Abstract
Purpose
This study aimed to review quantitative literature pertaining to studies of music-based interventions in palliative cancer care and to review the neurobiological literature that may bare relevance to the findings from these studies.
Methods
A narrative review was performed, with particular emphasis on RCTs, meta-analyses, and systematic reviews. The Cochrane Library, Ovid, PubMed, CINAHL Plus, PsycINFO, and ProQuest were searched for the subject headings music, music therapy, cancer, oncology, palliative care, pain, anxiety, depression, mood, quality of life, prevalence, neuroscience, functional imaging, endogenous opioids, GABA, 5HT, dopamine, and permutations of these same search terms. Data for the review were comprised of articles published between 1970 and 2012. References of all the cited articles were also reviewed.
Results
Available evidence suggests that music-based interventions may have a positive impact on pain, anxiety, mood disturbance, and quality of life in cancer patients. Advances in neurobiology may provide insight into the potential mechanisms by which music impacts these outcomes.
Conclusions
More research is needed to determine what subpopulation of cancer patients is most likely to respond to music-based interventions, what interventions are most effective for individual outcomes, and what measurement parameters best gauge their effectiveness.
Keywords: Music, Cancer, Oncology, Palliative, Neurobiology
Introduction
By alleviating the physical and psychological symptoms associated with malignancy, palliative care serves a vital role in the multidisciplinary care of cancer patients. Common symptoms such as pain, anxiety, and mood disturbance can be difficult to manage with standard pharmaceutical options and may significantly interfere with quality of life (QOL) [1, 2]. The search for complimentary interventions that are both cost effective and associated with few side effects has led to an increased interest in the therapeutic use of music for cancer patients within the field of palliative care [3–6]. This review summarizes findings from quantitative research literature. Furthermore, it discusses challenges and opportunities associated with this emerging area of research and provides practical suggestions for future investigation.
Different music-based interventions defined
The interventions in this review are generally classified as either music medicine or music therapy. In “music medicine” interventions, patients listen to prerecorded music that is administered by healthcare staff and preselected by study investigators, who may or may not have any formal training in music therapy [7, 8]. In “music therapy” interventions, patients are offered prerecorded, live, and/or interactive music that is individualized by a trained music therapist [9, 10]. Hence, the crucial distinction between music medicine (MM) and music therapy (MT) is that the former involves only a stimulus and response, and the latter involves a therapeutic relationship based on individualized assessment, treatment, and evaluation [7].
Specific clinical endpoints studied
Pain
Pain represents one of the most common symptoms affecting patients with advanced malignancy. One recent meta-analysis [11] pooled data from 52 studies (total N = 19,985) and estimated pain to occur in 33 % of patients who had completed treatment with curative intent, 59 % of patients undergoing anticancer therapy, and 64 % of patients with advanced/metastatic/terminal disease. A subsequent meta-analysis [12] pooled data from 64 studies (total N = 95,159), 34 of which reported pain prevalence in patients with all stages of cancer (including early disease), and 30 of which reported pain prevalence in patients with advanced cancer. The combined weighted mean prevalence of pain in the 14,961 patients with advanced cancer was estimated to be 75 %.
Multiple studies have demonstrated that music-based interventions may have a mild to moderate analgesic effect (Table 1). Five such randomized controlled trials (RCTs) (total N = 391) were analyzed in a 2011 Cochrane Review [13]. Prerecorded music was provided perioperatively for 15 out of 30 breast cancer patients undergoing mastectomy [14], during bone marrow biopsy for 29 out of 59 hematologic malignancy patients [15], as a single 30-min session in 62 out of 126 adult patients with various malignancies [16], during lumbar puncture in 20 out of 40 pediatric leukemia patients [17], and as a single session with guided imagery in 65 out of 136 adult patients with various malignancies [18]. Based on the combined results of these five studies, the authors classified music's analgesic effect as moderate, with a standardized mean difference (SMD) of −0.59, (95 % CI from −0.92 to −0.27, P = 0.0003). All five of the above studies reported pain by self-reported measurement scales. An earlier Cochrane Review examined the effect of music on analgesic requirements during a painful procedure (five studies), during a 2-h postoperative period (three studies), or during a 24-h postoperative period (five studies) [19]. Although none of the included studies were limited to oncologic or palliative care settings, the 13 included studies (N = 1016) did show that exposure to music was associated with a decrease in opioid requirement, with a SMD of −1.29 (95 % CI from −0.92 to −0.27, P = 0.0062). These results were consistent with those from a separate meta-analysis [20] which studied the use of music vs. standard care in adult patients undergoing colonoscopy. This meta-analysis included three trials [21–23] in which music was provided to a total of 130 out of 261 patients. The patients who received music required 29.7 % less analgesia with meperidine, alfentanil, or pethidine (P = 0.001) and 15 % less sedation with midazolam or propofol (P = 0.055). Finally, a single-arm study from 2006 [5] found that in 126 palliative care patients with pain (90 % of whom had cancer), mean self-reported pain scores decreased from 2.7 to 2.1 on a five-point VAS after a single MT session (P < 0.001).
Table 1.
Individual studies investigating the analgesic effect of music-based interventions in either oncologic or palliative care settings
| Author, year, type of study | Study population | Music intervention | Control | N, music group | N, control group | Results |
|---|---|---|---|---|---|---|
| Binns-Turner, 2008, RCTa [14] | Breast cancer patients undergoing mastectomy | MM: single session of prerecorded music through headphones (continuously from preoperative through postoperative period). Patients could select from classical, easy listening, inspirational, or new age | iPod and headphones but no music or sounds | 15 | 15 | Significant reduction in self-reported postop pain level by VAS (P = 0.007) |
| Danhauer et al., 2010, RCTa [15] | Hematologic malignancy patients undergoing lumbar puncture | MM: prerecorded music through headphones for duration of procedure. Patients could select from classical, harp, general instrumental, nature sounds, country, gospel, and jazz | Standard care | 29 | 30 | No significant reduction in self-reported intra-procedural pain level by VAS (P = 0.771) |
| Huang, 2006, RCTa [16] | Adult inpatients with various malignancies | MM: single 30-min session of prerecorded music through headphones. Patients could select from Taiwanese folk, Buddhist, harp, and piano recordings | Bed rest | 62 | 64 | Significant reduction in self-reported pain level by VAS (P < 0.001) |
| Nguyen et al., 2010, RCTa [17] | Pediatric leukemia patients undergoing lumbar puncture | MM: prerecorded music through headphones for duration of procedure. Patients could select from either traditional Vietnamese songs or children’s songs | iPod and headphones but no music or sounds | 20 | 20 | Significant reduction in self-reported intra-procedural pain level by VAS (P < 0.001) |
| Yonghui et al., 2009, RCTa [18] | Adult inpatients with various malignancies | MM: single 30-min session of unspecified music with unspecified guided imagery | Standard care | 65 | 71 | No significant reduction in self-reported pain detected by numeric rating scale (P > 0.05) |
| Gallagher, 2006, single-arm study | Adults with a terminal illnessb in an inpatient palliative care setting | MT: single session of varying length including live performance, listening to prerecorded music, and interactive techniques | None | 126 | 0 | Significant reduction in self-reported pain by VAS, from mean score of 2.7 before the session to mean score of 2.1 after the session (P < 0.001) |
MM music medicine, MT music therapy
aIncluded in 2011 Cochrane Review
bFor 90 % of the patients in this study, the terminal illness was cancer
Overall, these data (derived exclusively from MM-based approaches except for [5]) support the use of music to decrease subjective pain and analgesic requirements in acute pain settings. However, more research is needed to investigate the analgesic efficacy of music for chronic pain, since cancer patients (particularly those in palliative care settings) frequently suffer from chronic pain (e.g., from bone metastases, visceral tumor growth, neuropathic pain associated with chemotherapy, etc.). In future studies investigating music-based interventions for chronic pain, careful consideration should be given to the frequency, duration, and type of interventions used (e.g., consideration of interventions not necessarily limited to MM).
Anxiety
For many patients, the diagnosis of cancer can result in significant anxiety, which can interfere with sleep [24], enjoyment of life [25], interpersonal relationships [26], and overall daily activities [27]. Six studies using survey instruments found self-reported anxiety symptoms to be present in 19–48 % of cancer patients [1, 24, 28–31]. In contrast, three studies using structured clinical interviews found DSM-IV-defined Anxiety Disorders (e.g., generalized anxiety disorder, panic disorder, and post-traumatic stress disorder) to be present in 7.6 to 18 % of cancer patients [24, 32, 33].
Several studies have demonstrated that music-based interventions may have a mild to moderate anxiolytic effect (Table 2). Seven such studies (six RCTs and one controlled clinical trial (CCT), total N = 386) using self-report outcomes were analyzed in the 2011 Cochrane Review [13]. Music was provided perioperatively for 15 out of 30 breast cancer patients undergoing mastectomy [14], during invasive procedures for 20 out of 39 pediatric cancer patients [34], directly prior to the administration of adjuvant chemotherapy for 30 out of 60 breast cancer patients [35], during bone marrow biopsy for 29 out of 59 adults with hematologic malignancy [15], during chemotherapy for 10 out of 20 adult cancer patients [36], during radiation therapy for 19 out of 42 adult cancer patients [37], and as a single 30-min session for 65 out of 136 adult cancer patients with pain [18]. Based on the combined results of these seven studies, the SMD on the 80-point State-Trait Anxiety Inventory Scale (STAI-S) was −11.20 units (95 % CI −19.59 to −2.82, P = 0.0088). These results were consistent with those from four other RCTs involving patients without cancer, in whom perioperative anxiety was significantly reduced by music-based interventions [38–41]. One small but well-designed RCT specifically examined the effectiveness of a single 20–40-min MT session in reducing anxiety for terminally ill patients [42]. Although cancer was not an inclusion criterion, 24 out of 25 patients in the study had cancer, and all study participants were inpatients receiving palliative care services. Based on the Edmonton Symptom Assessment Scale anxiety scores before and after the intervention, the Mann–Whitney test showed that anxiety was significantly reduced in the music group compared to the control group (P = 0.005).
