Abstract
Characterizing the effects of alcohol and marijuana use on adolescent brain development is important for understanding potential alterations in neurodevelopment. Several cross sectional studies have identified group differences in white matter integrity after initiation of heavy alcohol and marijuana use, however none have explored white matter trajectories in adolescents pre- and post initiation of use, particularly for marijuana users. This study followed 16 adolescents with minimal alcohol and marijuana use at ages 16–18 over three years. At follow-up, teens were 19–22 years old; half of the participants initiated heavy alcohol use and half initiated heavy alcohol and marijuana use. Repeated-measures ANOVA revealed 20 clusters in association and projection fibers tracts (p < 0.01) in which a group by time interaction was found. Most consistently, white matter integrity (i.e., fractional anisotropy) decreased for those who initiated both heavy alcohol and marijuana use over the follow-up interval. No effect of time or change in white matter integrity was seen for those who initiated alcohol use only in the majority of clusters. In most regions, at the baseline time point, teens who would later initiate both alcohol and marijuana use demonstrated white matter integrity greater than or equal to teens that initiated alcohol use only. Findings suggest poorer tissue integrity associated with combined initiation of heavy alcohol and marijuana use in late adolescence. While pre-existing differences may also be related to likelihood of substance use, the present data suggest an effect on tissue integrity for these teens transitioning to combined alcohol and marijuana use in later adolescence.
Keywords: adolescence, alcohol, marijuana, white matter, diffusion tensor imaging, cognition, development, brain
1. Introduction
Alcohol and marijuana use are typically initiated during adolescence, with rates of lifetime use increasing significantly into young adulthood. Alcohol use increases from 30% to 70% between 8th and 12th grade, with 24% of high school seniors endorsing recent binge drinking (i.e., >5 drinks in a row in the last two weeks). Marijuana, the second most commonly used substance, shows similar increases with rates of use increasing from 15% to 45% during the same time period [1]. In fact, perceived risk of marijuana use has been declining, and the percent of high school seniors identifying as daily users (7%) has generally increased over the past two decades.
While alcohol and marijuana are the most commonly used substances among adolescents, their potential effects on the developing brain are not well understood. Elucidating the unique and interactive effects of these substances on brain development is crucial, as significant neural maturation in both gray and white matter occurs during adolescence. Specifically, the adolescent brain undergoes marked decreases in gray matter along with linear increases in white matter, purportedly associated with myelination and to some degree, regressive changes to axons and dendrites [2,3,4]. Progressive myelination during adolescence is likely associated with optimal cognitive processing and communication between brain regions [5], which in turn may result in better cognitive performance [6,7,8]. Any potential neurotoxic insults during this crucial maturation process could have long-lasting implications on cognitive development [9,10,11].
Longitudinal studies have found that initiation of alcohol use alone during adolescence is associated with poorer neuropsychological functioning over time, including worsening visuospatial functioning and attention [12,13,14] as well as deviations in brain response patterns when compared to non-using adolescent controls [15,16]. Widespread reductions in white matter integrity have also been found in adolescent binge drinkers when compared to non-drinking teenagers [17].
Adolescents who use marijuana typically engage in alcohol use [1]; therefore, it is not surprising that much of the marijuana-focused literature includes adolescents who use both marijuana and alcohol to some extent. Cross-sectional neuropsychological findings show that adolescent heavy marijuana users have worse psychomotor speed, complex attention, story memory, and planning and sequencing abilities, even after a month of abstinence, as well as deficits on tests of verbal and visual memory when compared to non-users [18,19,20]. Longitudinal examinations have found poorer verbal and working memory, which remitted with abstinence, but continued attention deficits [21]. Initiation of marijuana use during adolescence may have long-lasting neurocognitive consequences [22], particularly in the areas of sustained attention, executive functioning [23], impulse control [24], and verbal memory [19].
Structural and functional imaging has helped better elucidate the potential neurobiological underpinnings of these cognitive deficits. The only existing longitudinal imaging study reporting pre-and post marijuana use data found that smaller orbitofrontal volumes at age 12 predicted marijuana initiation by age 16 [25]. Smaller medial orbital frontal cortex morphometry has also been identified in adolescent marijuana users ages 16–19, and linked with younger age of initiation [26]. Cross-sectional structural MRI studies have found thinner cortices in prefrontal and insular regions and thicker cortices in posterior regions [27] in marijuana using adolescents compared to healthy controls; however it is unclear if differences existed prior to marijuana use. Several functional imaging studies have shown aberrations in brain response patterns and cerebral blood flow in marijuana and alcohol using adolescents [28,29,30,31,32,33]. There is some suggestion that these differences remit with abstinence [28,29], however findings are mixed [30,34].
Diffusion tensor imaging (DTI) studies have been fairly consistent in regards to white matter integrity in comorbid marijuana and alcohol using adolescents, with most cross-sectional research showing poorer white matter integrity (e.g., decreased fractional anisotropy) in alcohol and marijuana users compared to controls [35,36], and expected negative associations with neurocognitive performance [36]. Research has also shown some subtle differences between adolescent alcohol and combined alcohol and marijuana users, despite overall poorer white matter integrity in these two groups of teens compared to non-users after early initiation and repeated regular use [36,37,38,39]; such findings highlight the deleterious effects of alcohol on white matter tissue integrity independent from marijuana. Recently, data from our laboratory found that poorer white matter integrity predicted increased future substance use and aggressive/delinquent behaviors, which suggests that some of these imaging biomarkers may have clinical utility in predicting future outcomes [37].
In terms of clarifying if white matter abnormalities are related to dose-dependent effects of alcohol and/or marijuana, compared to pre-existing differences driving these behaviors, there are still few investigations that have been able to help address this question. Bava and colleagues (2012) found that the cumulative use of alcohol predicted future white matter health, independent of white matter health pre-initiation, providing some supporting evidence of the detrimental effects of alcohol regardless of potential pre-exiting differences [38].
Although cortical thickness differences have been noted prior to initiation of cannabis use [25], few, if any, studies have examined pre-existing white matter integrity in adolescent marijuana users and changes with increased use. This study examined the white matter and neurocognitive trajectories of adolescents that increased alcohol use compared to those that increased alcohol use and initiated marijuana use. We hypothesized that there would be no differences in white matter architecture or neurocognitive performance between teens prior to initiation (ages 16–18); however teens that later transitioned to heavy alcohol and marijuana use would show poorer cognition and white matter health than those using alcohol only by young adulthood (ages 19–22).
2. Results and Discussion
2.1. Demographics
Groups did not differ on age, gender, family history, or socioeconomic status at baseline (p > 0.05). Groups differed on externalizing and internalizing symptoms at baseline, and externalizing symptoms and state anxiety symptoms at 3-year follow-up (p < 0.05). Although not significant (p > 0.05), marijuana initiators (MJ) reported more other drug use episodes compared to alcohol initiators (ALC) at 3-year follow-up (see Table 1 and Figure 1).
Table 1.
