral head | 22 mm: 4.33 % (9/208) | 22 mm: 95.7 % (199/208) | 0.2502 |
| 26 mm: 2.71 % (22/812) | 26 mm: 97.3 % (790/812) | ||
| 32 mm: 1.60 % (3/187) | 32 mm: 98.4 % (184/187) | ||
| Neck geometry | PerFix: 4.44 % (16/360) | PerFix: 95.6 % (344/360) | 0.0077* |
| PerFix-910: 1.73 % (13/753) | PerFix-910: 98.3 % (740/753) | ||
| Cup abduction (°) | 43.5 ± 7.56 | 40.6 ± 6.24 | 0.0060* |
| Cup anteversion (°) | 12.3 ± 7.76 | 11.2 ± 6.93 | 0.3916 |
BMI body mass index, OA osteoarthritis, RA rheumatoid arthritis, ONFH idiopathic osteonecrosis of femoral head
Qualitative data were compared with χ2 test and quantitative data with the Pearson test
* Statically significant p-value <0.05
Table 3.
Multivariate analysis of the factors for dislocation
| Factors | Odds ratio | 95 % percentile | P value |
|---|---|---|---|
| Age | 1.03 | 0.938–1.009 | 0.1470 |
| BMI | 1.05 | 0.857–1.075 | 0.4349 |
| Gender | 1.12 | 0.392–2.954 | 0.8227 |
| Indication of THA | |||
| OA / RA | 4.96 | 0.700–22.28 | <0.001* |
| OA / ONFH | 14.8 | 4.961–44.43 | |
| OA / revision | 9.67 | 2.601–32.59 | |
| Neck geometry | 3.64 | 1.416–9.578 | 0.0076* |
| Cup abduction | 1.07 | 0.867–0.996 | 0.0379* |
| Cup anteversion | 1.06 | 0.886–1.008 | 0.0866 |
BMI body mass index, OA osteoarthritis, RA rheumatoid arthritis, ONFH idiopathic osteonecrosis of femoral head
Qualitative data were compared with χ2 test and quantitative data with the Pearson test
* Statically significant p-value <0.05
Incidence of recurrent dislocation and risk factors
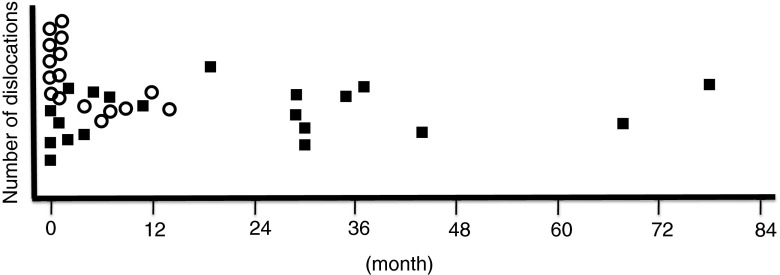
Among 36 hips with dislocation, 20 hips (55.6 %) had dislocated more than twice. Univariate and multivariate analysis revealed that the timing of the first dislocation was the only significant factor for recurrent dislocations with an odds ratio of 5.94 for each year (Table 4 and Table 5). The average timing of the first dislocation was 21.6 months in patients with recurrent dislocations and 3.6 months with a single dislocation (P = 0.0006) (Fig. 2). The hips with late dislocations showed a significantly higher incidence of recurrent dislocations; ten out of 11 hips (90.9 %) versus ten out of 25 hips (40.0 %) with early dislocation (P = 0.0046). Factors contributing to the overall dislocation rate mentioned above were not shown to be significant with respect to recurrent dislocation.
Table 4.