Table 2.
Individual studies investigating the anxiolytic effect of music-based interventions in either oncologic or palliative care settings
| Author, year, study type | Study population | Music intervention | Control | N, music group | N, control group | Results |
|---|---|---|---|---|---|---|
| Binns-Turner, 2008, RCTa [14] | Breast cancer patients undergoing mastectomy | MM: single session of prerecorded music through headphones (continuously from preoperative through postoperative period). Patients could select from classical, easy listening, inspirational, or new age | iPod with headphones but no music or sounds | 15 | 15 | Significant reduction in anxiety detected (P < 0.001). Mean STAI in music group fell from 41.5 to 30.7, while mean STAI in control group rose from 41.9 to 49.7 |
| Bufalini, 2009, CCTa, b [34] | Pediatric cancer patients undergoing invasive procedures (e.g., lumbar puncture, bone marrow biopsy, etc.) | MT: single 15-min session of music listening followed by interactive music making for the remainder of the invasive procedure (all during conscious sedation). For listening phase, patients could select from children’s songs, folk, ethnic, and pop | Conscious sedation alone | 20 | 19 | Significant reduction in anxiety of patients in music group compared to control group at all times throughout procedure by modified Yale Preoperative Anxiety Scale (P < 0.05). STAI-S scores were only measured in the parents of the patients undergoing invasive procedures, in whom no significant difference was found |
| Bulfone et al., 2009, RCTa [35] | Breast cancer patients receiving adjuvant chemotherapy | MM: single 15-min session of prerecorded music through headphones while waiting for chemotherapy. Patients could select from new age, Celtic, classical, soundtracks, or nature music | Standard care | 30 | 30 | Significant reduction in anxiety detected (P < .001). Mean STAI in music group fell from 46.2 to 36.3, while mean STAI in control group rose from 43.4 to 44.8 |
| Danhauer et al., 2010, RCTa` [15] | Hematologic malignancy patients undergoing bone marrow biopsy | MM: single 20- to 60- min session of prerecorded music through headphones for duration of BM biopsy. Patients could select from classical, harp, instrumental, nature sounds, country, gospel, and jazz | Standard care | 29 | 30 | No significant difference was found in the STAI-S scores between two groups (P = 0.766). However, “patient satisfaction with music was high; 66 % of the patients in the music group said that they very much preferred to listen to music with future biopsies” |
| Harper, 2001, RCT a [36] | Adult cancer patients receiving chemotherapy | MM: single 30-min session of prerecorded music through headphones during chemotherapy infusion. Patients were offered a new age recording published by Image Paths Inc., entitled, “Health Journeys: A Meditation To Help you with Chemotherapy” | Standard care | 10 | 10 | Borderline significant reduction in anxiety detected by STAI (P = 0.05). Mean STAI in music group fell from 42.9 to 28.5, while mean STAI in control group rose from 32.3 to 41.7. Although a significant reduction in anxiety was reportedly detected by the Beck Anxiety Inventory (P < 0.01), only BAI values after the intervention (not before) were specified |
| Smith et al., 2001, RCT a [37] | Adult cancer patients receiving radiation therapy | MM: multiple 30-min sessions of prerecorded music through headphones during simulation and daily treatments for the duration of therapy. Patients could select from rock and roll, big band, country and western, classical, easy listening, Spanish, or religious music | Standard care | 19 | 23 | No significant difference was found between two groups when mean STAI-S scores were compared. However, post hoc subgroup analysis showed that among patients with baseline state anxiety scores >34, those “patients in the experimental group had a steeper decline [from before until after the intervention(s)] compared to the controls” |
| Yonghui et al., 2009, RCTa, c [18] | Hospitalized adult cancer patients with pain | MM: Single 30-min session of prerecorded music with imagery during hospitalization | Standard care | 65 | 71 | Significant reduction in anxiety detected (P < 0.05). Mean STAI in music group fell from 57.9 to 33.8, but mean STAI in control group only fell from 58.6 to 55.9 |
| Horne-Thompson and Grocke, 2008, RCT [42] | Adults with a terminal illness in an inpatient palliative care setting (24 out of 25 of which had a diagnosis of cancer) | MT: single 20- to 40-min session conducted by a registered music therapist. Techniques included “playing live familiar music, singing, music and relaxation, music and imagery, improvisation, music-assisted counseling, reminiscence, and listening to recorded music” | Visit from volunteer that either read to, conversed with, or provided emotional support to the patient | 13 | 12 | Significant reduction of anxiety in music group compared to the control group by Mann–Whitney testing (P = 0.005). Eight patients in music group reported a decrease in anxiety of between 1 and 5 points on ESAS scale, while only 1 patient in control group reported a decrease in anxiety of 1 point. Three patients in control group reported increased anxiety after the study interval |
MM music medicine, MT music therapy
aIncluded in 2011 Cochrane Review [13]
bInsufficent information regarding presence/absence/method of randomization led to the classification of the Bufalini 2009 study [34] as a controlled clinical trial by the authors of the 2011 Cochrane review [13]. Note that the Bufalini 2009 study [34] used mYPAS scores to measure anxiety in the patients, but only used STAI-S scores to measure anxiety in the parents. Since the STAI-S scores in the parents (unlike the mYPAS scores in the patients) showed no significant difference, its inclusion in the pooled analysis with the other six trials would have tended to underestimate the effect of music on anxiety. Furthermore, a sensitivity analysis, excluding the results of both the Bufalini 2009 [34] and Yonghui 2009 [18] studies (based on unclear randomization methods), resulted in a mean difference of −9.46 (95 % CI −19.01 to 0.09, P = 0.05)
cPatients in the Yonghui 2009 study [18] were clearly randomized, hence its classification as an RCT by the authors of the 2011 Cochrane Review [13]. However, since its method of randomization was not entirely clear, it was excluded in the sensitivity analysis
Overall, these data (derived from six studies using MM and two studies using MT) support the use of music to reduce anxiety in situations such as before/during invasive procedures, chemotherapy, and radiation therapy. Relatively less is known about music’s capacity to decrease the need for pharmacologic anxiolytics/sedatives/hypnotics. Although one study in 327 patients undergoing elective surgery showed a greater decrease in preoperative STAI-S scores with relaxing music than 0.05–0.1mg/kg of midazolam (P < 0.001) [43], the relevance of this finding to the oncologic and palliative care settings remains uncertain. Furthermore, more research is needed to investigate the anxiolytic efficacy of music beyond the acute/situational anxiety setting, particularly for cancer patients in whom the recognition of disease progression and impending death may be particularly anxiety inducing [44, 45].
Mood disturbance
The period following diagnosis of cancer can be very emotional for many patients. Patients with frequent depressive symptoms may develop a sustained disturbance of mood and may eventually meet criteria for a DSM-IV-defined Affective Disorder (e.g., major depressive disorder or dysthymic disorder). Prevalence studies suggest that self-reported depressive symptoms in patients with cancer are common and perhaps more common in the terminal/advanced setting [46–49]. Four studies using survey instruments found depressive symptoms present in 53–74 % of cancer patients [46, 50–52]. A much more recent meta-analysis of 94 interview-based studies estimated the combined mean prevalence of major depressive disorder and dysthymic disorder in palliative and hematologic–oncologic settings [53]. From the 24 studies conducted in palliative care settings (total N = 4,007), the combined mean prevalence of these two disorders was found to be 24.6 %. From the 70 studies conducted in hematology–oncology settings (total N = 10,071), combined mean prevalence was found to be 20.7 %. To place these numbers in context, the NIMH estimates the combined prevalence of major depressive disorder and dysthymic disorder to be 8.2 % among US adults (two to three times lower than in cancer patients).
While multiple studies have found that music-based interventions may have a positive impact on mood (Table 3), this has not necessarily been the case for depression. Such a discrepancy may be at least partially explained by differences between methods used to assess mood disturbance versus those used to assess depression. For example, the commonly used Profile of Mood States (POMS) uses six domains to calculate a total mood disturbance score: depression–dejection, tension–anxiety, anger–hostility, fatigue–inertia, confusion–bewilderment, and vigor–activity. The first five domains are weighted positively and the last domain is weighted negatively, such that a higher score indicates a greater disturbance of mood. Henceforth, music could elicit improvement in mood via the five other domains but not in “depression/dejection.” This difference in outcomes was well illustrated in a 2011 Cochrane Review [13], which analyzed five trials examining the effect of music on depression (total N = 468 patients). Music was provided for 128 out of 182 adults with cancer receiving chemotherapy or radiation therapy [54], 34 out of 60 adults with hematologic malignancy admitted for autologous SCT [55], 27 out of 48 adults with cancer undergoing radiation therapy [56], 20 out of 42 women with metastatic breast cancer [57], and 65 out of 136 adult cancer patients with pain [18]. The pooled estimate from these five trials did not find a statistically significant effect of music on depression (SMD = −0.07, 95 % CI −0.40 to 0.27, P = 0.69). However, the same meta-analysis analyzed three trials examining the effect of music on mood (total N = 105), and the pooled estimate from these three studies did demonstrate a statistically significant effect (SMD = 0.42, 95 % CI 0.03 to 0.81, P = 0.03). These three studies investigating the outcome of mood provided music to 8 out of 15 adults with cancer-related pain [58], 34 out of 60 adults with hematologic malignancy admitted for autologous SCT [55], and 15 out of 30 children with neoplasms needing chemotherapy [59]. That Cassileth’s same study [55] showed no effect on depression, but did show an effect on mood, supports the idea that the difference between these two outcomes may be more than semantic. Among the 123 palliative care patients with mood disturbance in the single-arm study of Gallagher et al. in 2006 [5], mean self-reported mood disturbance scores improved from 1.8 to 0.7 on a five-point VAS after a single MT session (P < 0.001).
Table 3.