Demographic characteristics at 3-year follow-up unless otherwise noted.
| Alcohol initiators (ALC) (n = 8) Mean (SD) | Marijuana initiators (MJ) (n = 8) Mean (SD) | |
|---|---|---|
| 21.2 (19.9–22.1) | 20.6 (19.7–22.7) | |
| Age (SD; range) at baseline | 18.2 (0.7; 16.9–18.8) | 17.5 (0.8; 16.6–19.0) |
| % Caucasian | 75% | 63% |
| GPA at 3-year follow-up | 3.3 (0.6) | 3.1 (0.3) |
| Household Income at 3-year follow-up | 105.9K (57.3) | 163.3K (124.7) |
| Family history alcohol use disorder | 38% | 50% |
| Family history substance use disorder | 25% | 62% |
| Alcohol, lifetime use days at baseline (SD: range) | 26.3 (20.5; 3–60) | 37.1 (33.2; 0–85) |
| Alcohol, days use over follow-up (SD; range) | 205.9 (74.7; 131–312) | 295.0 (197.0; 100–625) |
| Binge Drinking Episodes over follow-up | 88.1 (71.2) | 156.3 (157.4) |
| Marijuana, lifetime use days at baseline (SD; range) | 1.0 (2.1; 0–6) | 3.6 (3.5; 0–9) |
| Marijuana, days use over follow-up (SD; range) * | 3.0 (3.7; 0–10) | 369.1 (168.3; 33–540) |
| Other drug use, lifetime use at baseline (SD; range) | 1.0 (0.7; 0.0–2.0) | 1.9 (4.5; 0.0–13.0) |
| Other drug use, days use over follow-up (SD; range) | 1.0 (0.3; 0.0–2.0) | 20.0 (33.1; 0.0–99.0) † |
| Beck Depression Inventory at baseline | 1.0 (1.0) | 4.6 (3.7) |
| Beck Depression Inventory at 3-year follow-up | 1.0 (1.6) | 5.5 (7.5) |
| State Trait Anxiety Inventory at baseline | 24.3 (2.6) | 29.1 (13.2) |
| State Trait Anxiety Inventory at 3-year follow-up * | 21.3 (2.4) | 29.8 (8.1) |
| Vocabulary T-score at baseline | 62.4 (9.0) | 57.5 (8.6) |
| CBCL Externalizing T-score at baseline * | 38.3 (7.7) | 52.1 (9.8) |
| ASR Externalizing T-score at 3-year follow-up * | 41.3 (12.8) | 59.4 (10.7) |
| CBCL Internalizing T-score at baseline * | 41.0 (8.3) | 50.4 (8.1) |
| ASR Internalizing T-score at 3-year follow-up | 38.5 (11.3) | 49.0 (15.5) |
* p < 0.05; † One sub with ninety-nine episodes, otherwise range (0–27).
Figure 1.
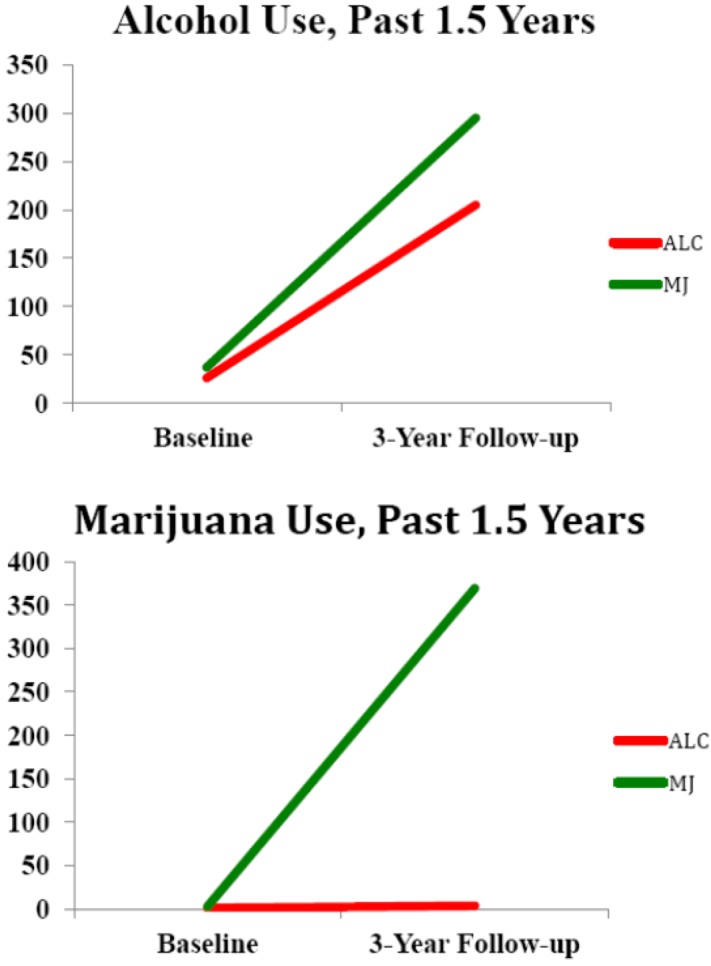
Participant alcohol and marijuana use at baseline and 3-year follow up (n = 16) for substance initiators (average marijuana use episodes at baseline, ALC = 1.0; MJ = 3.6 and follow-up, ALC = 3.0; MJ = 369.1)
2.2. White Matter Integrity over Time
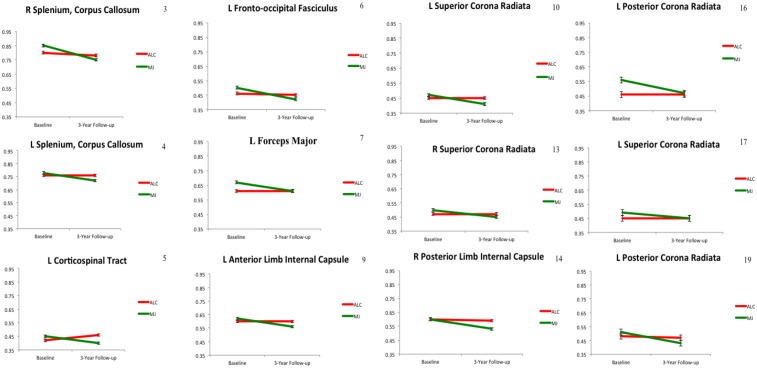
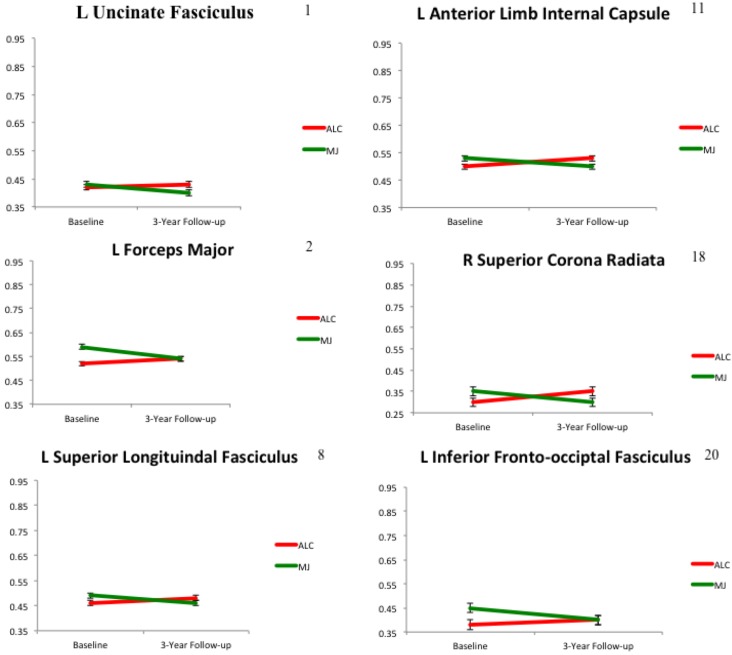
Repeated measures ANOVA revealed 20 clusters in which a significant group by time interaction effect was found in association, projection, and interhemispheric fiber tracts, F(1,14) = 16.7–67.4, p < 0.01. In 12 clusters, we saw no effect of time for ALC, but FA decreases from baseline to 3-year follow-up for MJ (see Figure 2 for regions). In 6 clusters, we saw FA increasing for ALC and decreasing for MJ (see Figure 3 for regions). In one cluster we observed increasing FA in ALC with no effect of time for MJ (left forceps minor), and in one cluster we observed FA decreasing for both ALC and MJ, with MJ decreasing at a steeper rate (right splenium corpus callosum).
