Abstract
The relationship between substance use, mental health disorders, and delinquency among youth is well documented. What has received far less attention from researchers is the relationship between these issues among truant youth, in spite of studies that document truants are a population at-risk for negative outcomes. The present study bridges this gap by (1) examining psychosocial functioning and delinquency among truants, and (2) assessing the efficacy of a Brief Intervention (BI) in reducing delinquent behavior over time. To meet these objectives, data were collected from 183 truant youth enrolled in an ongoing NIDA-funded BI project. Informed by a developmental damage perspective, a structural equation model was formulated and estimated. Interim results provide overall support for the model, and suggest the BI may be a promising, innovative intervention for truant youth. Service delivery implications and directions for future analyses are discussed.
The interrelationships of substance use, mental health disorders, and delinquency have been examined in a variety of ways, and comprise numerous cross-sectional and longitudinal studies involving at-risk youths, primarily those involved with the justice system. This body of literature provides ample evidence that significant relationships among these domains of behavior (e.g., D'Amico, Edelen, Miles, & Morral, 2008; Hayatbakhsh et al., 2008; Mannuzza, Klein, & Moulton, 2008; Paradise & Cauce, 2003; Salekin, 2008; Satterfield & Schell, 1997; Slade et al., 2008; Teplin et al., 2005; Van der Laan, Veenstra, Bogaerts, Verhulst, & Ormel, 2010; Vermeiren, De Clippele, Schwab-Stone, Ruchkin, & Deboutte, 2002). Alcohol and/or marijuana use, in particular, were often measured in these studies (e.g., Farrell, Danish, & Howard, 1992; Mason & Windle, 2002; Windle & Mason, 2004). With regard to mental health, the emotional/psychological issues examined typically included attention difficulties, impulsivity, and ADHD (e.g., Bor, McGee, & Fagan, 2004; Fergusson, Lynskey, & Horwood, 1997; White et al., 1994;), depression (e.g., Pelkonen, Marttunen, Kaprio, Huurre, & Aro, 2008), and, secondarily, psychopathy (Lynam, Caspi, Moffitt, Loeber, & Stouthamer-Loeber, 2007; Salekin, 2008).
With regard to substance use, positive relationships have consistently been found between alcohol, marijuana and other drug use (e.g., cocaine) and delinquent behavior in both cross-sectional and longitudinal studies involving a variety of samples in the U.S. (e.g., Mulvey, Schubert, & Chassin, 2010; Windle, 1993) and in other countries (e.g., Hayatbakhsh et al., 2008). Youths' emotional/psychological functioning problems have also been found to be related to substance use in delinquent (e.g., Teplin et al., 2005) and non-delinquent (e.g., Farrell, Danish, & Howard, 1992) samples of boys and girls.
In terms of emotional/psychological issues, considerable attention has focused primarily on conduct disorders characterized by aggressiveness, property destruction, deceitfulness, or lack of regard for rules or laws, which is quite prevalent among juvenile offenders, especially incarcerated youths (Lahey et al., 1994; Teplin, Abram, McClelland, Dulcan, & Mericle, 2002; Teplin et al., 2006; Wasserman, McReynolds, Ko, Katz, & Carpenter, 2005). Research findings suggest that conduct disordered juvenile offenders, especially those with callous traits comprise a minority of incarcerated youth, yet are responsible for the majority of crime, especially serious crime (Dembo et al., 2007; Frick & White, 2008; Hill & Maughan, 2001; Lynam et al., 2007; Salekin, 2008).