Univariate analysis of the factors for recurrent dislocation
| Factors | Recurrent (+) | Recurrent (−) | P value |
|---|---|---|---|
| Age (years old) | 63.0 ± 13.6 | 69.1 ± 10.3 | 0.1273 |
| Height (cm) | 153.3 ± 11.0 | 155.0 ± 11.3 | 0.6547 |
| Body weight (kg) | 55.8 ± 14.6 | 57.2 ± 12.8 | 0.7605 |
| BMI (kg/m2) | 23.6 ± 5.30 | 23.7 ± 3.26 | 0.9539 |
| Gender | Male: 50 % (6/12) | Male: 50 % (6/12) | 0.6353 |
| Female: 58.3 % (14/24) | Female: 41.7 % (10/24) | ||
| Indication of THA | OA: 45.5 % (5/11) | OA: 54.6 % (6/11) | 0.1391 |
| RA: 50 % (2/4) | RA: 50 % (2/4) | ||
| ONFH: 88.9 % (8/9) | ONFH: 11.1 % (1/9) | ||
| Revision: 41.7 % (5/12) | Revision: 58.3 % (7/12) | ||
| Diameters of femoral head | 22 mm: 55.6 % (5/9) | 22 mm: 44.4 % (4/9) | 0.9434 |
| 26 mm: 59.1 % (13/22) | 26 mm: 40.9 % (9/22) | ||
| 32 mm: 66.7 % (2/3) | 32 mm: 33.3 % (1/3) | ||
| Direction of dislocation | Anterior: 55.6 % (5/9) | Anterior: 44.4 % (4/9) | 1.0000 |
| Posterior: 55.6 % (15/27) | Posterior: 44.4 % (12/27) | ||
| Cup abduction (°) | 44.2 ± 8.87 | 42.8 ± 5.72 | 0.5750 |
| Cup anteversion (°) | 11.5 ± 7.87 | 13.2 ± 7.76 | 0.5160 |
| Timing of dislocation (month) | 21.6 ± 23.0 | 3.56 ± 4.65 | 0.0006* |
| Timing of dislocation (≤1 year, >1 year) | ≤1 year: 40.0 % (10/25) | ≤1 year: 60.0 % (15/25) | 0.0046* |
| >1 year: 90.9 % (10/11) | >1 year: 9.09 % (1/11) |
BMI body mass index, OA osteoarthritis, RA rheumatoid arthritis, ONFH idiopathic osteonecrosis of femoral head
Qualitative data were compared with χ2 test and quantitative data with the Pearson test
* Statically significant p-value <0.05
Table 5.
Multivariate analysis of the factors for recurrent dislocation
| Factors | Odds ratio | 95 % percentile | P value |
|---|---|---|---|
| Age | 1.01 | 0.892–1.164 | 0.8793 |
| BMI | 1.01 | 0.730–1.313 | 0.9512 |
| Gender | 3.79 | 0.180–165.9 | 0.3927 |
| Direction of dislocation | 7.27 | 0.576–197.5 | 0.1298 |
| Indication of THA | |||
| OA / RA | 6.82 | 0.115–630.6 | 0.5016 |
| OA / ONFH | 14.7 | 0.459–1181 | |
| OA / revision | 2.50 | 0.228–41.97 | |
| Timing of dislocation (year) | 5.94 | 0.663–0.985 | 0.0248* |
| Cup abduction | 1.03 | 0.804–1.157 | 0.7572 |
| Cup anteversion | 1.07 | 0.942–1.256 | 0.2975 |
BMI body mass index, OA osteoarthritis, RA rheumatoid arthritis, ONFH idiopathic osteonecrosis of femoral head
Qualitative data were compared with χ2 test and quantitative data with the Pearson test
* Statically significant p-value <0.05
Fig. 2.
Distribution of timing of the first dislocation. The average period to the first dislocation was 21.6 months in patients with a recurrent dislocation and 3.6 months with a single dislocation (P = 0.0006). The hips with a late dislocation show a significantly higher incidence of a recurrent dislocation compared to those with an early dislocation; ten out of 11 hips (90.9 %) versus ten out of 25 hips (40.0 %). ○ single dislocation, ■ recurrent dislocation
Subsequent clinical course
Revision THA for recurrent dislocation was performed in seven hips out of 20 including two hips in patients with an early dislocation and five hips with a late dislocation. Five hips were revised with a larger femoral head and an elevated liner and two hips had revision of both the acetabular cup and head. One hip with a revision of a larger head needed further revision of the acetabular cup. The remaining six hips did not have a dislocation after revision. There were two hips with recurrent dislocations in which the revision was indicated but the patients refused to have revisions.