Figure 2.
Group by time interactions for WM integrity showing decreasing FA in MJ and no effect of time in ALC (n = 16, p < 0.01); numbers corresponds to cluster order.
Figure 3.
Group by time interactions for WM integrity showing increasing FA in ALC and decreasing FA in MJ (n = 16, p < 0.01); numbers correspond to cluster order.
Analysis were re-examined controlling for internalizing, externalizing, binge drinking episodes, and other drug use episodes, and all findings remained significant (p < 0.01). Binge drinking episodes were not found to be a unique predictor of change in FA from baseline to follow-up in the larger sample (p > 0.05).
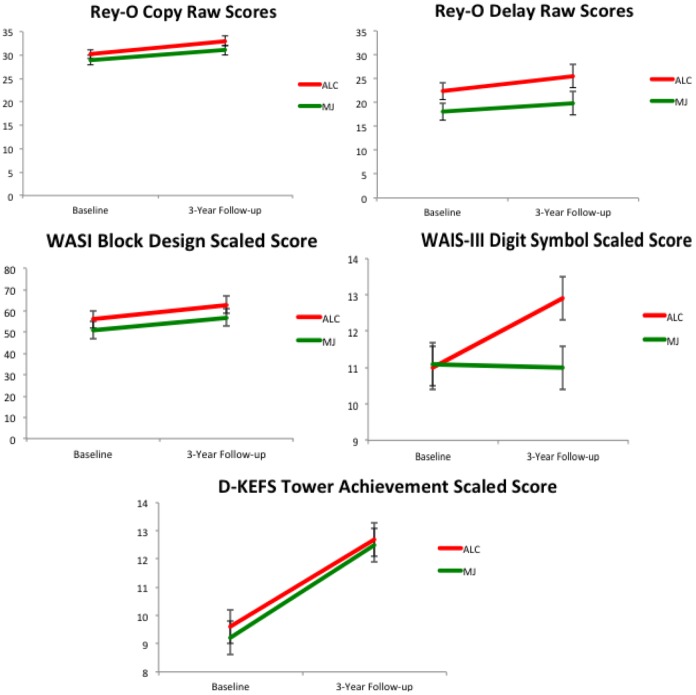
2.3. Neurocognitive Functioning over Time
Time and group by time interaction effects were observed on five neurocognitive tests. A main effect of time was found on the Rey-O Copy, F(1,14) = 11.9, p < 0.01, Rey-O Delay F(1.14) = 5.5, p = 0.03, WASI Block Design subtest scaled score F(1,14) = 18.2, p < 0.01, and DKEFS Tower Test total achievement scaled score F(1,14) = 17.0, p < 0.01 (better performance over time). A group by time interaction, F(1,14) = 8.1, p = 0.01, was found on the WAIS-III Digit Symbol subtest scaled score, as increasing performance over time was observed in ALC; however, no change was observed in MJ (Figure 4).
Figure 4.
Main effects of time (Rey, Block Design, Tower) and group by time interactions (Digit Symbol) for neuropsychological performance over three years (n = 16), norm-based scaled scores were corrected for age.
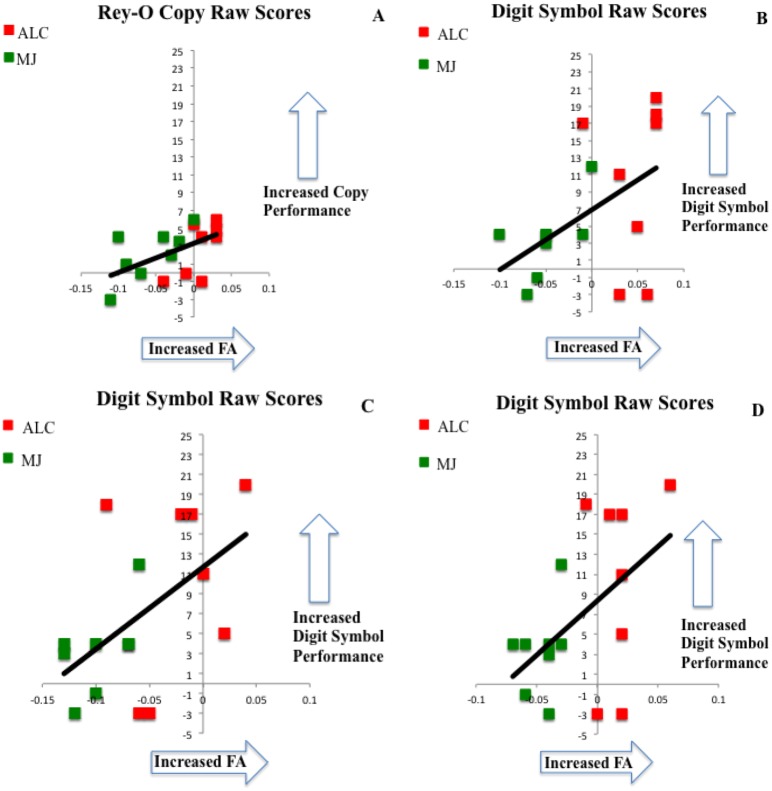
Neurocognitive Correlates with White Matter
Bivariate correlations exploring change in white matter integrity (FA) between 3-year follow-up and baseline and change in neuropsychological performance between 3-year follow-up and baseline were evaluated. A positive relationship was found between increased FA in the right superior corona radiata (r = 0.52, p = 0.03) and improved performance on the Rey-O Figure Copy. Increased FA in the right superior corona radiata (r = 0.50, p = 0.04), right splenium of the corpus callosum (r = 0.55, p = 0.03), and left forceps major (r = 0.52, p = 0.04) were also found to be related to improved performance on the Digit Symbol subtest. Relationships were not moderated by group status (see Figure 5). No significant correlations were found between substance use severity at follow-up and neuropsychological performance.
Figure 5.
