Abstract
Objective: Newer non-benzodiazepines zolpidem and zopiclone (“Z-drugs”) are often prescribed instead of benzodiazepine hypnotics, although there is no evidence of differences in effectiveness and safety. Aim was to compare perceptions on benefits and harms of benzodiazepines and Z-drugs between general practitioners (GPs) and community pharmacists (CPs).
Methods: A questionnaire was mailed to a random sample of 1,350 GPs and 600 CPs in 2012. They were asked to rate perceptions on a five-point Likert scale used for both benzodiazepines and Z-drugs. Wilcoxon signed rank test was performed for the comparison of perceptions between GPs and CPs. Due to multiple testing, only p-values ≤0.01 were considered statistically significant.
Results: 458 GPs and 202 CPs returned questionnaires (response 33.9% and 33.7%). Mean age of GPs was 53.3 years (40.6% female) and 48.8 years for CPs (59.2% females). Perceptions on benefits of benzodiazepines (and Z-drugs) between GPs and CPs were not different for 3 (and 2) of 5 items. Concerning side effects of benzodiazepines, there were no statistically significant differences for 3 of 5 comparisons. CPs perceived that 4 of 5 studied side effects of Z-drugs occur significantly more often than GPs (p=0.003 or less). For instance, whereas 45.2% of CPs answered that withdrawal effects on stopping happen often or very often/always on Z-drugs, these were only 28.3% of the GPs.
Conclusions: Although it is difficult to draw unambiguous conclusions from these findings, pharmacists might have a somewhat more critical view on Z-drugs, especially concerning side effects.
Keywords: cross-sectional studies, Germany, hypnotics and sedatives, attitude of health personnel
Abstract
Hintergrund und Fragestellung: Die neueren Benzodiazepinrezeptor-Agonisten Zolpidem und Zopiclon (“Z-Drugs”) werden in letzter Zeit häufiger als Hypnotika vom Benzodiazepintyp verschrieben, obwohl keine Belege für Unterschiede bezüglich des Nutzens und Schaden existieren. Ziel dieser Studie war es zu vergleichen, wie Hausärzte und Apotheker erwünschte und unerwünschte Wirkungen dieser Mittel einschätzen.
Methoden: Ein schriftlicher Fragebogen wurde 2012 an eine Zufallsauswahl von 1.350 Hausärzten und 600 Apothekenleitern versendet. Die gleichen Items wurden auf einer 5-Punkte-Likert-Skala sowohl für Benzodiazepine wie Z-Drugs abgefragt. Zum Vergleich zwischen Hausärzten und Apothekern wurden Wilcoxon Signed Rank Tests durchgeführt. Aufgrund der zahlreichen Tests wurden nur p-Werte ≤0,01 als statistisch signifikant angesehen.
Ergebnisse: Insgesamt antworteten 458 Hausärzte und 202 Apotheker (Rücklauf 33,9% und 33,7%). Hausärzte waren durchschnittlich 53,3 Jahre (40,6% weiblich) und Apotheker 48,8 Jahre alt (59,2% weiblich). Keine Unterschiede in der Einschätzung des Nutzens von Benzodiazepinen (bzw. Z-Drugs) fanden sich bei 3 (bzw. 2) von 5 Items. Keine Unterschiede zeigten sich auch bei 3 von 5 Items zu unerwünschten Wirkungen von Benzodiazepinen. Hingegen schätzten Apotheker, dass 4 der 5 untersuchten unerwünschten Wirkungen von Z-Drugs häufiger vorkamen als Hausärzte (p=0,003 oder kleiner). Beispielsweise antworteten 45,2% der Apotheker, dass Entzugserscheinungen häufig bzw. sehr häufig/immer unter Z-Drugs auftreten, hingegen nur 28,3% der Hausärzte.
Schlussfolgerungen: Obwohl es insgesamt schwierig ist, eindeutige Schlussfolgerungen aus diesen Befunden zu ziehen, scheinen Apotheker einen kritischeren Blick auf Z-Drugs und deren unerwünschte Wirkungen zu haben.