Individual studies investigating the effect of music-based interventions on mood disturbance in either oncologic or palliative care settings
| Author, year, type of study | Study population | Music intervention | Control | N, music group | N, control group | Results |
|---|---|---|---|---|---|---|
| Beck, 1989, RCTa [58] | Adults with documented cancer-related pain (setting: patients’ homes) | MM: three 45-min sessions of prerecorded music through headphones. Patients could select from classical, jazz, folk, rock, country and western, easy listening, and new age | Listening to 60-cycle hum through headphones | 8 | 7 | No significant difference detected in mean percent change of five-point VAS between groups (P = 0.599). However, “60 % of the subjects [in the music group] demonstrated at least some improvement in mood” |
| Cassileth et al., 2003, RCTa [55] | Adults with hematologic malignancy admitted for SCT | MT: median of five 20–30-min sessions (over median of 10 days). Live bedside music therapy was provided by trained music therapist | Standard care | 36 | 33 | Significant improvement in mood detected: Patients in the music therapy group scored 37 % lower on total POMS of mood disturbance (P = 0.01) and 28 % lower in the combined anxiety/depression domains (P = 0.065) |
| Duocastella, 1999, RCTa [59] | Pediatric cancer patients receiving inpatient chemotherapy | MT: single 45-min individualized MT session. Sessions included singing, instrument playing, movement to music, and musical games | Single session of non-musical activities led by music therapist | 15 | 15 | No significant improvement in mood detected using five-point Likert scale |
| Gallagher et al., 2006, single-arm studyb [5] | Adults with a terminal illness in an inpatient palliative care settingb | MT: single session of varying length including live performance, listening to prerecorded music, and interactive techniques | None | 123 | 0 | Significant improvement in mood detected: mean self-reported mood disturbance scores improved from 1.8 to 0.7 on a five-point VAS after a single music therapy session (P < 0.001) |
MM music medicine, MT music therapy
aIncluded in 2011 Cochrane Review
bPercentage of patients with cancer not specified
Overall, the limited data available regarding the outcome of mood (derived from three studies using MT and one study using MM) suggest that music may have a mild positive impact on the mood of cancer patients. Considering that the effects of music-based interventions on pain and anxiety have been most well demonstrated in acute settings, it may not be surprising that a single intervention (MM or MT based) may not show as much impact on mood disturbance, particularly chronically depressed mood. The availability of fast-acting pharmacologic analgesics and anxiolytics, versus the unavailability of any fast-acting pharmacologic antidepressant, may point toward potentially important neurobiological differences underlying these symptoms. With this in mind, particular consideration should be given to the frequency and duration (as well as the type) of interventions in future studies investigating the impact of music on mood in cancer patients.
Quality of life
Although there may be less prevalence data measuring overall QOL impairment in cancer patients (relative to pain, anxiety, and depression), the available data suggest that cancer is indeed associated with impaired QOL compared to the normal population [60–62]. This association could be expected for a number of reasons: first, because pain, anxiety, and depression are frequently incorporated into the tools used to measure HR-QOL in cancer patients; secondly, because all three of these symptoms have been shown to commonly affect patients with cancer [63]; and finally, because multiple studies in patients with multiple types of cancer have demonstrated independent associations between HR-QOL impairment and pain [64–68], anxiety [69–71], and depression [72–74].
Although the impact of music-based interventions on QOL has not been as extensively studied as pain, anxiety, or mood disturbance, four RCTs analyzed in the 2011 Cochrane Review [13] compared the impact of music-based interventions to standard care on QOL scores (Table 4). Clearly, QOL represents a more complex and multi-faceted outcome than pain, anxiety, or depression, and the comparison of results from these four studies was made even more complex by the fact that they all used different QOL assessment tools. In one of the four studies [57], pretest differences were too large for the results to be included in the pooled estimate. Through the other three trials, music was offered to 4 of 8 adults with cancer [75], 40 out of 80 adults with terminal cancer [76], and 124 out of 260 cancer patients receiving chemotherapy [77]. When the results from these three trials were subject to meta-analysis, a heterogeneous, nonsignificant effect was found (SMD = 2.01, 95 % CI −0.09 to 4.11, P = 0.06). Paradoxically, this nonsignificance actually resulted from a much larger beneficial effect reported in the study by Zhong [77] than that reported in the studies by Burns [75] and Hilliard [76]. When the results from the Burns and Hilliard studies were subject to meta-analysis (N = 88), this resulted in a homogenous and significant effect of MT on QOL (SMD = 1.02, 95 %CI 0.58 to 1.47, P = 0.00001). One interesting aspect of the Hilliard study was that even as the physical health of the patients in the music group declined, QOL scores improved. This was not the case in the control group, in whom QOL scores worsened as their physical health declined [76].
Table 4.
Individual studies investigating the effect of music-based interventions on QOL in either oncologic or palliative care settings
| Author, year, type of study | Study population | Music intervention | Control | N music group | N control group | Results |
|---|---|---|---|---|---|---|
| Hanser, 2006, RCTa [57] | Metastatic breast cancer patients (outpatient setting) | MT: three 45-min sessions consisting of live music, improvisation, and songwriting | Standard care | 20 | 22 | No significant improvement in QOL detected using the 136-point FACT-G scale. Although the music group’s mean score rose from 75.4 to 78.9, and the control group’s mean score only rose from 82.2 to 83.1, P > 0.05 |
| Burns, 2001, RCTa [75] | Adult outpatients with cancer | MT: 10 weekly 90–120-min sessions of the Bonny Method of Guided Imagery and “specially sequenced Western Art” music | Wait-list group | 4 | 4 | No significant improvement in QOL detected using 100-point QOL-Cancer Scale. Although the music group’s mean score rose from 75.40 to 91.77, and control group’s mean score only rose from 76.02 to 77.85, P > 0.05 |
| Hilliard, 2003, RCTa [76] | Adults with terminal cancer (setting: home hospice) | MT: 2–13 weekly/biweekly MT sessions of varying lengths. Techniques included singing, lyric analysis, instrument playing, song parody, planning of funerals, song gifts | Standard care | 40 | 40 | Significant improvement in QOL detected using 280-point Hospice QOL Index-Revised scale (P < 0.05). Music group’s mean score rose from 206.8 to 214.6, while control group’s mean score fell from 188.5 to 177.9 |
| Zhong and Gang, 2001, RCTa [77] | Adult cancer patients receiving chemotherapy | MM: twice daily 60-min sessions for 20 days | Standard care | 124 | 136 | Significant improvement in QOL detected using QOL Questionnaire for Chinese patients (P < 0.01). Music group’s mean score fell slightly from 49.2 to 47.2, while control group’s mean score fell from 49.9 to 34.5 |
MM music medicine, MT music therapy
aIncluded in 2011 Cochrane Review [13]
Clearly, more research is needed to investigate the impact of music on QOL. Given the crucial importance of this outcome to cancer patients in palliative care settings, future studies investigating the effect of music-based interventions on pain, anxiety, or mood disturbance in this patient population should incorporate QOL measurements into their outcome assessment.
Relevant advances in neurobiology
Previous speculations regarding the potential mechanisms of music-based interventions may have drastically oversimplified an extremely complex set of possible neurobiological processes [78]. Many investigators have proposed that music may compete with noxious stimuli and thereby close neurological gates of pain signal transmission, or that it may distract patients from threats that cause them to feel anxious, and/or that it may promote a sense of well-being in patients with an otherwise depressed mood. While these may all be valid theories, advances in neuroscience, and functional neuroimaging studies in particular, are providing dramatic new insights into the findings from clinical trials involving music-based interventions (Table 5).
Table 5.