Discussion
In our study of 1,250 hips, a dislocation occurred in 36 hips (2.9 %) including 16 (44.4 %) hips with one dislocation and 20 (55.6 %) hips with more than two dislocations. Although several factors are indicated that influence the dislocation rate overall, only the timing of the first dislocation was a significant factor for recurrent dislocations with an odds ratio of 5.94 for each year.
A review of the literature indicated numerous factors that have influenced the dislocation including patient-, implant-, and surgeon-related factors. Among the significant factors in this study, the primary diagnosis for THA strongly affected the incidence of dislocation (P < 0.001). The hips with ONFH, RA, or revisions are more likely to have a dislocation than those with OA. This is in accordance with other reports. Berry et al. showed that inflammatory hip disease increased dislocation rate with an odds ratio of 1.5 [14]. Alberton et al. reported an increased incidence of dislocation in hips after revision with a dislocation rate of 7.4 % [15]. The head–neck ratio, an implant-related factor, also significantly influenced the incidence of dislocation. PerFix-910 has a larger HNR compared to PerFix and reduced the dislocation rate with an odds ratio of 3.64. Similar findings were reported by Barrack et al. in that the dislocation rate with a stem with a larger (14/16) and circular cross-section neck was three times higher compared with the smaller (12/14) and trapezoidal neck [16, 17]. Larger head size has been reported to decrease the dislocation in many studies; however, head size was not identified as a significant factor in this study [18, 19]. This was due to three dislocations in hips with revision THA using a 32-mm head. When only the hips with primary THA were analysed, head size was a significant factor for dislocation, but not for the recurrent dislocation (data not shown).
Several factors have been associated with recurrent dislocation including cup malposition, abductor insufficiency and surgical approach [20]. Parvizi et al. and Yuan et al. independently suggested cup malposition as a major risk for recurrent dislocation [20, 21]. Although vertical placement of the cup was a risk factor for dislocation, this study did not identify cup position as an influencing factor for recurrent dislocation. Our study demonstrated that the timing of the first dislocation was the only factor to predict recurrence. Recurrent dislocation occurred in as many as 90.9 % of the hips with late dislocation compared with 40.0 % of the hips dislocated with early dislocation with an odds ratio of 5.94. These data were in accordance with previous reports. Von Knoch et al. showed that 55 % of the patients with a dislocation after five years had recurrence [12]. Brennan et al. also showed that the late dislocation significantly recurred compared to the early dislocation [22].
Conversely, multiple factors were shown to influence late dislocation. Reported risk factors include female sex, younger age, episode of trauma, polyethylene wear and implant loosening [7, 12, 23]. Woo and Morrey reported that the percentage of patients with dislocation five years after THA was 0.19 % in 1982 [2]. They later revised this percentage to 0.84 % with an extended follow-up duration in 2002 [12]. The proportion of late dislocation among all dislocation cases was as high as 32 % in a 2002 report. Late dislocation accounted for 31 % of all dislocations in this study, which was higher than the incidences previously reported [2, 24, 25]. This is most likely due to an extended follow-up period allowing for increased patient life span and therefore more time for dislocation to occur.
The definition of late dislocation differed among the studies. Khan et al. defined late dislocation that occurred after five weeks [1]. Whereas, the first dislocation that occurred five years after the operation was defined as late dislocation in other reports [12, 25]. Meek et al. reported that the majority of dislocations occur by 12 months (66 %), and a late, sudden increase was not observed in the dislocation rates [11]. They suggested that published dislocation rates are standardised at 12 months after surgery. Thus late dislocation was defined as the first dislocation that occurred beyond 12 months after operation in this study.
Recurrent dislocation with a late onset of the first dislocation has been proven to be refractory to conservative treatment. Surgical treatment was performed in seven hips out of 20 including two hips (20 %) in patients with an early dislocation and five hips (50 %) with a late dislocation. Pulido et al. showed that revision was necessary in 34 % of late dislocation cases, confirming the refractory nature of late dislocation [25]. Von Knoch et al. also reported that 61 % of the hips with recurrent dislocation and 33 % of the late dislocations were treated with reoperation [12].