Bivariate relationships between change in FA and change in neuropsychological performance (baseline subtracted from 3-year follow-up for both FA and neuropsychological measures); (A) FA in right superior corona radiata, (B) FA in right superior corona radiata, (C) FA in the right splenium of the corpus callosum, (D) FA in left forceps major.
2.4. Key Findings and Limitations
The aim of this preliminary study was to look at pre- and post white matter differences in teens after initiation of alcohol or alcohol and marijuana use in later adolescence (ages 16–22). We suspected teens that initiated alcohol and marijuana use would show decreasing FA values over time, as compared to those who only initiated alcohol use. In the vast majority of clusters, we found decreasing FA in alcohol and marijuana initiators and no effect of time in alcohol only initiators. A second group of clusters revealed increasing FA in alcohol only initiators (as would be expected in adolescent brain development) and decreasing FA in alcohol and marijuana initiators. Overall, we found that teens that initiated both heavy alcohol use and marijuana use demonstrated evidence of declining white matter integrity in association, projection, and corpus callosum fiber tracts, areas showing continued development throughout young adulthood [40]. We saw the inverse relationship for teens that initiated alcohol use only in late adolescence/early adulthood, as there was evidence for ongoing improvement in white matter integrity or limited change over time. Notably, in several clusters, marijuana initiators had average FA values equal to or significantly greater than alcohol only initiators, supporting evidence for marijuana-related toxicity, as opposed to pre-existing morphological tissue differences driving these relationships. Further, we saw evidence of improved white matter integrity (i.e., increased FA) linked to enhanced neurocognitive performance, along with improvement in neurocognitive performance over time in both groups of teens. It is possible that the bivariate relationships between change scores is largely driven by the improved performance on Digit Symbol over time in the ALC group; however the associations were not found to depend on group status.
While previous investigations in our laboratory have identified poorer white matter integrity in adolescent alcohol users compared to controls [17,36], and in some cases compared to those with marijuana use histories [40], this study is unique in that we identified a subset of teens at an initial time point with minimal use histories and evaluated them 3-years later, after initiation of either heavy alcohol use or heavy alcohol and marijuana use; previous work in our laboratory has predominately looked at between-group differences after initiation, as most teens enter the study and remain within their substance use patterns. In a recent study under review, we have observed poorer tract integrity in those adolescents with three or more years of regular substance use and younger age at initiation, including both alcohol and combined alcohol and marijuana use.
Elucidating pre-existing differences and changes associated with alcohol and marijuana use has been difficult. While pre-existing differences (for example, personality factors, or non-white matter related brain discrepancies) may still be driving the reported relationships in this investigation, there is strong support for a deleterious effect of combined alcohol and marijuana use on white matter health in those teens that transitioned to heavy use after their baseline assessment. Furthermore, the timing at which the teens initiated their heavier substance use differs from our previous white matter investigations. For example, in the vast majority of our investigations [17,35,40], teens were recruited into the study having already initiated alcohol and/or marijuana (prior to age 17), however in this sample, teens initiated heavier use around age 18 or older (on average), which is likely contributing to some discrepancies in findings (e.g., more subtle alcohol effects in the present investigation may be related to initiation of alcohol at an older age).
Few prospective studies have looked at pre-existing differences or subsequent brain changes in marijuana users prior to or after initiation of use. Cheetham and colleagues (2012) suggest evidence of pre-existing macrostructural brain differences, in that smaller orbitofrontal cortex volume predicted initiation of marijuana use by age 16. In our lab we have seen poorer white matter integrity predict increased substance use over an 18-month follow-up interval [37]. It is possible that neural circuits underlying particular brain regions important for cognitive control and reward may lead to vulnerabilities, which subsequently lead to marijuana use [25,37]. A recent investigation suggests a decline in cognitive functioning with persistent cannabis use. This longitudinal study found declines from premorbid functioning (assessed at age 13) after initiation of persistent cannabis use (age 38), on WAIS-IV IQ performance, and adolescent-onset users showed greater decline [22]. Studies such as these, taken together with the present findings, underscore two important points. First, it is likely that there are pre-existing neural vulnerabilities to initiate substance use and continue consumption of marijuana in some teens. Second, despite these potential existing differences, we are also likely to observe a negative effect of marijuana and alcohol use on brain tissue development whether pre-existing differences are present in the individual and/or sample. Changes in tissue development are likely related to cognitive alterations in cognitive functioning, even if changes are subtle.
While there are limited prospective white matter studies in adolescent marijuana users prior to initiation, cross sectional studies outside of our laboratory have also largely shown differences in adolescent marijuana users compared to non-using controls teens, despite some limited evidence to the contrary [41]. In 2009, Ashtari and colleagues [42] observed poor tract integrity in adolescent marijuana users. Similarly, in 2010, Yucel and colleagues [43] also found poorer white matter integrity in marijuana users when compared to controls. Gray matter alterations have been observed in several cross sectional investigations as well. For example, we have seen some discrepancies in prefrontal cortex, amygdala, and cerebellum volume in adolescent cannabis users compared to controls in our studies [44,45,46]. Other laboratories report dose-dependent relationships with temporal lobe structures such as hippocampus and amygdala [47] and alterations in cortical thickness [27] in frontal and parietal regions. Alterations in microstructural tissue integrity and macrostructural volume suggest a neurotoxic effect of marijuana on adolescent neurodevelopmental trajectories. Cannabinoid receptors are believed to modulate neurotransmission and may influence genetic expression of neurodevelopment [48], which may underlie many of the neurocognitive and structural neuroimaging differences observed in human subjects research with adolescent marijuana users. Preclinical evidence suggests cognitive/behavioral and social changes after exposure to Δ9-tetrahydrocannbinol (THC), as well as other cannabinoid agonists in adolescent rats [49,50].
While the strengths of this investigation include the prospective design and limited lifetime substance use episodes besides alcohol and marijuana, there are several limitations that must be noted. The sample size is small and multiple comparison corrections were less stringent and therefore replication of this preliminary work is important. Further, while alcohol use did not statistically differ between the groups (e.g., lifetime use, binge drinking) or predict change in white matter integrity, the marijuana users do report more binge drinking episodes and it is possible frequency and severity of alcohol use (vs. marijuana-related toxicity) contribute to the between group differences reported in this study. Future work should also focus on identifying and following a representative group of adolescents ages 19–22 with minimal alcohol and marijuana use to better disentangle the effects of these substances; however identifying and recruiting adolescents ages 19–22 who do not transition to some degree of heavy episodic drinking is challenging given the prevalence of alcohol use during this developmental window. Of course, self-report measures (e.g., lifetime alcohol use, marijuana use) can be limited and may impact statistical estimates.
3. Experimental Section
3.1. Participants
Participants in this study were adolescents ages 16–18 who were originally recruited as controls in an ongoing longitudinal study of adolescent marijuana and alcohol users (R01 DA021182), but who initiated heavy alcohol and/or marijuana use over the follow-up period (3 years post-baseline). At baseline, all participants (n = 16) had minimal substance use (see Table 1 and Figure 1). At the 3-year follow-up they were classified into two groups, those who reported very limited marijuana use (≤10 use episodes each visit), minimal alcohol use at baseline, and significantly increased alcohol use at 3-year follow-up (ALC, n = 8), and those who reported minimal marijuana use at baseline, minimal alcohol use at baseline, and significantly increased alcohol and marijuana use at 3-year follow-up (MJ, n = 8).
