Abstract
As prevalence of metabolic syndrome has rapidly increased over the past decade, lifestyle changes including dietary habits are considered as a therapeutic cornerstone for metabolic syndrome, cardiovascular complications and type 2 diabetes. We evaluated the effectiveness of a telephone-delivered nutrition education to improve metabolic parameters compared with a single-visit with a dietitian in subjects with metabolic syndrome. A total of seventy-one adults who met diagnostic criteria for the metabolic syndrome were randomly assigned to either the single-visit group or the in-depth nutrition education group during a 3-month intervention study period. The in-depth telephone-delivered nutrition education group had an initial visit with a dietitian and additional two telephone counseling during the first 4 weeks of the study periods. Sixty-six subjects completed a 3-month intervention study. The trial examined participant's anthropometric changes and dietary intakes as well as changes in the metabolic syndrome factors. At the end of the trial, the in-depth nutrition education group showed significantly higher reduction in weight, body fat and abdominal circumference compared with the other group (p < 0.05). In the in-depth nutrition groups, the prevalence of metabolic syndrome was decreased to 45.5%, while 69.7% of the subjects were metabolic syndrome patients in the single-visit group (p < 0.05). These results demonstrate that the telephone-intervention counseling is a feasible mean to deliver dietary intervention in patients with metabolic syndrome.
Keywords: Telephone intervention, Metabolic syndrome, Nutrition therapy
Introduction
Improvements in standards of living and changes in dietary habits have resulted in changes in disease incidence and causes of death in Korea. The incidence of coronary artery disease has rapidly increased over the past decade, and cardiovascular disease has been ranked the first as a cause of death [1]. The prevalence of metabolic syndrome, which is a dependent factor of cardiovascular disease, is approximately 30% among adults older than 30 years of age [2]. In patients with metabolic syndrome who have several concomitant diseases, the incidence of developing coronary artery disease is 2 times higher and that of type 2 diabetes is 6-folds of healthy individuals resulting in 2 to 4 times higher mortality rate among metabolic syndrome patients [3,4]. Accordingly, metabolic syndrome has a great effect on medical expenses and quality of life, and implementation of a systematic nutrition education program is required to prevent and manage metabolic syndrome.
Medical nutrition therapy (MNT) involves implementation of effective nutrition education while considering environmental factors, eating habits, and the clinical state of patients to promote changes in life styles. The MNT protocol for patients with various chronic diseases, including diabetes [5-7], hypertension [8-10], and hyperlipidemia [11-13], is suggested on the basis of nutrition assessment, diagnosis, intervention, and the monitoring/evaluation process as well as in-depth nutrition education with one-time basic education and 2 or 3 additional nutritional counseling sessions, considering the personal state of the patient.
MNT provided by a professional dietician according to the standardized MNT protocol is required to maximize benefits while reducing the enormous medical expenses associated with the treatment of patients with chronic diseases. However, a follow-up nutrition education, which is designed to promote implementation of nutrition treatment for patients, involves face-to-face interviews and thereby requires patients to visit hospitals, takes too much time, and has associated issues of cost and convenience.
Accordingly, the continuous provision of information is required to manage patients with chronic diseases, and several telehealth methods, such as mail, internet, and telephone counseling as communication channels, have been suggested [14,15]. When nutrition education occurs online, health information can be provided with ease at a lower cost and with convenient access without time constraints, but a proper treatment adjustment according to the status of the patient can be limited. Telephone counseling is a part of linguistic persuasion, which improves behavioral changes and self-efficacy and is currently provided for self-management of patients with diabetes as a method of increasing compliance [16]. The advantages of telephone counseling are easy access, facilitation of feedback by interaction, monitoring, and positive reinforcement of the patient's level of knowledge, correction of distorted awareness, and implementation of a directed diet [17,18]. Therefore, telephone counseling can be used to facilitate nutrition treatment follow-up management with the merits of time saving and reduction of medical expenses [19]. Although the effectiveness of MNT on several diseases has been studies extensively, few studies have examined the effects of MNT on metabolic syndrome by telephone counseling. Therefore, the aim of this study was to evaluate the effectiveness of dietary management through nutrition education and telephone counseling in clinical index and nutrient intake for patients with metabolic syndrome in Korea.
Materials and Methods
Recruitment and subjects eligibility
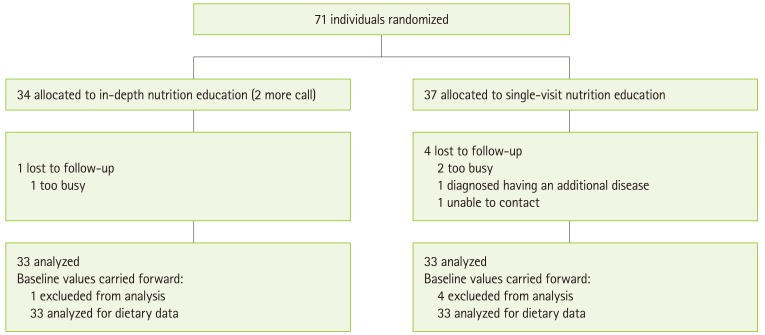
This research was designed for patients who visited the health promotion center of a university hospital located in Gyeonggi-do from September to December 2011 for medical checkups. The diagnostic criteria for metabolic syndrome were in accordance with the National Cholesterol Education Program Adult Treatment Panel III (NCEP-ATP III) and the WHO Asia-Pacific obesity abdominal circumference diagnosis, and the study subjects had more than 3 types of risk factors for metabolic syndrome [20]. The diagnostic criteria for metabolic syndrome were as follows: an abdominal circumference greater than 90 cm and 80 cm for men and women, respectively; blood triglyceride levels greater than 150 mg/dL; a high-density lipoprotein (HDL) cholesterol level less than 40 mg/dL and 50 mg/dL for men and women, respectively; systolic/diastolic blood pressure greater than 130/85 mmHg; and a fasting blood glucose level greater than 100 mg/dL. This randomized, comparative clinical research study was conducted in 71 participants who agreed to participate. Subjects who were diagnosed with a stroke or angina in the past 3 months, had a history of surgery or incontrollable cancer, were participating in other nutrition education programs, and had dietary disorders were excluded. Using the hospital registration number, the research subjects were randomized into the single-visit nutrition education group (37 persons) and the in-depth nutrition education group (34 persons). During 3 months, all five subjects dropped out for personal reasons; 3 subjects were dismissed due to busy working schedule, and 1 subject was dismissed due to need to start medication for other disease, 1 subject was dropped out for losing follow up. The final total of 66 subjects was retained for 3 months of study and completed the ending study visit (Figure 1). This study was approved by the Bundang Seoul National University Institutional Review Board and written informed consent was obtained from each subject.