Individual studies and review articles investigating the neurobiology of music, pain, anxiety, and depression
| Author, year | Description | Findings |
|---|---|---|
| Becerra et al., 2001 [79] | fMRI was used to examine changes in neural activation due to painful thermal stimuli (delivered to the skin of the left hand through a Peltier-based thermode at 46 °C) in 8 healthy male subjects, who rated their pain levels using a Visual Analog Scale | Two temporal phases of pain response were observed: early and late. During the early phase, increased signal was seen in reward regions such as the left anterior nucleus acccumbens (NAc), the ventral tegmentum (VT), the periaqueductal gray (PAG), the sublenticular extended amygdala (SLEA) of the basal forebrain, and the orbital gyrus. In the late response, decreased signal was seen in the left posterior NAc, while increased signal was seen in classical pain regions such as the thalamus, S1, insula, and anterior cingulate gyrus |
| Blood et al., 1999 [110] | PET was used to examine changes in regional cerebral blood flow (rCBF) related to emotional responses to music. Ten musicians were exposed to 6 versions of a novel musical passage varying systematically in degree of dissonance | Subjective pleasantness and unpleasantness ratings were correlated with consonance and dissonance, respectively. Increasing consonance was correlated with increasing activity in the orbitofrontal cortex, frontal polar cortex, and the subcallosal cingulate gyrus. Increasing dissonance was correlated with increasing activity in the precuneus region and the right parahippocampal gyrus |
| Blood and Zatorre, 2001 [97] | PET was used to examine changes in rCBF related to “intensely pleasant emotional responses to music” manifesting as piloerective chills measured by electrodermal monitoring. Ten musicians were exposed to self-selected music, control music, amplitude-matched noise, and silence. rCBF values were extracted from individual scans and plotted against chill intensity | Increasing chill intensity was correlated with increasing activity in the left ventral striatum (including the NAc) and dorsomedial midbrain (including the PAG), and decreasing activity in the right amygdala, left hippocampus, and ventral medial prefrontal cortex |
| Engel et al., 2009 [82] | This article reviews findings from multiple neuroimaging studies using fMRI, PET, and radioligand binding experiments to investigate anxiety in healthy subjects as well as patients with panic disorder, generalized anxiety disorder, social anxiety disorder, and specific phobias | Enhancement of activity in the amygdala was a very common finding. Enhanced activity was also commonly found in the prefrontal cortex, insula, and the anterior cingulate cortex |
| Menon and Levitin, 2005 [98] | High-resolution fMRI was used to examine changes in neural activation due to “passive music listening.” Fourteen non-musicians were exposed to 10 intact samples of music and 10 scrambled samples for control stimuli. Hemodynamic changes were subject to statistical, functional connectivity, and effective connectivity analyses | Passive listening to music resulted in significant activation of multiple specific structures including the NAc, the VTA, and the hypothalamus. Functional connectivity analysis showed that responses in the NAc and the VTA were highly correlated, “suggesting an association between dopamine release and NAc response to pleasant music” |
| Nestler and Carlezon, 2005 [85] | This article reviews the mesolimbic dopamine reward circuit in depression. Data from animal studies and some human studies are discussed | The authors discuss how abnormalities in the VTA and NAc may be related to depressive symptoms such as anhedonia, reduced motivation, decreased energy level, etc. Roles of specific proteins, such as the transcription factor cAMP response element binding protein (CREB) and the endogenous kappa-opioid receptor agonist Dynorphin are reviewed |
| Pereira, 2011 [106] | fMRI was used to investigate blood oxygenation level dependence (BOLD) responses to musical stimuli that varied according to participant familiarity and preference. Fourteen non-musicians underwent a listening test which consisted of 15 s excerpts from 110 pop/rock songs which they rated by degree of familiarity and preference. During fMRI, the participants were then exposed to 48 excerpts, with 12 excerpts from each of the following categories based upon the listening test results: familiar liked, familiar unliked, unfamiliar liked, and unfamiliar unliked | Familiarity was found to have a greater impact than preference in triggering BOLD responses in the following emotion-related regions: putamen, amygdala, NAc, anterior cingulate cortex, and thalamus |
| Salimpoor et al., 2011 [100] | Ligand-based PET was used to estimate dopamine release in the striatum based on the competition between endogenous dopamine and [11C] raclopride for binding to D2 dopamine receptors. Information about the dynamics of dopamine release over time was collected using fMRI. Eight participants were exposed to self-selected pleasurable musical excerpts versus neutral musical excerpts. Electrodermal skin conductance was used to measure piloerective chills while participants provided subjective feedback about degree of listening pleasure | Compared to neutral musical excerpts, pleasurable musical stimuli (concurrently measured by chill intensity and subjective participant ratings) resulted in distinct striatal responses detectable by PET and fMRI. Ligand-based PET data revealed increased endogenous dopamine transmission, as indicated by decreased [11C] raclopride binding potential in the right NAc. fMRI showed increased BOLD response in the right NAc during peak pleasure experience epochs |
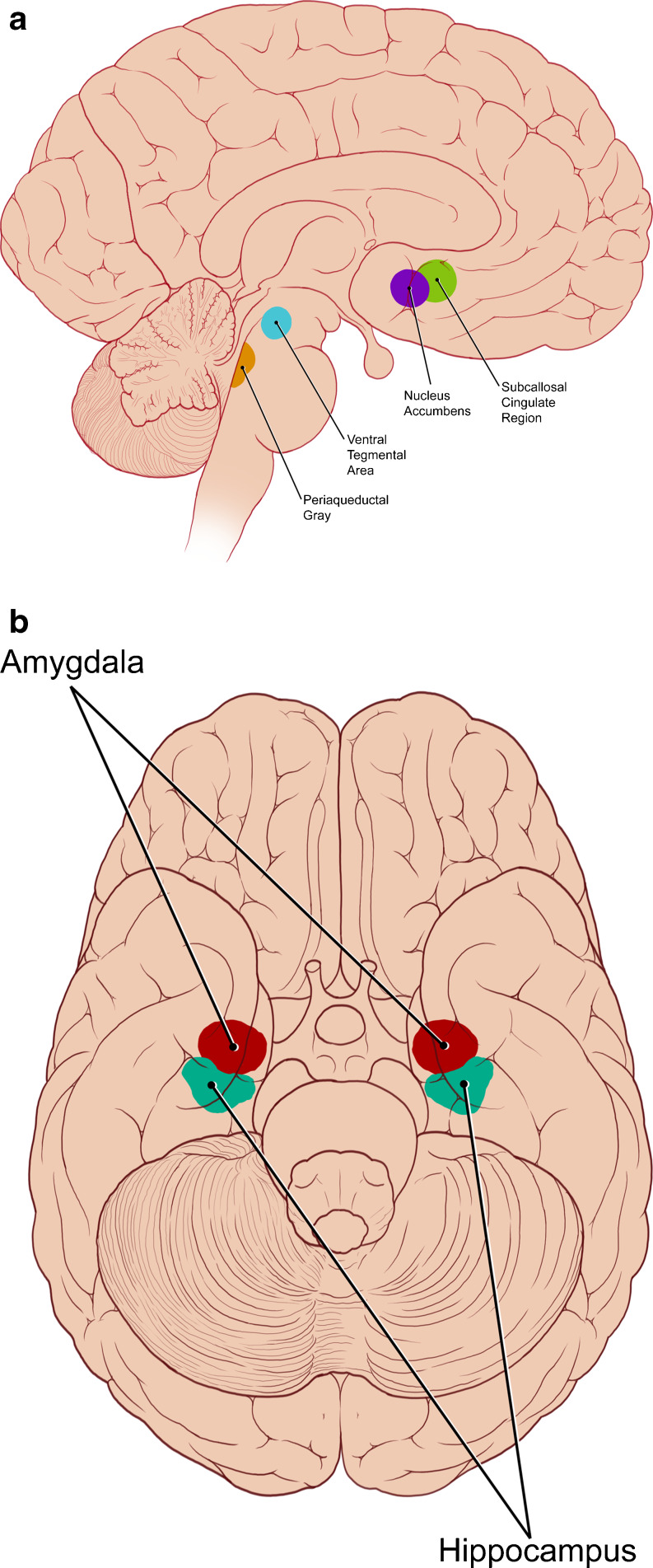
Multiple studies have explored changes in activity within the brains of healthy, asymptomatic adults upon exposure to music. Broadly speaking, functional imaging data have shown that music modulates the activity of multiple limbic and paralimbic brain structures, but especially the ventral striatum (including the nucleus accumbens), the dorsomedial midbrain (including the ventral tegmental area and periaqueductal gray), the amygdala, and the hippocampus (Fig. 1a, b). This particular neuroanatomic distribution is striking for at least two reasons. The first is that functional abnormalities in these same structures are implicated in the pathophysiology of pain [79–81], anxiety [82–84], and depression [85–87]. The second is that these same structures are known to be densely populated by receptors of ligands associated with pain, anxiety, and depression—namely, endogenous opioids [88, 89], GABA [90, 91], and dopamine [92, 93].
Fig. 1.
a Sagittal view of neuroanatomic regions affected by music (and implicated in the pathophysiology of pain, anxiety, and/or depression). b Inferior view of neuroanatomic regions affected by music (and implicated in the pathophysiology of pain, anxiety, and/or depression)
Listening to music has long been known to evoke strong emotional responses which can sometimes be accompanied by physical manifestations, e.g., piloerection, more commonly known as “goosebumps” or “chills” [94, 95]. The suppression of this response with the mu-opioid receptor agonist nalaxolone provided early evidence that endogenous opioid activity might underlie pleasurable responses to music [96]. Positron emission tomography experiments subsequently showed that piloerection in response to music may be associated with increased regional cerebral blood flow to the ventral striatum and the dorsomedial midbrain but decreased regional cerebral blood flow (rCBF) to the hippocampus and amygdala [97]. Even in the absence of piloerective responses, fMRI evidence suggested that consonant musical excerpts may increase activity in the ventral striatum and the anterior insula [98, 99], while dissonant excerpts may increase activity in the amygdala and hippocampus [99]. Data collected from [11C] raclopride PET demonstrated that intensely pleasurable responses to music may be associated with dopamine release in the striatal system [100]. This dopaminergic activity in the NAc following exposure to music (and other pleasurable stimuli, e.g., sex, food, and drugs of abuse) may itself be modulated by endogenous opioids [101]. Furthermore, evidence from animal models suggests that opioid efferent projections from the NAc may directly mediate reward-related behavior [102]. Within the dorsomedial midbrain (which was found to receive increased rCBF during highly pleasurable musical experiences as shown in [97]), the substructure known as the periaqueductal gray has been shown to be densely populated with endogenous opioid receptors and may be involved in both opioid-mediated reward [103] and analgesia [79, 104]. Preliminary research suggests that the action of endogenous opioids in the PAG may be influenced by the hormone oxytocin [105]; the blood concentrations of which was found to be increased (along with subjective relaxation) in perioperative patients exposed to soothing music [106]. Although multiple functional imaging studies have shown music to modulate the activity of the amygdala [97, 107], and multiple functional imaging studies have demonstrated an association between anxiety and enhanced amygdalar activity [82, 83, 108, 109], no radioligand binding experiments have specifically investigated the effect of music on gamma amino-butyric acid activity in the brain. With regard to mood disturbance, it is worth noting that music has been shown to modulate the activity of the subcallosal cingulate region [107, 110], an area which has been shown to have decreased rCBF in patients with depression [111]. Furthermore, deep brain stimulation of the subcallosal cingulate region has been shown to be an effective treatment for severe depression [86]. Finally, platelet concentrations of serotonin, which may correlate with neuronal concentrations of serotonin [112, 113], were found to be increased in humans exposed to euphonic music, but decreased in humans exposed to cacophonic music [114].
Overall, these advances in neurobiology suggest that music may affect specific neuronal pathways that are implicated in the pathophysiology of pain, anxiety, and depression. Thus, future neurobiological studies may provide objective insight into the mechanisms by which music may affect these subjective symptoms that commonly afflict patients with cancer.