Adolescents were recruited from local schools. A parent or guardian was required to provide consent to participate in the study at baseline, and adolescents were required to provide assent in accordance with the University of California, San Diego Research Protections Program procedures. Exclusionary criteria were: history of a lifetime DSM-IV Axis I disorder (other than cannabis or alcohol abuse or dependence), history of learning disability, history of neurological disorder or head trauma with loss of consciousness >2 min, history of a serious physical health problem, complicated or premature birth; uncorrectable sensory impairments; left handedness; MRI contraindications, and use of psychoactive medications at project intake. Weekly toxicology screening was performed for four weeks prior to neuropsychological testing and neuroimaging scan session at both time points to confirm abstinence from marijuana prior to visit.
3.2. Procedures
At the baseline and 3-year follow-up, teens received a detailed substance use and mental health interview, diffusion tensor imaging session, and a comprehensive neuropsychological evaluation. Parents were also administered detail interviews to corroborate both demographic, psychosocial functioning, and substance use behaviors.
3.2.1. Substance Use and Mental Health Assessment
Substance use was assessed using the Customary Drinking and Drug Use Record (CDDR) [51]. This measure provided characterization of lifetime (baseline) and past 1.5-year use of alcohol, marijuana, nicotine, and eight other classes of illicit drugs at each appointment; DSM-IV abuse and dependence criteria were also collected. The Child Behavior Checklist (baseline) and corresponding Adult Self Report (3-year follow-up) was used to identify externalizing and internalizing symptoms experienced in the 6-months prior to appointment [52]. The Beck Depression Inventory and State Trait Anxiety Inventory [53,54] were used to assess depressive symptoms and state anxiety. Family history of substance use and psychiatry disorders was assessed with the Family History Assessment Module [55].
3.2.2. Neuropsychological Testing
Performance on approximately twenty standardized neuropsychological tests examining the domains of complex attention, processing speed, verbal memory, visuospatial functioning, and executive functioning were examined pre- and post alcohol and marijuana initiation. Measures include: (1) complex attention: California Verbal Learning Test-II Trial 1 and Trial 1–5 Total Recall (CVLT-II) [56], Wechsler Adult Intelligence Scale-Third Edition (WAIS-III) [57], Digit Symbol, Arithmetic, and Digit Span Backward subtests; Paced Auditory Serial Addition Test (PASAT) [58]; (2) processing speed: Delis-Kaplan Executive Function System (D-KEFS) Trail Making Test Number Sequencing, Letter Sequencing, and Motor Speed subtests [59]; (3) verbal memory: Wechsler Memory Scale-Third Edition (WMS-III) [60], Logical Memory I, II, and Recognition; CVLT-II Short and Long Delay Free Recall, CVLT-II Recognition [56]; (4) visuospatial functioning: Rey-Osterrieth Complex Figure Copy and Delay Accuracy (Rey-O) [61], Wechsler Abbreviated Scale of Intelligence Block Design subtest (WASI) [62]; and (5) executive functioning: D-KEFS Trial Making Test Number-Letter Switching, Tower Test Achievement, and Verbal Letter Fluency subtests [59].
3.2.3. Diffusion Tensor Imaging Acquisition and Processing
DTI scans at baseline and 3-year follow-up were acquired at the University of California, Center for Functional MRI (CFMRI) on a General Electric 3.0T magnet using an 8-channel gradient head coil. Diffusion was encoded through a single-shot dual spin echo excitation along 15 diffusion directions with b = 2000 s/mm2 and 4 averages in addition to the normalization image with no diffusion encoding (b = 0). Image parameters for the DTI sequence were: TE = 93.4 ms, TR = 12,400 ms, FOV = 24 cm, 36 contiguous slices, slice thickness = 3.0 mm, and image matrix = 128 × 128. Two field maps (TE/TR = 3.8/1000 ms) were collected and applied to correct for signal loss and inhomogenities in the magnetic field [63].
Image processing was conducted using software from the Oxford Centre for Functional Magnetic Resonance Imaging of the Brain software library (FSL) [64]. Pre-alignment processing steps included a six-degree of freedom affine registration for head motion and eddy current distortion (FLIRT-FMRIB’s Linear Registration Tool) [65] and correction for field distortions using PRELUDE (Phase Region Expanding Labeler for Unwrapping Discrete Estimates) [66] and FUGUE (FMRIB’s Utility for Geometrically Unwarping EPIs) [67]. Pre-processed images were then subjected to tensor decomposition to derive fractional anisotropy (FA) estimates. FMRIB’s Diffusion Toolbox [68] was used to calculate diffusion estimates for each subject. Tract-based spatial statistics (TBSS) identified white matter tracts common to all participants at both baseline and 3-year follow-up (for further description see [35,36,40]). Individual FA maps were registered to a standard template in MNI-152 space and averaged across participants to create a mean FA image. A white matter skeleton was then derived representing centers of all tracts common to all participants. To minimize partial-volume effects, values were thresholded at FA > 0.2. FA data from each subject was projected onto the derived skeleton and resulting data formed the basis of voxelwise cross-subject statistical comparisons [69].
3.3. Data Analyses
3.3.1. Demographic Comparisons.
One-way analysis of variance (ANOVA) and Chi-square tests examined between group differences on several demographic characteristics (e.g., age, ethnicity, mental health functioning) at baseline and 3-year follow-up.
3.3.2. DTI Statistical Analyses.
Whole brain repeated-measures analysis of variance were carried out (Analysis of Functional NeuroImages (AFNI, 3dANOVA3) [70] to identify between-group and within-subject differences across all participants at baseline and 3-year follow-up. Main effects of time, group, and their interaction were specified; it was determined a priori that if the interaction was significant, only clusters showing significant interaction effects would be examined in follow-up analyses. Multiple comparisons were corrected with voxel probability and cluster size thresholding using Monte Carlo simulations. Only clusters ≥9 µL (9 contiguous 1 × 1 × 1 mm voxels) with an individual voxel effect of α < 0.01 were interpreted, yielding a brain-wise α < 0.05 of finding such a cluster under the null hypothesis.
3.3.3. Neuropsychological Performance, White Matter Correlates, and Substance Use Severity
Repeated-measures ANOVA was used to examine neurocognitive trajectories at baseline and 3-year follow-up for each cognitive measure listed above. Main effect of time, group, and their interaction was specified. Change scores (baseline subtracted from 3-year follow-up) were computed for all 20 DTI clusters found to be significant and all neuropsychological measures (raw scores). Bivariate correlations between DTI change scores and changes in neuropsychological performance were examined. Similarly, bivariate correlations were explored between substance use severity (e.g., marijuana, alcohol, and binge drinking episodes over past 1.5 years) reported at 3-year follow-up and neuropsychological performance at follow-up.