Figure 1.
The flow diagram of study participants.
Study design
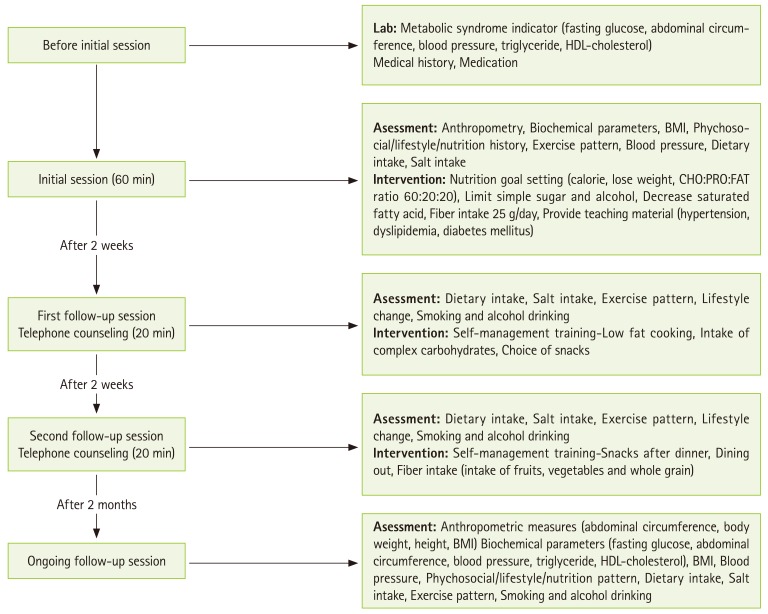
Initial nutrition education was provided to both groups, and follow-up nutrition education was provided only to subjects in the in-depth nutrition education group through two telephone counselings apart by 2 weeks during the first 4 weeks of trial. A registered dietitian conducted MNT for 3 months according to a modified protocol for metabolic syndrome patients based on MNT protocol for diabetic patients which is established by the American Dietetic Association [21,22]. Figure 2 presents details on the MNT protocol. The initial nutrition education was performed to enable basic self-management through calories counting by using food exchange table and meal pattern management. For in-depth nutrition education group, during follow-up nutrition education, acceptance and understanding were evaluated, considering life styles including dietary habits, and clinical state; in addition, customized education was evaluated through proper feedback and focused on encouraging maintenance of dietary changes according to the dietary guide and individual personal risk factors.
Figure 2.
Protocol of medical nutrition therapy.
Nutritional assessment
Subjects completed a questionnaire regarding general characteristics and life styles including smoking history, drinking history, and dietary habits. Anthropometric and biochemical assessment were performed twice, before initial nutrition education and 3-month later. Height and weight were measured using an automatic height/weight measuring machine (GL-150P; G-Tech International, Korea), with the subject in an erect posture, barefoot in light clothing. Height was measured by 0.1 cm with a linear height measuring machine, and weight, percentage of body fat, and muscle mass were measured with a device that applies the impedance method by part through the multi-frequency method (Inbody 3.0; Biospace, Korea). Body mass index (BMI) was calculated by dividing the subject's weight by the square of the height. For the abdominal circumference, the lowest rib part and the middle part of the upper pelvis crista iliaca were measured by 0.1 cm units using a measuring tape. Blood pressure was calculated using an average after maintaining a stable state in a sitting posture for 5 minutes and measuring the systolic and diastolic blood pressure twice using an automatic blood pressure gauge (Sysmex XE-2100; Sysmex, Japan). Blood glucose, total cholesterol, triglyceride, HDL cholesterol, and low-density lipoprotein cholesterol levels were analyzed using an autoanalyzer (Autoanalyzer Hitachi 747; Hitachi Ltd., Japan) after deserting 15 mL of venous blood at room temperature for more than 60 minutes since 12-hour vacant stomach and separating serum through 15-minute centrifugal separation at 2,500 rpm for 15 minutes. The homeostasis model assessment of insulin resistance (HOMA-IR) was calculated as follows:
| HOMA-IR = fasting insulin (µ/mL) × fasting plasma glucose (mmol/L)/22.5. |
Analysis of food intake was performed for all subjects before initial nutrition education and used the 24-hour recall method; the dish names, materials, and quantities of food were recorded. Dietary intakes for all participants were reevaluated by the 24-hour recall method 3 months after the education. A nutrition management program, CAN-Pro (Computer Aided Nutritional analysis program, version 4.0) was used to conduct analyses on nutrient intakes.
