Abstract
A history of traumatic and/or stressful experiences is prevalent among HIV-infected individuals and has been consistently associated with poorer health outcomes. However, little is known about incident stressful experiences and the factors that predict these experiences among HIV-infected individuals. Data from a longitudinal study of 611 HIV-infected individuals in the Southeastern US were used to examine the frequency and types of incident stress reported in a 27-month period and to determine predictors associated with 3 incident stress measures (all stressful events, severe stressful events, and traumatic events such as physical assault). Incident stressful experiences frequently occurred among study participants, as 91% reported at least one stressful experience (median= 3.5 experiences) and 10% of study participants reported traumatic stress in any given 9-month reporting period. Financial stressors were the most frequently reported by study participants. Greater emotional distress, substance use, and number of baseline stressful experiences were significantly associated with reporting a greater number of incident stressful experiences and any traumatic experiences. Study results indicate that efforts are needed to identify individuals at risk for traumatic events and/or substantial stressors and to address the factors, including mental health and substance abuse that contribute to these experiences.
Keywords: HIV, AIDS, Trauma, Stress, Mental Health, Substance Abuse
INTRODUCTION
Among individuals with HIV disease, a history of traumatic and stressful life experiences has been associated with negative outcomes including reduced antiretroviral medication adherence (Mugavero et al., 2006), virologic failure (Parienti et al., 2004; Pence et al., 2006), mortality and opportunistic infection (Leseman et al. 2007; Mugavero et al., 2007) as well as increased sexual and drug use behaviors that raise the risk for secondary HIV transmission (Hamburger et al., 2004; Kelly et al., 1993). Studies of traumatic and stressful experiences have consistently identified a high lifetime prevalence of these experiences among HIV-infected individuals (Allers and Benjack, 1991; Cohen et al., 2004; Kelly et al., 1993; Simoni and Ng, 2000; Vlahov et al., 1998; Wyatt, Myers & Williams, 2002; Whetten et al., 2006). For example, in the Coping with HIV/AIDS in the Southeast (CHASE) sample of HIV-infected patients in the Southeast, 30% of respondents reported childhood sexual abuse and 40% reported sexual and/or physical abuse before age 18 (Whetten et al, 2006). CHASE participants were approximately twice as likely as members of the general population to have experienced abuse (Briere and Elliot 2003). Similarly high rates of childhood abuse have also been reported in HIV-infected individuals in other parts of the U.S. (Cohen et al., 2004; Kelly et al., 1993; Simoni and Ng, 2000; Vlahov et al., 1998; Wyatt, Myers & Williams, 2002).
The burden of current or ongoing traumatic and stressful experiences has not been widely characterized among individuals with HIV/AIDS. However, studies that have investigated recent trauma among HIV-infected individuals have identified relatively high levels of these experiences. For example, the HIV/AIDS Cost and Service Utilization Study (HCSUS), a national study of HIV-infected individuals receiving medical care (1996–1998), asked research participants about physical abuse since HIV diagnosis and documented that 20.5% of women, 11.5% of men who reported having sex with men (MSM), and 7.5% of heterosexual men reported physical abuse by a partner since HIV diagnosis (Zierler et al., 2000). The only longitudinal study we identified in the literature that examined incident stressful experiences among individuals with HIV or at risk for HIV infection was the HIV Epidemiology Research Study (HERS) of women with or at risk for HIV. This study documented an incidence rate for violent events (defined as being physically attacked or raped) of 6.2 per 100 person years over a 5-year period (Gruskin et al., 2002). Higher CD4 count, younger age, being single/widowed/divorced, prior physical or sexual abuse, depression, having multiple sexual partners, and using illegal substances were associated with incidence of violent events. No studies were identified that examined a wide range of incident stressful and traumatic events, beyond physical and/or sexual abuse, in a representative HIV-infected population.
A more comprehensive understanding of the incident traumatic and stressful experiences among individuals with HIV and the factors that contribute prospectively to these experiences is a necessary step in devising strategies to address ongoing trauma and stress and reduce their associated negative consequences. This article describes the frequency and prospective predictors of a wide range of incident traumatic and stressful events experienced by participants of the CHASE study over a 27-month follow-up period.
METHODS
Sample and Procedure
Participants were recruited for The Coping with HIV/AIDS in the Southeast (CHASE) study from eight infectious diseases clinics in 5 Deep South states (AL, GA, LA, NC, SC). The CHASE sampling strategy was designed to provide a cohort reflective of patients in the Deep South receiving HIV care outside of the region’s three largest metropolitan statistical areas (MSAs) (Charlotte, NC; Atlanta, GA; and New Orleans, LA) (U.S. Census Bureau, 2005). Eligibility criteria included being HIV-infected, English-speaking, and passing the Short Portable Mental Status Questionnaire (SPMSQ) (Pfeiffer, 1975), which tests for major cognitive impairment. Using consecutive sampling, 789 HIV-infected individuals were approached to participate in the study from December 2001 through April 2002. Sixteen individuals (2.0%) were excluded based on the SPMSQ. Of the 773 eligible subjects invited to participate, 611 (79%) enrolled in the CHASE study (Pence et al, 2007). Eighty-eight percent of participants (n=539) were available for survey at one or more of the follow-up data points.
Patients completed detailed interviews at baseline and every 9 months thereafter for a total study duration of 27 months. Clinical information from patients’ medical records was recorded on standardized chart abstraction forms. Greater detail about study recruitment is provided elsewhere (Pence et al., 2007; Mugavero et al., 2006).
