Abstract
Background: Surgical procedures advocated for management of residual hepatic hydatid cyst cavity have been a subject of controversy. The aim of this study was to compare omentoplasty (OP) and external tube drainage (ETD).
Material and methods: This was a prospective randomized controlled study conducted on radiologically documented cases of hepatic hydatidosis (n=50) in a tertiary care hospital of Kashmir. Patients were divided into two groups; in one group ETD was performed and in another OP was done.
Results: Twenty-eight patients were offered ETD and 22 OP. There was no statistically significant difference in mean operative time. The overall complication rate was higher in ETD (42.86%) as compared to OP (22.73%). In ETD group two patients had bile leak and infection of residual cavity each; whereas no such complication was seen in OP. The mean pain scores were elevated in ETD (p<0.0016).The mean hospital stay was more in ETD as compared to OP (p<0.0031). Also time for resumption of activities of daily life was more in ETD (p<0.0026). The recurrence of disease was seen in three patients in ETD as compared to none in OP.
Conclusion: Omentoplasty offers a number of advantages over external tube drainage and should remain the preferred option whenever possible.
Keywords: hydatid cyst, omentoplasty, external tube drainage, laparoscopy, liver
Abstract
Einleitung: Die chirurgischen Verfahren zur Behandlung von vorhandenen Echinococcus-Zysten in der Leber werden kontrovers beurteilt. Das Ziel dieser Studie war es, die Omentumplastik (OP) mit dem externen Schlauch-Drainageverfahren (ETD) zu vergleichen.
Material und Methoden: Eine prospektive randomisierte, kontrollierte Studie an radiologisch nachgewiesenen Fällen von Leberechinococcose (n=50) wurde in einem Krankenhaus der Maximalversorgung von Kashmir durchgeführt. Die Patienten wurden in zwei Gruppen eingeteilt: Bei der einen Gruppe wurde die externe Schlauchdrainage (ETD) durchgeführt, die andere Gruppe wurde operativ mit Omentumplastik (OP) behandelt.
Ergebnisse: 28 Patienten erhielten das ETD-Verfahren und 22 wurden operativ mit Omentumplastik (OP) behandelt. Die gesamte Komplikationsrate war bei ETD höher (42,86 %), verglichen mit dem OP-Verfahren (22,73 %). In den ETD-Gruppen entstanden bei zwei Patienten Gallenfisteln und Infektionen der Zysten, während in der Kontrollgruppe keine Komplikationen beobachtet wurden. Bei der ETD-Gruppe waren die durchschnittlichen Schmerzskalen (pain scores) erhöht (p<0,0016). Der mittlere Krankenhausaufenthalt war bei ETD länger als bei dem OP-Verfahren (p<0,0031). Die Zeit bis zur Wiederaufnahme des täglichen Lebens war bei ETD länger (p<0,0026). Rückfälle wurden bei drei ETD-Patienten gesehen, keine Rückfälle bei OP.
Folgerung: Omentumplastik bietet eine Reihe von Vorteilen gegenüber dem ETD-Verfahren und sollte – wenn möglich – die bevorzugte Therapie sein.
Introduction
Hydatid disease of the liver has been known since ancient times. The disease has a worldwide distribution and is most commonly seen in sheep rearing areas of the world. Hydatid disease is a zoonotic infection caused by adult or larval stages of the tapeworm of genus Echinococcus [1]. Carnivores like dogs act as definitive hosts and harbor the adult worm whereas sheep and other herbivores are intermediate hosts. Humans are the accidental intermediate hosts. Once within the man or other intermediate host the ingested eggs hatch in the duodenum to release the true larvae (oncospheres) that penetrate the mucosa of small intestine and enter the portal circulation. Liver acts as the first effective filter for most of the larvae and therefore is the most common site of involvement (65–75%) [2].