In recent years, however, increasing attention has been paid to ADHD-impulsivity and its relationship to delinquency and other psychosocial functioning problems among juvenile offenders. Past neglect of this relationship is surprising, given the prevalence of this disorder among these youths. For example, Teplin and colleagues (2006) found a six month prevalence of ADHD among 17% of male, and 21% of female detainees in an large urban county . Further, a sizable comorbidity has been found between ADHD and affective disorders (e.g., depression), substance use disorders, and anxiety disorders among juvenile offenders (Abram, Teplin, McClelland, & Dulcan, 2003; see also Molina & Pelham Jr., 2003). Related research indicates that ADHD delinquents may be more cognitively impaired in comparison to ADHD youths who are not involved in delinquent behavior. This finding suggests that significant neuropsychological deficits may exist in this group (Moffitt & Silva, 1988). Furthermore, as reported by Winters, Botzet, Fahnhorst, Baumel, and Lee (2009), impulsivity is an important component of ADHD among youths, and is associated with, and often precedes, an increased engagement in a variety of problem behaviors such as drug use and risky sexual activities (e.g., having sexual intercourse without using a condom).
Given the importance of the above findings, relatively few studies have documented the complex relationships between youths' substance use and mental health status in multiple domains (e.g., ADHD, depression, anxiety, and mania) to delinquent behavior over time. Further, we were unable to locate studies that have examined these relationships specifically among truant youth.
The Need for Research on Truant Youth
Truant youth represent a critical group needing more focused research and involvement in intervention services.. According to the Office of Juvenile Justice and Delinquency Prevention (Baker, Sigmon, & Nugent, 2001), hundreds of thousands of youth are truant each day, with many chronically absent. Relatedly, truant youth are often experiencing problems in school, troubled family situations, failing grades, and psychosocial difficulties which includes drug use (Dembo & Turner, 1994; Dembo et al., in press). Truant youth are often treated as management and disciplinary problems (DeKalb, 1999; Diebolt & Herlache, 1991; Dougherty, 1999). Resources are focused on identifying, locating, and transitioning truant youth back into their respective schools with sanctions and/or citations rather than identifying their problems and linking them with needed service programs (Dembo & Gulledge, 2009). The limited number of available studies involving selected samples of truant youth indicate these youth are often experiencing serious interrelated problems with regard to a stressed family life (Baker,et al., 2001; Kearney & Silverman, 1995), alcohol and other drug use (Baker et al., 2001; Dembo & Turner, 1994; Diebolt & Herlache, 1991), emotional/psychological functioning (Diebolt & Herlache, 1991; Egger, Costello, & Angold, 2003; Kearney & Silverman, 1995), and poor educational functioning (e.g., low grades, high rates of being retained in grade or placed in remedial or special programs) (Dembo & Turner, 1994; Garry, 1996; Ingersoll & LeBoeuf, 1997; Dembo et al., in press). Research also suggests that truant youths are at considerable risk of continuing their troubled behavior in school and entering the juvenile justice system (Garry, 1996; Ingersoll & LeBoeuf, 1997; Loeber & Farrington, 2000; Puzzanchera, Stahl, Finnegan, Tierney, & Snyder, 2003; also see Henry, Thornberry, & Huizinga, 2009).
In light of these findings, however, there is a lack of research examining the longitudinal relationships among truant youths' substance use, mental health, and delinquency. Reaching truant youth before they become more seriously involved in drug use and other delinquent behavior provides an excellent opportunity to reduce the likelihood they will move into the juvenile justice system. With few exceptions (e.g., Henry & Huizinga, 2007; McCluskey, Bynum, & Patchin, 2004), however, truancy has not received significant attention by criminologists.
The noted interrelated problem behaviors experienced by truant youth support the concept of problem behavior theory. According to this view, youth who engage in one specific form of deviant behavior (e.g., truancy) are also significantly more likely to report engaging in other types of deviant behaviors (e.g., drug use, delinquency) (LeBlanc & Bouthillier, 2003). The co-occurrence of such experiences among adolescents is reflective of a range of emotional difficulties that lead to expressions of problematic behavior. Thus, engagement in deviant behavior is seen as a symptom of the larger “general syndrome,” commonly referred to as problem behavior syndrome [(PBS) (Jessor & Jessor, 1977)].