Statistical analysis
SPSS (Statistical Package for Social Sciences, version 12.0) was used to analyze the data. Statistical differences between the single-visit nutrition education group and the in-depth nutrition education group were verified with t-test and χ2 test. Changes in the anthropometric, biochemical data, and nutrient intake as a result of education were evaluated by the paired t-test. All clinical variables were shown in the average ± standard deviation or percentage, and p < 0.05 indicated statistical significance.
Results
General characteristics
The general characteristics of study subjects are provided in Table 1. The ages of the subjects were 48.1 ± 12.3 in the single-visit nutrition education group and 48.6 ± 13.4 in the in-depth nutrition education group, and there were 19 men (57.6%) in the the single-visit nutrition education group and 16 men (48.5%) in the in-depth nutrition education group. There was similar distribution of general characteristics such as age and sex between the two groups without a significant difference.
Table 1.
General characteristics of the subjects
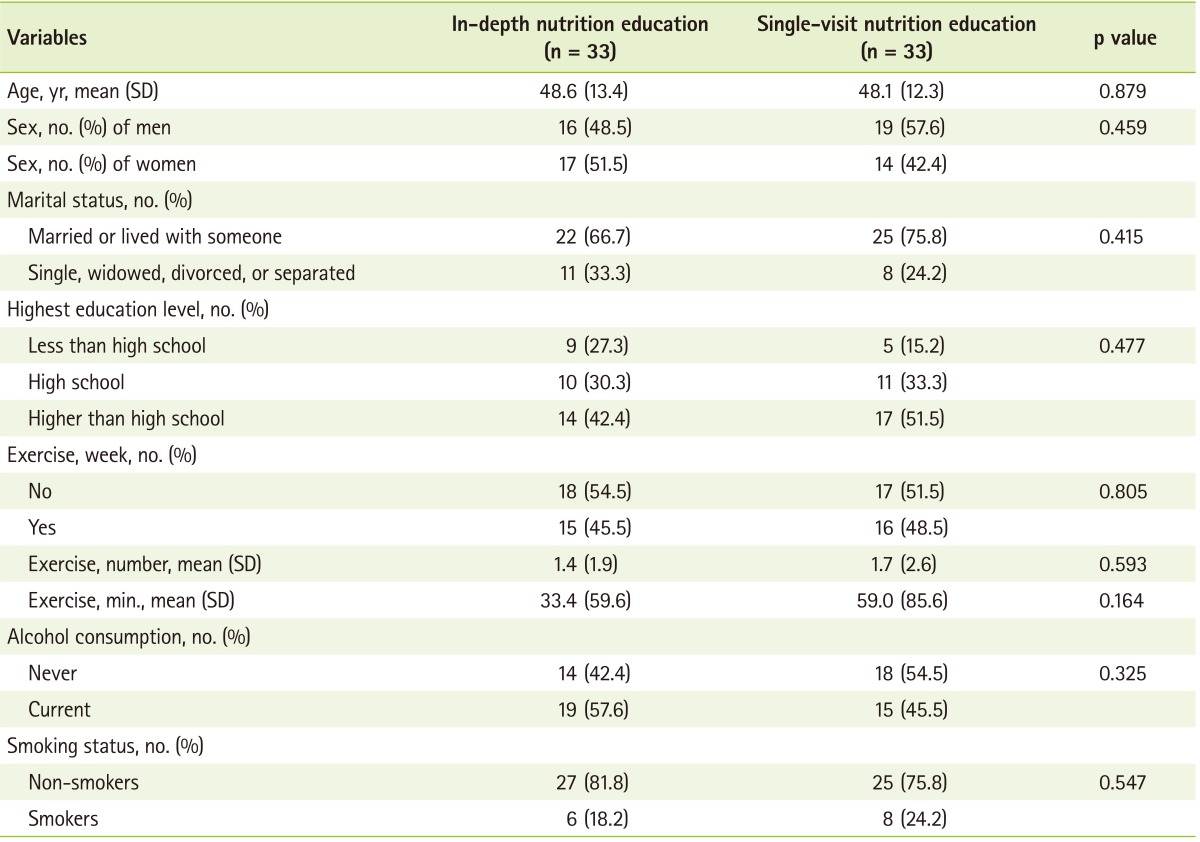
p value; t-test and χ2 test.
A total of 48.5% and 45.5% of the single-visit nutrition education group and of the in-depth nutrition education group exercised, respectively and 45.5% in the single-visit nutrition education group and 57.6% in the in-depth nutrition education group currently consumed alcohol. A total of 75.8% in the single-visit nutrition education group and 81.8% in the in-depth nutrition education group were non-smokers, and there was a similar distribution between the two groups in regard to exercise, drinking, and smoking behaviors without a significant difference.
Analysis of dietary intakes
Table 2 lists nutrients and calorie intake before and after nutrition education using the 24-hour recall method. Calorie intake compared with prescription quantity decreased significantly from 104.2% to 86.4% in the single-visit nutrition education group and from 112.2% to 102.2% in the in-depth nutrition education group (p < 0.05). Carbohydrate intake also decreased from 283.9 g/d to 242.5 g/d and 294.5 g/d to 233.8 g/d in the in-depth nutrition education group and in the single-visit nutrition education group, respectively (p < 0.05). Carbohydrate, protein, and fat intake compared with total calorie intake were not significantly different in both groups.
Table 2.