Introduction
Hypnotics such as short-acting benzodiazepines and the newer non-benzodiazepines zolpidem and zopiclone (“Z-drugs”) are the most common pharmacological treatment for insomnia [1], [2]. Although there is no evidence of differences in clinical effectiveness and safety between these substance groups [3], [4], Z-drugs are increasingly prescribed since their introduction in the early 1990s while the use of benzodiazepine hypnotics decreased [2], [5], [6]. A reason for this trend seems to be that general practitioners (GPs) attribute Z-drugs with greater benefits and fewer side effects compared to benzodiazepines [1], [7]. GPs further perceived that Z-drugs were safer for elder patients, which also contradicts the current evidence. Benefits of hypnotics for older persons are modest at best and are outweighed by the increased risks [8].
Community pharmacists (CPs) have an important role in providing information on medicines. Their own profession as well as a large majority of physicians want pharmacists’ involvement in counselling patients about adverse effects [9], a result that has also been found for hypnotics [10]. Pharmacists are experts on drugs and might have a better knowledge on adverse effects. This hypothesis is supported by a comparison of therapeutic knowledge of GPs and CPs on simple analgesics [11] but not for opioids in another study [12]. However, no further evidence is available on this topic.
The aim of this study was to compare perceptions on benefits and harms of benzodiazepines and Z-drugs between German GPs and CPs.
Patients, materials and methods
Design, participants and measures
In Germany, about 55,000 GPs are working in the outpatient sector and there are about 22,000 community pharmacies. Two questionnaire surveys were mailed to 1,350 and 600 randomly selected GPs and owners of community pharmacies, respectively. The surveys were conducted between May and November 2012 and the designs were quite comparable. Several strategies shown by a Cochrane review to increase response to postal questionnaires were applied [13]. Those include pre-notification, a short questionnaire, follow-up contact, providing a second copy of the questionnaire at follow-up, personalised postcards and letters, hand-written signatures, and academic origin of the study. A postcard announcement was sent one week before the two-sided questionnaire including a pre-addressed return envelope was mailed out. Three weeks later, a reminder including another copy of the questionnaire and a pre-addressed return envelope were sent to all non-responders. No further actions were taken and no financial incentives were provided.
Both questionnaires included two sections concerning the perceptions of benefits and harms of benzodiazepines and Z-drugs for the treatment of insomnia. In order to do so, the same questions consisting of 12 items were asked on both benzodiazepines and Z-drugs. Each of these items was rated on a five-point Likert scale. For instance, answers on participants’ estimates on the frequencies of side effect of these hypnotics ranged from “never/very rarely” to “very often/always”. These items were adopted from a British study on the same topic [7].
Results of the GP survey with a focus on the comparison of benzodiazepines and Z-drugs have already been published elsewhere [1]. The questionnaire is available online (http://www.smw.ch/fileadmin/smw/pdf/SMW-13745-Appendix.pdf).
Statistical analysis
Baseline characteristics are presented as percentages or means with standard deviation. The non parametric Wilcoxon signed rank test was used for the comparison of perceptions between GPs and CPs. Responses on the five-point Likert scales are presented within three categories. Due to multiple testing, only p-values ≤0.01 were considered statistically significant.
All analyses were performed with SAS for Windows version 9.2 (SAS Institute Inc., Cary, NC).
Results
Baseline characteristics
Out of 1,350 questionnaires sent out to GPs, 458 were returned (response 33.9%). Mean age of the respondents was 53.3 years (SD: 8.7) and 40.6% of them were female. On average, they were 16.3 years in practice and nearly half of them work in single-handed practices (51.9%).
Of the 600 pharmacist surveys, 202 were received (response 33.7%). The mean age of CPs was 48.8 years (SD: 11.0). With 59.2% the proportion of females was higher compared to the physicians. On average, 2.5 pharmacists work in the pharmacies of the respondents.