4. Conclusions
In conclusion, this prospective study found decreased white matter integrity for teens that initiated heavy alcohol and marijuana use three years after a baseline assessment. Limited findings were identified for those that initiated alcohol use only in late adolescence/early adulthood. The data suggests a deleterious effect of marijuana use on white matter health in the context of heavy alcohol use. While previous studies from our laboratory also find poorer white matter integrity in teens who report alcohol use during earlier adolescence (prior to age 17), this study finds a lesser impact of alcohol use on white matter tissue integrity for those that initiate alcohol use only at a later age (over 18 vs. prior to age 17). We also observed positive associations between increased white matter health and better neurocognitive functioning in the combined sample. Future follow-up investigations will focus on replication with larger sample sizes, and explore the role of gender (hormones) and genetics (family history).
Importantly, combining multimodal neuroimaging will help to examine the relationships between white matter integrity, gray matter volume, and cortical thickness in relation to adolescent substance use, prior to and after escalation of use. We hope to identify brain changes that are the result of increased substance use in order to appropriately develop cognitive interventions. Neuroimaging biomarkers for predicting youth at increased vulnerability for substance use disorders and other risk taking behaviors is critical for prevention of functional decline and future development of mental health disorders that typically arise during young adulthood.
Acknowledgements
This research was made possible by funding from the National Institute on Drug Abuse (R01 DA021182, PI Tapert; F32 DA032188, PI Jacobus) and the National Institute on Alcohol Abuse and Alcoholism (R01 AA013419, PI Tapert).
Conflict of Interest
The authors declare no conflict of interest.
References
- 1.Johnston L.D., O’Malley P.M., Bachman J.G., Schulenberg J.E. Monitoring the Future National Results on Adolescent Drug Use: Overview of Key Findings, 2012. Institute for Social Research, The University of Michigan; Ann Arbor, MI, USA: 2013. [Google Scholar]
- 2.Gogtay N., Giedd J.N., Lusk L., Hayashi K.M., Greenstein D., Vaituzis A.C., Nugent T.F., III, Herman D.H., Clasen L.S., Toga A.W., et al. Dynamic mapping of human cortical development during childhood through early adulthood. Proc. Natl. Acad. Sci. USA. 2004;101:8174–8179. doi: 10.1073/pnas.0402680101. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Giedd J.N., Blumenthal J., Jeffries N.O., Castellanos F.X., Liu H., Zijdenbos A., Paus T., Evans A.C., Rapoport J.L. Brain development during childhood and adolescence: A longitudinal MRI study. Nat. Neurosci. 1999;2:861–863. doi: 10.1038/13158. [DOI] [PubMed] [Google Scholar]
- 4.Stiles J., Jernigan T.L. The basics of brain development. Neuropsychol. Rev. 2010;20:327–348. doi: 10.1007/s11065-010-9148-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Giedd J.N. The teen brain: Insights from neuroimaging. J. Adolesc. Health. 2008;42:335–343. doi: 10.1016/j.jadohealth.2008.01.007. [DOI] [PubMed] [Google Scholar]
- 6.Fryer S.L., Frank L.R., Spadoni A.D., Theilmann R.J., Nagel B.J., Schweinsburg A.D., Tapert S.F. Microstructural integrity of the corpus callosum linked with neuropsychological performance in adolescents. Brain Cogn. 2008;67:225–233. doi: 10.1016/j.bandc.2008.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Nagy Z., Westerberg H., Klingberg T. Maturation of white matter is associated with the development of cognitive functions during childhood. J. Cogn. Neurosci. 2004;16:1227–1233. doi: 10.1162/0898929041920441. [DOI] [PubMed] [Google Scholar]
- 8.Mabbott D.J., Noseworthy M., Bouffet E., Laughlin S., Rockel C. White matter growth as a mechanism of cognitive development in children. Neuroimage. 2006;33:936–946. doi: 10.1016/j.neuroimage.2006.07.024. [DOI] [PubMed] [Google Scholar]
- 9.Jacobus J., Bava S., Cohen-Zion M., Mahmood O., Tapert S.F. Functional consequences of marijuana use in adolescents. Pharmacol. Biochem. Behav. 2009;92:559–565. doi: 10.1016/j.pbb.2009.04.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Schweinsburg A.D., Brown S.A., Tapert S.F. The influence of marijuana use on neurocognitive functioning in adolescents. Curr. Drug Abuse Rev. 2008;1:99–111. doi: 10.2174/1874473710801010099. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Squeglia L.M., Jacobus J., Tapert S.F. The influence of substance use on adolescent brain development. Clin. EEG Neurosci. 2009;40:31–38. doi: 10.1177/155005940904000110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Squeglia L.M., Spadoni A.D., Infante M.A., Myers M.G., Tapert S.F. Initiating moderate to heavy alcohol use predicts changes in neuropsychological functioning for adolescent girls and boys. Psychol. Addict. Behav. 2009;23:715–722. doi: 10.1037/a0016516. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Tapert S.F., Brown S.A. Neuropsychological correlates of adolescent substance abuse: Four-year outcomes. J. Int. Neuropsychol. Soc. 1999;5:481–493. doi: 10.1017/S1355617799566010. [DOI] [PubMed] [Google Scholar]
- 14.Tapert S.F., Granholm E., Leedy N.G., Brown S.A. Substance use and withdrawal: Neuropsychological functioning over 8 years in youth. J. Int. Neuropsychol. Soc. 2002;8:873–883. doi: 10.1017/s1355617702870011. [DOI] [PubMed] [Google Scholar]
- 15.Squeglia L.M., Pulido C., Wetherill R.R., Jacobus J., Brown G.G., Tapert S.F. Brain response to working memory over three years of adolescence: Influence of initiating heavy drinking. J. Stud. Alcohol Drugs. 2012;73:749–760. doi: 10.15288/jsad.2012.73.749. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Squeglia L.M., Schweinsburg A.D., Pulido C., Tapert S.F. Adolescent binge drinking linked to abnormal spatial working memory brain activation: Differential gender effects. Alcohol. Clin. Exp. Res. 2011;35:1831–1841. doi: 10.1111/j.1530-0277.2011.01527.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.McQueeny T., Schweinsburg B.C., Schweinsburg A.D., Jacobus J., Bava S., Frank L.R., Tapert S.F. Altered white matter integrity in adolescent binge drinkers. Alcohol. Clin. Exp. Res. 2009;33:1278–1285. doi: 10.1111/j.1530-0277.2009.00953.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Thoma R.J., Monnig M.A., Lysne P.A., Ruhl D.A., Pommy J.A., Bogenschutz M., Tonigan J.S., Yeo R.A. Adolescent substance abuse: The effects of alcohol and marijuana on neuropsychological performance. Alcohol. Clin. Exp. Res. 2011;35:39–46. doi: 10.1111/j.1530-0277.2010.01320.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Solowij N., Jones K.A., Rozman M.E., Davis S.M., Ciarrochi J., Heaven P.C., Lubman D.I., Yucel M. Verbal learning and memory in adolescent cannabis users, alcohol users and non-users. Psychopharmacology. 2011;216:131–144. doi: 10.1007/s00213-011-2203-x. [DOI] [PubMed] [Google Scholar]