Changes in caloric and nutrient intake at baseline and 3-month follow-up of intervention
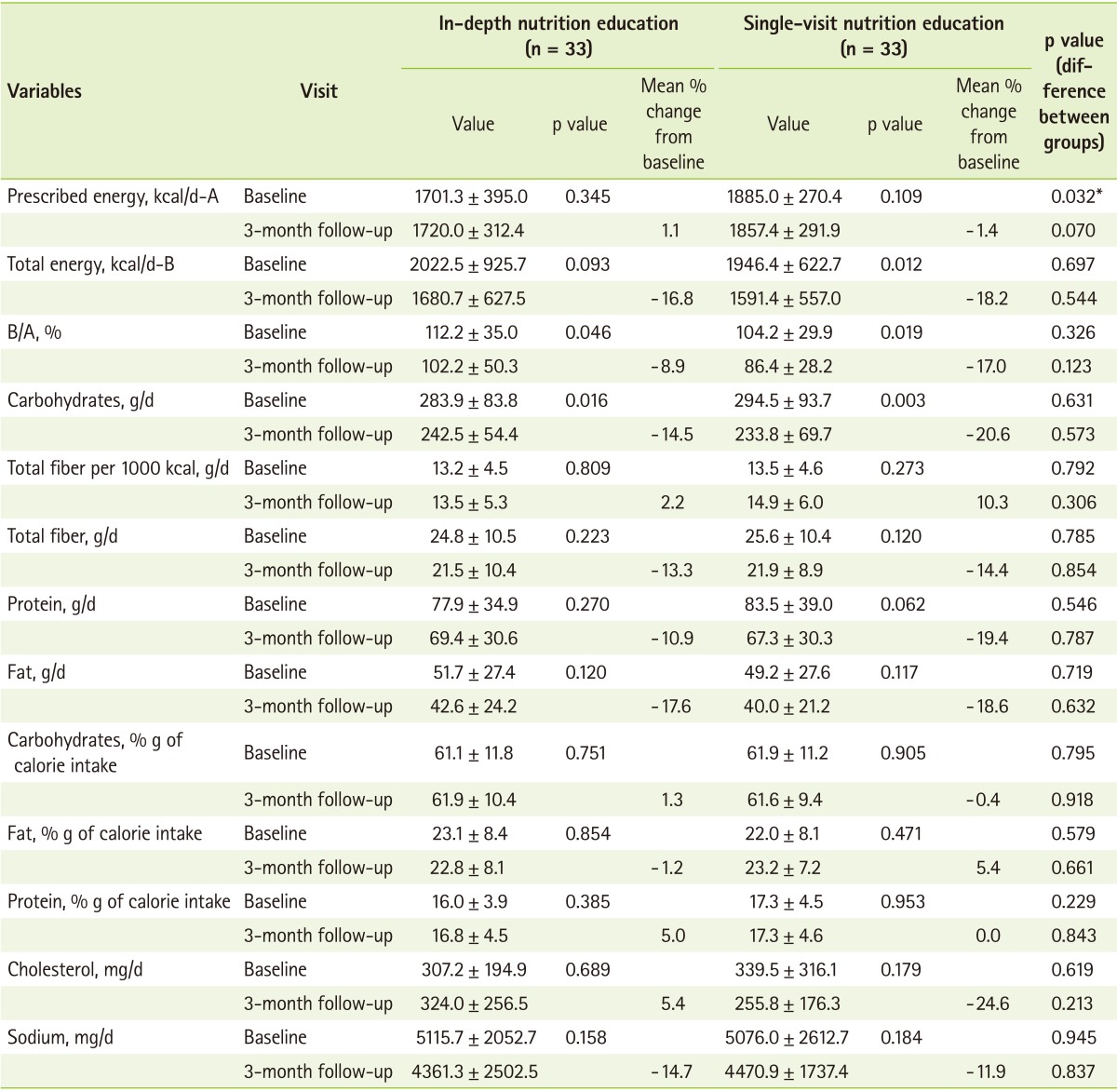
Values are presented as mean ± SD.
B/A: total energy/prescribed energy.
*Comparing the values between groups using unpaired t-test.
calorie intake were not significantly different in both groups.
Physical and biochemical measurements of study subjects are shown in Table 3. At baseline, there was no significant difference between two groups in both anthropometric and biochemical measurements. The average body weight was changed from 76.2 ± 14.5 kg to 75.4 ± 15.0 kg in the single-visit nutrition education group and body fat was changed from 29.0 ± 7.4% to 29.3 ± 5.7%, which was not significant. In the in-depth nutrition education group, body weight and abdominal circumference was reduced significantly after 3 months (p = 0.05). At initial assessment, the BMI in the single-visit nutrition education group and the in-depth nutrition education group was 27.0 ± 2.7 kg/m2 and 26.0 ± 3.5 kg/m2, respectively, which is greater than the average obesity criteria in Korea (25 kg/m2), and change of BMI after education was significantly different only in the in-depth nutrition education group (p < 0.05). Changes in systolic blood pressure were not significantly decreased in both groups, and diastolic blood pressure increased from 70.9 ± 2.2 mmHg to 77.4 ± 2.2 mmHg in the in-depth nutrition education group, which was below the diagnostic criteria of metabolic syndrome.
Table 3.