There is a critical need to: (1) document the concurrent and longitudinal relationships among truant youths' substance use, mental health, and delinquency, and (2) assess the effect of intervention services on reducing delinquent behavior over time. These were the two main needs driving the objectives of the current research. Due to considerable interest in the field on brief interventions, we present interim results from an ongoing NIDA-funded Brief Intervention (BI) project.
This project is a prospective, longitudinal study involving substance involved truant youth The study is using random assignment to assess the impact of two Brief Intervention strategies ( BI-Youth and BI-Youth and Parent) in comparison to Standard Truancy Services (control condition), with regard to the youth's psychosocial functioning in the areas of drug use, involvement in sexual risk behavior, and delinquency/crime over time. The results presented here highlight the baseline and longitudinal data on the first 183 truant youth enrolled in the project and conclude with implications for intervention services.
The Tested Longitudinal Model
We hypothesized that truant youths' mental health problem (reflecting ADHD, mania, anxiety, and depression), substance involvement (reflecting alcohol use, marijuana use, use of other drugs, and DSM – IV drug use diagnosis) and delinquency, measured at baseline, constitute covarying psychosocial experiences. Further, each of these experiences is hypothesized to influence the youths' delinquent behavior at the three-month follow-up. A delinquency autoregressive effect is hypothesized for delinquency at six-month follow-up, which is also hypothesized to be influenced by baseline mental health and substance use. Finally, a delinquency autoregressive effect is hypothesized for delinquency at twelve-month follow-up, again hypothesized to be influenced by baseline mental health and substance use. Figure 1 presents a visual representation the longitudinal structural equation model being tested.
Figure 1.
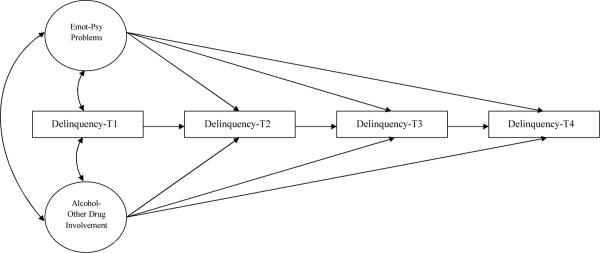
The Emotional-Psychological Problem, Alcohol/Other Drug Use, and Delinquency Longitudinal Model
This model specification is consistent with a developmental damage view, which asserts that the experience of stressful situations/events (e.g., mental health issues, family problems [including physical and/or sexual abuse]) relates to adverse consequences, including delinquency, over time. In line with this approach to problematic behaviors (Dembo, Williams, Wothke, Schmeidler, & Brown, 1992; Grella, Stein, & Greenwell, 2005; Robertson, Baird-Thomas, & Stein, 2008), youth mental health, substance use, and delinquency experiences establish a framework for the initiation and continuation of delinquent behavior over time. Although numerous multivariate studies have been completed on predictors of youth delinquency (see, for example, Lau & Chan, 1997; Lin & Dembo, 2008; Kim & Kim, 2008), our model is distinctive in its simultaneous incorporation of mental health problem and substance use/involvement variables.
Method
Subjects
The primary location for recruitment of subjects into the BI project occurred at a south Florida Juvenile Assessment Center, Truancy Intake Center (TIC). Eligible youth had to meet the following criteria: (1) between the ages of 11 and 15, (2) have no official record of delinquency or up to two misdemeanor arrests, (3) have some indication of alcohol or other drug use, as determined, for example, by a screening instrument, the Personal Experience Screening Questionnaire [PESQ (Winters, 1992)] or reported by a county school district social worker located at the TIC, and (4) live within a 25 mile radius of the TIC. In addition to the TIC, any social worker or guidance counselor from area schools can make referrals to the project.