- 20.Medina K.L., Hanson K.L., Schweinsburg A.D., Cohen-Zion M., Nagel B.J., Tapert S.F. Neuropsychological functioning in adolescent marijuana users: Subtle deficits detectable after a month of abstinence. J. Int. Neuropsychol. Soc. 2007;13:807–820. doi: 10.1017/S1355617707071032. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Hanson K.L., Winward J.L., Schweinsburg A.D., Medina K.L., Brown S.A., Tapert S.F. Longitudinal study of cognition among adolescent marijuana users over three weeks of abstinence. Addict. Behav. 2010;35:970–976. doi: 10.1016/j.addbeh.2010.06.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Meier M.H., Caspi A., Ambler A., Harrington H., Houts R., Keefe R.S., McDonald K., Ward A., Poulton R., Moffitt T.E. Persistent cannabis users show neuropsychological decline from childhood to midlife. Proc. Natl. Acad. Sci. USA. 2012 doi: 10.1073/pnas.1206820109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Fontes M.A., Bolla K.I., Cunha P.J., Almeida P.P., Jungerman F., Laranjeira R.R., Bressan R.A., Lacerda A.L. Cannabis use before age 15 and subsequent executive functioning. Br. J. Psychiatry. 2011;198:442–447. doi: 10.1192/bjp.bp.110.077479. [DOI] [PubMed] [Google Scholar]
- 24.Gruber S.A., Silveri M.M., Dahlgren M.K., Yurgelun-Todd D. Why so impulsive? White matter alterations are associated with impulsivity in chronic marijuana smokers. Exp. Clin. Psychopharmcol. 2011;19:231–242. doi: 10.1037/a0023034. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Cheetham A., Allen N.B., Whittle S., Simmons J.G., Yucel M., Lubman D.I. Orbitofrontal volumes in early adolescence predict initiation of cannabis use: A 4-year longitudinal and prospective study. Biol. Psychiatry. 2012;71:684–692. doi: 10.1016/j.biopsych.2011.10.029. [DOI] [PubMed] [Google Scholar]
- 26.Churchwell J.C., Lopez-Larson M., Yurgelun-Todd D.A. Altered frontal cortical volume and decision making in adolescent cannabis users. Front. Psychol. 2010;1:225. doi: 10.3389/fpsyg.2010.00225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lopez-Larson M.P., Bogorodzki P., Rogowska J., McGlade E., King J.B., Terry J., Yurgelun-Todd D. Altered prefrontal and insular cortical thickness in adolescent marijuana users. Behav. Brain Res. 2011;220:164–172. doi: 10.1016/j.bbr.2011.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Schweinsburg A.D., Schweinsburg B.C., Medina K.L., McQueeny T., Brown S.A., Tapert S.F. The influence of recency of use on fMRI response during spatial working memory in adolescent marijuana users. J. Psychoactive Drugs. 2010;42:401–412. doi: 10.1080/02791072.2010.10400703. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Jacobus J., Goldenberg D., Wierenga C.E., Tolentino N.J., Liu T.T., Tapert S.F. Altered cerebral blood flow and neurocognitive correlates in adolescent cannabis users. Psychopharmacology (Berl.) 2012;222:675–684. doi: 10.1007/s00213-012-2674-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Tapert S.F., Schweinsburg A.D., Drummond S.P., Paulus M.P., Brown S.A., Yang T.T., Frank L.R. Functional MRI of inhibitory processing in abstinent adolescent marijuana users. Psychopharmacology (Berl.) 2007;194:173–183. doi: 10.1007/s00213-007-0823-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Jager G., Block R.I., Luijten M., Ramsey N.F. Cannabis use and memory brain function in adolescent boys: A cross-sectional multicenter functional magnetic resonance imaging study. J. Am. Acad. Child Adolesc. Psychiatry. 2010;49:561–572. doi: 10.1016/j.jaac.2010.02.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Schweinsburg A.D., Nagel B.J., Schweinsburg B.C., Park A., Theilmann R.J., Tapert S.F. Abstinent adolescent marijuana users show altered fMRI response during spatial working memory. Psychiatry Res. 2008;163:40–51. doi: 10.1016/j.pscychresns.2007.04.018. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Schweinsburg A.D., Schweinsburg B.C., Cheung E.H., Brown G.G., Brown S.A., Tapert S.F. fMRI response to spatial working memory in adolescents with comorbid marijuana and alcohol use disorders. Drug Alcohol Depend. 2005;79:201–210. doi: 10.1016/j.drugalcdep.2005.01.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Padula C.B., Schweinsburg A.D., Tapert S.F. Spatial working memory performance and fMRI activation interaction in abstinent adolescent marijuana users. Psychol. Addict. Behav. 2007;21:478–487. doi: 10.1037/0893-164X.21.4.478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Bava S., Frank L.R., McQueeny T., Schweinsburg B.C., Schweinsburg A.D., Tapert S.F. Altered white matter microstructure in adolescent substance users. Psychiatry Res. 2009;173:228–237. doi: 10.1016/j.pscychresns.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Bava S., Jacobus J., Mahmood O., Yang T.T., Tapert S.F. Neurocognitive correlates of white matter quality in adolescent substance users. Brain Cogn. 2010;72:347–354. doi: 10.1016/j.bandc.2009.10.012. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Jacobus J., Thayer R.E., Trim R.S., Bava S., Frank L.R., Tapert S.F. White matter integrity, substance use, and risk taking in adolescence. Psychol. Addict. Behav. 2012 doi: 10.1037/a0028235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Bava S., Jacobus J., Thayer R., Tapert S.F. Longitudinal changes in white matter integrity among adolescent substance users. Alcohol. Clin. Exp. Res. 2013;37:E181–E189. doi: 10.1111/j.1530-0277.2012.01920.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Jacobus J., McQueeny T., Bava S., Schweinsburg B.C., Frank L.R., Yang T.T., Tapert S.F. White matter integrity in adolescents with histories of marijuana use and binge drinking. Neurotoxicol. Teratol. 2009;31:349–355. doi: 10.1016/j.ntt.2009.07.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Lebel C., Beaulieu C. Longitudinal development of human brain wiring continues from childhood into adulthood. J. Neurosci. 2011;31:10937–10947. doi: 10.1523/JNEUROSCI.5302-10.2011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Delisi L.E., Bertisch H.C., Szulc K.U., Majcher M., Brown K., Bappal A., Ardekani B.A. A preliminary DTI study showing no brain structural change associated with adolescent cannabis use. Harm Reduct. J. 2006;3:17. doi: 10.1186/1477-7517-3-17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Ashtari M., Cervellione K., Cottone J., Ardekani B.A., Sevy S., Kumra S. Diffusion abnormalities in adolescents and young adults with a history of heavy cannabis use. J. Psychiatr. Res. 2009;43:189–204. doi: 10.1016/j.jpsychires.2008.12.