Comparison of perceptions on benzodiazepines and Z-drugs
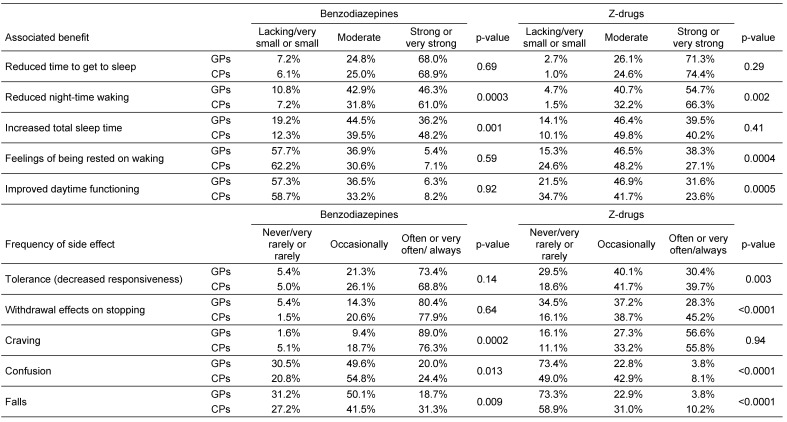
Attitudes of GPs and CPs on benefits and side effects of benzodiazepines and Z-drugs are summarized in Table 1 (Tab. 1). Perceptions on benefits of benzodiazepines between GPs and CPs were not different for 3 of the 5 items. CPs rated these drugs to be more effective in terms of reduced night-time waking and increased total sleep time. On the other hand, no statistically significant differences between GPs and CPs were found for 2 out of 5 items on benefits of Z-drugs. GPs perceived that Z-drugs were significantly more effective in terms of feelings of being rested on waking and improved daytime functioning, but CPs believed that the effect on reduced night-time waking is stronger (p=0.002 or less for all comparisons).
Table 1. Perceptions of GPs* and CPs on benefits and side effects of benzodiazepines and Z-drugs.
* Small differences in percentages compared to the publication on perceptions of GPs on benzodiazepines and Z-drugs [1] are due to a higher amount of missing values for paired comparisons.
Concerning side effects of benzodiazepines, there were no statistically significant differences between GPs and CPs for 3 of the 5 items. GPs rated craving more often and CPs believed that falls are more often under benzodiazepines. Interestingly, for 4 of the 5 studied side effects of Z-drugs CPs perceived that they occur statistically significant more often then GPs (p=0.003 or less for all comparisons). For instance, whereas 45.2% of the participating CPs answered that withdrawal effects on stopping happen often or very often/always on Z-drugs, these were only 28.3% of the GPs. No statistically significant difference between both groups was found for craving.
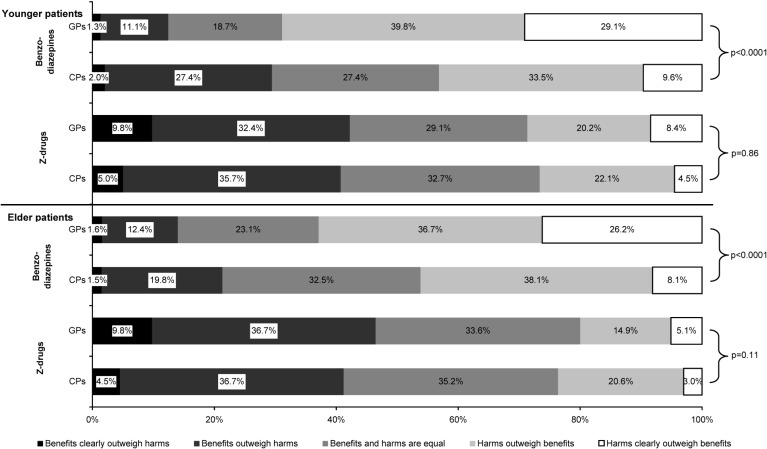
When comparing the overall ratio of benefits and harms of both drugs in younger and elder patients, GPs more often perceived that harms outweigh benefits in younger and older patients using benzodiazepines (Figure 1 (Fig. 1)). On the other hand, no difference between GPs and CPs was found for the ratio of benefits and harms of Z-drugs for younger as well as elder patients.
Figure 1. Perceptions of GPs* and CPs on overall benefits and harms of benzodiazepines and Z-drugs in younger and elder patients.
* Small differences in percentages compared to the publication on perceptions of GPs on benzodiazepines and Z-drugs [1] are due to a higher amount of missing values for paired comparisons.
Discussion
Although there is no compelling evidence for clinically relevant differences in effectiveness and safety between both substance groups [3], [4], the newer Z-drugs are often prescribed instead of short-acting benzodiazepine hypnotics. A reason for this seems to be that GPs attribute Z-drugs with greater benefits and fewer side effects compared to benzodiazepines [1], [7]. The starting point of this analysis was the hypothesis that pharmacists might have a better knowledge on adverse effects of drugs. This was supported by an earlier study in which pharmacists displayed a better therapeutic knowledge of simple analgesics than GPs [11] but refused in another survey for opioids [12]. Although findings for benzodiazepines were ambiguous, for 4 of the 5 studied side effects of Z-drugs CPs perceived that they occur more often then GPs. However, when comparing attitudes of pharmacists between both substance groups, Z-drugs were rated to be safer than benzodiazepines for all 5 items (p<0.0001 for all comparisons). The same result was found for GPs [1].
