Abstract
Background
The aim of this study was to measure ultraviolet radiation (UVR) exposures of lifeguards in pool settings and evaluate their personal UVR protective practices.
Methods
Lifeguards (n = 168) wore UVR sensitive polysulfone (PS) film badges in wrist bracelets on 2 days and completed a survey and diary covering sun protection use. Analyses were used to describe sun exposure and sun protection practices, to compare UVR exposure across locations, and to compare findings with recommended threshold limits for occupational exposure.
Results
The measured UVR exposures varied with location, ranging from high median UVR exposures of 6.2 standard erythemal doses (SEDs) to the lowest median of 1.7 SEDs. More than 74% of the lifeguards’ PS badges showed UVR above recommended threshold limits for occupational exposure. Thirty-nine percent received more than four times the limit and 65% of cases were sufficient to induce sunburn. The most common protective behaviors were wearing sunglasses and using sunscreen, but sun protection was often inadequate.
Conclusions
At-risk individuals were exposed to high levels of UVR in excess of occupational limits and though appropriate types of sun protection were used, it was not used consistently and more than 50% of lifeguards reported being sunburnt at least twice during the previous year.
Keywords: lifeguards, occupational UVR exposure, sun protection behaviors
INTRODUCTION
Outdoor workers are a group that receives regular and significant solar ultraviolet radiation (UVR) exposures [Holman et al., 1983; Larko and Diffey, 1983; Herlihy et al., 1994], often well in excess of recommended guidelines [Rosenthal et al., 1988; Gies and Wright, 2003]. However, measures to help reduce the UVR exposures of outdoor workers using personal protective equipment such as hats, clothing, sunscreens, and sunglasses (sometimes provided by employers in the US) have not been well accepted and appear to be adopted on an ad hoc basis, depending upon the employer [Glanz et al., 2007]. Occupational exposure to solar UVR is a risk and one that employers may be under a legal obligation to control.
Occupational exposure to UVR was first addressed by the American Congress of Governmental and Industrial Hygienists (ACGIH) in the late 1960s, when they produced threshold limit values (TLV’s) for a range of wavelengths across the ultraviolet region of the spectrum [ACGIH, 2008]. These ACGIH TLV’s have subsequently been adopted by the International Radiation Protection Association (IRPA) in 1989 [IRPA, 1989] and then by the International Commission on Non-Ionizing Radiation Protection [ICNIRP, 1999]. The occupational exposure limit is a maximum personal daily dose of 30 J m−2 of UVR, weighted for the spectral characteristics of the radiation. In December 2006 Australia introduced a Radiation Protection Standard covering occupational exposure to UVR [ARPANSA, 2006] utilizing the TLV’s of ACGIH and ICNIRP and adding a risk management approach listing the responsibilities of both employers and employees in reducing UVR exposures. Compliance with allowed exposure limits will be made mandatory for occupational exposures to artificial sources of UVR but a risk management approach applies to reducing exposures of outdoor workers to solar UVR.
In this study, where lifeguards as outdoor workers are the subjects, comparison with the ACGIH and ICNIRP TLV’s and the UVR exposure limit of 30 J m−2 is particularly relevant. The weighted dose calculated using the erythemal spectral response function of the Commission Internationale de l’Eclairage [CIE, 1987] allows comparison with previous research. Weighting solar UVR with the ACGIH/ICNIRP action spectrum produces a weighted irradiance that is smaller than the CIE erythemal response weighted irradiance. As the two spectral responses differ at wavelengths above 300 nm, changes in the spectral distribution of incident solar UVR with changing zenith angle during the day, will produce differing effects when weighted with the responses of the CIE and the ACGIH/ICNIRP. The differences in the two response functions below 290 nm play no role for solar UVR exposures as there is little solar UVR below 290 nm at the earth’s surface at mid latitudes. Comparisons of both ACGIH/ICNIRP and CIE weighted solar irradiances have been done previously [Gies and Wright, 2003], where the ratio of CIE to ACGIH/ICNIRP weighted irradiance is approximately 4 during the day between 9 a.m. and 5 p.m. while the sun is high enough in the sky to produce significant weighted irradiance. This is also when most of the day’s biologically effective UVR dose is incident.
Both UV Index forecasts and measurements can be used to estimate the potential hazards of sun exposure when outdoors and these are available online for many locations in the US UV Index Websites (2008). Solar UVR weighted against the CIE erythemal effectiveness is used to generate the UV Index [ICNIRP, 1995; WHO, 2002], and a figure of 0.30 W m−2 effective when multiplied by 40 gives a corresponding UV Index of 12. In recent years the CIE has introduced the concept of a standard erythemal dose (SED), where 1 SED is defined as 100 J m−2 effective [CIE, 1999] when weighted with the erythemal response function of the CIE [1987]. The relationship between solar UVR intensity in UV Index and the times to exceed the ACGIH/ICNIRP TLV of 30 J m−2, and the time required to exceed 2 SEDs and achieve erythema for people with sensitive skin, is given in Table I. For the levels of solar UVR typical in summer (UV Index values of 10–12), Table I shows that people will exceed the TLV’s of the ACGIH/ICNIRP in 6–8 min and people with sensitive skin will achieve erythema in 11–13 min. For anyone outside for periods exceeding 10 min, including outdoor workers, use of sun protection is therefore both necessary and advisable.
TABLE I.