Conclusions
In 2002, the WHO approved the following definition of palliative care: “An approach that improves the quality of life of patients and their families facing the problems associated with life-threatening illness, through the prevention and relief of suffering by means of early identification and impeccable assessment and treatment of pain and other problems, physical, psychosocial and spiritual” [115]. In the future, music-based interventions may prove to become valuable tools in the “relief of suffering” of cancer patients. Specifically, music may help alleviate pain, anxiety, and mood disturbance, all of which commonly occur in cancer, and all of which may be associated with impaired QOL. The potential of music to reduce the need for analgesics and/or anxiolytics, even if only by a small amount, may still have major clinical implications, especially given the frequency with which advanced age and hepato-renal dysfunction coexist in the palliative cancer care population (and hence their predisposition to pharmacologic toxicity). Furthermore, when the only pharmacologic agents available for mood disturbance take weeks to months to take effect, interventions that provide more immediate benefits, even if modest, may warrant further investigation.
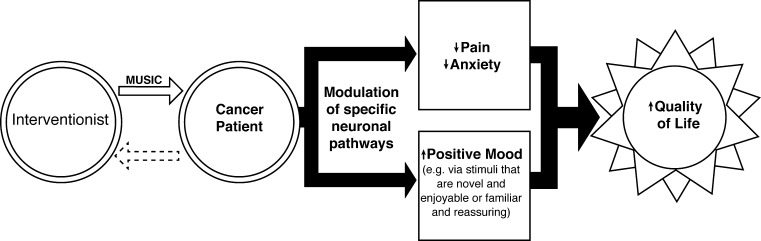
It is not difficult to imagine how, for cancer patients unfamiliar with the standard inpatient healthcare environment, the hospital setting could be associated with unexpected pain (e.g., from repeated injections, blood draws, and other invasive procedures), anxiety (e.g., from loud equipment alarms and time-constrained conversations regarding prognosis often clouded by medical jargon), and even depression (e.g., related to the existential issues of having a life-threatening illness, limited social interaction, frequently interrupted sleep, etc.). The capacity of music to restore a sense of familiarity, and the therapeutic value of such a reassuring stimulus (regardless of where a patient may be in his or her disease trajectory), may be underestimated. Such reassuring familiarity could be provided in the form of a playlist of favorite songs on a portable mp3 player with headphones or even through melodic arrangement by a live music therapist that actually incorporates tones from the surrounding environment [116]. It should not necessarily be assumed that the benefits of music are limited to the relief of symptoms; that is to say, that music merely counteracts the negative consequences of disease (Fig. 2). The need for beauty (and for some, spiritual solace) may be particularly great toward the end of life for many patients. In this respect, music may exceed where standard pharmacologic means fall short. Many qualitative studies support both the potential symptom-alleviating and wellness-promoting effects of music [3, 10, 117–125]. However, quantitative data in these areas still remain limited.
Fig. 2.
General conceptual model for the potentially therapeutic impact(s) of music-based interventions in cancer patients
In the absence of more RCTs with larger sample sizes, meta-analyses [13, 20, 126] can provide useful quantitative assessments of impact. However, controlling for variation in study design, study population, specific intervention(s), and outcome assessment methods, presents enormous challenges. For example, different music therapists can introduce variability in outcomes, even when the same specific interventions are used [127]. The data presented in the individual trials and the meta-analyses discussed in this review should therefore be considered preliminary and interpreted with caution. The statistical quality of the data in question remains diminished by high risk of bias, which almost invariably arises from the inherent difficulties associated with conventional blinding in music-based intervention studies. Furthermore, without reliable biomarkers for pain, anxiety, and depression, defining the “gold standard” in quantitative assessment of these outcomes remains formidable. Fortunately, the cost of music-based interventions remains relatively low [128], and breakthroughs in the field of neurobiology continue to advance our understanding of the anatomical and biochemical basis of how music works in the brain, and why symptoms such as pain, anxiety, and mood disturbance might be influenced.
Further investigation is warranted to determine (1) if certain subpopulations of cancer patients are more likely to respond to music-based interventions than others, (2) what interventions are most effective for such responsive patients, and (3) what measurement parameters best gauge their effectiveness. Greater collaboration between the fields of music therapy and music neuroscience may accelerate the pursuit of these objectives. Finally, given the emerging evidence that earlier involvement of palliative care may improve outcomes in certain cancer patients [129], and that psychological stress may be linked to up-regulation of inflammatory processes that promote tumor growth and angiogenesis [130–133], it follows that research into the potential of music to specifically promote relaxation and reduce stress [134], perhaps earlier in cancer’s trajectory, may also be warranted.
Acknowledgments
Thanks to David Aten of MDACC Medical Graphics & Photography for illustrating all figures and to Mei Dong and Biquan Luo for the help with translation.
Conflict of Interest
I have no financial relationships to disclose. I have full control over the content of this article. I submit the entirety of this manuscript for review by Supportive Care in Cancer.
References
- 1.Smith EM, Gomm SA. Assessing the independent contribution to quality of life from anxiety and depression in patients with advanced cancer. Palliat Med. 2003;17(6):509–509. doi: 10.1191/0269216303pm781oa. [DOI] [PubMed] [Google Scholar]
- 2.Ferrell BR. The impact of pain on quality of life. A decade of research. Nurs Clin N Am. 1995;30(4):609–624. [PubMed] [Google Scholar]
- 3.O’Callaghan C. Objectivist and constructivist music therapy research in oncology and palliative care. Music Med. 2009;1(1):41–60. [Google Scholar]
- 4.Olofsson A, Fossum B. Perspectives on music therapy in adult cancer care: a hermeneutic study. Oncol Nurs Forum. 2009;36(4):1–10. doi: 10.1188/09.ONF.E223-E231. [DOI] [PubMed] [Google Scholar]
- 5.Gallagher L, Lagman R, Walsh D, Davis M, LeGrand S. The clinical effects of music therapy in palliative medicine. Support Care Cancer. 2006;14(8):859–866. doi: 10.1007/s00520-005-0013-6. [DOI] [PubMed] [Google Scholar]
- 6.Stanczyk MM. Music therapy in supportive cancer care. Rep Pract Oncol Radiother. 2011;16(5):170–172. doi: 10.1016/j.rpor.2011.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Trondalen G, Bonde LO. Music therapy: models and interventions. In: MacDonald R, Kreutz G, Mitchell L, editors. Music, health, and wellbeing. New York: Oxford University Press; 2012. pp. 40–64. [Google Scholar]
- 8.Dileo C. Music therapy and medicine: theoretical and clinical applications. Silver Spring: American Music Therapy Association; 1999. [Google Scholar]
- 9.Bruscia K. Defining music therapy. 2. Gilsum: Barcelona; 1998. [Google Scholar]
- 10.Munro S, Mount B. Music therapy in palliative care. Can Med Assoc J. 1978;119(9):1029–1034. [PMC free article] [PubMed] [Google Scholar]
- 11.van den Beuken-van EM, de Rijke J, Kessels A, Schouten H, van Kleef M, Patijn J. Prevalence of pain in patients with cancer: a systematic review of the past 40 years. Ann Oncol. 2007;18(9):1437–1449. doi: 10.1093/annonc/mdm056. [DOI] [PubMed] [Google Scholar]
- 12.Higginson IJ, Murtagh F. Cancer pain epidemiology. In: Bruera E, Portenoy RK, editors. Cancer pain: assessment and management. New York: Cambridge University Press; 2010. pp. 37–52. [Google Scholar]
- 13.Bradt J, Dileo C, Grocke D, Magill L (2011) Music interventions for improving psychological and physical outcomes in cancer patients. Cochrane Database of Systematic Reviews (8). doi:10.1002/14651858 [DOI] [PubMed]
- 14.Binns-Turner P. Perioperative music and its effects on anxiety, hemodynamics, and pain in women undergoing mastectomy. Birmingham: University of Alabama; 2008. [PubMed] [Google Scholar]
- 15.Danhauer SC, Vishnevsky BA, Campbell CR, McCory TP, Tooze JA, Kanipe KN, Arrington SA, Holland EK, Lynch MB, Hurd DD, Cruz J. Music for patients with hematological malignancies undergoing bone marrow biopsy: a randomized controlled study of anxiety, perceived pain, and patient satisfaction. J Soc Integr Oncol. 2010;8(4):140–147. [PMC free article] [PubMed] [Google Scholar]
- 16.Huang S. The effects of music on cancer pain. Cleveland: Case Western Reserve University; 2006. [Google Scholar]