Changes in intervention diets on cardiovascular risk variables at baseline and 3-month follow-up of intervention
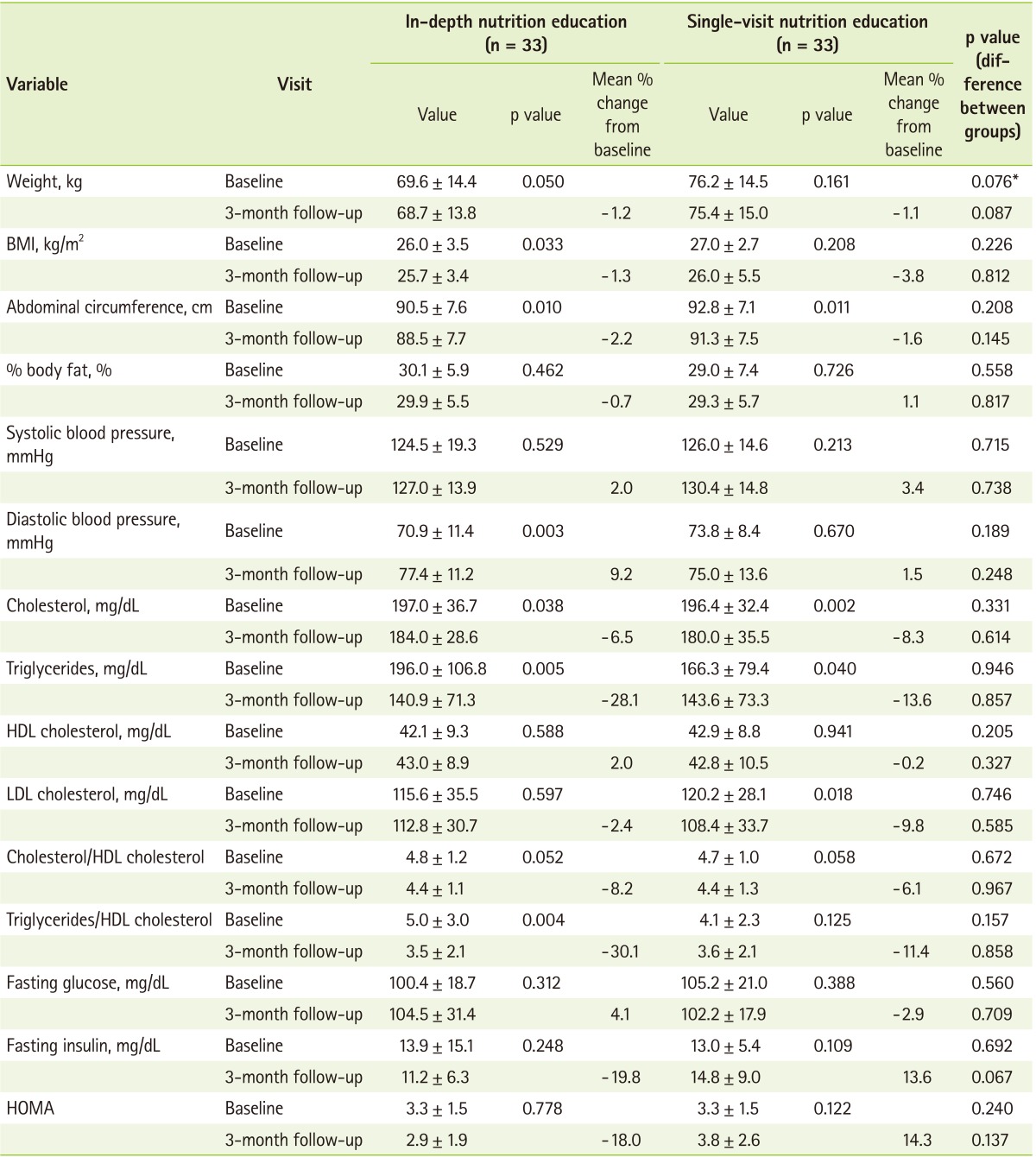
Values are presented as mean ± SD.
HOMA: homeostasis model assessment.
*Comparing the values between groups using unpaired t-test.
In the in-depth nutrition education group, the cholesterol concentration decreased by 6.58% from 197.0 ± 36.7 mg/dL to 184.0 ± 28.6 mg/dL (p < 0.05) and the triglyceride value also decreased from 196.0 ± 106.8 mg/dL to 140.9 ± 71.3 mg/dL, which is below the diagnostic criteria (p < 0.01). The cholesterol/HDL-cholesterol ratio in the in-depth nutrition education group and the single-visit nutrition education group decreased by 6.1% and 8.2%, respectively after the intervention. The triglyceride/HDL-cholesterol ratio decreased by 30.1% in the in-depth nutrition education group, but there was no significant difference in the single-visit nutrition education group.
Prevalence changes of metabolic syndrome
The prevalence changes of metabolic syndrome by nutrition treatment are shown in Table 4. In the in-depth nutrition education group, fasting blood glucose, triglyceride, HDL-cholesterol, blood pressure, and abdominal circumference was account for 14.3% (16 items), 19.6% (22 items), 21.4% (24 items), 19.6% (22 items), and 25.0% (28 items), respectively in a total of 112 metabolic syndrome risk factors. Following 3 month of MNT, the total number of risk factors decreased to 85 items in the in-depth nutrition education group, in which fasting blood glucose, triglyceride, HDL-cholesterol, blood pressure, and abdominal circumference were decreased by 17.6% (15 items), 12.9% (11 items), 20.0% (17 items), 23.5% (20 items), and 25.9% (22 items), respectively. In the single-visit nutrition education group, fasting blood glucose, triglyceride, HDL-cholesterol, blood pressure, and abdominal circumference were decreased by 17.2% (17 items), 19.2% (19 items), 21.2% (21 items), 16.2% (16 items), and 26.3% (26 items), which showed that the total number of risk factors of metabolic syndrome decreased to 99 items. Over the 3 month intervention period, the changes in prevalence of metabolic syndrome were significantly different between two groups (in-depth nutrition education group: 45.5% vs. in the single-visit nutrition education group: 69.7%) (p < 0.05).
Table 4.