The Variation of Time to Exceed the TLVs of the ACGIH and ICNIRP Guidelines, the Time to Achieve Erythema, and the Equivalent SEDs/hr for Solar UVR of Various UV Indices
| UV Index | Time to exceed TLV (min) | Time to achieve erythema (min) | Ambient UVR (SEDs/hr) |
|---|---|---|---|
| 3 | 26.4 | 44.4 | 2.7 |
| 4 | 19.8 | 33.3 | 3.6 |
| 6 | 13.2 | 22.2 | 5.4 |
| 8 | 9.9 | 16.7 | 7.2 |
| 10 | 7.9 | 13.3 | 9.0 |
| 12 | 6.6 | 11.1 | 10.8 |
| 14 | 5.7 | 9.5 | 12.6 |
Note that WHO recommend that protection against solar UVR be used when the UV Index is 3 or greater [WHO, 2002].
The World Health Organization (WHO) has recommended that for latitudes between 30°N and 30°S sun protection should be used all year round and for latitudes between 30°N and 40°N sun protection should be used between May and August [WHO, 1995], recommendations that would apply to many areas of the United States and are relevant to outdoor workers. Little quantitative information is available about the sun exposure and protection practices of one highly exposed group of outdoor workers, lifeguards. Lifeguards are exposed to potentially high levels of ambient UVR as a result of their occupational duties, yet little has been done to quantify the levels they receive while on duty. The aim of this study was to measure UVR exposures of lifeguards in pool settings in four metropolitan regions of the United States and evaluate their personal UVR protective practices.
MATERIALS AND METHODS
Participants and Setting
The data reported here come from a study conducted in association with a nationwide dissemination study of a skin cancer prevention program at swimming pools entitled Diffusion of an Effective Skin Cancer Prevention Program [Glanz et al., 2005]. All procedures were approved by the Institutional Review Board (IRB) at Emory University. Sixteen pools in four metropolitan areas were invited to participate. After a call for pools willing to participate in this additional ancillary study, pools were chosen to conform to the study design and maximize the prospects for successful study completion. Pools were required to have a minimum staff of 15 lifeguards as well as be able to recruit no less than 15 parent and children pairs for the overall study. The pool locations were selected equally from two different regions of geographic latitude and therefore different ambient solar UVR: two areas were at <35° latitude (southern: Phoenix, Arizona and Austin, Texas) and two areas were >40° latitude (north: Omaha, Nebraska and Portland, Oregon). The target sample to complete the study was 10 lifeguards from each of the 16 pools. Data collection took place over a 4-day period that included 2 weekdays and 2 weekend days, and involved 2 days of on-site data collection. Data were collected in June and July of 2006. Each lifeguard completed three self-report measures (baseline survey, 4-day diary, and final survey). They were also observed twice by research staff (on 1 weekday and 1 weekend day) to evaluate their use of observable sun protection [O’Riordan et al., 2009]; and wore polysulfone (PS) dosimeters to measure personal UVR exposure for 2 days.
Recruitment and Data Collection Procedures
On the day preceding the start of data collection, lifeguards were approached as they arrived at the pool for work, or during a break. Study procedures were explained to potential participants and those who agreed to participate signed consent forms and completed a baseline survey. Of the 213 eligible lifeguards, 185 or 86.9% agreed to participate (13.1% refusal rate). Of these 185 lifeguards who agreed to participate, 17 failed to actually do so.
Self-Report Measures: Sun Habits Survey and Diary
To compare self-reported sun exposure and sun protection practices with independent assessments, both a survey and a 4-day diary were used. The survey included the main outcome measures used in a previous study [Glanz et al., 2005], and is typical of large population intervention trial measures [Glanz and Mayer, 2005; Glanz et al., 2008]. The diary provided a more precise time-matched measure of sun exposure and protection, for comparison with the objective indicators. The Sun Habits Survey included questions on sun-protection habits, sunscreen use patterns, skin cancer risk factors, sunburn history, UVR exposure, and demographics, using measures selected or adapted from tools used in earlier studies [Glanz et al., 2002]. Demographic information gathered on the surveys included gender, age, race/ethnicity, income level, and marital status. Skin cancer risk for the lifeguards was assessed by self-report through a brief version of the brief skin cancer risk assessment tool (BRAT) [Glanz et al., 2003] scale in the survey. Skin cancer risk factor questions included skin color, hair color, eye color, sunburn history, tanning propensity, and history of skin cancer. These were used to categorize participants into low, moderate, or high-risk groups. The brief set of risk factor items was based on previous studies [Weinstock, 1992] and adapted from the [Glanz et al., 2003].
On the surveys, usual solar UVR exposure was assessed by two questions asking the average number of hours (1 or less, 2,3,4,5, or 6) spent in the sun between 10 a.m. and 4 p.m. during the summer on weekdays and on weekends. A weekly average number of daily hours of sun exposure was computed by multiplying the weekday average by 5, and the weekend average by 2, and dividing by 7.
Sun protection habits included whether participants wear a shirt with sleeves, use sunscreen, wear sunglasses, seek shade, and wear a hat when outside on a sunny day and were measured on a 4-point ordinal scale ranging from 1 (rarely or never) to 4 (always). A composite sun protection habits score for each subject was calculated by adding the responses to all five items on the 1–4 point ordinal scale and dividing by 5. Similarly, a composite score for each form of sun protection was calculated using the responses of all lifeguards and the 4-point ordinal scale and averaging over the lifeguards.