The main management of hydatid liver is surgical which basically entails removal of the cyst leaving behind a residual cavity. The various options available for managing the residual cyst cavity are: leaving the cavity open, simple closure, marsupialization, external tube drainage, introflexion, capitonnage, omentoplasty, partial capitonnage with omentoplasty, Roux-en-Y cystojejunostomy and radiofrequency ablation; with omentoplasty (OP) and external tube drainage (ETD) being most popular and promising [3], [4], [5], [6], [7], [8], [9]. The aim of this study was to compare OP and ETD.
Material and methods
This study was conducted in an academic tertiary care hospital of Kashmir over a period of four years from July 2008 to June 2012 and included 50 patients of Ultrasonography (USG) and Contrast Enhanced Computed Tomography (CECT) documented hydatid cysts of the liver. Serology for hydatid was done as a part of the protocol. Patients with Gharbi Type V hydatid cysts (dead cysts that appear calcified on ultrasonography) and infected hydatid cysts were excluded from the study. Any contraindication to general anesthesia was also considered as an exclusion criterion. Albendazole 15 mg/kg/day was started a fortnight before surgery and was continued for another fortnight after it.
Ours was a prospective study. Patients underwent a standard hydatid cystectomy either by laparoscopic or by open approach. The patients/attendants were explained the procedure in detail and an informed consent was taken for the same. In patients who were operated by open method, a right subcostal incision was made. Laparoscopically, trocars were placed according to the location of the cyst. The operative field was carefully protected from any spillage by using gauze packs soaked in 10% povidine iodine as a scolicidal agent. The cysts were aspirated and an equal amount of 10% povidine iodine was injected into the cyst and was left there for 10 minutes. The cyst contents were evacuated and the cavity was cleaned with gauze soaked in 10% povidine iodine. The laminated and the germinal membrane of the cyst were removed and a formal hydatid cystectomy was accomplished. Pericystectomy was not offered to any of our patients as a matter of protocol. The cyst cavity was then examined for any communication with biliary system and if present, it was primarily closed with 4-0 Polyglactin 910 (Centisorb, Centinnial™ Surgical Sutures Ltd., Thane, IN).
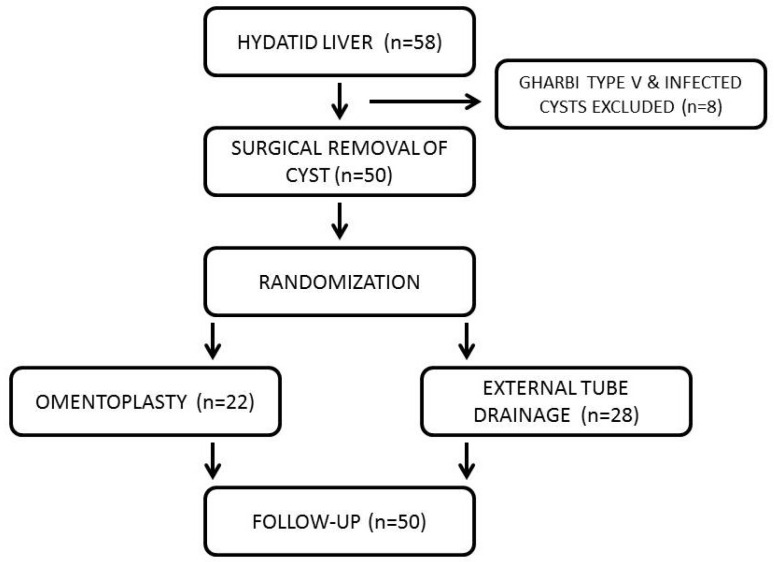
For the management of residual cavity patients were randomly allocated into two groups. This randomization was done by a computer-generated chart (Figure 1 (Fig. 1)). ETD was done in Group I (28 patients) by using a 22 F Foley’s two-way catheter [Polymedicure Ltd., Faridabad, IN] placed in the cyst cavity and exteriorized through a separate skin wound or any of the laparoscopic port sites. OP was done in Group II (22 patients) by placing a viable pedicle of omentum in the cyst cavity and fixing it to the cyst wall with 2-0 Polyglactin 910 [Centisorb, Centinnial™ Surgical Sutures Ltd., Thane, IN]. A 24 F tube drain [Diagnostix India, Bhiwani, IN] was placed in the Morrison’s pouch in all the patients.