Change in metabolic syndrome factors
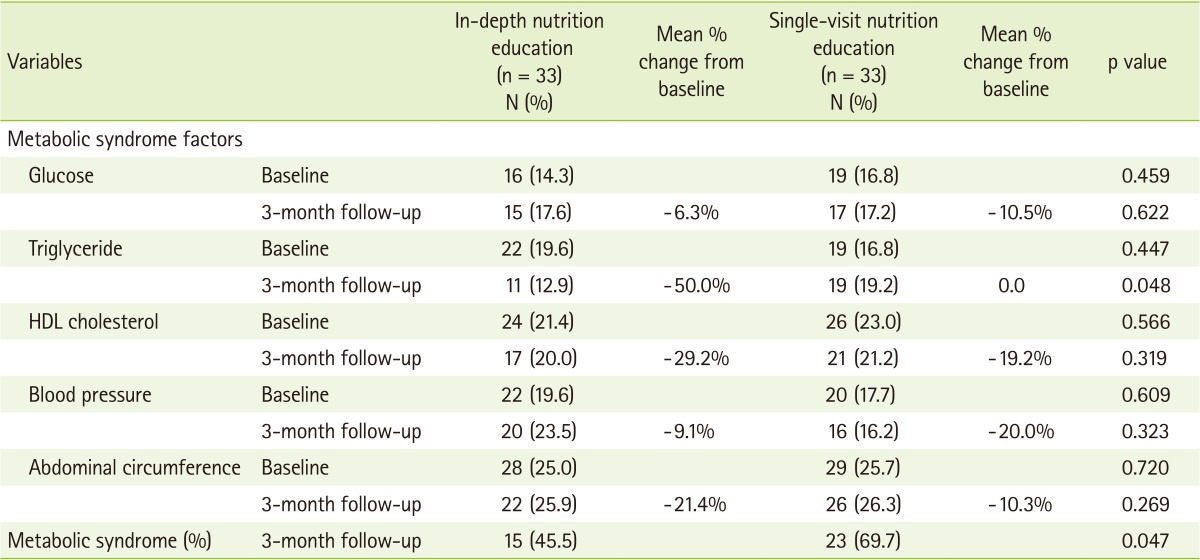
p value by χ2 test.
Discussion
As the chronic disease and the resulting death rate increase, it is important to discover the risk factors of metabolic syndrome and is necessary to develop optimal medical services for these patients. Accordingly, this study was designed to determine nutrient intake and the effects on risk factors of metabolic syndrome through telephone nutrition counseling according to the standard MNT guide for patients with metabolic syndrome who visited a health improvement center.
The effects of nutrition education on abdominal circumference were significant in both the a single-visit nutrition education group and the in-depth nutrition education group, which showed the usefulness of continuous management through telephone counseling in the prevention of cardiovascular disease and treatment of metabolic syndrome. Additionally, total cholesterol and triglyceride levels were significantly reduced after nutrition education; in particular, cholesterol concentrations decreased by more than 6.6% in both groups. This reduced rate of serum cholesterol levels is equivalent to previous research results showing that total cholesterol levels decreased 3 to 14% by NCEP dietary guideline continued for more than 3 months [20] and coincident with the previous study results showing that serum total cholesterol levels decreased by 8 to 15%; improvements in lipid levels were achieved by individual education [11].
When considering the total cholesterol versus HDL-cholesterol rate (that is, the arteriosclerosis indicator is more than 5), cardiovascular risk is reported to increase; this research showed that the changes of arteriosclerosis were greater in the in-depth nutrition education group than the single-visit nutrition education group, which suggested that the in-depth nutrition education was more effective in the prevention of cardiovascular disease. According to the research of Lim et al. [2], which was conducted based on a Korean National Health and Nutrition Examination Survey (KNHANES) in 1998 and 2001, the prevalence rate of metabolic syndrome increased rapidly from 23.6% in 1998 to 28.0% in 2001 and was related to the increased percentage change of patients with low HDL cholesterol levels (36.3%), high triglycerides (18.0%), and abdominal circumference (17.0%).
According to research results for the relation between hyperlipidemia and coronary artery disease, a 1% decrease in cholesterol level reduced the frequency of coronary artery disease by 2% [23,24] and a 10% decrease in cholesterol level from dietary therapy and medication therapy reduced the incidence of cardiac infarction by 20% [25,26]. Accordingly, the management of lipids and abdominal obesity through standardized MNT, as suggested by this study, should be widely implemented to reduce the incidence rate of cardiovascular diseases.
There was no significant change in blood glucose homeostatic indicators, such as fasting blood glucose levels, insulin, and HOMA-IR after MNT intervention in both groups. Because a diet with high carbohydrate content increases blood fasting glucose concentration and decreases HDL-cholesterol concentration in general, the intake of carbohydrates is encouraged to maintain 50-60% of total calories for patients with metabolic syndrome [23]. However, the intake of carbohydrates after nutrition education in both groups was more than 60% and there was no significant difference in the carbohydrates intake rate against total calorie intake. It might explicate no change in blood glucose homeostatic indicators, although the intake of carbohydrates was decreased after nutrition education. There were no significant differences between two groups in dietary intakes and especially in sodium intakes after 3 month MNT. It could be due to difficulty in adapting change in dietary habits and especially in reducing sodium intakes for short period of time. According to the study by Kim et al. [27], patients with metabolic syndrome had a higher carbohydrate intake ratio than normal, while the intakes of nutrients such as vitamins and minerals were poor. Therefore, patient centered personalized MNT should be implemented by a professional dietician under proper diet therapy protocol continuously.
There were significant differences between two groups on risk factors of metabolic syndrome such as triglyceride and prevalence of metabolic syndrome after 3 months nutrition education. It seems that when subjects are motivated through customized education rather than general education, the efficiency of the education is increased. Although a face-to-face interview has merits in that close relationships are formed by the conformity of subjects, it is difficult to accept many applicants at limited time due to restrictions of time and space.