The Sun Habits Diary is a record of sun exposure and protective behavior, adapted from a diary developed for earlier skin cancer prevention research [Glanz et al., 1997]. Participants were instructed to complete the diary from 10 a.m. to 4 p.m. (6 hr including midday) for 4 consecutive days (including 2 weekend days), which was used to estimate weekly sun exposure and sun protection. To report sun exposure and protection, participants were asked to record whether they were outdoors for each hour of the day between 10 a.m. and 4 p.m. as well as to indicate any protective habits that they used for the hours when they were outside (sunscreen, hat, shade, shirt with sleeves, sunglasses). A weekly percentage of each sun-protection habit for the corresponding times being outside was computed by multiplying the weekday average by 5, the weekend average by 2, dividing by 7, and converting that time to a percentage.
The validity of the survey and diary instruments for assessing sun protection habits including sunscreen use and sun protection with hats, shirts, and sunglasses was established in earlier analyses from this study [Glanz et al., 2009; O’Riordan et al., 2009].
Personal UVR Exposure Data Collection
The UVR exposure of approximately 10 lifeguards per pool (minimum 7 and maximum 13) was monitored from 8 a.m. to 4 p.m. each day at the four participating pools in each city: Austin, Phoenix, Omaha, and Portland. To measure UVR exposure, each lifeguard wore a PS badge in a protective wrist bracelet, shown previously to be a reliable site for personal dosimetry [Thieden et al., 2000]. The total number of lifeguard exposures over the 6 hr badge periods was 336 from 168 individuals, of which 329 were completed, returned, and measured (a 98% return rate). However, complete survey and diary data were available for only 162 of the lifeguards.
Ambient Solar UVR
Each day of the study, pairs of PS badges were placed on a horizontal unshaded surface to measure the mean ambient solar UVR (and its standard deviation) incident at the pool setting. Each pair of badges was changed over and replaced with new badges every hour on the hour from 9 a.m. until 4 p.m. The UVR measurement data from each set of badges provided a continuous measurement that could be summed to obtain the total solar UVR incident that day between the hours of 8 a.m. to 4 p.m. while the study was underway, while also providing an indication of how solar UVR varied each hour during the exposure period.
Polysulfone Film Dosimeters
PS film has been used as a UVR dosimeter since 1976 [Davis et al., 1976]. The absorbance of the PS film changes on exposure to UVR and can be related to the incident erythemally effective dose (EED) in J m−2. The dose–response to solar UVR of the PS film used in this study was determined from simultaneous exposure of the PS film and measurement of the incident solar UVR spectra at the ARPANSA laboratory in Melbourne, described previously [Herlihy et al., 1994; Gies and Wright, 2003]. The incident spectra are weighted with either the erythemal response of the Commission International de l’Eclairage [CIE, 1987] or that of the ACGIH [2008] and ICNIRP [1999] to give the effective UVR in W m−2. The EED in J m−2 can be obtained from integrating the effective UVR in W m−2 over the time the badge is exposed.
Previous studies [Diffey, 1987, 1989] recommended that the PS exposures should be kept within the “linear” region, where the change in absorbance, ΔA is <0.3. However, given the high UVR levels in summer, the absorbance of PS badges exposed for an hour in an unshaded position can often exceed this ΔA <0.3 limit. Therefore an upper limit for ΔA of 0.5 has been used wherever possible, both in previous studies [Herlihy et al., 1994; Gies et al., 1995; Gies and Wright, 2003] and also in this study. As in these previous studies, this study used 35 μm PS film mounted on preglued white cardboard holders 25 mm × 40 mm with a central aperture of 8 mm. PS film badges were constructed by ARPANSA, numbered sequentially, the initial absorbance measured at 330 nm, and the badge then stored in an envelope impervious to UVB. Both the absorbance measurements (pre- and postexposure) were made on the same Varian DMS 90 UV/visible spectrophotometer.
Statistical Analysis
Preliminary analyses included calculating descriptive statistics for all variables and scales and examining survey and diary completion rates, and dosimeter return rates, for lifeguards at each pool. To assess the self-reported UVR exposures of the lifeguards, median times reported outside on the surveys, and diaries were calculated.
After laboratory testing, the objectively measured PS badge data were converted to logarithm SEDs described and then compared descriptively by city. Then, the ambient UVR at each location was computed from the ambient PS badges. Results from the personal PS wristband were divided by results from the ambient badges to compute the percent of ambient UVR received by each participant. Last, comparison of the PS badge data and the recommendations of the ACGIH/ICNIRP weighted exposures were made.
Lifeguard responses to surveys and diaries were also analyzed to determine the reported usage of each type of sun protection. From the surveys, patterns of use of forms of sun protection were compared between baseline and follow-up assessments. To provide a continuous measure of sun protection use and for comparisons between cities, diary data were used. The number of hours using each form of protection was divided by the number of hours outdoors, to obtain the percentage of time outdoors that lifeguards used sun protection. To determine if the use of sun protection differed by city, the individual items were examined using one-way analysis of variances (ANOVAs) with city as the between-subjects factor. All significant main effects were followed with Tukey post hoc tests to determine any differences by city. All analyses were conducted in SPSS 16.0.