Measures
Incident Stressful Events, Severely Stressful Events, and Traumatic Events (Appendix 1)
A modified version of the Life Events Survey (LES) (Leserman et al., 2008; Sarason et al., 1978) was used to measure stressful events in the 9 months prior to the baseline interview and in the intervals between the follow-up interviews. The full LES was modified to include only events considered to be moderately to severely stressful based on previous studies with interviewer-based objectively rated stresses. In prior research this objective rating was shown to be consistently related to CD4+ T-lymphocyte and HIV disease progression (Leserman et al., 2002; Leserman et al., 2005). Moderately stressful experiences included 26 possible experiences such as relationship difficulties; death or serious illness of a friend or non-immediate family member; employment difficulties (e.g. loss of job); non-HIV-related serious illnesses or injuries; moderate financial difficulties (including being behind in bills and having bill collectors calling); safety fears; and transitions such as leaving parents’ home for the first time or moving several times (See Appendix A for a description of the stressful/traumatic experiences). Severely stressful experiences included 21 possible experiences including divorce/separation, death or illness of an immediate family member, hospitalization, major financial problems (e.g., foreclosure), more than a week in prison, and sexual and physical abuse. We also created a category of experiences considered as traumatic (a subset of the severely stressful events category) that included those experiences that would satisfy criterion A(1) of the definition of post-traumatic stress disorder (American Psychiatric Association, 1990) which were sexual and physical assault and death of a spouse/partner or child. For analysis purposes, we considered three global measures of stressful experiences: 1) the number of all stressful experiences (moderate and severe) 2) the number of severely stressful experiences and 3) whether a traumatic experience occurred (Mugavero et al., 2006). We calculated these measures for the 9 months before baseline and for each of the three 9 month follow-up intervals. The baseline interview also included an inventory of lifetime exposure to traumatic events, which was summarized as a count variable reflecting the number of types of such events, as described previously (Leserman et al. 2008; Sarason et al. 1978; Leserman et al., 2007).
Mental Illness and Substance Use
At each interview, participants completed the Brief Symptoms Inventory (BSI), an assessment of current (previous 7 days) psychological symptoms with items addressing 9 domains of mental status including depression and anxiety (Derogatis et al., 1983; Derogatis 1993). Substance use in the last 30 days was measured with the Addiction Severity Index (ASI). Alcohol severity and drug severity scores were calculated according to ASI documentation (McLellan et al., 1992). Post-traumatic stress disorder (PTSD) symptoms in the past 9 months were assessed with the PTSD Checklist, a 17-item instrument assessing DSM-IV PTSD symptom criteria (Blanchard et al., 1996). PTSD diagnoses were assigned using the scoring that follows DSM-IV symptom criteria.
Demographic, Clinical, and Coping Variables
Coping styles were assessed at baseline with 16 items from the Brief Cope (Carver 1997). Consistent with previous definitions (Mugavero 2006; Carver 1997) and an exploratory factor analysis, we formed a scale for maladaptive (denial, self blame, and behavioral disengagement) coping style ranging from 1–4, which had satisfactory internal reliability (Cronbach’s alpha = 0.72).
Demographic and social variables were recorded at the baseline interview. Health-related measures included the SF-36 Physical Health Composite Score to measure physical functioning (McHorney, Ware, Lu and Sherbourne, 1994;) at each wave, whether the participant consider him or herself permanently or temporarily disabled at baseline, and CD4+ T lymphocyte count at each interview wave, which was defined as the CD4 measure closest to the interview date within a window of 6 months prior to the interview. For participants with no CD4 count from the medical record in the 6 months prior to baseline (n=149, 24%), we used self-reported data on CD4 count from the participant surveys instead. For participants missing a CD4 count within the 6-month window at follow-up time points, we used the most recent post-baseline CD4 from the chart if available (n=140, 10% of follow-up time points) or self-reported CD4 count from the participant surveys (n=250, 18% of follow-up time points).
Statistical Analysis
To describe the incidence of each type of stressful event, we present the proportion of interviews (up to 4 per participant) at which each type of event was reported. The stressful incidents were grouped by stress category for ease of presentation and interpretation resulting in 11 stressful experiences categories (sexual assault, physical assault, health, death of family or close friend; financial stresses; relationship stress, employment stress, legal stress, safety-related stress, and life transition). For comparability with the report of stressful event incidence from the HERS study, we calculated the incidence rate of each type of stressful experiences by dividing the number of stressful experiences by person years of observation. For ease of interpretation, we also translated these rates into a three-year risk (the proportion of participants expected to experience each type of stressful experiences over three years).
To explore prospective predictors of incident stressful events, we present unadjusted and adjusted associations of baseline and time-varying (lagged by one wave) characteristics with our three outcome measures reported at 9, 18, and 27 months: all stressful events, severely stressful events, and traumatic events. To account for the dependency between repeated observations on the same individuals, we used mixed-effects Poisson regression (for number of stressful events and number of severely stressful events) and mixed-effects logistic regression (for any traumatic event), including individual-level random effects and specifying an exchangeable correlation matrix (Fitzmaurice et. al, 2004). Likelihood ratio tests indicated that clinic-level random effects made a negligible contribution to the fit of the models, so these terms were not included in final models. We considered predictors that were of interest a priori including demographic and social variables, health-related variables, and mental health-related variables, which included emotional distress, substance use, and maladaptive coping. For parsimony, we included only variables with bivariable associations with of a p-value < .20. Collinearity was tested by examining pairwise correlations between predictor variables. The correlations were all less than .45. To examine whether mental health may moderate the relationship of baseline stressful experiences with incident stressful experiences, we created an interaction term between baseline stress and the global BSI score. Based on likelihood ratio tests, this interaction term was included when modeling all stressful experiences and severely stressful experiences but not when modeling traumatic experiences.
RESULTS
Participant Characteristics (Table 1)
Table 1.
Baseline Characteristics of the CHASE Participants
| Overall | |
|---|---|
| N=611 | |
| Age, years (range 20–71) | 40.1 ± 8.7 |
| Female gender | 191 (31.3%) |
| Race/ethnicity | |
| Caucasian non-Latino | 189 (31.6%) |
| African American non-Latino | 383 (64.0%) |
| Other* | 26 (4.4%) |
| Education beyond high school | 278 (45.7%) |
| Health insurance | |
| Private | 116 (19.0%) |
| Public | 373 (61.3.%) |
| None | 120 (19.6%) |
| Disabled | 223 (36.5%) |
| CD4 <200 cells/mm3 | 117 (22.7%) |
| VL <400 copies/mL | 237 (46.1%) |
| Mental health indicators | |
| PTSD | 98 (16.0%) |
| Probable psychiatric disorder (BSI) | 329 (53.9%) |
| Substance use, past 9 months | |
| Drinking to intoxication weekly | 40 (6.9%) |
| Any non-marijuana drug use | 136 (22.3%) |
| Crack use | 67 (11.1%) |
| Opioid use | 5 (0.8%) |
| Polysubstance use | 119 (20.0%) |
Includes Latino (2.7%), Asian (0.5%), Native American (1.2%)
Other modes of transmission were reported by 25 (4.1%) participants and 65 (10.7%) had an unknown mode of transmission.