Another location for recruitment was at a community diversion program where case managers could refer youth who met project eligibility. Project enrollment procedures were as follows (1) A project staff member meets with the youth and his/her parent/guardian and provides an overview of the project and its services. (2) They are informed that project services are provided in-home, are free, and that participation is voluntary. (3) For interested parents and youth, an in-home meeting is scheduled to discuss the project further, to answer any questions they have, complete the consent and assent processes, and to conduct separate baseline interviews with the youth and his/her parent/guardian. Following completion of the baseline interviews, the youth and parent/guardian are randomly assigned to one of three project service conditions: (1) the Standard Truancy Services, plus a referral service overlay involving three in-home visits by a project staff member (STS), (2) two BI sessions with the youth (Y), or (3) two BI sessions with the youth, one BI session with the parent (YP). With youth and parent permission, all BI sessions were audio recorded to assess fidelity. All study procedures were approved and monitored by the local IRB.
Of the 422 eligible truancy youth who were eligible for enrollment, 56% of families agreed to an initial in-home meeting. Of families who agreed to an initial in-home meeting, 77% completed the baseline assessment resulting in a sample of 183 youth. Comparisons of participating and non-participating youth with regard to gender, race, and ethnicity found no statistically significant differences between the two groups. However, older age youth (M = 14.77 (SD =1.30) were more likely to participate than younger-aged youth (M= 14.37 (SD = 1.12), t (420)=3.31, p<.001).
The main data collection instruments used in the study were the Adolescent Diagnostic Interview [(ADI) Winters & Henly, 1993], and the Parent/Guardian ADI (Winters & Stinchfield, 2003). Both the ADI and Parent ADI were designed to be delivered within a highly structured and standardized format (e.g., most questions are yes/no) to capture DSM- IV criteria to establish substance use disorders and related areas of functioning. Item construction primarily involved advice from an expert panel and feedback from field testers. DSM guidelines and results from the statistical analysis provided the basis for scoring rules. Reliability and validity studies, involving over 1000 drug clinic adolescents for the ADI and about 200 parents/guardians for the ADI-P, provide a wide range of psychometric evidence pertaining to interrater agreement, test-retest reliability, convergent validity (with clinical diagnoses), self-report measures, and treatment referral recommendations (Winters & Henly, 1993; Winters & Stinchfield, 2003).
Overview of the Brief Intervention
The primary goals of the BI therapist sessions are to promote abstinence and prevent relapse among drug using adolescents by promoting or strengthening coping skills that work to help the individual resist temptations to use and to increase social behaviors that are likely to interfere with drug seeking and using behaviors. Specific coping skill program elements are based on elements from Rational-Emotive Therapy (RET), which strives to alter beliefs that encourage and promote the use of effective coping-skills, and Problem-Solving Therapy (PST), which focus on developing the specific coping skills. These BI components dovetail with the view that drug involvement is learned behavior that develops within a context of personal, environmental, and social factors (Catalano, Hawkins, Wells, & Miller, 1991; Clark & Winters, 2002). Developed over the course of an adolescent's learning history and prior experience with drugs, coping skill deficits are viewed as primary determinants of drug use. Thus, the goal of the BI sessions is to diminish coping skill deficits and to promote coping skills (Winters & Leitten, 2007). Each BI session with project youth and parents lasts for 1–1/4 hours and the sessions occur about a week apart. Following is a brief description of these sessions:
Session 1(Youth). Focuses on discussing information about the youth's substance use and related consequences, the level of willingness to change, examining the causes and benefits of change, and discussing what goals for change the youth would like to select and pursue. Youth are allowed to pursue goals of drug abstinence or reduction in drug use.
Session 2 (Youth). Reviews the youth's progress with the agreed upon goals, identifies risk situations associated with difficulty in achieving goals, discusses strategies to overcome barriers toward goal achievement, reviews where the youth is in the state of change process, and negotiates either continuation or advancement of goals.
Session 3 (Parent). Informed by an integrated behavioral and family therapy approach, the parent session addresses: the youth's substance use issues, parent attitudes and behaviors regarding this use, parent monitoring and supervision to promote progress towards their child's intervention goals, and parent communication skills to enhance youth-parent connectedness.