RESULTS
Sample Characteristics
The 168 participating lifeguards were 59.3% females, averaged 19.4 years old (SD = 5.6), and mostly white (89.9%) and unmarried (98.1%). Most were either high school students or graduates (51.3%) or college students (41%). The lifeguards were categorized into groups at low (28.4%), moderate (35.8%), and high risk (35.8%) for skin cancer. The mean number of sunburns reported for the previous summer was 2.2 ± 1.3 (median 2.0).
UVR Exposures of Lifeguards
The amount of time spent outside varied considerably among lifeguards, although most of the lifeguards reported that they spent significant time outside, with median times of 4.29 hr per day initially and 4.43 hr/day in the follow-up (based on the 6 hr covered by the surveys). The objectively measured UVR exposures of individual lifeguards varied considerably, following a log–normal distribution with measured exposures ranging from a low of 0.1 SEDs up to maximum individual exposures of approximately 30 SEDs depending upon the location (Table II). Maximum measured UVR exposures for individual lifeguards at each location were 31.8 SEDs in Austin, 30.6 SEDs in Phoenix, 23.1 SEDs in Omaha, and 10.9 SEDs in Portland. A graph of the logarithm of measured UVR exposures in SEDs versus the number of lifeguards with that exposure for all four locations is shown in Figure 1. The peak of the graph occurs between approximately 5 and 10 SEDs, depending on the location, easily sufficient to induce erythema in any of the lifeguards with fair to medium skin types who were not using sun protection.
TABLE II.
A Comparison for Each of the Different Locations of the Measured Medians (and Inter Quartile Ranges, IQR) of UVR Exposures of Lifeguards in SEDs and as a Percentage of Ambient UVR, as Well as the Time Spent Outside in Hours
| Lifeguard PS dosimeters | Austin (n = 80) | Phoenix (n = 81) | Omaha (n = 84) | Portland (n = 84) | All sites (n = 329)a |
|---|---|---|---|---|---|
| Median UVR (SEDs) | 3.3 | 3.2 | 6.2 | 1.7 | 3.3 |
| IQR | 1.3–7.2 | 0.8–10 | 3.0–8.0 | 0.68–3.6 | 1.2–6.8 |
| Median % ambient | 12 | 18 | 29 | 12 | 16 |
| IQR | 4.0–22 | 4.4–37 | 13–37 | 64–22 | 5.6–28 |
| Median time | 4.3 | 4.3 | 5.4 | 4.0 | 4.4 |
| Outside (hr) IQR | 3.0–5.6 | 2.2–6.4 | 4.3–6.5 | 1.9–6.1 | 2.6–6.2 |
| Median UVR | |||||
| ACGIH J m−2 | 82 | 84 | 156 | 43 | 84 |
| % >30 J m−2 | 73 | 73 | 88 | 63 | 74 |
| % >2 SEDs | 64 | 68 | 85 | 44 | 65 |
| Ambient solar UVR | |||||
| Mean | 31.3 ± 6.4 | 30.6 ± 6.9 | 27.1 ± 3.7 | 16.1 ± 5.6 | |
| Range (SEDs) | 19–39 | 23–42 | 21–38 | 10–25 | |
The UVR exposures in terms of ACGIH weighted exposures, as well as the percentage of lifeguards exceeding the TLV of 30 J m−2 are also shown as is the percentage exceeding an exposure of 2 SEDs (approximately equivalent to an erythemal dose for people with fair skin). Lastly, mean measured daily total ambient solar UVR in SEDs is shown for each location.
Each lifeguard wore a PS dosimeter on 2 separate days, n = 168 lifeguards and 329 dosimeters completed, returned, and measured.
FIGURE 1.
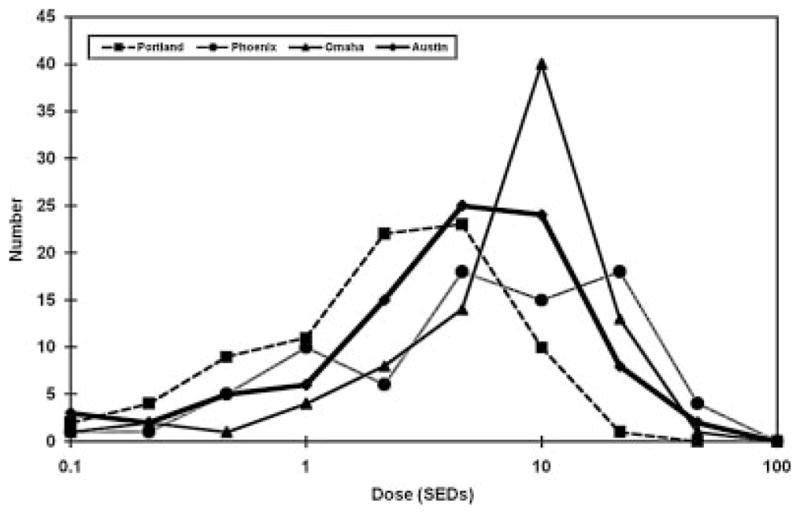
A graph of the measured exposures in SEDs for all the workers, indicating that the exposure distributions approximate a log–normal distribution.