A majority of CHASE participants were African American (64%) and nearly one-third of participants were female (31%). Less than half (45.7%) reported any education past high school and over one-third (36.5%) were disabled. Mental illness was relatively common among participants, as 53.9% had scores on the BSI that indicated a probable mental disorder. Nearly one-quarter reported any drug use (non-marijuana) in the previous 9 months.
Incidence of Stressful Experiences (Table 2)
Table 2.
Frequency of stressful and traumatic experiences
| Experience | Percent of 9-month time intervals in which at least one event was reported* | Incidence rate (number of events per 100 person-years) | Percent of participants expected to experience at least one event during 3 years of follow-up** |
|---|---|---|---|
| All stressful events: | 395.8 | ||
| % reporting any stressful events | 91.3% | ---- | 100.0% |
| Severely stressful events: | 116.4 | ||
| % reporting any severely stressful events | 61.4% | ---- | 97.0% |
| Any traumatic event | 10.0% | 12.7 | 31.6% |
| Specific Categories of Stressful Events (%) | |||
| Sexual assault | 0.9% | 1.1 | 3.1% |
| Physical assault | 7.6% | 9.3 | 23.4% |
| Health: Major illness, injury, accident | 37.0% | 69.5 | 84.3% |
| Death of family member or close friend | 34.9% | 57.5 | 77.8% |
| Major illness of family/close friend | 30.0% | 55.0 | 74.2% |
| Financial | 60.2% | 78.6 | 87.8% |
| Relationship | 34.1% | 56.6 | 78.9% |
| Employment | 23.0% | 46.0 | 72.1% |
| Legal | 10.8% | 16.1 | 35.8% |
| Safety-related | 19.6% | 28.3 | 54.1% |
| Life transition | 15.6% | 23.5 | 45.4% |
1,998 9-month time intervals reported by 611 participants (maximum of four time intervals per participant: baseline interview and 9, 18, and 27-month follow-ups).
The incidence rate of each type of event (events/person-years of observation) was transformed into a predicted risk over three years of follow-up using the formula Risk = 1 − exp(−Rate × time period).
Incident stressful experiences were highly prevalent among study participants. In any given 9-month follow-up period, participants reported a median of 3 stressful experiences (interquartile range (IQR) 2-5) and 1 severely stressful experience (IQR 0-2). Ninety-one percent reported at least one stressful event, 61% reported at least one severely stressful event, and 10% reported at least one traumatic event in an average 9-month period. For the entire 27-month follow-up period, the incidence rate of any stressful experiences was 396 per hundred person years (meaning an average participant would be expected to experience nearly 4 events per year), and the incidence rate of severely stressful experiences was 116 per hundred person years. The incidence rate of traumatic experiences was 13 per hundred person years. When the cumulative incidence rates were translated into expected risks over three years of follow-up (for greater ease of interpretation) virtually all participants were expected to experience at least one stressful and one severely stressful event and 32% were expected to experience at least one traumatic event.
Incidence of Specific Types of Stressful Experiences (Table 2)
Financial stress was the most frequently reported stressful experience, with 60% of participants reporting this issue in any given 9-month interval. Of those reporting financial stressors, nearly one-third described such experiences during all three of the 9-month follow-up periods, indicating ongoing financial concerns. For the entire 27-month follow-up period, there was an incidence rate of any financial stressors of 79 per hundred person years
Reporting a major illness or injury that was non-HIV related was also relatively common, as 37% reported experiencing this in any given 9-month follow-up period. One-third of participants (35%) reported the death of a close relative or friend during any given 9-month period. Death of a close friend was reported the most frequently. Physical abuse was reported by 7.6% of participants in any given follow-up period. Sexual abuse was rare, affecting 1% of participants in any given follow-up period. For the entire follow-up period, there was an incidence rate of sexual assault at 1.1 per hundred person years. Being arrested for a serious crime was also relatively rare at less than 2% for any given 9-month follow-up period.
Bivariable Associations of Participant Characteristics with Stressful Experiences (Table 3)
Table 3.
Bivariable Associations of Participant Characteristics with Incident Stressful Experiences
| Characteristic | # of any type of stressors* | # of severely stressors* | Traumatic Experiences^ |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Age, decade | .87 (.82, .92) | .93 (.85, 1.00) | .60 (.42, .87) |
| Female gender | 1.16 (1.03, 1.30) | 1.21 (1.04, 1.41) | 1.24 (.65, 2.36) |
| Nonwhite | .97 (.86, 1.09) | 1.06 (.91, 1.24) | .67 (.36, 1.28) |
| Education less than high school | 1.14 (.99, 1.31) | 1.21 (1.01, 1.47) | 1.87 (.88, 3.95) |
| Sexual Orientation – identify as “heterosexual” | .94 (.84, 1.05) | .82 (.71, .96) | 1.02 (.55, 1.92) |
| Married/steady partner | .96 (.85, 1.08) | .93 (.80, 1.10) | .80 (.42, 1.53) |
| Health insurance | |||
| Private | .76 (.66, .88) | .46 (.38, .57) | .35 (.15, .81) |
| Public | 1.15 (1.03, 1.29) | 1.48 (1.27, 1.72) | 1.35 (.72, 2.53) |
| None | 1.06 (.92, 1.22) | 1.10 (.91, 1.33) | 1.62 (.78, 3.38) |
| Employed | .89 (.80, 1.00) | .64 (.55, .74) | .32 (.17, .61) |
| Disabled | 1.10 (.98, 1.23) | 1.33 (1.15, 1.55) | 2.65 (1.45, 4.87) |
| CD4 <200 cells/mm3 | 1.17 (1.03, 1.33) | 1.06 (.88, 1.29) | 1.81 (.81, 4.07) |
| VL <400 copies/mL | .89 (.79, 1.01) | .81 (.69, .95) | 1.06 (.56, 2.01) |
| SF-36 physical functioning score, per 10 units | .96 (.92, 1.00) | .82 (.77, .87) | .91 (.72, 1.15) |
| PTSD | 1.50 (1.30, 1.73) | 1.65 (1.37, 1.99) | 4.74 (2.25, 9.98) |
| BSI per 10 units | 1.21 (1.15, 1.26) | 1.36 (1.27, 1.45) | 2.39 (1.83, 3.10) |
| ASI alcohol score, per 10 units | 1.03 (.95, 1.12) | 1.04 (.94, 1.15) | 1.30 (.89, 1.91) |
| ASI Drug use score, per 10 units | 1.26 (1.13, 1.41) | 1.34 (1.17, 1.55) | 3.59 (2.08, 6.17) |
| Maladaptive coping | 1.34 (1.24, 1.47) | 1.38 (1.23, 1.54) | 2.44 (1.53, 3.87) |
| Baseline stressful experiences# | 1.21 (1.15, 1.13) | 1.31 (1.23, 1.39) | 6.48 (2.82, 14.9) |
Mixed-effects Poisson Regression
Mixed-effects Logistic Regression
Baseline stress for each category: baseline number of any stressors; baseline number of severe stressors, and any baseline trauma
Several demographic characteristics were associated with stressful experiences. Women reported a higher number of any stressful or severely stressful experiences than their male counterparts. Younger age was associated with a higher number of any stressful experiences and being more likely to experience an incident traumatic event. Race/ethnicity, age, sexual orientation, education, and being married/having a steady partner were not significantly associated with any of the categories of stressful experiences. Health status characteristics including disability, CD4 count, and viral load were also not associated with stressful experiences.