Figure 1. Flow chart showing the design of the study.
Various intraoperative and postoperative parameters like operative time, postoperative pain, postoperative stay and time to return to activities of daily life were evaluated. The operative time was defined as the time taken from incising the skin or inserting the trocar till the skin/port closure. Intraoperative complications were noted and dealt with accordingly. Postoperative complications, morbidity and hospital stay were observed. Drainage of bile was noted and a cavitogram was obtained before removing the intracavitary drain. Drains were removed only when the 24 hour output was less than 10 mL. Postoperative pain was measured by visual analog scale. The pain scores were obtained at 2, 6, 8, 12 and 24 hours and then once daily till the time of discharge. Analgesics were administered if the visual analog pain score was greater than 6. Wound was inspected for any soakage or signs of infection. Any patient with features of sepsis was evaluated by complete septic profile and an abdominal sonogram with a 3.5 MHz convex sector transducer probe, performed in the standard manner, to rule out any intraabdominal collection. All the patients were followed in the outpatients department and the time taken for return to routine work was noted. To detect recurrence, the patients were followed up with USG every 3 monthly for a year and then 6 monthly for another year and a CECT was done if needed.
Statistical analysis was done by Graphpad Instat Version 3.10 for Windows [Graphpad softwares Inc., San Diego, California, USA]. To calculate the p-value, “Fisher’s exact test” or “unpaired t-test” was used, as and when needed. An ethical clearance was obtained from the local ethics committee.
Results
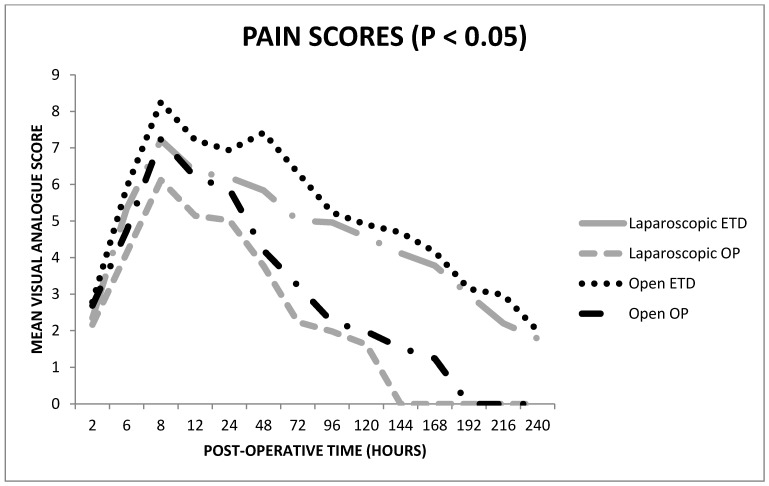
Both the groups were comparable in their baseline clinicopathologic characteristics and every attempt was made to minimize the confounding factors (Table 1 (Tab. 1)). Forty-four patients were operated by open technique (right subcostal incision) and six were operated laparoscopically. Among the former ETD was done in 24 and OP in 20 patients. The mean operative time in the laparoscopic ETD group was 95.75 ± 4.35 min and that in laparoscopic OP group was 98.50 ± 0.7071 min (p=0.9110). The mean time taken to complete open ETD and open OP was 62.21 ± 8.62 min and 66.80 ± 7.564 min (p=0.8793) respectively. The only intraoperative complication seen in either ETD or OP was anaphylaxis and occurred in one each (p=0.9890).
Table 1. Clinico-pathological parameters of the two groups were comparable in all respects.