- 17.Nguyen TN, Nilsson S, Hellstrom A, Bengtson A. Music therapy to reduce pain and anxiety in children with cancer undergoing lumbar puncture: a randomized clinical trial. J Pediatr Oncol Nurs. 2010;27:146–155. doi: 10.1177/1043454209355983. [DOI] [PubMed] [Google Scholar]
- 18.Yonghui W, Zongfu M, Yanru Q. Influence of music therapy on anxiety, depression and pain of cancer patients. Chin Nurs Res. 2009;13:1172–1175. [Google Scholar]
- 19.Cepeda MS, Carr DB, Lau J, Alvarez H (2006) Music for pain relief. Cochrane Database of Systematic Reviews 2:CD004843 [DOI] [PubMed]
- 20.Rudin D, Kiss A, Wetz RV, Sottile VM. Music in the endoscopy suite: a meta-analysis of randomized controlled studies. Endoscopy. 2007;39:507–510. doi: 10.1055/s-2007-966362. [DOI] [PubMed] [Google Scholar]
- 21.Smolen D, Topp R, Singer L. The effect of self-selected music during colonoscopy on anxiety, heart rate, and blood pressure. Appl Nurs Res. 2002;15(3):126–136. doi: 10.1053/apnr.2002.34140. [DOI] [PubMed] [Google Scholar]
- 22.Lee DWH, Chan K-W, Poon C-M, Ko C-W, Chan K-H, Sin K-S, Sze T-S, Chan ACW. Relaxation music decreases the dose of patient-controlled sedation during colonoscopy: a prospective randomized controlled trial. Gastrointest Endosc. 2002;55(1):33–36. doi: 10.1067/mge.2002.120387. [DOI] [PubMed] [Google Scholar]
- 23.Schiemann U, Gross M, Reuter R. Improved procedure of colonoscopy under accompanying music therapy. Eur J Med Res. 2002;7:131–134. [PubMed] [Google Scholar]
- 24.Stark D, Kiely M, Smith A, Velikova G, House A, Selby P. Anxiety disorders in cancer patients: their nature, associations, and relation to quality of life. J Clin Oncol. 2002;20(14):3137–3148. doi: 10.1200/JCO.2002.08.549. [DOI] [PubMed] [Google Scholar]
- 25.Zimmerman L, Story KT, Gaston-Johansson F, Rowles JR. Psychological variables and cancer pain. Cancer Nurs. 1996;19:44–53. doi: 10.1097/00002820-199602000-00006. [DOI] [PubMed] [Google Scholar]
- 26.Mystakidou K, Tsilika E, Parpa E, Katsouda E, Galanos A, Vlahos L. Psychological distress of patients with advanced cancer: influence and contribution of pain severity and pain interference. Cancer Nurs. 2006;29:400–405. doi: 10.1097/00002820-200609000-00009. [DOI] [PubMed] [Google Scholar]
- 27.Lin C-C, Lai Y-L, Ward SE. Effect of cancer pain on performance status, mood states, and level of hope among Taiwanese cancer patients. J Pain Symptom Manag. 2003;25(1):29–37. doi: 10.1016/s0885-3924(02)00542-0. [DOI] [PubMed] [Google Scholar]
- 28.Dahl A, Haaland C, Mykletun A, Bremnes R, Dahl O, Klepp O, Wist E, Fosså S. Study of anxiety disorder and depression in long-term survivors of testicular cancer. J Clin Oncol. 2005;23(10):2389–2395. doi: 10.1200/JCO.2005.05.061. [DOI] [PubMed] [Google Scholar]
- 29.Brintzenhofe-Szoc KM, Levin TT, Li Y, Kissane DW, Zabora JR. Mixed anxiety/depression symptoms in a large cancer cohort: prevalence by cancer type. Psychosomatics. 2009;50(4):383–391. doi: 10.1176/appi.psy.50.4.383. [DOI] [PubMed] [Google Scholar]
- 30.Kolva E, Rosenfeld B, Pessin H, Breitbart W, Brescia R. Anxiety in terminally ill cancer patients. J Pain Symptom Manag. 2011;42(5):691–701. doi: 10.1016/j.jpainsymman.2011.01.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Teunissen SCCM, de Graeff A, Voest EE, de Haes JCJM. Are anxiety and depressed mood related to physical symptom burden? A study in hospitalized advanced cancer patients. Palliat Med. 2007;21(4):341–346. doi: 10.1177/0269216307079067. [DOI] [PubMed] [Google Scholar]
- 32.Spencer R, Nilsson M, Wright A, Pirl W, Prigerson H. Anxiety disorders in advanced cancer patients. Cancer. 2010;116(7):1810–1819. doi: 10.1002/cncr.24954. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Wilson KGC HM, Graham SM, Allard P, Chary S, Gagnon P, Macmillan K, De Luca M, O'Shea F, Kuhl D, Fainsinger RL, Clinch JJ. Depression and anxiety disorders in palliative cancer care. J Pain Symptom Manag. 2007;33(2):118–129. doi: 10.1016/j.jpainsymman.2006.07.016. [DOI] [PubMed] [Google Scholar]
- 34.Bufalini A. Role of interactive music in oncological pediatric patients undergoing painful procedures. Minerva Pediatr. 2009;61(4):379–389. [PubMed] [Google Scholar]
- 35.Bulfone T, Quattrin R, Zanotti R, Regattin L, Brusaferro S. Effectiveness of music therapy for anxiety reduction in women with breast cancer in chemotherapy treatment. Holist Nurs Pract. 2009;23(4):238–242. doi: 10.1097/HNP.0b013e3181aeceee. [DOI] [PubMed] [Google Scholar]
- 36.Harper EI. Reducing treatment-related anxiety in cancer patients: comparison of psychological interventions. Dallas: Southern Methodist University; 2001. [Google Scholar]
- 37.Smith M, Casey L, Johnson D, Gwede C, Riggin OZ. Music as a therapeutic intervention for anxiety in patients receiving radiation therapy. Oncol Nurs Forum. 2001;28(5):855–862. [PubMed] [Google Scholar]
- 38.Cooke M, Chaboyer W, Schluter P, Hiratos M. The effect of music on preoperative anxiety in day surgery. J Adv Nurs. 2005;52(1):47–55. doi: 10.1111/j.1365-2648.2005.03563.x. [DOI] [PubMed] [Google Scholar]
- 39.Nilsson U, Rawal N, Unosson M. A comparison of intra-operative or postoperative exposure to music—a controlled trial of the effects on postoperative pain. Anaesthesia. 2003;58(7):699–703. doi: 10.1046/j.1365-2044.2003.03189_4.x. [DOI] [PubMed] [Google Scholar]
- 40.Nilsson U, Unosson M, Rawal N. Stress reduction and analgesia in patients exposed to calming music postoperatively: a randomized controlled trial. Eur J Anaesthesiol. 2005;22(2):96–102. doi: 10.1017/s0265021505000189. [DOI] [PubMed] [Google Scholar]
- 41.Voss J, Good M, Yates B, Baun M, Thompson A, Hertzog M. Sedative music reduces anxiety and pain during chair rest after open-heart surgery. Pain. 2004;112(1–2):197–203. doi: 10.1016/j.pain.2004.08.020. [DOI] [PubMed] [Google Scholar]
- 42.Horne-Thompson A, Grocke D. The effect of music therapy on anxiety in patients who are terminally ill. J Palliat Med. 2008;11(4):582–590. doi: 10.1089/jpm.2007.0193. [DOI] [PubMed] [Google Scholar]
- 43.Bringman H, Giesecke K, ThÖRne A, Bringman S. Relaxing music as pre-medication before surgery: a randomised controlled trial. Acta Anaesthesiol Scand. 2009;53(6):759–764. doi: 10.1111/j.1399-6576.2009.01969.x. [DOI] [PubMed] [Google Scholar]
- 44.McHugh P, Lewis S, Ford S, Newlands E, Rustin G, Coombes C, Smith D, O'Reilly S, Fallowfield L. The efficacy of audiotapes in promoting psychological well-being in cancer patients: a randomised, controlled trial. Br J Cancer. 1995;71(2):388–392. doi: 10.1038/bjc.1995.79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Noyes RJ, Holt C, Massie M. Anxiety disorders. In: Holland J, editor. Psycho-oncology. New York: Oxford University Press; 1998. pp. 548–563. [Google Scholar]
- 46.Hinton J. Psychiatric consultation in fatal illness. Proc R Soc Med. 1972;65(11):1035. doi: 10.1177/003591577206501164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Bukberg JB, Holland JC. A prevalence study of depression in a cancer hospital population. Proc Am Assoc Cancer Res. 1980;21:382. [Google Scholar]
- 48.Derogatis L, Morrow G, Fetting J, Penman D, Piasetsky S, Schmale A, Henrichs M, Carnicke C. The prevalence of psychiatric disorders among cancer patients. JAMA: J Am Med Assoc. 1983;249(6):751–757. doi: 10.1001/jama.249.6.751. [DOI] [PubMed] [Google Scholar]
- 49.Chochinov H, Wilson K, Enns M. Prevalence of depression in the terminally ill: effects of diagnostic criteria and symptom threshold judgements. Am J Psychiatry. 1994;151:537–540. doi: 10.1176/ajp.151.4.537. [DOI] [PubMed] [Google Scholar]
- 50.Craig TJ, Abeloff MD. Psychiatric symptomatology among hospitalized cancer patients. Am J Psychiatr. 1974;131(12):1323–1327. [PubMed] [Google Scholar]
- 51.Achute K, Vauhkonen ML. Cancer and psyche. Helsinki: Kunnallispaino; 1970. [Google Scholar]
- 52.Peck A. Emotional reactions to having cancer. Am J Roentgenol. 1972;114(3):591–599. doi: 10.2214/ajr.114.3.591. [DOI] [PubMed] [Google Scholar]
- 53.Mitchell AJ, Chan M, Bhatti H, Halton M, Grassi L, Johansen C, Meader N. Prevalence of depression, anxiety, and adjustment disorder in oncological, haematological, and palliative-care settings: a meta-analysis of 94 interview-based studies. Lancet Oncol. 2011;12(2):160–174. doi: 10.1016/S1470-2045(11)70002-X. [DOI] [PubMed] [Google Scholar]
- 54.Guangrong C, Yi Q, Peiwen L. Music therapy in treatment of cancer patients. Chin Ment Heal J. 2001;15(3):179–181. [Google Scholar]
- 55.Cassileth BR, Vickers AJ, Magill LA. Music therapy for mood disturbance during hospitalization for autologous stem cell transplantation. Cancer. 2003;98(12):2723–2729. doi: 10.1002/cncr.11842. [DOI] [PubMed] [Google Scholar]