BI Counselor Training - BI counselors received training from a skilled trainer on all intervention components as well as a treatment manual . During training, counselors were required to provide BI services to several practice cases while being observed. Following a review and approval of these sessions by the BI skilled trainer, with a focus on developing therapist adherence (aided by a rating checklist) and competence (e.g., perceived warmth and interest in the client, presentation clarity, ability to elicit client feedback), the interventionist were allow to deliver BI to e project families.
Standard truancy services (STS)
For the participants in the control condition, in addition to the normal truancy services provided by the school district, truant youths and their parents/guardians in the project had access to a countywide agency and service resource guide to assist them in connecting with needed services/programs. Developed over a period of several years, this resource guide contains hundreds of agency listings. Informed by the concept of equipoise (Freedman, 1987), we sought to provide meaningful services to individuals in each research condition. Hence, this service referral assistance provided truant youth and their families in the control condition with an additional resource that is not routinely available to them.
To control for possible effects due to service exposure, STS youths/families receive 3 hour-visits by a project staff member. On each visit, the project staff member had a copy of a county government-developed agency and service resource guide with them. In addition to a general inquiry on events since the last session, she or he asks the youth and his or her parents/guardians: (1) if they used any services and (2) if they have any additional service needs; and, if so, make an appropriate referral.
Initial and Follow-up Interviews
Baseline interviews were completed with 183 youth and their parents/guardians between March 2007 and June 2010. Each youth and parent/guardian was paid $15 for completing the interview. The baseline interviews for parents/guardians averaged 30 minutes; the youth interviews averaged one hour. The three month follow-up interviews were scheduled for 90-days following the date of the youth's last participation in project services (i.e., the last intervention or Standard Truancy Services session). The six month follow-up interview date was scheduled for 90 days following completion of the 3 month follow-up interview; and the 12 month follow-up interview was scheduled for 180 days after the completion date of the 6 month follow-up interview. Just as in the baseline interviews, each youth and parent/guardian was paid $15.00 for each follow-up interview. The majority of youths were interviewed in their home at each follow-up time point, while a very small number of youth were interviewed in secure program settings, such as residential commitment programs, county jails, or a juvenile detention center. For 3 month, 6 month, and 12 month follow up interviews, respectively, 1.3%, 0.8%, and 2.5% of youth were interviewed in a secure program setting.
We achieved very high rates of 3 month (n=139; 91.4%), 6 month (n=116; 91.1%)), and 12 month (n=72; 91.1%) follow-up interview completion. The majority of the follow-up interviews were completed within 60 days of the proceeding interview: ninety-eight percent of the 3 month follow-up interviews, 97% percent of the 6 month follow-up interviews, and 98% of the 12 month follow-up interviews Similarly, high percentages of follow-up interviews were completed within 30 days of the anniversary of their preceding interview: 85.5% of the 3 month follow-up interviews, 84.1% of the 6 month follow-up interviews, and 87.3% of the 12 month follow-up interviews.
Sample Characteristics
Most of the youth in the study (n=183) were male (65%). They averaged 14.81 years in age (SD= 1.31). Thirty-nine percent of the youth were Caucasian, 24% were African American, 28% were Hispanic, 2% were Asian, and 8% were from other, mainly multi-ethnic backgrounds. Relatively few youth (13%) lived with both their biological parents. On the other hand, a majority of the youth were living either with their biological mother alone (33%) or with their mother and another adult (36%). Nine percent of the caretakers reported an annual income of more than $75,000, while 39% reported annual incomes of $25,000 or less. Median family income was $25,000 to $40,000.
Maximum Likelihood (ML) and Bayesian Estimation
The responses to the mental health questions in the Adolescent Diagnostic Interview were linked to DMS-IV criteria In order to create summary measures for each domain, exploratory and confirmatory factor analyses using maximum likelihood (ML) and Bayesian estimation procedures were used.