This study has several limitations. As the posterolateral approach was used in all cases, our findings might differ from studies that used a different approach. However, as the posterior approach has been associated with higher rates of dislocation [3, 6], we believe that it was meaningful to examine the incidence of dislocation using this approach. Also, the sample size of 1,250 hips was relatively small compared to the previous large-scale study [18]. The number of dislocations and recurrent dislocations were 36 and 20, respectively. However, if the sample size were larger, the factors such as the number of surgeons, types of implant, and types of approach would vary widely, making the analysis less precise. THAs in this study were performed in a single institution using the same implants in most hips through the same approach; therefore, there was the advantage of minimising the effects of confounding variables. Additionally, the follow-up period ranged from one year to 14 years postoperatively, and some patients were followed up only for a short period of time. As the incidence of dislocation is cumulative, a longer observation period is required for analysing late dislocation. Lastly, the effects of stem anteversion as well as combined anteversion on the dislocation rate were not examined in this study as the stem anteversion could not be measured precisely using the plain radiographs. However, excessively large or small stem anteversion results in the inappropriately combined anteversion might lead to the functional implant malposition. This topic needs further clarification using postoperative computed tomography data.
Conclusion
Dislocation occurred in 36 hips (2.9 %) after THA, including 20 (55.6 %) hips with recurrent dislocation. Although several factors are indicated in influencing the dislocation rate overall, only the timing of the first dislocation was the significant factor for recurrent dislocation with an odds ratio of 5.94 for each year. Late dislocation is refractory to conservative treatment and requires surgical treatment instead. These results suggest that the directed care is necessary for patients with a late dislocation to avoid recurrence.
Acknowledgments
Conflict of interest
All the authors have no conflict of interest related to this work.
Footnotes
This work was supported by Grant-in-Aid for Scientific Research from the Japan Society for the Promotion of Science (No. 24592268).
References
- 1.Ali Khan MA, Brakenbury PH, Reynolds IS. Dislocation following total hip replacement. J Bone Joint Surg Br. 1981;63-B:214–218. doi: 10.1302/0301-620X.63B2.7217144. [DOI] [PubMed] [Google Scholar]
- 2.Woo RY, Morrey BF. Dislocations after total hip arthroplasty. J Bone Joint Surg Am. 1982;64:1295–1306. [PubMed] [Google Scholar]
- 3.Vicar AJ, Coleman CR. A comparison of the anterolateral, transtrochanteric, and posterior surgical approaches in primary total hip arthroplasty. Clin Orthop Relat Res. 1984;188:152–159. [PubMed] [Google Scholar]
- 4.Ekelund A, Rydell N, Nilsson OS. Total hip arthroplasty in patients 80 years of age and older. Clin Orthop Relat Res. 1992;281:101–106. [PubMed] [Google Scholar]
- 5.Pellicci PM, Bostrom M, Poss R. Posterior approach to total hip replacement using enhanced posterior soft tissue repair. Clin Orthop Relat Res. 1998;355:224–228. doi: 10.1097/00003086-199810000-00023. [DOI] [PubMed] [Google Scholar]
- 6.Masonis JL, Bourne RB. Surgical approach, abductor function, and total hip arthroplasty dislocation. Clin Orthop Relat Res. 2002;405:46–53. doi: 10.1097/00003086-200212000-00006. [DOI] [PubMed] [Google Scholar]
- 7.Paterno SA, Lachiewicz PF, Kelley SS. The influence of patient-related factors and the position of the acetabular component on the rate of dislocation after total hip replacement. J Bone Joint Surg Am. 1997;79:1202–1210. doi: 10.2106/00004623-199708000-00013. [DOI] [PubMed] [Google Scholar]