Comparison of Measured Exposures by Location
Table II shows the median measured UVR exposures in SEDs for each group of lifeguards by location. The highest median was for the Omaha lifeguards with 6.2 SEDs, compared with Austin 3.3 SEDs, and a median in Phoenix of 3.2 SEDs, despite the fact that both Austin and Phoenix had higher measured mean daily ambient UVR than in Omaha (30 SEDs vs. 27 SEDs) (Table II). The major reason for the higher UVR exposures for the lifeguards in Omaha in comparison to the other locations is that they spent at least an hour longer outside in similar ambient UVR than did the lifeguards in Austin and Phoenix (Table II). The varying amount of shade available at the different pools or due to individuals’ shade seeking due to higher temperatures in the more southern locations may also have contributed to this difference. Portland lifeguards had the lowest median UVR exposures at 1.7 SEDs, as well as the lowest measured mean ambients, likely due to being farthest north of all of the locations. The distributions of UVR exposures by location in Figure 1 also show that Portland UVR exposures are concentrated at lower levels while the distributions for Omaha and Austin are concentrated at higher levels. As exposures above 2 SEDs are expected to induce erythema in people with fair skin, a large proportion of the lifeguards could have been sunburnt unless they were using sun protection.
Table II also shows the median percentage of ambient UVR received by lifeguards at each location, calculated by comparing the individual lifeguard’s measured exposure against the local ambient PS badge measurements made at the same time. Austin and Portland lifeguards both had a median percentage of ambient UVR of 12%, which given that Austin had almost twice as much ambient solar UVR meant that the Austin lifeguard exposures were approximately twice as high. The Omaha lifeguards received not only the largest UVR exposures but also received a median of 29% of ambient, the highest percentage of all locations.
Comparison With Occupational TLVs
Also shown in Table II are the median occupational exposures in terms of the ACGIH/ICNIRP weighted exposures, which can be compared against the TLV of 30 J m−2. Table II shows the percentage of lifeguards whose badges received UVR exposures in excess of the allowed TLV. Across all sites 74% of the workers exceeded the limits, with Omaha the highest at 88%, followed by Phoenix (73%), Austin (73%), and Portland (63%). PS badge measurements indicated that 39% of all workers, received in excess of four times the TLV. For a typical summer’s day with a maximum UV Index of 12, it takes approximately 6 min to exceed the TLVs but takes longer to achieve erythema for people with skin types I and II [Fitzpatrick, 1988], approximately 11 min. Table II also shows that 65% of all lifeguards’ PS badges received sufficient solar UVR to possibly sunburn (2 SEDs), with Omaha again leading with 85%, then Phoenix (68%), Austin (64%), and Portland (44%).
Use of Personal Sun Protection
The types of personal sun protective behavior practiced by the lifeguards and assessed in this study were: sunscreen, hat, shirt, sunglasses, and the use of shade. Survey responses provided data on “usual” use of the different forms of protection (rarely or never, sometimes, usually, always) and the percentage of time each lifeguard used each form of sun protection during the 4-day study period were calculated from the diaries.
Generally, there was little difference between the use patterns of sun protective behaviors for the two survey occasions, baseline, and follow-up. Sunglasses were most commonly used, with a composite score of 3.5, followed by sunscreen (composite score 2.8), shade (composite score 2.3), and shirts (composite score 2.1). Hats were the type of protection used least often (composite score 2.0).
Table III shows the weekly percentage of time each item was used while outside calculated from diary data. Again, sunglasses are the most frequently used method (median 82.4% of time) followed by sunscreen (median 51.2%). Shade (median 17.2%), hat (median 15.7%), and shirts (median 15.0%) were least used.
TABLE III.
The Median Weekly Percentage of Time Outside Using the Various Sun Protection Behaviors From the Lifeguard Diary Descriptives, Overall, and by City
| Overall (n = 162) | Austin (n = 40) | Phoenix (n = 41) | Omaha (n = 41) | Portland (n = 39) | |
|---|---|---|---|---|---|
| Using sunglasses | 82.4 | 71.9 | 90.4 | 83.9 | 83.9 |
| Using sunscreen | 51.23 | 6.2 | 76.4 | 52.0 | 50.0 |
| Using a hat | 15.7 | 37.0 | 33.3 | 0.0 | 31.5 |
| Using a shirt | 15.0 | 19.9 | 29.2 | 6.9 | 31.3 |
| Using shade | 17.2 | 31.2 | 25.6 | 11.9 | 9.1 |
The variation in use of sun protection by city is also shown in Table III. Mean differences between cities were explored through the use of one-way ANOVAs with city as the between-subjects factor and each sun protection category as dependent variables. Sunglasses use was the most often used form of sun protection and was consistent across cities. Lifeguards in Omaha, which had the highest UVR exposures also used significantly less sun protection, other than for sunglasses and sunscreen use.
DISCUSSION
As in previous studies on outdoor workers, the current study shows that measured solar UVR exposures of the lifeguards were often substantial, with 65% of them in excess of the occupational TLVs and with almost 40% of all workers’ PS badges exceeding the TLVs by more than four times. There was also a wide distribution of exposures (Fig. 1). UVR exposures do not follow a normal distribution but generally follow a log–normal distribution covering a wide range of exposures [Diffey and Gies, 1998]. The very high measured UVR exposures were especially alarming when considered together with the lack of controls for minimizing exposure and the predominantly white sample of workers in this study. These results suggest that solar UVR exposure is not being taken seriously as a hazard in workplaces, particularly in one with such an obvious UVR exposure potential and that there is a significant risk to the health of outdoor workers, particularly lifeguards, in the US from occupational UVR exposure. Overall, lifeguards use of sun protection practices varied substantially depending on the method of protection and geographic location, with the lowest levels of sun protection being observed in Omaha, a site with the highest measured UVR exposures.