Substance use and mental health issues were associated with stressful experiences. Higher scores on the ASI drug use scale (indicating greater problematic use) and higher levels of emotional distress, as measured by the BSI global score, were associated with experiencing all three categories of stressful experiences.
Multivariable Associations of Participant Characteristics with Incident Stressful Experiences (Table 4)
Table 4.
Multivariable Analysis of the Associations of Participant Characteristics with Incident Stressful Experiences
| # of any type of stressors | # of severe stressors | Traumatic experiences | |
|---|---|---|---|
| OR (95% CI) | OR (95% CI) | OR (95% CI) | |
| Fixed characteristics | |||
| Age, per 10 years | .90 (.85, .96) | .92 (.84–1.00) | .53 (.35, .79) |
| Female gender | 1.04 (.93, 1.16) | 1.15 (.98–1.35) | 1.37 (.70–2.68) |
| Less than high school education | .98 (.85, 1.13) | 1.06 (.87–1.29) | 1.24 (.57, 2.72) |
| Nonwhite | 1.01 (.90, 1.13) | 1.09 (.93–1.29) | .79 (.41, 1.54) |
| Disabled | .96 (.83, 1.10) | 1.02 (.83, 1.26) | 3.15 (1.33, 7.46) |
| Unemployed not disabled | .98 (.84, 1.14) | 1.11 (.89, 1.39) | 2.03 (.81, 5.10) |
| Lifetime traumatic experiences | 1.01 (.99, 1.04) | 1.00 (.96, 1.03) | .94 (.82, 1.09) |
| ASI alcohol score, per 10 units | .96 (.89, 1.02) | .97 (.88, 1.06) | 1.06 (.76, 1.48) |
| ASI drug score, per 10 units | 1.11 (1.01, 1.23) | 1.19 (1.05, 1.35) | 1.93 (1.21, 3.07) |
| Private insurance | .86 (.74, 1.00) | .63 (.48–.81) | .59 (.20, 1.76) |
| No insurance | .89 (.77–1.04) | .91 (.74, 1.12) | 1.33 (.59, 2.96) |
| Maladaptive coping | 1.07 (.97, 1.17) | 1.01 (.88,1.15) | .93 (.54, 1.60) |
| Number of stressful events in 9 months before baseline* | 1.25 (1.14, 1.37) | 1.73 (1.23, 2.43) | 2.34 (1.00, 5.36) |
| PTSD diagnosis | .98 (.83, 1.14) | .1.01 (.81, 1.25) | 1.17 (.51, 2.72) |
| Time-varying characteristics | |||
| SF-36 physical health score, per 10 units | .99 (.95–1.04) | .91 (.85–.98) | 1.34(.99, 1.80) |
| CD4 < 200 cells/mm3 (within last 6 months) | 1.14 (1.00–1.29) | 1.10 (.90–1.34) | 1.82 (.76, 1.36) |
| BSI global mental health score, per 10 units | 1.23 (1.13–1.35) | 1.30 (1.16, 1.47) | 1.87 (1.31, 2.66) |
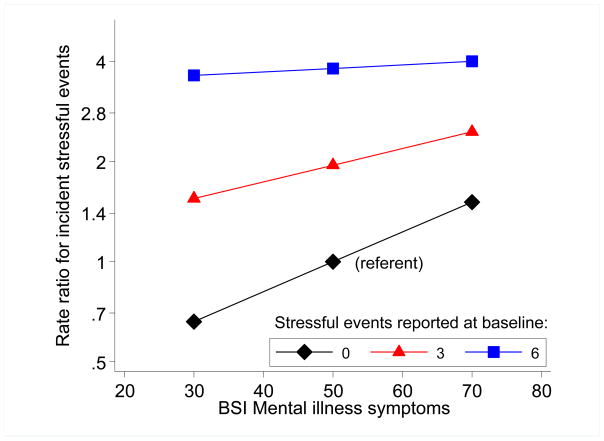
| Interaction term between baseline stressful experiences and global BSI | .97 (.96–.99) | .94 (.89–.99) | (not included)# |
Baseline stressful experiences for each category: baseline number of any stressful experiences; baseline number of severely stressful experiences, and any baseline traumatic experiences
Based on likelihood ratio tests, this interaction term was included when modeling all stressful experiences and severely stressful experiences but not when modeling traumatic experiences.