In the postoperative period, the patients managed by OP fared better as compared to the ETD group. Two patients (7.14%) had bile leak in the ETD group whereas no bile leak was seen in the OP group (p=0.4971). Infection of the residual cavity was seen in two (7.14%) patients in ETD group while in OP group none of the patients had such complications (p=0.4971). Basal atelectasis of the right side was noted in three patients (10.71%) of ETD and in one patient (4.54%) of OP (p=0.6209). Wound infection was seen in four patients (two each in ETD and OP (p=1.0000)). Though the overall number of complications in ETD (12 (42.86%)) was more as compared to OP (5 (22.73%)), it did not reach statistical significance (p=0.2287).
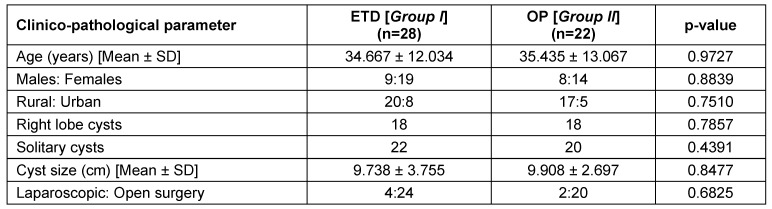
Pain scores were significantly less in OP as compared to ETD. The mean visual analog score for pain on the first postoperative day was 5.14 ± 0.132 in the OP group and 6.01 ± 0.118 in the ETD group (p<0.0001). On the second postoperative day, the mean pain scores observed were 3.84 ± 0.307 in OP and 6.14 ± 0.15 in the ETD group (p=0.0009). On the third postoperative day, the mean pain scores were 2.84 ± 0.307 in OP and 5.84 ± 0.7656 in the ETD group (p<0.0001). Pain scores reported on the subsequent days revealed a similar trend favoring OP (Figure 2 (Fig. 2)). The pain scores in patients operated laparoscopically were significantly lower than their open counterparts (p<0.0001).
Figure 2. The pain scores peaked at 8 hours in the postoperative period but were significantly lower in the OP group.
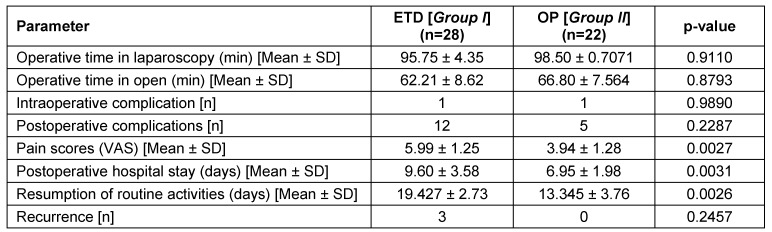
The drains were removed at a mean duration of 5.05 ± 1.28 days in OP group and 8.15 ± 1.56 days in ETD group (p<0.0031). The mean postoperative hospital stay was significantly shorter (p<0.0031) in patients who underwent OP (6.95 ± 1.98 days) as compared to ETD (9.60 ± 3.58 days). Patients with OP returned earlier to activities of daily life as compared to ETD (13.345 ± 3.76 days versus 19.427 ± 2.73 days, (p<0.0026)). No mortality was noted in our series. Routine follow-up scans picked up a recurrence in three of our patients receiving ETD; however no recurrence was seen in the OP group (p<0.2457). A summary of all the observations is depicted in Table 2 (Tab. 2).
Table 2. Summary of observations in the two groups.
Discussion
In recent years, hydatidosis has been recognized as a public health problem of nearly global dimensions and has been attributed to occupational or domestic exposure (rearing of sheep/pets, consumption of contaminated vegetables) [2]. Foci have also been identified from India where the highest prevalence has been reported from Andhra Pradesh and Tamil Nadu [10]. A study in Delhi showed that approximately 10% of sheep slaughtered in Delhi slaughter houses were infected with the larval forms of the parasite [11]. Because the practice of close contact with domestic animals such as dogs is rare in Kashmir, which is Muslim dominated; the sheep-dog association is implicated in the life cycle of the parasite [2].