Very few of the lifeguards in this study were appropriately and adequately protected. Adequate protection was defined (for the purpose of this study) as using all five forms of sun protective behavior; that is, hats, shirts, sunscreens, sunglasses, and shade use and achieving an average composite score for the five forms of protection of 2.5 or higher.
Use of sun protection by the lifeguards was variable, with sunglasses having the highest usage followed by sunscreens, which was encouraging with the second highest usage of the five forms of protection. Reduction in sun exposure by the use of sunscreen has been demonstrated to reduce the rate of squamous cell carcinoma and daily use of sunscreen can reduce the rate of appearance of new solar keratoses and increase the rate at which existing keratoses regress [Pathak, 1991; Thompson et al., 1993]. The overall mean composite scores for all sun protective behaviors for both the baseline survey and follow-up were 2.56. However, without the high composite scores from sunglass use, which contribute very little to skin cancer prevention, the overall means were 2.33 and 2.34, respectively, which indicate that less than half of the lifeguards were in the categories usually or always use sun protection.
The measured levels of exposure reported in Table II are very high. Previous measurements of personal exposure to solar UVR [Gies et al., 1995] have shown that the measured personal exposures are generally dependent upon the ambient levels. Given that the study was conducted at different times over the summer in different locations, it is very likely that had it been possible to conduct all of the measurements in the height of summer, the exposures would have been higher. The measured mean lifeguards’ exposures range from 12% to 29% of ambient and are in general agreement with previous studies where PS badges were attached to the back of the hand, with results ranging from 15% to 65% [Holman et al., 1983; Herlihy et al., 1994]. A previous study of outdoor workers in Queensland [Gies et al., 1995] that looked at lifeguards in beach settings, found for the period during which the subjects were outdoors, the chest badges of lifeguards received 21% of available ambient UVR, which compares closely with the overall mean of this study of 20.5%.
The skin cancer risk was moderate or high for 71.6% of the lifeguards, of whom 89.9% were white. This seems to indicate that overall a substantial proportion of the lifeguards were susceptible to sunburn and its associated health effects if not properly protected. This is similar to two studies on outdoor workers in California, where although a majority of farmworkers (78%) had skin types that had a high propensity to tan and a low propensity to burn [Salas et al., 2005], a substantial proportion (22%) did not, while another study on construction, transport, and postal workers [Stepanski and Mayer, 1998], found 33% of the workers reported having skin types I and II on the Fitzpatrick skin type classifications [Fitzpatrick, 1988]. Another study on outdoor workers in the building and construction industry in Queensland [Gies and Wright, 2003] also found that a substantial proportion of the workers (42%) had skin types I and II. Given the potential skin cancer risk of these individuals involved in outdoor occupations that are exposed to high levels of ambient UVR, it is crucial that sun protection interventions are developed and tailored to their personal needs. To try and ensure that they reduce the levels of personal UVR exposure they receive, a comprehensive approach utilizing all forms of sun protection on a regular basis with good cooperation between employees and their employer would be a positive starting point.
Possible limitations of this study may be that the measurements were only done on 2 days for each group of lifeguards. The natural shade available at each of the pools also varied considerably, which in some cases would limit the participants’ ability to use shade to reduce solar UVR exposures, although all locations had shade on-site in the form of a lifeguard office and/or locker room area. The variation in natural shade was accounted for by the fact that each location had ambient solar UVR measurements carried out at that location during the day, making it possible to compute exposure as “percent of ambient UVR” in the local area in the immediate vicinity of the pool. As all pools were participating in the Pool Cool diffusion study [Glanz et al., 2005], they had at least some sun protection items such has sunscreen available onsite, and more than 80% had policies to encourage sun safety for their employees. However, despite this apparent commitment to sun safety at the pool sites, lifeguards’ exposures were extremely high and their protection was insufficient. In a recent study in New Zealand, it was found [Hammond et al., 2008] that outdoor workers’ perceptions of workplace support were associated with their sun protection practices. This suggests the importance of workplace level initiatives.
The fact that responses to the follow-up survey did not change appreciably from the initial survey suggest that any social desirability bias, or reactivity, in the study does not appear to have affected the findings. The strengths of this study are the high number of participants in total, the high response rate, and the fact that the survey, the follow-up, and the diaries gave similar results, giving some confidence in the responses of the participants.
The results of this study indicate that lifeguards, a category of outdoor workers with significant potential for exposure to solar UVR, receive substantial UVR exposures, often sufficient to induce sunburn. Despite the use of sun protective measures, the survey questionnaire indicated incidents of overexposure and subsequent sunburn occurred on average 2.2 times for each lifeguard the previous summer. Many of the lifeguards (63–88% depending upon the location) regularly received UVR exposures in excess of the occupational UVR TLVs.
The implications for both the employers and the employee lifeguards of the cumulative effect of these UVR exposures need to be considered. Managers need to make a clear commitment to sun safety and workplace protection [Hammond et al., 2008]. This should be part of a multi-level approach that takes into account employees’ personal attributes, socio cultural, environmental, and organizational factors, and the development of a policy for the particular workplace.
Acknowledgments
Contract grant sponsor: National Cancer Institute; Contract grant number: CA 92505-S1.