All Stressful Experiences
In multivariable analyses, greater emotional distress during the time period prior to the measure of incident stress was associated with reporting a higher number of any stressful experiences in the ensuing follow-up period (OR 1.23, 95% CI 1.13, 1.35). The following example illustrates the effects of emotional distress, An African-American male participant with median scores for CD4 count, physical functioning, drug use, previous trauma, and age, and the lowest level of emotional distress reported would be predicted to report 2 incident stressful events. In contrast, a participant with the same characteristics except for reporting the highest level of emotional distress would be predicted to report 4 stressful experiences in a 9-month period. We also observed interaction between global BSI score and baseline stressful experiences in predicting incident stressful experiences, indicating that the influence of emotional distress on subsequent stressful experiences was greater for those with lower numbers of baseline stressful experiences. Greater problematic drug use (OR 1.11, 95% CI 1.01, 1.23) was also associated with reporting more incident stressful experiences. In addition, not having private insurance, younger age, and greater number of stressful experiences reported at baseline were predictors of a higher number of incident stressful experiences.
Severely Stressful Experiences
Higher levels of emotional distress (OR 1.31, CI 1.16, 1.47) were associated with reporting a higher number of incident severely stressful events during the ensuing follow-up period. Further, a similar interaction was observed between global BSI and baseline severely stressful experiences in predicting incident severely stressful experiences. In addition, greater problematic drug use, poorer physical functioning, and greater number of severely stressful events reported at baseline were associated with incident severely stressful events.
Traumatic Experiences
Greater emotional distress was significantly associated with experiencing an incident traumatic event (OR 1.87, CI 1.31, 2.66) in the ensuing follow-up period. Problematic drug use, reporting trauma in the 9 months prior to baseline, younger age, and being disabled were also associated with being more likely to experience a traumatic event during the follow-up period.
DISCUSSION
Study results indicate that incident stressful experiences frequently occur among individuals living with HIV/AIDS. Nearly all participants reported at least one moderately or severely stressful experience during any given 9-month follow-up period and 61% reported at least one severely stressful experience during any given follow-up period. Study participants often experienced multiple stressors, as on average, participants experienced 3.5 moderate or severe stressors in each of the 9-month follow-up periods. Financial stressors, such as no money for basic needs or being behind in bills, were the most frequently reported stressful experiences. Of those reporting financial stress, nearly one-third reported financial stress during each of the reporting periods, indicating that they were experiencing ongoing financial concerns. Although 40% of CHASE participants reported a history of childhood physical and/or sexual abuse, incident physical and sexual assaults were relatively infrequent at 7.6% and 1% respectively in any given 9-month period.
The high levels of incident stress are concerning because they can negatively affect the quality of life of these individuals as well as potentially contributing to negative health outcomes. Incident stressful experiences have been associated with poorer medication adherence and increased HIV risk behavior independent of demographic and psychosocial factors (Mugavero et al., 2009; Pence et al., 2010, Leserman et al., 2008). Efforts to prevent or reduce incident stressful experiences are needed to attenuate their potential negative consequences.
Incident stress can be addressed directly by assuring that HIV case management and other relevant services are available to assist with common stressors such as financial difficulties and relationship problems. Incident stressful experiences can also be affected indirectly by addressing factors that contribute to their occurrence. Data analysis revealed several consistent predictors of the three categories of incident stress including mental health, substance use, and baseline levels of stressful experiences. These relationships were present even after controlling demographic and health characteristics. Mental illness and substance use have also been associated with other negative outcomes among people living with HIV/AIDS including being less likely to have antiretroviral medications prescribed, poorer medication adherence, and greater risk behavior (Sherbourne et al., 2000; Spire et al, 2000; Arnsten et al., 2000; Avants et al., 2000; Kelly et al., 1993; Turner et al., 2001; Fairfield et al., 1999). The results of this study regarding the association of mental health concerns and incident stress are consistent with those of the HERS study, which found a connection between mental health and incident trauma among women with or at risk for HIV disease (Gruskin et al., 2002).
Because the current study was longitudinal, it was clear that emotional distress and substance use predated the stressful and traumatic events reported by participants; however, the causal nature of these relationships may be complex. While individuals with mental health and substance use issues are at risk for future stressful events, the mental health and substance use problems of many of these individuals may be in part a result of previous trauma suggesting a potentially destructive cycle of stressful experiences and mental health and substance use problems. Intervening in this pattern by providing mental health and substance abuse treatment or interventions specifically targeting the psychological sequelae of past abuse for HIV-positive individuals may be particularly critical to improve outcomes for individuals with these complex issues. A number of interventions have shown promise in treating mental health and substance use issues among individuals with HIV/AIDS including group psychotherapy, cognitive behavior therapy, integrated mental health and substance use services, and treatments programs that combine several treatment modalities (Whetten et al., 2006; Sikkema et al., 2010; Basu et al., 2005; Scott-Sheldon et al., 2008; Himelhoch et al., 2007; Crepaz et al., 2008. Sikkema 2007)
Not surprisingly, stressful experiences reported in the 9 months prior to baseline strongly predicted future stress. Further, the interaction for global BSI score and baseline stressful experiences was associated with any stressful experiences and severely stressful experiences, indicating a moderating effect of baseline stressful experiences on the influence of emotional distress on incident stressful experiences. It may be that for those with higher levels of baseline stress, current mental health status has less of an effect on incident stress than those whose stress is at lower levels. The lack of effect of emotional distress for those with greater baseline stress may be due in part to a ceiling effect for these individuals. Since their level of stressful experiences was high and potentially close to a maximum level to begin, the level of emotional distress may have had little influence on future levels of stressful or traumatic experiences. These findings have clinical implications in identifying a high-risk population. Individuals with low baseline stress appear to be vulnerable to incident stressful and traumatic events when faced with higher levels of emotional distress. These individuals may particularly benefit from case management or mental health interventions at times of increased emotional distress.
Although the number of different types of lifetime trauma experienced by the participant was related to incident stressful experiences in bivariable analyses, this relationship was not identified in the multivariate models. These findings seem to indicate a stronger influence of more recent stressful experiences on incident stress. There were few strong relationships between demographic characteristics and incident stress. However, younger age was associated with increased risk of any incident stress and with incident traumatic stress. In addition, being disabled was strongly associated with traumatic stress. This finding is consistent with previous studies that identified individuals with disabilities to be at greater risk for experiencing physical or sexual abuse. (Powers, Hughes, & Lund, 2009; Nosek and Howland 1997; Myers and Calvey 1999)
Limitations
The results of this study should be interpreted in the context of the study limitations. While the CHASE cohort is largely representative of HIV-infected individuals in medical care in the Southeast U.S., this sample may lack generalizability to individuals in other regions of the country. However, focusing upon an understudied region of the US that is disproportionately impacted by the domestic HIV epidemic may also be considered a strength. The study results may also be influenced by selection bias, due to missing data at the three follow-up data points. In addition, despite the longitudinal design, it is difficult to determine the causal direction of the relationships between stress and its predictors (e.g., Do depression and substance use lead to stressful events or vice versa?).