Interestingly, about 70% of both GPs and CPs believed that benzodiazepines as well as Z-drugs have a strong or very strong effect in terms of reduced time to get to sleep. This is contrary to current evidence derived from meta-analyses of randomized trials. The improvements in sleep latency were found to be small when compared with placebo and the non-specific placebo response is a major contributor to the effectiveness of hypnotics [14], [15]. Another interesting finding is that the overall ratio of benefits and harms of Z-drugs in elder patients was comparable to their younger counterparts or even rated more positive. This was found for both healthcare professionals and is not supported by current evidence. For persons aged 60 years or older, the benefits of hypnotics may not justify the increased risk [8]. This is important because prescribing of hypnotics increases with age [5], [6]. An overestimation of true effectiveness and the perception of fewer side effects of Z-drugs might lead to more frequent use.
Though a large sample of German GPs and CPs could be studied, some limitations have to be considered. The response of about one third for both surveys seems to be low and this might lead to selection bias. However, this response is quite comparable with other recently published surveys of German GPs [1]. Another source of bias might be social desirability when studying healthcare professionals’ perceptions on psychotropic substances that have the potential to cause dependence and tolerance. It might also be that responses are related to evidence-based knowledge in some participants and to experience-based knowledge in others, which might lead to different perceptions. A further criticism refers to the fact that questions on perceptions on benefits and side effects were not divided into short-term and long-term use. However, this was also not done in the survey of British GPs conducted by Siriwardena et al. [7], from which items were adopted.
Conclusions
It is difficult to draw unambiguous conclusions from the findings of this study. Pharmacists seem to have a somewhat more critical view on Z-drugs, especially concerning side effects. However, they also perceive more often than GPs that benefits outweigh harms in younger and older patients using benzodiazepines. Overall, both GPs as well as CPs perceived that Z-drugs were more effective and safer compared to benzodiazepines, which is not supported by current evidence. Such beliefs of healthcare professionals seem to be a barrier for the implementation of guidelines.
Notes
Acknowledgements
I thank all participating GPs and CPs for their support, and Dr. Roland Windt, Melanie Tamminga, Tim Jacobs, Julia Marwede and Barbara Hetmanek for their help in conducting the studies. We are grateful to Prof. Niroshan Siriwardena who provided a copy of his questionnaire developed for his survey.
Ethical approval
The ethics committee of the University of Bremen advised that an ethical approval was not required (email dated 4 May 2011).
Funding
This work is funded by a grant of the Deutsche Forschungsgemeinschaft (DFG; project funding reference number HO 4782/1-1) and by an additional bonus of the University of Bremen.
Competing interests
The author declares to have no competing interests.
References
- 1.Hoffmann F. Perceptions of German GPs on benefits and risks of benzodiazepines and Z-drugs. Swiss Med Wkly. 2013;143:w13745. doi: 10.4414/smw.2013.13745. Available from: http://dx.doi.org/10.4414/smw.2013.13745. [DOI] [PubMed] [Google Scholar]
- 2.Sivertsen B, Nordhus IH, Bjorvatn B, Pallesen S. Sleep problems in general practice: a national survey of assessment and treatment routines of general practitioners in Norway. J Sleep Res. 2010 Mar;19(1 Pt 1):36–41. doi: 10.1111/j.1365-2869.2009.00769.x. Available from: http://dx.doi.org/10.1111/j.1365-2869.2009.00769.x. [DOI] [PubMed] [Google Scholar]
- 3.Dündar Y, Boland A, Strobl J, Dodd S, Haycox A, Bagust A, Bogg J, Dickson R, Walley T. Newer hypnotic drugs for the short-term management of insomnia: a systematic review and economic evaluation. Health Technol Assess. 2004 Jun;8(24):iii–x, 1. doi: 10.3310/hta8240. [DOI] [PubMed] [Google Scholar]