The treatment of hydatid disease has been the responsibility of surgeons for many years. The rationale for elective surgical treatment of a hydatid lesion of liver is based on the plea that it may grow and cause troublesome symptoms and life threatening complications. After the removal of hydatid cyst of the liver, the management of the residual cavity has remained a matter of contention with most of the authorities narrowing on to ETD and OP as the procedures of choice. Proponents of ETD claim that it is technically easier to perform, takes lesser time and identifies biliary leaks. Proponents of OP claim its superiority owing to the facts that it results in decreased postoperative stay, complications and is associated with a lesser rate of recurrence and residual infection [12], [13], [14], [15], [16].
As expected, the difference between the operative time of laparoscopic and open surgery was statistically significant (p<0.0001). This is ascribed to the learning curve of laparoscopy. Though there was a marginal difference in the operative times of ETD and OP, it did not reach statistical significance. We might expect that ETD will take lesser time to complete as it does not require applying any sutures between the tube and the cyst wall, unlike OP. However this advantage is offset by the time taken to exteriorize the tube. Our data was similar to that reported by Malik et al. [8] who noted a mean operative time of 105 min in ETD and 95 min for OP, thereby having no significant difference in operative time between the two procedures. However none of their patients were operated laparoscopically.
A well vascularized flap of omentum not only obliterates the cavity and absorbs any secretions present there but also contributes to innate immunity [17]. This was reflected in the absence of bile leak or infection of residual cavity in the OP group. It is not surprising to expect that the intracavitary drain may act as a portal for infection. Two patients with ETD developed fever with localizing signs to right upper abdomen on the fourth postoperative day. An USG of the abdomen revealed collection in the residual cavity which on aspiration was purulent and grew Staphylococcus epidermidis. Though the intracavitary drains were draining purulent material, percutaneous aspiration of the collection under the cover of intravenous antibiotics resulted in good response. Bile leaks resolved conservatively and none of our patients required endoscopic sphincterotomy or stenting. An additional tube drain in the abdomen interfered with early ambulation and resulted in increased frequency of basal atelectasis in the ETD group. The increased overall complication rate of ETD has also been reported elsewhere [18], [19].
The major causes of postoperative pain are the stretching of the wound during surgery and the total length of the fascial incision [20]. The presence of an additional tube through the abdominal cavity acts as a constant source of stretching and consequently results in pain. Thus it is not surprising to find out that the pain scores in ETD group were significantly higher as compared to the OP group. The maximum scores of pain were observed at 8 hours postoperatively in both the groups, presumably due to exhaustion of the effects of analgesia and anesthesia. To the best of our knowledge, none of the studies published so far in English Literature have alluded to this aspect of comparison. Patients receiving laparoscopy had significantly lower pain scores as compared to their open counterparts, probably due to the lesser length of fascial incisions.
Less postoperative pain and absence of an additional tube drain translated into early ambulation, acceptance of orals and discharge of patients in the OP group. This was also reflected in the earlier resumption of activities of daily life by this group of patients. Another factor contributing to early discharge of patients in the OP group was the absence of bile leak and consequent early removal of the tube drain. Data published by Muftuoglu et al. [21] and Utkan et al. [22] support our study. We did not encounter any mortality. In our study there were three recurrences (10.72%) in ETD group and none in OP group. Malik et al. [8] published similar results with a recurrence rate of 12% in ETD and none in OP.
Obviously, OP cannot be offered to all the patients, especially in a country like India where abdominal tuberculosis is rampant causing fibrosis of omentum making its mobilization difficult. One of the criticisms of our study is that it was not a double blinded study. However, the postoperative pain assessment was somewhat blinded as all scoring was performed by the attending nurse who was unaware of the ongoing study. Our study may also be criticized on the plea that we did not do a cost analysis. It was not done because we were offering both laparoscopy and open procedures and as we were not having a dedicated laparoscopic unit for this study, cost assessment of wear and tear of the reusable instruments and other materials like insufflation agents was difficult.