Conclusions
Study results indicate that incident stressful experiences frequently occur among individuals with HIV/AIDS. As these stressful experiences have been associated with poorer health outcomes (Mugavero et al., 2009; Pence et al., Leserman et al., 2008) and may lead to lowered quality of life, preventing these stressors or attenuating the mutable factors, including emotional distress and substance use, that predict stressful experiences is critical. More research is needed to determine the interventions that can be successful in reducing incident stress and trauma. These likely include improved identification of those experiencing high levels of stressful experiences, provision of evidence base mental health and substance use treatment, land targeted case management to address unmet needs, particularly among those most vulnerable to incident stress and trauma.
FIGURE 1.
Illustration of the Interaction Between Baseline Stressful Experiences and Mental Health Symptomatology in Predicting Incident Stressful Events:
Acknowledgments
Sources of support: This study was supported by grant 1 R03 MH081776-01 from the National Institute of Mental Health (NIMH) of the National Institutes of Health (NIH). The original CHASE study was supported by the NIMH, the National Institute of Drug Abuse, and the National Institute of Nursing Research (Grant# 5R01MH061687-05) of the NIH. MJM is supported by grant K23MH082641 from the NIMH of the NIH. The content is solely the responsibility of the authors and does not necessarily represent the official views of the NIMH or the NIH.
Appendix A
| Stressor | Moderate Stressor | Severe stressor | Trauma (subset of severe stressors) |
|---|---|---|---|
| Death of Family or Friend | |||
| Spouse | X | X | |
| Child | X | X | |
| Mother | X | ||
| Father | X | ||
| Brother | X | ||
| Sister | X | ||
| Grandparent | X | ||
| Other relative | X | ||
| Close friend | X | ||
| Sexual Assault | X | X | |
| Physical Assault | X | X | |
| Health | |||
| Major illness/injury not HIV related | X | ||
| Hospitalized | X | ||
| Car Accident | X | ||
| Illness/Injury | |||
| Spouse | X | ||
| Child | X | ||
| Mother | X | ||
| Father | X | ||
| Brother | X | ||
| Sister | X | ||
| Grandparent | X | ||
| Other relative | X | ||
| Close Friend | X | ||
| Financial* | |||
| Behind in Bills | X | ||
| Bill collectors calling | X | ||
| Foreclosure | X | ||
| Repossession of car | X | ||
| Had to sell possessions | X | ||
| No money for basic Needs | X | ||
| Relationship | |||
| Get Married/Engaged | X | ||
| Divorced | X | ||
| Increased arguments | X | ||
| Estrangement | X | ||
| Employment | |||
| Employment Problems | X | ||
| Lost job | X | ||
| Looking for work if out of work | X | ||
| Long hours | X | ||
| Legal | |||
| Arrested for serious Crime | X | ||
| Prison | X | ||
| Spouse/relative Arrested | X | ||
| Safety | |||
| Felt unsafe in Neighborhood | X | ||
| Burglarized | X | ||
| Transitions | |||
| Pregnant/Baby | X | ||
| Ended formal Schooling | X | ||
| Left home for first Time | X | ||
| Child left home | X | ||
| Moved more than once | X |
Only one financial need is counted when calculating the number of moderate/severely stressful experiences and severely stressful experiences no matter how many financial concerns identified by study participants
References
- Allers CT, Benjack KJ. Connections Between Childhood Abuse and HIV Infection. Journal of Counseling and Devolopment. 1991;70:309–313. [Google Scholar]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 4. Washington, DC: 1990. [Google Scholar]
- Arnsten JH, Demas PA, Grant RW, Gourevitch MN, Farzadegan H, Howard AA, Schoenbaum EE. Impact of active drug use on antiretroviral therapy adherence and viral suppression in HIV-infected drug users. Journal of General Internal Medicine. 2000;17(5):377–80. doi: 10.1046/j.1525-1497.2002.10644.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Avants SK, Warburton LA, Hawkins KA, Margolin A. Continuation of high-risk behavior by HIV-positive drug users: treatment implications. Journal of Substance Abuse Treatment. 2000;19(1):15–22. doi: 10.1016/s0740-5472(99)00092-6. [DOI] [PubMed] [Google Scholar]
- Basu S, Chwastiakb LA, Bru RD. Clinical management of depression and anxiety in HIV-infected adults. AIDS. 2005;19:2057–2067. doi: 10.1097/01.aids.0000182518.84407.32. [DOI] [PubMed] [Google Scholar]
- Blanchard EB, Jones-Alexander J, Buckley TC, Forneris CA. Psychometric properties of the PTSD Checklist (PCL) Behavioral Research Therapy. 1996;34:669–673. doi: 10.1016/0005-7967(96)00033-2. [DOI] [PubMed] [Google Scholar]
- Briere J, Elliott DM. Prevalence and psychological sequelae of self-reported childhood physical and sexual abuse in a general population sample of men and women. Child Abuse Negl. 2003;27:1205–1222. doi: 10.1016/j.chiabu.2003.09.008. [DOI] [PubMed] [Google Scholar]
- Carver C. You want to measure coping but your protocol’s too long: Consider the Brief COPE. International Journal of Behavioral Medicine. 1997;4:92–100. doi: 10.1207/s15327558ijbm0401_6. [DOI] [PubMed] [Google Scholar]
- Cohen MH, Cook JA, Grey D, Young H, Hanau LH, Tien P, Levine AM, Wilson TM. Medically eligible women who do not use HAART: the importance of abuse, drug use, and race. American Journal of Public Health. 2004;94:1147–51. doi: 10.2105/ajph.94.7.1147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Crepaz N, Passin WF, Herbst JH, et al. Meta-analysis of cognitive-behavioral interventions on HIV-positive persons’ mental health and immune functioning. Health Psychol. 2008;27(1):4–14. doi: 10.1037/0278-6133.27.1.4. [DOI] [PubMed] [Google Scholar]
- Derogatis LR, Melisaratos N. The Brief Symptom Inventory: an introductory report. Psychological Medicine. 1983;13:595–605. [PubMed] [Google Scholar]
- Derogatis LR. Brief Symptoms Inventory (BSI): Administration, Scoring, and Procedures Manual. Minneapolis, MN: NCS Pearson, Inc; 1993. [Google Scholar]
- Fairfield KM, Libman J, Davis RB, Eisenberg DM, Phillips RS. Delays in protease inhibitor use in clinical practice. Journal of General Internal Medicine. 1999;14:395–401. doi: 10.1046/j.1525-1497.1999.08198.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fitzmaurice GM, Laird NM, Ware JH. Wiley Series in Probability and Statistics. Hoboken, NJ: John Wiley & Sons, Inc; 2004. Applied Longitudinal Analysis. [Google Scholar]