- 56.Clark M, Isaacks-Downton G, Wells N, Redlin-Frazier S, Eck C, Hepworth J, Chakravarthy B. Use of preferred music to reduce emotional distress and symptom activity during radiation therapy. J Music Ther. 2006;43(3):247–265. doi: 10.1093/jmt/43.3.247. [DOI] [PubMed] [Google Scholar]
- 57.Hanser SB. Effects of a music therapy intervention on quality of life and distress in women with metastatic breast cancer. J Soc Integr Oncol. 2006;4(3):116–124. doi: 10.2310/7200.2006.014. [DOI] [PubMed] [Google Scholar]
- 58.Beck S (1989) The effect of therapeutic use of music on cancer related pain. PhD thesis, University of Utah, Salt Lake City
- 59.Duocastella AC. Effect of music on children with cancer. Revista de Enfermeria. 1999;22(4):293–298. [PubMed] [Google Scholar]
- 60.de Haes JC, Van Knippenberg FC. The quality of life of cancer patients: a review of the literature. Soc Sci Med. 1985;20(8):809–817. doi: 10.1016/0277-9536(85)90335-1. [DOI] [PubMed] [Google Scholar]
- 61.Brucker PS, Yost K, Cashy J, Webster K, Cella D. General Population and cancer patient norms for the Functional Assessment of Cancer Therapy-General (FACT-G) Eval Health Prof. 2005;28(2):192–211. doi: 10.1177/0163278705275341. [DOI] [PubMed] [Google Scholar]
- 62.Hammerlid E, Taft C. Health-related quality of life in long-term head and neck cancer survivors: a comparison with general population norms. Br J Cancer. 2001;84(2):149–156. doi: 10.1054/bjoc.2000.1576. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Donovan KA, Thompson LM, Jacobsen PB. Pain, depression, and anxiety in cancer. In: Moore RJ, editor. Handbook of pain and palliative care: biobehavioral approaches for the life course. Heidelberg: Springer; 2012. pp. 615–637. [Google Scholar]
- 64.Padilla GV, Ferrell B, Grant MM, Rhiner M. Defining the content domain of quality of life for cancer patients with pain. Cancer Nurs. 1990;13:108–115. [PubMed] [Google Scholar]
- 65.Wang XS, Cleeland CS, Mendoza TR, Engstrom MC, Liu S, Xu G, Hao X, Wang Y, Ren XS. The effects of pain severity on health-related quality of life. Cancer. 1999;86(9):1848–1855. [PubMed] [Google Scholar]
- 66.Berthold DR, Pond GR, Roessner M, de Wit R, Eisenberger M, Tannock I. Treatment of hormone-refractory prostate cancer with docetaxel or mitoxantrone: relationships between prostate-specific antigen, pain, and quality of life response and survival in the TAX-327 Study. Clin Cancer Res. 2008;14(9):2763–2767. doi: 10.1158/1078-0432.CCR-07-0944. [DOI] [PubMed] [Google Scholar]
- 67.Breivik H, Cherny N, Collett B, de Conno F, Filbet M, Foubert A, Cohen R, Dow L. Cancer-related pain: a pan-European survey of prevalence, treatment, and patient attitudes. Ann Oncol. 2009;20(8):1420–1433. doi: 10.1093/annonc/mdp001. [DOI] [PubMed] [Google Scholar]
- 68.So W, Marsh G, Ling W, Leung F, Lo J, Yeung M, Li G. The symptom cluster of fatigue, pain, anxiety, and depression and the effect on the quality of life of women receiving treatment for breast cancer: a multicenter study. Oncol Nurs Forum. 2009;36(4):E205–E214. doi: 10.1188/09.ONF.E205-E214. [DOI] [PubMed] [Google Scholar]
- 69.Skarstein J, Aass N, Fosså S, Skovlund E, Dahl A. Anxiety and depression in cancer patients: relation between the Hospital Anxiety and Depression Scale and the European Organization for Research and Treatment of Cancer Core Quality of Life Questionnaire. J Psychosom Res. 2000;49(1):27–34. doi: 10.1016/s0022-3999(00)00080-5. [DOI] [PubMed] [Google Scholar]
- 70.Saevarsdottir T, Fridriksdottir N, Gunnarsdottir S. Quality of life and symptoms of anxiety and depression of patients receiving cancer chemotherapy: longitudinal study. Cancer Nurs. 2010;33(1):E1–E10. doi: 10.1097/NCC.0b013e3181b4adb5. [DOI] [PubMed] [Google Scholar]
- 71.Pereira MG, Figueiredo AP, Fincham FD. Anxiety, depression, traumatic stress and quality of life in colorectal cancer after different treatments: a study with Portuguese patients and their partners. Eur J Oncol Nurs. 2012;16(3):227–232. doi: 10.1016/j.ejon.2011.06.006. [DOI] [PubMed] [Google Scholar]
- 72.Payne S. A study of quality of life in cancer patients receiving palliative chemotherapy. Soc Sci Med. 1992;35(12):1505–1509. doi: 10.1016/0277-9536(92)90053-s. [DOI] [PubMed] [Google Scholar]
- 73.Grassi L, Indelli M, Marzola M, Maestri A, Santini A, Piva E, Boccalon M. Depressive symptoms and quality of life in home-care-assisted cancer patients. J Pain Symptom Manag. 1996;12(5):300–307. doi: 10.1016/s0885-3924(96)00181-9. [DOI] [PubMed] [Google Scholar]
- 74.Brown L, Kroenke K, Theobald D, Wu J, Tu W. The association of depression and anxiety with health-related quality of life in cancer patients with depression and/or pain. Psycho-Oncology. 2010;19(7):734–741. doi: 10.1002/pon.1627. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Burns D. The effect of the bonny method of guided imagery and music on the mood and life quality of cancer patients. J Music Ther. 2001;38(1):51–65. doi: 10.1093/jmt/38.1.51. [DOI] [PubMed] [Google Scholar]
- 76.Hilliard R. The effects of music therapy on the quality and length of life of people diagnosed with terminal cancer. J Music Ther. 2003;40(2):113–137. doi: 10.1093/jmt/40.2.113. [DOI] [PubMed] [Google Scholar]
- 77.Zhong X, Gang H. Effect of music therapy and relaxation inner image on quality of life in cancer patients receiving chemotherapy. Chinese Mental Health J. 2001;15(3):176–178. [Google Scholar]
- 78.Koelsch S. A neuroscientific perspective on music therapy. Ann N Y Acad Sci. 2009;1169(1):374–384. doi: 10.1111/j.1749-6632.2009.04592.x. [DOI] [PubMed] [Google Scholar]
- 79.Becerra L, Breiter HC, Wise R, Gonzalez RG, Borsook D. Reward circuitry activation by noxious thermal stimuli. Neuron. 2001;32(5):927. doi: 10.1016/s0896-6273(01)00533-5. [DOI] [PubMed] [Google Scholar]
- 80.Chen A. New perspectives in EEG/MEG brain mapping and PET/fMRI neuroimaging of human pain. Int J Psychophysiol. 2001;42(2):147–159. doi: 10.1016/s0167-8760(01)00163-5. [DOI] [PubMed] [Google Scholar]
- 81.Millan MJ. Descending control of pain. Prog Neurobiol. 2002;66(6):355–474. doi: 10.1016/s0301-0082(02)00009-6. [DOI] [PubMed] [Google Scholar]
- 82.Engel K, Bandelow B, Gruber O, Wedekind D. Neuroimaging in anxiety disorders. J Neural transm. 2009;116(6):703–716. doi: 10.1007/s00702-008-0077-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Stein MB, Simmons AN, Feinstein JS, Paulus MP. Increased amygdala and insula activation during emotion processing in anxiety-prone subjects. Am J Psychiatry. 2007;164:318–327. doi: 10.1176/ajp.2007.164.2.318. [DOI] [PubMed] [Google Scholar]
- 84.Martin EI, Ressler KJ, Binder E, Nemeroff CB. The neurobiology of anxiety disorders: brain imaging, genetics, and psychoneuroendocrinology. Psychiatr Clin N Am. 2009;32:549–575. doi: 10.1016/j.psc.2009.05.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Nestler EJ, Carlezon WA. The mesolimbic dopamine reward circuit in depression. Biol Psychiatry. 2006;59(12):1151–1159. doi: 10.1016/j.biopsych.2005.09.018. [DOI] [PubMed] [Google Scholar]
- 86.Mayberg HS. Limbic-cortical dysregulation: a proposed model of depression. J Neuropsychiatry Clin Neurosci. 1997;9(3):471–481. doi: 10.1176/jnp.9.3.471. [DOI] [PubMed] [Google Scholar]
- 87.Drevets WC, Price JL, Bardgett ME, Reich T, Todd RD, Raichle ME. Glucose metabolism in the amygdala in depression: relationship to diagnostic subtype and plasma cortisol levels. Pharmacol Biochem Behav. 2002;71(3):431–447. doi: 10.1016/s0091-3057(01)00687-6. [DOI] [PubMed] [Google Scholar]
- 88.Koneru A, Satyanarayana S, Rizwan S. Endogenous opioids: their physiological role and receptors. Global J Pharmacol. 2009;3(3):149–153. [Google Scholar]
- 89.Akil H, Watson SJ, Young E, Lewis ME, Khachaturian H, Walker JM. Endogenous opioids: biology and function. Annu Rev Neurosci. 1984;7(1):223–255. doi: 10.1146/annurev.ne.07.030184.001255. [DOI] [PubMed] [Google Scholar]
- 90.McDonald AJ, Mascagni F, Muller JF. Immunocytochemical localization of GABABR1 receptor subunits in the basolateral amygdala. Brain Res. 2004;1018(2):147–158. doi: 10.1016/j.brainres.2004.05.053. [DOI] [PubMed] [Google Scholar]
- 91.Gray JA, McNaughton N. The neuropsychology of anxiety: an enquiry into the functions of the septo-hippocampal system. Oxford Psychology Series. 2. New York: Oxford University Press; 2003. [Google Scholar]
- 92.Levey AI, Hersch SM, Rye DB, Sunahara RK, Niznik HB, Kitt CA, Price DL, Maggio R, Brann MR, Ciliax BJ. Localization of D1 and D2 dopamine receptors in brain with subtype-specific antibodies. Proc Natl Acad Sci U S A. 1993;90(19):8861–8865. doi: 10.1073/pnas.90.19.8861. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Dailly E, Chenu F, Renard CE, Bourin M. Dopamine, depression and antidepressants. Fundam Clin Pharmacol. 2004;18(6):601–607. doi: 10.1111/j.1472-8206.2004.00287.x. [DOI] [PubMed] [Google Scholar]