Conclusion
From our study we conclude that for the management of residual hepatic hydatid cyst cavity OP is a better surgical procedure than ETD as there are lesser chances of cavity infection, bile leakage and recurrence. OP also has an added advantage of decreased postoperative pain. We recommend that OP should be the preferred approach whenever possible. Additional studies may be needed to substantiate the facts.
Notes
Competing interests
The authors declare that they have no competing interests.
Authors’ contribution
AR & AAW conceived the study, operated the patients and drafted the manuscript. ARL, SMK, MAC and SAR were involved in the work-up and postoperative management of the patients and did the literature survey and critical revisions of the manuscript. All the authors have read and approved the manuscript.
References
- 1.Xynos E, Pechlivanides G, Tzortzinis A, Papageorgiou A, Vassilakis JS. Hydatid disease of the liver. Diagnosis and surgical treatment. HPB Surg. 1991 May;4(1):59–66. doi: 10.1155/1991/45101. Available from: http://dx.doi.org/10.1155/1991/45101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Mushtaque M, Mir MF, Malik AA, Arif SH, Khanday SA, Dar RA. Atypical localizations of hydatid disease: Experience from a single institute. Niger J Surg. 2012;18(1):2–7. doi: 10.4103/1117-6806.95466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Mentes A, Yüzer Y, Ozbal O, Coker A, Ilter T, Musoğlu A. Omentoplasty versus introflexion for hydatid liver cysts. J R Coll Surg Edinb. 1993 Apr;38(2):82–85. [PubMed] [Google Scholar]
- 4.Kama NA, Sahin M, Göçmen E, Bayrak M, Kulaçoğlu H, Akat AZ. The results of surgical techniques in hepatic hydatidosis: treatment with drainage versus treatment without drainage--a 6-year experience. J R Coll Surg Edinb. 1998 Aug;43(4):254–256. [PubMed] [Google Scholar]
- 5.Demirci S, Eraslan S, Anadol E, Bozatli L. Comparison of the results of different surgical techniques in the management of hydatid cysts of the liver. World J Surg. 1989 Jan-Feb;13(1):88–90. doi: 10.1007/BF01671161. Available from: http://dx.doi.org/10.1007/BF01671161. [DOI] [PubMed] [Google Scholar]
- 6.Rakas FS, el-Mufti M, Mehta PM, Abuthina H, Challeni CR. Omentoplasty or tube drainage for the management of the residual cavity following the removal of an hepatic hydatid cyst. Hepatogastroenterology. 1990 Dec;37 Suppl 2:55–57. [PubMed] [Google Scholar]
- 7.Atmatzidis KS, Pavlidis TE, Papaziogas BT, Mirelis C, Papaziogas TB. Recurrence and long-term outcome after open cystectomy with omentoplasty for hepatic hydatid disease in an endemic area. Acta Chir Belg. 2005 Apr;105(2):198–202. [PubMed] [Google Scholar]
- 8.Malik AA, Bari S, Shah KA, Shah FA, Amin R. External tube drainage versus omentopexy in the management of residual hepatic hydatid cyst cavity. Internet J Surg. 2008;15(1) doi: 10.5580/cb8. Available from: http://dx.doi.org/10.5580/cb8. [DOI] [Google Scholar]
- 9.Bilge A, Sözüer EM. Diagnosis and surgical treatment of hepatic hydatid disease. HPB Surg. 1994;8(2):77–81. doi: 10.1155/1994/95701. Available from: http://dx.doi.org/10.1155/1994/95701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reddy CR, Narasiah IL, Parvathi G, Rao MS. Epidemiology of hydatid disease in Kurnool. Indian J Med Res. 1968 Aug;56(8):1205–1220. [PubMed] [Google Scholar]