- Gruskin L, Gange SJ, Celentano D, Schuman P, Moore JS, Zierler S, Vhalov D. Incidence of violence against HIV-infected and uninfected women: findings from the HIV Epidemiology Research (HER) study. Journal of Urban Health. 2002;79:512–24. doi: 10.1093/jurban/79.4.512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hamburger ME, Moore J, Koenig LJ, Vhalov D, Shoenbaum EE. Persistence of inconsistent condom use: relation to abuse history and HIV serostatus. AIDS and Behavior. 2004;8:333–344. doi: 10.1023/B:AIBE.0000044080.04397.97. [DOI] [PubMed] [Google Scholar]
- Himelhoch S, Medoff DR, Oyeniyi G. Efficacy of group psychotherapy to reduce depressive symptoms among HIV-infected individuals: a systematic review and meta-analysis. AIDS Patient Care STDS. 2007;21(10):732–9. doi: 10.1089/apc.2007.0012. [DOI] [PubMed] [Google Scholar]
- Kelly JA, Murphy DA, Bahr GR, Morgan MG, Kalichman SC, Stevenson LY, Brasfield TL, Bernstein BM, St Lawrence JS. Factors associated with severity of depression and high-risk sexual behavior among persons diagnosed with human immunodeficiency virus (HIV) infection. Health Psychology. 1993;12:215–219. doi: 10.1037//0278-6133.12.3.215. [DOI] [PubMed] [Google Scholar]
- Leserman J, Petitto JM, Gu H, Gaynes BN, Barraso J, Golden RN, Perkins DO, Folds JD, Evans DL. Progression to AIDS, a clinical AIDS condition and mortality: psychosocial and physiological predictors. Psychosomatic Medicine. 2002;32(6):1059–1073. doi: 10.1017/s0033291702005949. [DOI] [PubMed] [Google Scholar]
- Leserman J, Whetten K, Lowe K, Stangl D, Swartz MS, Thielman NM. How trauma, recent stressful events, and PTSD affect functional health status and health utilization in HIV-infected patients in the south. Psychosomatic Medicine. 2005;67(3):500–507. doi: 10.1097/01.psy.0000160459.78182.d9. [DOI] [PubMed] [Google Scholar]
- Leserman J, Pence BW, Whetten K, Mugavero MJ, Thielman NM, Swartz MS, Stangl D. Relation of lifetime trauma and depressive symptoms to mortality in HIV. American Journal of Psychiatry. 2007;11:1707–1713. doi: 10.1176/appi.ajp.2007.06111775. [DOI] [PubMed] [Google Scholar]
- Leserman J, Ironson G, O’Cleirigh C, Fordiani JM, Balbin E. Stressful life events and adherence in HIV. AIDS Patient Care STDS. 2008;22(5):403–411. doi: 10.1089/apc.2007.0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McHorney CA, Ware JE, Jr, Lu JF, Sherbourne CD. The MOS 36-item Short Form Health Survey (SF-36): III. Tests of data quality, scaling assumptions, and reliability across diverse patient groups. Medical Care. 1994;32(1):0–66. doi: 10.1097/00005650-199401000-00004. [DOI] [PubMed] [Google Scholar]
- McLellan AT, Kushner H, Metzger D, et al. The Fifth Edition of the Addiction Severity Index. Journal of Substance Abuse Treatment. 1992;9:199–213. doi: 10.1016/0740-5472(92)90062-s. [DOI] [PubMed] [Google Scholar]
- Mugavero MJ, Pence BW, Whetten K, Leserman J, Swartz M, Stangl D, Thielman NM. Predictors of AIDS-Related Morbidity and Mortality in a Southern U.S. Cohort. AIDS Patient Care STDS. 2007;21:681–690. doi: 10.1089/apc.2006.0167. [DOI] [PubMed] [Google Scholar]
- Mugavero M, Ostermann J, Whetten K, Leserman J, Swartz M, Stangl D, Thieleman N. Barriers to antiretroviral adherence: the importance of depression, abuse, and other traumatic events. AIDS Patient Care & STDS. 2006;20:418–428. doi: 10.1089/apc.2006.20.418. [DOI] [PubMed] [Google Scholar]
- Mugavero MJ, Raper J, Reif S, Whetten K, Leserman J, Thielman NM, Pence BW. Overload: The Impact of Incident Stressful Events on Antiretroviral Medication Adherence and Virologic Failure in a Longitudinal, Multi-site HIV Cohort Study. Psychosomatic Medicine. 2009;71(9):920–926. doi: 10.1097/PSY.0b013e3181bfe8d2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Myers L. Independent Living Research Utilization. TIRR Memorial Hermann; 1999. People with Disabilities and Abuse. Available at: http://www.bcm.edu/ilru/html/publications/readings_in_IL/abuse.html. [Google Scholar]
- Nosek MA, Howland C. Sexual abuse and people with disabilities. In: Sipski ML, Alexander CJ, editors. Sexual function in people with disability and chronic illness. Gaithersburg, Maryland: Aspen Publishers, Inc; 1997. pp. 577–594. [Google Scholar]
- Parienti JJ, Massari V, Descamps D, Vabret A, Bouvet E, Larouze B, Verdon R. Predictors of virologic failure and resistance in HIV-infected patients treated with nevirapine- or efavirenz-based antiretroviral therapy. Clinical Infectious Diseases. 2004;38:1311–1316. doi: 10.1086/383572. [DOI] [PubMed] [Google Scholar]
- Pence BW, Miller WC, Gaynes BN, Eron JJ., Jr Psychiatric Illness and Virologic Response in Patients Initiating Highly Active Antiretroviral Therapy. Journal of Acquired Immune Deficiency Syndromes. 2006 doi: 10.1097/QAI.0b013e31802c2f51. [DOI] [PubMed] [Google Scholar]
- Pence BW, Reif S, Whetten K, Leserman J, Stangl D, Swartz M, Thielman N, Mugavero MJ. Minorities, the poor, and survivors of abuse: HIV-infected patients in the US deep South. Southern Medical Journal. 2007;100(11):1114–1122. doi: 10.1097/01.smj.0000286756.54607.9f. [DOI] [PubMed] [Google Scholar]
- Pence BW, Raper JL, Reif S, Whetten K, Thielman NM, Leserman J, Mugavero MJ. The Association of Incident Stressful and Traumatic Life Events with HIV Sexual Transmission Risk Behaviors. Psychosomatic Medicine. doi: 10.1097/PSY.0b013e3181e9eef3. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pfeiffer E. A short portable mental status questionnaire for the assessment of organic brain deficit in elderly patients. Journal of the American Geriatric Society. 1975;23:433–441. doi: 10.1111/j.1532-5415.1975.tb00927.x. [DOI] [PubMed] [Google Scholar]
- Population Division U.S. Census Bureau. Table 1: Annual Estimates of the Population of Metropolitan Micropolitan Statistical Areas: April 1 2000 to July 1, 2005 (CBSA-EST2005–01) [Accessed September 10, 2006]; Available at: http://www.census.gov/population/www/estimates/Estimates%20pages_final.html.