Currently, ML estimation procedures are extensively used in statistical analyses. In recent years, however, Bayesian analysis is becoming increasingly utilized. Bayesian estimation is a preferred approach for analyzing relatively complex models, especially when data are sparse or samples are small--where asymptotic distributions, underlying ML/other frequentist estimation procedures, are unlikely to hold (Lynch, 2010; Rupp, Dey, & Zumbo, 2004; Scheines, Hoijtink, and Boomsma, 1999). When samples are large, the results of maximum likelihood and Bayesian analysis tend to be similar.
Two estimates of model adequacy are important in Bayesian analysis, which is firmly established in mainstream statistics: convergence and mixing, and model fit. In Bayesian analysis, Markov chain Monte Carlo (MCMC) estimation algorithms are used to make random draws of parameter values, resulting in an approximation of the joint distribution of all parameters in the analysis. Usually, several MCMC chains are used, involving different starting values and different random seeds in making the random draws (Muthèn & Asparouhov, 2010; see also Lynch, 2010). The Gelman-Rubin diagnostic (Gelman & Rubin, 1992; see also Gelman, Carlin, Stern, & Rubin, 2004), referred to as the potential scale reduction (PSR) factor, is often used to assess convergence-mixing. A PSR value close to 1 and below 1.1 is considered as evidence that convergence and adequate mixing have been achieved.
Model fit refers to assessing whether the model fits the data well enough to permit the drawing of inferences about the parameters (Lynch, 2010). One of the best approaches for examining model fit is posterior predictive distribution checking, introduced by Gelman, Meng, Stern, and Rubin (1996) and refined by Gelman et al., (2004). As implemented in Mplus (Muthèn & Muthèn, 2010), a posterior predictive p-value (PPP) fit statistic is based on the commonly used likelihood-ratio chi-square test of an H0 model against an unrestricted H1 model (Muthèn & Asparouhov, 2010). A low PPP value (e.g., .05 or .01 [see Asparouhov & Muthèn, 2010]) indicates a poor fit, with values around 0.5 reflecting an excellent fit. These procedures were used in for following domains: Emotional (Attention Deficit Hyperactivity Disorder (ADHD), Mania, Anxiety, and Depression), and Problem Substance Use (alcohol, marijuana and other drugs). Additionally, youth were asked to self-report on delinquency behavior and time in secure settings. Each domain is discussed separately below.
Emotional/Psychosocial Factors Using Bayesian Estimation
The youth reported high levels of emotional and psychological disorders in the domains of Attention Deficit Hyperactivity Disorder (ADHD), Mania, Anxiety, and Depression, The rates of these problems in the sample and the results of efforts to create summary measures in each domain is described below.
Attention deficit hyperactivity disorder
Four questions were keyed to DSM-IV criteria for ADHD and were included in the youth ADI interviews (Winters & Henly, 1993). From 32 to 71 percent of the youths reported ever experiencing one or more of these issues, see Table 1.
Table 1.
Youth Responses to the Mental Health Questions
| Percentage | ||
|---|---|---|
| Variable | Question | Responding Yes |
| ADHD | ||
| Inattention | Do you find that you are the type of person who gets complaints from parents or teachers that you don't listen to instructions or directions? | 55 |
| Impulsivity | Do you frequently tend to act before thinking? | 71 |
| Difficulty waiting | Do you often have difficulty waiting for your turn during games or when doing things with other people your age? | 32 |
| Fidgeting | Do you often fidget and find it difficult to sit still? | 52 |
| Mania | ||
| Elation | Has there ever been a period of time of at least several days, during which time you were not using alcohol or other drugs, when you felt on top of the world—as though you had special abilities or superhuman talents? | 26 |
| Boundless energy | During such a period, when you were not using alcohol or drugs, have you ever felt that you had tremendous energy, like that of a superperson? | 39 |
| Racing thoughts | During such a period, when you were not using alcohol or drugs, did you ever feel as though your thoughts were racing? | 42 |
| Sleeplessness | During such a period, when you were not using alcohol or drugs, did you ever feel that you could go for a long period without sleep? | 30 |
| Anxiety | ||
| Parents | Do you worry a great deal when you are away from home that something bad might happen to your parents? | 45 |
| Social phobia | Do you often refuse to go to school because you are afraid that something bad will happen to your parents or some other important person? | 9 |
| Academic/peer | Do you ever worry a lot about how well you are doing as a student or whether you have enough friends? | 37 |
| Future | Do you worry a great deal about how future events will turn out? | 67 |
| Depression | ||
| Sadness | Has there ever been a continuous 2-week time period during which you felt sad or down most of the time—as if you didn't care about anything anymore? | 55 |
| Crying | Have you ever continuously felt like crying for several days in a row? | 32 |
| Insomnia | Have you ever had any trouble sleeping that lasted for many days? | 38 |
| Suicidal ideation | Have you ever felt so down that you felt like ending your life? | 20 |
| Suicide attempts | Have you ever actually attempted suicide? | 8 |
Note. N = 182 or 183, depending on variable.