The authors are grateful to the Australian Radiation Protection and Nuclear Safety Agency (ARPANSA) which supported the senior author’s use of equipment to analyze the dosimeters. We acknowledge contributions of Lucja Bundy, Kristen Burgess, Lucja Bundy, Dawn Hall, Erica Davis, Nicole Dubruiel, Maria Fawzy, and Nancy Marencin for their assistance with data collection and processing. Dr. Karen Glanz’s effort was supported in part by a Distinguished Scholar Award from the Georgia Cancer Coalition. The study was supported by Grant Number CA 92505 from the National Cancer Institute.
Abbreviations
- ACGIH
American Congress of Governmental and Industrial Hygienists
- ARPANSA
Australian Radiation Protection and Nuclear Safety Agency
- ANOVAs
analysis of variances
- BRAT
brief skin cancer risk assessment tool
- CIE
Commission Internationale de l’Eclairage (International Lighting Commission)
- ΔA
absorbance change
- EED
erythemally effective dose
- ICNIRP
International Commission on Non-Ionizing Radiation Protection
- IRPA
International Radiation Protection Association
- PS
polysulfone
- SEDs
standard erythemal doses
- TLVs
threshold limit values
- UVR
ultraviolet radiation
- WHO
World Health Organization
References
- American Congress of Governmental and Industrial Hygienists. Threshold limit values and biological exposure indices. Cincinnati: ACGIH; 2008. p. 256. [Google Scholar]
- Australian Radiation Protection and Nuclear Safety Agency. Occupational exposure to ultraviolet radiation. Melbourne: ARPANSA; 2006. p. 31. Radiation Protection Series Publication No. 12. http://www.arpansa.gov.au/Publications/codes/rps12.cfm. [Google Scholar]
- CIE Research Note. A reference action spectrum for ultraviolet induced erythema in human skin. CIE J. 1987;6:17–22. [Google Scholar]
- Commission Internationale de L’Eclairage. Erythema reference action spectrum and standard erythema dose. Vienna: CIE; 1999. p. 8. [Google Scholar]
- Davis A, Deane G, Diffey B. Possible dosimeter for ultraviolet radiation. Nature. 1976;261:169–170. doi: 10.1038/261169a0. [DOI] [PubMed] [Google Scholar]
- Diffey B. A comparison of dosimeters used for solar ultraviolet radiometry. Photochem Photobiol. 1987;46:55–60. doi: 10.1111/j.1751-1097.1987.tb04735.x. [DOI] [PubMed] [Google Scholar]
- Diffey B. Ultraviolet radiation dosimetry with polysulphone film. In: Diffey B, editor. Radiation measurement in photobiology. London: Academic Press; 1989. pp. 135–159. [Google Scholar]
- Diffey B, Gies P. The confounding influence of sun exposure in melanoma. Lancet. 1998;351:1101–1102. doi: 10.1016/s0140-6736(05)79381-8. [DOI] [PubMed] [Google Scholar]
- Fitzpatrick T. The validity and practicality of sun-reactive skin types I through VI. Arch Dermatol. 1988;124:869–871. doi: 10.1001/archderm.124.6.869. [DOI] [PubMed] [Google Scholar]
- Gies P, Wright J. Measured solar ultraviolet radiation exposures of outdoor workers in Queensland in the building and construction industry. Photochem Photobiol. 2003;78:342–348. doi: 10.1562/0031-8655(2003)078<0342:msureo>2.0.co;2. [DOI] [PubMed] [Google Scholar]
- Gies P, Roy C, Toomey S, Maclennan R, Watson M. Solar UVR exposures of three groups of outdoor workers on the Sunshine Coast, Queensland. Photochem Photobiol. 1995;62:1015–1021. [Google Scholar]
- Glanz K, Mayer J. Reducing ultraviolet radiation exposure to prevent skin cancer: Methodology and measurement. Am J Prev Med. 2005;29:131–142. doi: 10.1016/j.amepre.2005.04.007. [DOI] [PubMed] [Google Scholar]
- Glanz K, Silverio R, Farmer A. Diary reveals sun protective practices. Skin Cancer Found J 14:27–28. Reprinted as “Daily diary reveals sun protective practices”. Primary Care and Cancer. 1997;17(5):21–23. [Google Scholar]
- Glanz K, Geller A, Shigaki D, Maddock J, Isnec M. A randomized trial of skin cancer prevention in aquatics settings: The Pool Cool program. Health Psych. 2002;21:579–587. [PubMed] [Google Scholar]
- Glanz K, Schoenfeld E, Weinstock M, Layi G, Kidd J, Shigaki D. Development and reliability of a brief skin cancer risk assessment tool. Cancer Detect Prev. 2003;27(4):311–315. doi: 10.1016/s0361-090x(03)00094-1. [DOI] [PubMed] [Google Scholar]
- Glanz K, Steffen A, Elliott T, O’Riordan D. Diffusion of an effective skin cancer prevention program: Design, theoretical foundations, and first year implementation. Health Psychol. 2005;24:477–487. doi: 10.1037/0278-6133.24.5.477. [DOI] [PubMed] [Google Scholar]