In this study, continuous nutrition education consultation was conducted through telephone counseling. Previous studies indicated that online mediation programs through web-based customized intervention programs and the use of the internet and e-mail increased the efficiency of dietary intervention programs [28,29]. However, the telephone is an important mode of communication between patients and medical personnel, and telephone management has merits allowing an opportunity to provide advice and nutrition education, and acts as a bridge between the home and hospital thereby improves patient satisfaction with medical personnel by helping discover problems, provides follow-up education, and reinforces performance [30]. As shown in the results from this study, telephone counseling can effectively provide advice and education and seems to be useful for patients with metabolic syndrome who require continuous health behaviors improvements.
According to a precedent study, low-calorie and low-fat meals with more than 150 minutes of exercise a week decreased the body weight greater than 7% and the prevalence of metabolic syndrome by 58% [31]. This has important significance clinically because it shows that risk factors of disease can be reduced through changes in life styles. The in-depth clinical nutrition education method suggested by the present study shows that incidence rates of metabolic syndrome can be reduced by promoting life styles including dietary habits after nutrition education.
Because telephone counseling has been shown to increase intentions of performing nutrition management, individual education through long-term follow-up management should be implemented in the treatment of patients with metabolic syndrome. Although the prevalence of metabolic syndrome was investigated 3 months after nutrition education in this study, studies on the long-term effects of MNT should also be performed.
Acknowledgments
This research was supported by Basic Science Research Program through the National Research Foundation of Korea (NRF) funded by the Ministry of Education, Science and Technology, (project no. : NRF-2009-0068721).
References
- 1.Statistics Korea [Internet] The statistics of mortality and the causes. Daejeon: Statistics Korea; 2011. [cited 2013 May 10]. Available from: http://kostat.go.kr/ [Google Scholar]
- 2.Lim S, Park KS, Lee HK, Cho SI Korean National Health and Nutrition Examination Surveys. Changes in the characteristics of metabolic syndrome in Korea over the period 1998-2001 as determined by Korean National Health and Nutrition Examination Surveys. Diabetes Care. 2005;28:1810–1812. doi: 10.2337/diacare.28.7.1810. [DOI] [PubMed] [Google Scholar]
- 3.Malik S, Wong ND, Franklin SS, Kamath TV, L'Italien GJ, Pio JR, Williams GR. Impact of the metabolic syndrome on mortality from coronary heart disease, cardiovascular disease, and all causes in United States adults. Circulation. 2004;110:1245–1250. doi: 10.1161/01.CIR.0000140677.20606.0E. [DOI] [PubMed] [Google Scholar]
- 4.Lakka HM, Laaksonen DE, Lakka TA, Niskanen LK, Kumpusalo E, Tuomilehto J, Salonen JT. The metabolic syndrome and total and cardiovascular disease mortality in middle-aged men. JAMA. 2002;288:2709–2716. doi: 10.1001/jama.288.21.2709. [DOI] [PubMed] [Google Scholar]
- 5.Wilson C, Brown T, Acton K, Gilliland S. Effects of clinical nutrition education and educator discipline on glycemic control outcomes in the Indian health service. Diabetes Care. 2003;26:2500–2504. doi: 10.2337/diacare.26.9.2500. [DOI] [PubMed] [Google Scholar]
- 6.Franz MJ, Monk A, Barry B, McClain K, Weaver T, Cooper N, Upham P, Bergenstal R, Mazze RS. Effectiveness of medical nutrition therapy provided by dietitians in the management of non-insulin-dependent diabetes mellitus: a randomized, controlled clinical trial. J Am Diet Assoc. 1995;95:1009–1017. doi: 10.1016/S0002-8223(95)00276-6. [DOI] [PubMed] [Google Scholar]
- 7.Ash S, Reeves MM, Yeo S, Morrison G, Carey D, Capra S. Effect of intensive dietetic interventions on weight and glycaemic control in overweight men with Type II diabetes: a randomised trial. Int J Obes Relat Metab Disord. 2003;27:797–802. doi: 10.1038/sj.ijo.0802295. [DOI] [PubMed] [Google Scholar]
- 8.Pritchard DA, Hyndman J, Taba F. Nutritional counselling in general practice: a cost effective analysis. J Epidemiol Community Health. 1999;53:311–316. doi: 10.1136/jech.53.5.311. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Welty FK, Nasca MM, Lew NS, Gregoire S, Ruan Y. Effect of onsite dietitian counseling on weight loss and lipid levels in an outpatient physician office. Am J Cardiol. 2007;100:73–75. doi: 10.1016/j.amjcard.2007.02.056. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Koopman H, Spreeuwenberg C, Westerman RF, Donker AJ. Dietary treatment of patients with mild to moderate hypertension in a general practice: a pilot intervention study (2). Beyond three months. J Hum Hypertens. 1990;4:372–374. [PubMed] [Google Scholar]
- 11.Shon CM, Nho MR, Lee YH, Lim JH. The clinical and cost effectiveness of medical nutrition therapy in persons with hypercholesterolemia. J Korean Diet Assoc. 2003;9:32–39. [Google Scholar]
- 12.Delahanty LM, Sonnenberg LM, Hayden D, Nathan DM. Clinical and cost outcomes of medical nutrition therapy for hypercholesterolemia: a controlled trial. J Am Diet Assoc. 2001;101:1012–1023. doi: 10.1016/S0002-8223(01)00250-4. [DOI] [PubMed] [Google Scholar]