- Powers LE, Hughes RB, Lund EM. Interpersonal Violence and Women With Disabilities: A Research Update. National Online Resource Center on Violence Against Women; 2009. Available at: http://new.vawnet.org/Assoc_Files_VAWnet/AR_WomenWithDisabilities.pdf. [Google Scholar]
- Sarason IG, Johnson JH, Siegel JM. Assessing the impact of life changes: development of the Life Experiences Survey. Journal of Consulting and Clinical Psychology. 1978;46(5):932–946. doi: 10.1037//0022-006x.46.5.932. [DOI] [PubMed] [Google Scholar]
- Scott-Sheldon LA, Kalichman SC, Carey MP, Fielder RL. Stress management interventions for HIV-positive adults: a meta-analysis of randomized controlled trials, 1989 to 2006. Health Psychol. 2008;27(2):129–39. doi: 10.1037/0278-6133.27.2.129. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sherbourne CD, Stewart AL. The MOS social support survey. Social Science and Medicine, 1991. 1991;32:705–14. doi: 10.1016/0277-9536(91)90150-b. [DOI] [PubMed] [Google Scholar]
- Sherbourne CD, Hays RD, Fleishman JA, Vitiello B, Magruder KM, Bing EG, McCaffrey D, Burnam A, Longshore D, Eggan F, Bozzette SA, Shapiro MF. Impact of psychiatric conditions on health-related quality of life in persons with HIV infection. American Journal of Psychiatry. 2000;157(2):248–54. doi: 10.1176/appi.ajp.157.2.248. [DOI] [PubMed] [Google Scholar]
- Sikkema KJ, Hansen NB, Kochman A, Tarakeshwar N, Neufeld S, Meade CS, Fox AM. Outcomes from a group intervention for coping with HIV/AIDS and childhood sexual abuse: reductions in traumatic stress. AIDS and Behavior. 2007;11(1):49–60. doi: 10.1007/s10461-006-9149-8. [DOI] [PubMed] [Google Scholar]
- Sikkema KJ, Watt M, Drabkin AS, Meade CS, Hansen NB, Pence BW. Mental health treatment to reduce HIV transmission risk behavior: a positive prevention model. AIDS and Behavior. 2010;14(2):252–262. doi: 10.1007/s10461-009-9650-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Simoni JM, Ng MT. Trauma, coping, and depression among women with HIV/AIDS in New York City. AIDS Care. 2000;12:567–80. doi: 10.1080/095401200750003752. [DOI] [PubMed] [Google Scholar]
- Spire B, Duran S, Souville M, Leport C, Raffi F, Moatii JP. Adherence to Highly Active Antiretroviral Therapies (HAART) in HIV-infected patients: from a predictive to a dynamic approach. Social Science and Medicine. 2002;54(10):481–96. doi: 10.1016/s0277-9536(01)00125-3. [DOI] [PubMed] [Google Scholar]
- Turner BJ, Fleishman JA, Wenger N, London AS, Burnam MA, Shapiro MF, Bing EG, Stein MD, Longshore D, Bozzette SA. Effects of drug abuse and mental disorders on use and type of antiretroviral therapy in HIV-infected persons. Journal of General Internal Medicine. 2001;16:625–33. doi: 10.1046/j.1525-1497.2001.016009625.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vlahov D, Wientge D, Moore J, et al. Violence against women with or at risk for HIV infection. AIDS and Behavior. 1998;2:53–60. [Google Scholar]
- Whetten K, Leserman J, Lowe K, et al. Prevalence of Childhood Sexual Abuse and Physical Trauma in an HIV-Positive Sample From the Deep South. American Journal of Public Health. 2006;96:1028–30. doi: 10.2105/AJPH.2005.063263. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Whetten K, Reif S, Ostermann J, Swartz M, Whetten R, Conover C, Bouis S, Thielman N, Eron J. Improving health outcomes among individuals with HIV, Mental illness, and substance use disorders in the Southeast. AIDS Care 2006. 2006;18(Supp1):18–26. doi: 10.1080/09540120600839330. [DOI] [PubMed] [Google Scholar]
- Wyatt GE, Myers HF, Williams JK. Does a history of trauma contribute to HIV risk for women of color? Implications for prevention and policy. American Journal of Public Health. 2002;92:660–5. doi: 10.2105/ajph.92.4.660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Zierler S, Cunningham WE, Andersen R, et al. Violence victimization after HIV infection in a US probability sample of adult patients in primary care. American Journal of Public Health. 2000;90:208–15. doi: 10.2105/ajph.90.2.208. [DOI] [PMC free article] [PubMed] [Google Scholar]