- 94.Panksepp J. The emotional sources of “chills” induced by music. Music Percept. 1995;13(2):171–207. [Google Scholar]
- 95.Khalfa S, Peretz I, Blondin J, Manon R. Event-related skin conductance responses to musical emotions in humans. Neurosci Lett. 2002;328(2):145–149. doi: 10.1016/s0304-3940(02)00462-7. [DOI] [PubMed] [Google Scholar]
- 96.Goldstein A. Thrills in response to music and other stimuli. Physiol Psychol. 1980;8(1):126–129. [Google Scholar]
- 97.Blood AJ, Zatorre RJ. Intensely pleasurable responses to music correlate with activity in brain regions implicated in reward and emotion. Proc Natl Acad Sci. 2001;98(20):11818–11823. doi: 10.1073/pnas.191355898. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Menon V, Levitin DJ. The rewards of music listening: response and physiological connectivity of the mesolimbic system. NeuroImage. 2005;28(1):175–184. doi: 10.1016/j.neuroimage.2005.05.053. [DOI] [PubMed] [Google Scholar]
- 99.Koelsch S, Fritz T, Müller K, Friederici AD. Investigating emotion with music: an fMRI study. Human Brain Mapp. 2005;27(3):239–250. doi: 10.1002/hbm.20180. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Salimpoor VN, Benovoy M, Larcher K, Dagher A, Zatorre RJ. Anatomically distinct dopamine release during anticipation and experience of peak emotion to music. Nat Neurosci. 2011;14(2):257–262. doi: 10.1038/nn.2726. [DOI] [PubMed] [Google Scholar]
- 101.Bardo M. Neuropharmacological mechanisms of drug reward: beyond dopamine in the nucleus accumbens. Crit Rev Neurobiol. 1998;12:37–67. doi: 10.1615/critrevneurobiol.v12.i1-2.30. [DOI] [PubMed] [Google Scholar]
- 102.Gardner EL, Vorel SR. Cannabinoid transmission and reward-related events. Neurobiol Dis. 1998;5(6):502–533. doi: 10.1006/nbdi.1998.0219. [DOI] [PubMed] [Google Scholar]
- 103.Olmstead MC, Franklin KBJ. The development of a conditioned place preference to morphine: effects of micro-injections into various CNS sites. Behav Neurosci. 1997;111:1324–1334. doi: 10.1037//0735-7044.111.6.1324. [DOI] [PubMed] [Google Scholar]
- 104.Pavlovic ZW, Bodnar RJ. Opioid supraspinal analgesic synergy between the amygdala and periaqueductal gray in rats. Brain Res. 1998;779(1–2):158–169. doi: 10.1016/s0006-8993(97)01115-3. [DOI] [PubMed] [Google Scholar]
- 105.Yang J, Liang J-Y, Li P, Pan Y-J, Qiu P-Y, Zhang J, Hao F, Wang D-X. Oxytocin in the periaqueductal gray participates in pain modulation in the rat by influencing endogenous opiate peptides. Peptides. 2011;32(6):1255–1261. doi: 10.1016/j.peptides.2011.03.007. [DOI] [PubMed] [Google Scholar]
- 106.Nilsson U. Soothing music can increase oxytocin levels during bed rest after open-heart surgery: a randomised control trial. J Clin Nurs. 2009;18(15):2153–2161. doi: 10.1111/j.1365-2702.2008.02718.x. [DOI] [PubMed] [Google Scholar]
- 107.Pereira CS, Teixeira J, Figueiredo P, Xavier J, Brattico E. Music and emotions in the brain: familiarity matters. PLoS One. 2011;6(11):e27241. doi: 10.1371/journal.pone.0027241. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 108.Phan KL, Wager T, Taylor SF, Liberzon I. Functional neuroanatomy of emotion: a meta-analysis of emotion activation studies in PET and fMRI. NeuroImage. 2002;16(2):331. doi: 10.1006/nimg.2002.1087. [DOI] [PubMed] [Google Scholar]
- 109.Somerville LH, Kim H, Johnstone T, Alexander AL, Whalen PJ. Human amygdala responses during presentation of happy and neutral faces: correlations with state anxiety. Biol Psychiatry. 2004;55(9):897–903. doi: 10.1016/j.biopsych.2004.01.007. [DOI] [PubMed] [Google Scholar]
- 110.Blood AJ, Zatorre RJ, Bermudez P, Evans AC. Emotional responses to pleasant and unpleasant music correlate with activity in paralimbic brain regions. Nat Neurosci. 1999;2(4):382–382. doi: 10.1038/7299. [DOI] [PubMed] [Google Scholar]
- 111.Drevets WC, Price JL, Simpson JR, Todd RD, Reich T, Vannier M, Raichle ME. Subgenual prefrontal cortex abnormalities in mood disorders. Nature. 1997;386(6627):824–827. doi: 10.1038/386824a0. [DOI] [PubMed] [Google Scholar]
- 112.Stahl SM. The human platelet: a diagnostic research tool for the study of biogenic amines in psychiatric and neurologic disorders. Arch Gen Psychiatry. 1977;34:509–516. doi: 10.1001/archpsyc.1977.01770170019001. [DOI] [PubMed] [Google Scholar]
- 113.Pletscher A. Platelets as models for monoaminergic neurons. In: Youdim MBH, editor. Essays in neurochemistry and neuropharmacology. London: Wiley; 1978. pp. 49–101. [PubMed] [Google Scholar]
- 114.Evers S, Suhr B. Changes of the neurotransmitter serotonin but not of hormones during short time music perception. Eur Arch Psychiatry Clin Neurosci. 2000;250(3):144–147. doi: 10.1007/s004060070031. [DOI] [PubMed] [Google Scholar]
- 115.Organization WH (2013) http://www.who.int/cancer/palliative/definition/en/. Accessed 30 March 2012
- 116.Rosetti A (2011) Treating stress, speech disorders with music. NPR Science Friday (December 16)
- 117.Magill L. The use of music therapy to address the suffering in advanced cancer pain. J Palliat Care. 2001;17(3):167. [PubMed] [Google Scholar]
- 118.Daykin N, Bunt L, McClean S. Music and healing in cancer care: a survey of supportive care providers. Arts Psychother. 2006;33(5):402–413. [Google Scholar]
- 119.Magill-Levreault L. Music therapy in pain and symptom management. J Palliat Care. 1993;9(4):42–48. [PubMed] [Google Scholar]
- 120.O'Kelly J, Koffman J. Multidisciplinary perspectives of music therapy in adult palliative care. Palliat Med. 2007;21(3):235–241. doi: 10.1177/0269216307077207. [DOI] [PubMed] [Google Scholar]
- 121.Mandel SE. The role of the music therapist on the hospice/palliative care team. J Palliat Care. 1993;9(4):37–39. [PubMed] [Google Scholar]
- 122.Munro S. Music therapy in palliative/hospice care. New York: Magnamusic-Baton; 1984. [Google Scholar]
- 123.Hilliard RE. The use of music therapy in meeting the multidimensional needs of hospice patients and families. J Palliat Care. 2001;17(3):161–166. [PubMed] [Google Scholar]
- 124.Dileo C, Loewy JV. Music therapy at the end of life. Cherry Hill: Jeffrey; 2005. [Google Scholar]
- 125.Von Hodenberg F. Music therapy with patients undergoing radiation and chemotherapy. Lonely waters. Oxford: Sobell; 1995. pp. 61–67. [Google Scholar]
- 126.Bradt J, Dileo C (2010) Music therapy for end-of-life care. Cochrane Database of Systematic Reviews (1). doi:10.1002/14651858.CD007169.pub2 [DOI] [PubMed]
- 127.Kain ZN, Caldwell-Andrews AA, Krivutza DM, Weinberg ME, Gaal D, Wang S-M, Mayes LC. Interactive music therapy as a treatment for preoperative anxiety in children: a randomized controlled trial. Anesth Analg. 2004;98(5):1260–1266. doi: 10.1213/01.ane.0000111205.82346.c1. [DOI] [PubMed] [Google Scholar]
- 128.Romo R, Gifford L. A cost-benefit analysis of music therapy in a home hospice. Nurs Econ. 2007;25(6):353–358. [PubMed] [Google Scholar]
- 129.Temel J, Greer J, Muzikansky A, Gallagher E, Admane SJ VA, Dahlin C, Blinderman C, Jacobsen J, Pirl W, Billings J, Lynch T. Early palliative care for patients with metastatic non-small-cell lung cancer. N Engl J Med. 2010;363(8):733–742. doi: 10.1056/NEJMoa1000678. [DOI] [PubMed] [Google Scholar]
- 130.Thaker P, Han L, Kamat A, Arevalo J, Takahashi R, Lu C, Jennings N, Armaiz-Pena G, Bankson J, Ravoori M, Merritt W, Lin Y, Mangala L, Kim T, Coleman R, Landen C, Li Y, Felix E, Sanguino A, Newman R, Lloyd M, Gershenson D, Kundra V, Lopez-Berestein G, Lutgendorf S, Cole S, Sood A. Chronic stress promotes tumor growth and angiogenesis in a mouse model of ovarian carcinoma. Nat Med. 2006;12(8):939–944. doi: 10.1038/nm1447. [DOI] [PubMed] [Google Scholar]
- 131.Cohen L, Cole SW, Sood AK, Prinsloo S, Kirschbaum C, Arevalo JMG, Jennings NB, Scott S, Vence L, Wei Q, Kentor D, Radvanyi L, Tannir N, Jonasch E, Tamboli P, Pisters L. Depressive symptoms and cortisol rhythmicity predict survival in patients with renal cell carcinoma: role of inflammatory signaling. PLoS One. 2012;7(8):e42324. doi: 10.1371/journal.pone.0042324. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 132.Moreno-Smith M, Lutgendorf SK, Sood AK. Impact of stress on cancer metastasis. Futur Oncol. 2010;6(12):1863–1881. doi: 10.2217/fon.10.142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 133.Armaiz-Pena GN, Lutgendorf SK, Cole SW, Sood AK. Neuroendocrine modulation of cancer progression. Brain, Behav Immun. 2009;23(1):10–15. doi: 10.1016/j.bbi.2008.06.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Yehuda N. Music and stress. J Adult Develop. 2011;18(2):85–94. [Google Scholar]