- 13.Henkin Y, Shai I, Zuk R, Brickner D, Zuilli I, Neumann L, Shany S. Dietary treatment of hypercholesterolemia: do dietitians do it better? A randomized, controlled trial. Am J Med. 2000;109:549–555. doi: 10.1016/s0002-9343(00)00566-0. [DOI] [PubMed] [Google Scholar]
- 14.Goode AD, Reeves MM, Eakin EG. Telephone-delivered interventions for physical activity and dietary behavior change: an updated systematic review. Am J Prev Med. 2012;42:81–88. doi: 10.1016/j.amepre.2011.08.025. [DOI] [PubMed] [Google Scholar]
- 15.Eakin EG, Lawler SP, Vandelanotte C, Owen N. Telephone interventions for physical activity and dietary behavior change: a systematic review. Am J Prev Med. 2007;32:419–434. doi: 10.1016/j.amepre.2007.01.004. [DOI] [PubMed] [Google Scholar]
- 16.Kim CG, Chung CH. Effects of telephone consulting program on self-efficacy and self-care in NIDDM patients. J Korean Acad Adult Nurs. 2002;14:306–314. [Google Scholar]
- 17.Davis RM, Hitch AD, Salaam MM, Herman WH, Zimmer-Galler IE, Mayer-Davis EJ. TeleHealth improves diabetes self-management in an underserved community: diabetes TeleCare. Diabetes Care. 2010;33:1712–1717. doi: 10.2337/dc09-1919. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Kris-Etherton PM, Taylor DS, Smiciklas-Wright H, Mitchell DC, Bekhuis TC, Olson BH, Slonim AB. High-soluble-fiber foods in conjunction with a telephone-based, personalized behavior change support service result in favorable changes in lipids and lifestyles after 7 weeks. J Am Diet Assoc. 2002;102:503–510. doi: 10.1016/s0002-8223(02)90116-1. [DOI] [PubMed] [Google Scholar]
- 19.Izquierdo RE, Knudson PE, Meyer S, Kearns J, Ploutz-Snyder R, Weinstock RS. A comparison of diabetes education administered through telemedicine versus in person. Diabetes Care. 2003;26:1002–1007. doi: 10.2337/diacare.26.4.1002. [DOI] [PubMed] [Google Scholar]
- 20.Alberti KG, Eckel RH, Grundy SM, Zimmet PZ, Cleeman JI, Donato KA, Fruchart JC, James WP, Loria CM, Smith SC, Jr International Diabetes Federation Task Force on Epidemiology and Prevention; Hational Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; International Association for the Study of Obesity. Harmonizing the metabolic syndrome: a joint interim statement of the International Diabetes Federation Task Force on Epidemiology and Prevention; National Heart, Lung, and Blood Institute; American Heart Association; World Heart Federation; International Atherosclerosis Society; and International Association for the Study of Obesity. Circulation. 2009;120:1640–1645. doi: 10.1161/CIRCULATIONAHA.109.192644. [DOI] [PubMed] [Google Scholar]
- 21.American Dietetic Association. Nutrition practice guidelines for type 1 and 2 diabetes mellitus [CD-ROM] Chicago (IL): American Dietetic Association; 2001. Medical nutrition therapy evidence-based guides for practice. [Google Scholar]
- 22.Franz MJ. The role of nutrition therapy and dietitians in the management of the metabolic syndrome. Curr Diab Rep. 2007;7:60–65. doi: 10.1007/s11892-007-0011-9. [DOI] [PubMed] [Google Scholar]
- 23.The Lipid Research Clinics Coronary Primary Prevention Trial results. I. Reduction in incidence of coronary heart disease. JAMA. 1984;251:351–364. doi: 10.1001/jama.1984.03340270029025. [DOI] [PubMed] [Google Scholar]
- 24.The Lipid Research Clinics Coronary Primary Prevention Trial results. II. The relationship of reduction in incidence of coronary heart disease to cholesterol lowering. JAMA. 1984;251:365–374. [PubMed] [Google Scholar]
- 25.Rossouw JE, Lewis B, Rifkind BM. The value of lowering cholesterol after myocardial infarction. N Engl J Med. 1990;323:1112–1119. doi: 10.1056/NEJM199010183231606. [DOI] [PubMed] [Google Scholar]
- 26.Law MR, Wald NJ, Thompson SG. By how much and how quickly does reduction in serum cholesterol concentration lower risk of ischaemic heart disease? BMJ. 1994;308:367–372. doi: 10.1136/bmj.308.6925.367. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Kim M, Kim J, Bae W, Kim S, Lee Y, Na W, Sohn C. Relationship between nutrients intakes, dietary quality, and serum concentrations of inflammatory markers in metabolic syndrome patients. Korean J Community Nutr. 2011;16:51–61. [Google Scholar]
- 28.Park SY, Yang YJ, Kim Y. Effects of nutrition education using a ubiquitous healthcare (u-Health) service on metabolic syndrome in male workers. Korean J Nutr. 2011;44:231–242. [Google Scholar]
- 29.Kang JY, Cho SW, Lee JY, Sung SH, Park YK, Paek YM, Choi TI. The effects of a worksite on-line health education program on metabolic syndrome risk factors and nutrient intakes of male workers. Korean J Nutr. 2010;43:57–68. [Google Scholar]
- 30.Song MS, Kim HS. Effect of the diabetes outpatient intensive management programme on glycaemic control for type 2 diabetic patients. J Clin Nurs. 2007;16:1367–1373. doi: 10.1111/j.1365-2702.2007.01800.x. [DOI] [PubMed] [Google Scholar]
- 31.Knowler WC, Barrett-Connor E, Fowler SE, Hamman RF, Lachin JM, Walker EA, Nathan DM Diabetes Prevention Program Research Group. Reduction in the incidence of type 2 diabetes with lifestyle intervention or metformin. N Engl J Med. 2002;346:393–403. doi: 10.1056/NEJMoa012512. [DOI] [PMC free article] [PubMed] [Google Scholar]