- 8.Soong M, Rubash HE, Macaulay W. Dislocation after total hip arthroplasty. J Am Acad Orthop Surg. 2004;12:314–321. doi: 10.5435/00124635-200409000-00006. [DOI] [PubMed] [Google Scholar]
- 9.Dudda M, Gueleryuez A, Gautier E, Busato A, Roeder C. Risk factors for early dislocation after total hip arthroplasty: a matched case–control study. J Orthop Surg (Hong Kong) 2010;18:179–183. doi: 10.1177/230949901001800209. [DOI] [PubMed] [Google Scholar]
- 10.Bozic KJ, Ong K, Lau E, Kurtz SM, Vail TP, Rubash HE, Berry DJ. Risk of complication and revision total hip arthroplasty among Medicare patients with different bearing surfaces. Clin Orthop Relat Res. 2010;468:2357–2362. doi: 10.1007/s11999-010-1262-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Meek RM, Allan DB, McPhillips G, Kerr L, Howie CR. Late dislocation after total hip arthroplasty. Clin Med Res. 2008;6:17–23. doi: 10.3121/cmr.2008.770. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.von Knoch M, Berry DJ, Harmsen WS, Morrey BF. Late dislocation after total hip arthroplasty. J Bone Joint Surg Am. 2002;84-A:1949–1953. doi: 10.2106/00004623-200211000-00007. [DOI] [PubMed] [Google Scholar]
- 13.McLaren RH. Prosthetic hip angulation. Radiology. 1973;107:705–706. doi: 10.1148/107.3.705. [DOI] [PubMed] [Google Scholar]
- 14.Berry DJ, von Knoch M, Schleck CD, Harmsen WS. The cumulative long-term risk of dislocation after primary Charnley total hip arthroplasty. J Bone Joint Surg Am. 2004;86-A:9–14. doi: 10.2106/00004623-200401000-00003. [DOI] [PubMed] [Google Scholar]
- 15.Alberton GM, High WA, Morrey BF. Dislocation after revision total hip arthroplasty: an analysis of risk factors and treatment options. J Bone Joint Surg Am. 2002;84-A:1788–1792. [PubMed] [Google Scholar]
- 16.Barrack RL, Butler RA, Laster DR, Andrews P. Stem design and dislocation after revision total hip arthroplasty: clinical results and computer modeling. J Arthroplasty. 2001;16:8–12. doi: 10.1054/arth.2001.28359. [DOI] [PubMed] [Google Scholar]
- 17.Barrack RL. Dislocation after total hip arthroplasty: implant design and orientation. J Am Acad Orthop Surg. 2003;11:89–99. doi: 10.5435/00124635-200303000-00003. [DOI] [PubMed] [Google Scholar]
- 18.Bystrom S, Espehaug B, Furnes O, Havelin LI. Femoral head size is a risk factor for total hip luxation: a study of 42,987 primary hip arthroplasties from the Norwegian Arthroplasty Register. Acta Orthop Scand. 2003;74:514–524. doi: 10.1080/00016470310017893. [DOI] [PubMed] [Google Scholar]
- 19.Amlie E, Hovik O, Reikeras O. Dislocation after total hip arthroplasty with 28 and 32-mm femoral head. J Orthop Traumatol. 2010;11:111–115. doi: 10.1007/s10195-010-0097-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Parvizi J, Kim KI, Goldberg G, Mallo G, Hozack WJ. Recurrent instability after total hip arthroplasty: beware of subtle component malpositioning. Clin Orthop Relat Res. 2006;447:60–65. doi: 10.1097/01.blo.0000218749.37860.7c. [DOI] [PubMed] [Google Scholar]
- 21.Yuan L, Shih C. Dislocation after total hip arthroplasty. Arch Orthop Trauma Surg. 1999;119:263–266. doi: 10.1007/s004020050406. [DOI] [PubMed] [Google Scholar]
- 22.Brennan SA, Khan F, Kiernan C, Queally JM, McQuillan J, Gormley IC, O'Byrne JM. Dislocation of primary total hip arthroplasty and the risk of redislocation. Hip Int. 2012;22:500–504. doi: 10.5301/HIP.2012.9747. [DOI] [PubMed] [Google Scholar]
- 23.Vaughn BK. Managing chronic dislocated total hip arthroplasty. Semin Arthroplasty. 1993;4:16–24. [PubMed] [Google Scholar]
- 24.Coventry MB. Late dislocations in patients with Charnley total hip arthroplasty. J Bone Joint Surg Am. 1985;67:832–841. [PubMed] [Google Scholar]
- 25.Pulido L, Restrepo C, Parvizi J. Late instability following total hip arthroplasty. Clin Med Res. 2007;5:139–142. doi: 10.3121/cmr.2007.717. [DOI] [PMC free article] [PubMed] [Google Scholar]