- 11.Rana UV, Sehgal S, Bhatia R, Bhardwaj M. Hydatidosis in animals in and around Delhi. J Commun Dis. 1986 Jun;18(2):116–119. [PubMed] [Google Scholar]
- 12.Merrett N, Hunt DR. Recurrent hepatic hydatid disease or prior omentoplasty: diagnostic dilemma. Aust N Z J Surg. 1989 Oct;59(10):791–794. doi: 10.1111/j.1445-2197.1989.tb07010.x. Available from: http://dx.doi.org/10.1111/j.1445-2197.1989.tb07010.x. [DOI] [PubMed] [Google Scholar]
- 13.Akin ML, Erenoglu C, Uncu EU, Basekim C, Batkin A. Surgical management of hydatid disease of the liver: a military experience. J R Army Med Corps. 1998 Oct;144(3):139–143. doi: 10.1136/jramc-144-03-04. Available from: http://dx.doi.org/10.1136/jramc-144-03-04. [DOI] [PubMed] [Google Scholar]
- 14.Gourgiotis S, Stratopoulos C, Moustafellos P, Dimopoulos N, Papaxoinis G, Vougas V, Hadjiyannakis E. Surgical techniques and treatment for hepatic hydatid cysts. Surg Today. 2007;37(5):389–395. doi: 10.1007/s00595-006-3398-z. Available from: http://dx.doi.org/10.1007/s00595-006-3398-z. [DOI] [PubMed] [Google Scholar]
- 15.Arikan S, Kocakusak A, Yucel AF, Daduk Y. Evaluation of tube drainage method in the treatment of hydatid cyst of liver. Hepatogastroenterol. 2007;54(74):470–474. [PubMed] [Google Scholar]
- 16.Marincaş M, Brătucu E, Badarau A, Straja D, Boru CE, Stefan I, Drilea E. External drainage of the hepatic post hydatid remnant cavity. Chirurgia (Bucur) 2009 Mar-Apr;104(2):151–157. [PubMed] [Google Scholar]
- 17.Platell C, Cooper D, Papadimitriou JM, Hall JC. The omentum. World J Gastroenterol. 2006;6(2):169–176. doi: 10.3748/wjg.v6.i2.169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Ozacmak ID, Ekiz F, Ozmen V, Isik A. Management of residual cavity after partial cystectomy for hepatic hydatidosis: comparison of omentoplasty with external drainage. Eur J Surg. 2000 Sep;166(9):696–699. doi: 10.1080/110241500750008448. Available from: http://dx.doi.org/10.1080/110241500750008448. [DOI] [PubMed] [Google Scholar]
- 19.Reza Mousavi S, Khoshnevis J, Kharazm P. Surgical treatment of hydatid cyst of the liver: drainage versus omentoplasty. Ann Hepatol. 2005 Oct-Dec;4(4):272–274. [PubMed] [Google Scholar]
- 20.Rashid A, Nazir S, Kakroo SM, Chalkoo MA, Razvi SA, Wani AA. Laparoscopic interval appendectomy versus open interval appendectomy: a prospective randomized controlled trial. Surg Laparosc Endosc Percutan Tech. 2013 Feb;23(1):93–96. doi: 10.1097/SLE.0b013e318277df6a. Available from: http://dx.doi.org/10.1097/SLE.0b013e318277df6a. [DOI] [PubMed] [Google Scholar]
- 21.Muftuoglu MA, Koksal N, Topaloglu U. The role of omentoplasty in the surgical management of remnant cavity in hepatic hydatid cyst. HPB (Oxford) 2005;7(3):231–234. doi: 10.1080/13651820410022889. Available from: http://dx.doi.org/10.1080/13651820410022889. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Utkan NZ, Cantürk NZ, Gönüllü N, Yildirir C, Dülger M. Surgical experience of hydatid disease of the liver: omentoplasty or capitonnage versus tube drainage. Hepatogastroenterology. 2001 Jan-Feb;48(37):203–207. [PubMed] [Google Scholar]