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Yucel M., Zalesky A., Takagi M.J., Bora E., Fornito A., Ditchfield M., Egan G.F., Pantelis C., Lubman D.I. White-matter abnormalities in adolescents with long-term inhalant and cannabis use: A diffusion magnetic resonance imaging study. J. Psychiatry Neurosci. 2010;35:409–412. doi: 10.1503/jpn.090177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Medina K.L., McQueeny T., Nagel B.J., Hanson K.L., Yang T.T., Tapert S.F. Prefrontal cortex morphometry in abstinent adolescent marijuana users: Subtle gender effects. Addict. Biol. 2009;14:457–468. doi: 10.1111/j.1369-1600.2009.00166.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.McQueeny T., Padula C.B., Price J., Medina K.L., Logan P., Tapert S.F. Gender effects on amygdala morphometry in adolescent marijuana users. Behav. Brain Res. 2011;224:128–134. doi: 10.1016/j.bbr.2011.05.031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Medina K.L., Nagel B.J., Tapert S.F. Abnormal cerebellar morphometry in abstinent adolescent marijuana users. Psychiatry Res. 2010;182:152–159. doi: 10.1016/j.pscychresns.2009.12.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Cousijn J., Wiers R.W., Ridderinkhof K.R., van den Brink W., Veltman D.J., Goudriaan A.E. Grey matter alterations associated with cannabis use: Results of a VBM study in heavy cannabis users and healthy controls. Neuroimage. 2012;59:3845–3851. doi: 10.1016/j.neuroimage.2011.09.046. [DOI] [PubMed] [Google Scholar]
- 48.Rubino T., Parolaro D. Long lasting consequences of cannabis exposure in adolescence. Mol. Cell. Endocrinol. 2008;286:S108–S113. doi: 10.1016/j.mce.2008.02.003. [DOI] [PubMed] [Google Scholar]
- 49.Abush H., Akirav I. Short- and long-term cognitive effects of chronic cannabinoids administration in late-adolescence rats. PloS One. 2012;7:e31731. doi: 10.1371/journal.pone.0031731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Schneider M., Schomig E., Leweke F.M. Acute and chronic cannabinoid treatment differentially affects recognition memory and social behavior in pubertal and adult rats. Addict. Biol. 2008;13:345–357. doi: 10.1111/j.1369-1600.2008.00117.x. [DOI] [PubMed] [Google Scholar]
- 51.Brown S.A., Myers M.G., Lippke L., Tapert S.F., Stewart D.G., Vik P.W. Psychometric evaluation of the Customary Drinking and Drug Use Record (CDDR): A measure of adolescent alcohol and drug involvement. J. Stud. Alcohol. 1998;59:427–438. doi: 10.15288/jsa.1998.59.427. [DOI] [PubMed] [Google Scholar]
- 52.Achenbach T., Rescorla L. Manual for the Aseba School-Age Forms & Profiles. Research Center for Children, Youth, and Families, University of Vermont; Burlington, VT, USA: 2001. [Google Scholar]
- 53.Beck A. Beck Depression Inventory (BDI) Psychological Corporation; San Antonio, TX, USA: 1978. [Google Scholar]
- 54.Spielberger C., Gorsuch R., Lushene R. Manual for the State-Trait Anxiety Inventory. Consulting Psychologists Press; Palo Alto, CA, USA: 1970. [Google Scholar]
- 55.Rice J.P., Reich T., Bucholz K.K., Neuman R.J., Fishman R., Rochberg N., Hesselbrock V.M., Nurnberger J.I., Jr., Schuckit M.A., Begleiter H. Comparison of direct interview and family history diagnoses of alcohol dependence. Alcohol. Clin. Exp. Res. 1995;19:1018–1023. doi: 10.1111/j.1530-0277.1995.tb00983.x. [DOI] [PubMed] [Google Scholar]
- 56.Delis D.C., Kramer J.H., Kaplan E., Ober B.A. California Verbal Learning Test. 2nd. The Psychological Corporation; San Antonio, TX, USA: 2001. [Google Scholar]
- 57.Wechsler D. Wais-III Manual. Psychological Corporation; New York, NY, USA: 1997. [Google Scholar]
- 58.Gronwall D.M.A. Paced auditory serial-addition task: A measure of recovery from concussion. Percept. Mot. Skills. 1974;44:367–373. doi: 10.2466/pms.1977.44.2.367. [DOI] [PubMed] [Google Scholar]
- 59.Delis D.C., Kaplan E. Delis-Kaplan Executive Functioning Scale Manual. Psychological Corporation; San Antonio, TX, USA: 2000. [Google Scholar]
- 60.Wechsler D. Manual for the Wechsler Memory Scale. 3rd. Psychological Corporation; New York, NY, USA: 1997. [Google Scholar]
- 61.Corwin J., Bylsma F.W. Translations of excerpts from Andre Rey’s “psychological examiniation of traumatic encephalopathy” and P.A. Osterrieth’s “the complex figure copy test”. Clin. Neuropsychol. 1993;7:3–21. [Google Scholar]
- 62.Wechsler D. Manual for the Wechsler Abbreviated Scale of Intelligence. Psychological Corporation; San Antonio, TX, USA: 1999. [Google Scholar]
- 63.Andersson J.L., Kare S. A model-based method for retrospective correction of geometric distortions in diffusoin weighted EPI. Neuroimage. 2002;16:177–199. doi: 10.1006/nimg.2001.1039. [DOI] [PubMed] [Google Scholar]
- 64.Smith S.M., Jenkinson M., Woolrich M.W., Beckmann C.F., Behrens T.E., Johansen-Berg H., Bannister P.R., de Luca M., Drobnjak I., Flitney D.E., et al. Advances in functional and structural MR image analysis and implementation as FSL. Neuroimage. 2004;23:S208–S219. doi: 10.1016/j.neuroimage.2004.07.051. [DOI] [PubMed] [Google Scholar]
- 65.Jenkinson M., Bannister P., Brady M., Smith S. Improved optimization for the robust and accurate linear registration and motion correction of brain images. Neuroimage. 2002;17:825–841. doi: 10.1006/nimg.2002.1132. [DOI] [PubMed] [Google Scholar]
- 66.Jenkinson M. Fast, automated, n-dimensional phase-unwrapping algorithm. Magn. Reson. Med. 2003;49:193–197. doi: 10.1002/mrm.10354. [DOI] [PubMed] [Google Scholar]
- 67.Jenkinson M., Smith S. A global optimisation method for robust affine registration of brain images. Med. Image Anal. 2001;5:143–156. doi: 10.1016/S1361-8415(01)00036-6. [DOI] [PubMed] [Google Scholar]
- 68.Behrens T.E., Woolrich M.W., Jenkinson M., Johansen-Berg H., Nunes R.G., Clare S., Matthews P.M., Brady J.M., Smith S.M. Characterization and propagation of uncertainty in diffusion-weighted MR imaging. Magn. Reson. Med. 2003;50:1077–1088. doi: 10.1002/mrm.10609. [DOI] [PubMed] [Google Scholar]
- 69.Smith S.M., Jenkinson M., Johansen-Berg H., Rueckert D., Nichols T.E., Mackay C.E., Watkins K.E., Ciccarelli O., Cader M.Z., Matthews P.M., et al. Tract-based spatial statistics: Voxelwise analysis of multi-subject diffusion data. Neuroimage. 2006;31:1487–1505. doi: 10.1016/j.neuroimage.2006.02.024. [DOI] [PubMed] [Google Scholar]
- 70.Cox R.W. AFNI: Software for analysis and visualization of functional magnetic resonance neuroimages. Comput. Biomed. Res. 1996;29:162–173. doi: 10.1006/cbmr.1996.0014. [DOI] [PubMed] [Google Scholar]