- Glanz K, Buller DB, Saraiya M. Reducing ultraviolet radiation exposure among outdoor workers: State of the evidence and recommendations. Environ Health. 2007;6:22–32. doi: 10.1186/1476-069X-6-22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Glanz K, Yaroch AL, Dancel M, Saraiya M, Crane LA, Buller DB, Manne S, O’Riordan DL, Heckman CJ, Hay J, Robinson JK. Measures of sun exposure and sun protection practices for behavioral and epidemiologic research. Arch Dermatol. 2008;144(2):217–222. doi: 10.1001/archdermatol.2007.46. [DOI] [PubMed] [Google Scholar]
- Glanz K, McCarty F, Nehl EJ, O’Riordan DL, Gies P, Bundy L, Locke AE, Hall DM. Validity of self-reported sunscreen use by parents, children and lifeguards. Am J Prev Med. 2009;36:63–69. doi: 10.1016/j.amepre.2008.09.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hammond V, Reeder AI, Gray AR, Bell ML. Are workers or their workplaces the key to occupational sun protection? Health Promot JAus. 2008;19:97–101. doi: 10.1071/he08097. [DOI] [PubMed] [Google Scholar]
- Herlihy E, Gies P, Roy C, Jones M. Personal dosimetry of solar UVR for different outdoor activities. Photochem Photobiol. 1994;60:288–294. doi: 10.1111/j.1751-1097.1994.tb05106.x. [DOI] [PubMed] [Google Scholar]
- Holman C, Gibson I, Stephenson M, Armstrong B. Ultraviolet irradiation of human body sites in relation to occupation and outdoor activity: Field studies using personal UVR dosimeters. Clin Exp Dermatol. 1983;8:269–277. doi: 10.1111/j.1365-2230.1983.tb01779.x. [DOI] [PubMed] [Google Scholar]
- International Commission on Non-Ionizing Radiation Protection. Global solar UV Index. Oberschleissheim: ICNIRP; 1995. p. 21. ICNIRP-1/95. [Google Scholar]
- International Commission on Non-Ionizing Radiation Protection, ICNIRP. Guidelines on limits of exposure to ultraviolet radiation of wavelengths between 180 nm and 400 nm (Incoherent Optical Radiation) In: Matthes R, Bernhardt J, McKinlay A, editors. Guidelines on limiting exposure to non-ionizing radiation. Munich: Markl-Druck; 1999. p. 376. [Google Scholar]
- International Radiation Protection Association/International Committee on Non Ionizing Radiation Protection (IRPA/INIRC) Proposed change to the IRPA 1985 guidelines on limits of exposure to ultraviolet radiation. Health Phys. 1989;56:971–972. [PubMed] [Google Scholar]
- Larko O, Diffey B. Natural UV-B radiation received by people with outdoor, indoor, and mixed occupations and UV-B treatment of psoriasis. Clin Exp Dermatol. 1983;8:279–285. doi: 10.1111/j.1365-2230.1983.tb01780.x. [DOI] [PubMed] [Google Scholar]
- O’Riordan DL, Nehl E, Gies P, Bundy L, Burgess K, Davis E, Glanz K. Validity of covering-up sun protection habits: Association of observations and self-report. J Am Acad Dermatol. 2009;60:739–744. doi: 10.1016/j.jaad.2008.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pathak M. Intrinsic photoprotection in human skin. In: Lowe N, editor. Physicians guide to sunscreens. New York: Marcel Dekker Inc; 1991. pp. 39–49. [Google Scholar]
- Rosenthal F, Phoon C, Bakalian A, Taylor H. The ocular dose of ultraviolet radiation to outdoor workers. Invest Ophthal Visual Sci. 1988;29:649–656. [PubMed] [Google Scholar]
- Salas R, Mayer J, Hoerster K. Sun protective behaviors of California farmworkers. J Occup Environ Med. 2005;47:1244–1249. doi: 10.1097/01.jom.0000177080.58808.3b. [DOI] [PubMed] [Google Scholar]
- Stepanski B, Mayer J. Solar protection behaviours among outdoor workers. J Occup Environ Med. 1998;40:43–48. doi: 10.1097/00043764-199801000-00009. [DOI] [PubMed] [Google Scholar]
- Thieden E, Agren MS, Wulf HC. The wrist is a reliable body site for personal dosimetry of ultraviolet radiation. Photodermatol Photo-immunol Photomed. 2000;16:57–61. doi: 10.1034/j.1600-0781.2000.d01-4.x. [DOI] [PubMed] [Google Scholar]
- Thompson S, Jolley D, Marks R. Reduction of solar keratoses by regular sunscreen use. N Engl J Med. 1993;329:1147–1151. doi: 10.1056/NEJM199310143291602. [DOI] [PubMed] [Google Scholar]
- US UV Index Websites. US UV Index forecasts and data for the US available at the following. 2008 http://uvb.nrel.colostate.edu/UVB/, http://www.srrb.noaa.gov, http://www.epa.gov/sunwise/uvindex.html#map, http://www.cpc.ncep.noaa.gov/products/stratosphere/uv_index/uv_current_map.shtml.
- Weinstock M. Assessment of sun sensitivity by questionnaire: Validity of items and formulation of a prediction rule. J Clin Epidemiol. 1992;45:547–552. doi: 10.1016/0895-4356(92)90104-u. [DOI] [PubMed] [Google Scholar]
- World Health Organization. WHO/EHG/95.17. Geneva: WHO; 1995. Protection against exposure to ultraviolet radiation; p. 33. [Google Scholar]
- World Health Organization. Global solar UV Index: A practical guide. Geneva: WHO; 2002. p. 28. [Google Scholar]