- 4.NICE – National Institute for Clinical Excellence. Guidance on the use of zaleplon, zolpidem and zopiclone for the short-term management of insomnia. London: National Institute for Clinical Excellence; 2004. (Technology Appraisal Guidance; 77). Available from: http://www.nice.org.uk/nicemedia/pdf/TA077fullguidance.pdf. [Google Scholar]
- 5.Andersen AB, Frydenberg M. Long-term use of zopiclone, zolpidem and zaleplon among Danish elderly and the association with sociodemographic factors and use of other drugs. Pharmacoepidemiol Drug Saf. 2011 Apr;20(4):378–385. doi: 10.1002/pds.2104. Available from: http://dx.doi.org/10.1002/pds.2104. [DOI] [PubMed] [Google Scholar]
- 6.Hausken AM, Furu K, Skurtveit S, Engeland A, Bramness JG. Starting insomnia treatment: the use of benzodiazepines versus z-hypnotics. A prescription database study of predictors. Eur J Clin Pharmacol. 2009 Mar;65(3):295–301. doi: 10.1007/s00228-008-0565-8. Available from: http://dx.doi.org/10.1007/s00228-008-0565-8. [DOI] [PubMed] [Google Scholar]
- 7.Siriwardena AN, Qureshi Z, Gibson S, Collier S, Latham M. GPs' attitudes to benzodiazepine and 'Z-drug' prescribing: a barrier to implementation of evidence and guidance on hypnotics. Br J Gen Pract. 2006 Dec;56(533):964–967. [PMC free article] [PubMed] [Google Scholar]
- 8.Glass J, Lanctôt KL, Herrmann N, Sproule BA, Busto UE. Sedative hypnotics in older people with insomnia: meta-analysis of risks and benefits. BMJ. 2005 Nov;331(7526):1169. doi: 10.1136/bmj.38623.768588.47. Available from: http://dx.doi.org/10.1136/bmj.38623.768588.47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Bryant LJ, Coster G, Gamble GD, McCormick RN. General practitioners' and pharmacists' perceptions of the role of community pharmacists in delivering clinical services. Res Social Adm Pharm. 2009 Dec;5(4):347–362. doi: 10.1016/j.sapharm.2009.01.002. Available from: http://dx.doi.org/10.1016/j.sapharm.2009.01.002. [DOI] [PubMed] [Google Scholar]
- 10.Tanskanen P, Airaksinen M, Tanskanen A, Enlund H. Counselling patients on psychotropic medication: physicians' opinions on the role of community pharmacists. Pharm World Sci. 2000 Apr;22(2):59–61. doi: 10.1023/A:1008714922814. Available from: http://dx.doi.org/10.1023/A:1008714922814. [DOI] [PubMed] [Google Scholar]
- 11.Briggs A, Scott E, Steele K. Analgesics: a comparison of therapeutic knowledge and inter-professional liaison between general practitioners and community pharmacists. Br J Gen Pract. 1997 Jun;47(419):378–379. [PMC free article] [PubMed] [Google Scholar]
- 12.Furstenberg CT, Ahles TA, Whedon MB, Pierce KL, Dolan M, Roberts L, Silberfarb PM. Knowledge and attitudes of health-care providers toward cancer pain management: a comparison of physicians, nurses, and pharmacists in the state of New Hampshire. J Pain Symptom Manage. 1998 Jun;15(6):335–349. doi: 10.1016/S0885-3924(98)00023-2. Available from: http://dx.doi.org/10.1016/S0885-3924(98)00023-2. [DOI] [PubMed] [Google Scholar]
- 13.Edwards PJ, Roberts I, Clarke MJ, Diguiseppi C, Wentz R, Kwan I, Cooper R, Felix LM, Pratap S. Methods to increase response to postal and electronic questionnaires. Cochrane Database Syst Rev. 2009;(3):MR000008. doi: 10.1002/14651858.MR000008.pub4. Available from: http://dx.doi.org/10.1002/14651858.MR000008.pub4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Holbrook AM, Crowther R, Lotter A, Cheng C, King D. Meta-analysis of benzodiazepine use in the treatment of insomnia. CMAJ. 2000 Jan;162(2):225–233. [PMC free article] [PubMed] [Google Scholar]
- 15.Huedo-Medina TB, Kirsch I, Middlemass J, Klonizakis M, Siriwardena AN. Effectiveness of non-benzodiazepine hypnotics in treatment of adult insomnia: meta-analysis of data submitted to the Food and Drug Administration. BMJ. 2012;345:e8343. doi: 10.1136/bmj.e8343. Available from: http://dx.doi.org/10.1136/bmj.e8343. [DOI] [PMC free article] [PubMed] [Google Scholar]