Confirmatory factor analysis of the ADHD items
Confirmatory factor analysis, using maximum likelihood and Bayesian estimation, were was used to assess how well a one factor model, involving each of the four ADHD items, fit the data (Muthèn & Muthèn 1998–2010, version 6.1). For the ML estimation, the comparative fit index (CFI) and the Tucker-Lewis index (TLI) were used to evaluate model fit. The typical range for both CFI and TLI is between 0 and 1, although the TLI may achieve values slightly greater than 1,with values greater than .90 indicating an acceptable fit and values greater that .95 indicating a good fit (Hu & Bentler, 1999). Two additional indices were used to assess model fit: (1) the root mean square error of approximation (RMSEA); RMSEA values of .05 or less indicate a close model fit, and values between .05 and .08 indicate an adequate fit (Browne & Cudeck, 1993); and (2) the weighted root mean square residual (WRMR) for categorical variables; Yu and Muthén (2001) suggest WRMR <.90 indicate good models. Results indicated a very good fit for the single factor model (Chi-square=3.70[2], p=0.16; CFI= 0.987, TLI= 0.960, RMSEA= 0.068, WRMR= 0.464), with all standardized loadings greater than .50. Bayesian estimation also confirmed the existence of a one factor model. Good Markov chain Monte Carlo algorithm convergence was achieved, indicated by a low potential scale reduction value of 1.03. In addition, a good model fit, reflected in a posterior predictive p-value of 0.478 was obtained. Based on these results, an ADHD factor score was created for use in further analyses1.
Mania
With regard to mania symptoms, a quarter of the youths reported feeling elated for several days at least once in their lives, during which they felt they had special abilities or superhuman talents; forty percent of the youths reported experiencing boundless energy or having racing thoughts during these periods; and three-out-of-ten youths reported sleeplessness during such a period, see Table 1.
Confirmatory factor analysis of the mania items
Confirmatory factor analysis, using ML and Bayesian estimation, was used to assess how well a one factor model, involving each of the four mania items, fit the data (Muthèn & Muthèn 1998–2010, version 6.1). ML results indicated a very good fit for the single factor model (Chi-square= 3.18[2], p= 0.20; CFI= 0.986, TLI= 0.959, RMSEA= 0.057, WRMR= 0.480), with all standardized loadings greater than .45. . Bayesian estimation also confirmed the existence of a one factor model. Good Markov chain Monte Carlo algorithm convergence was achieved, indicated by a low potential scale reduction value of 1.05. In addition, a good model fit reflected by a posterior predictive p-value of 0.370 was obtained. Based on these results, a MANIA factor score was created for use in further analyses1. .
Anxiety
Many youths expressed anxiety. Two-thirds of the youths reported worry about their future; forty percent expressed concern over their parents' safety when they were away from home or worry about how well they were doing at school and having enough friends; and nearly ten percent noted they often refused to attend school due to fear of what might happen to a parent or other important person in their lives, See Table 1.
Confirmatory factor analysis of the anxiety items
Confirmatory factor analysis, using ML was used to assess how well a one factor model, involving each of the four anxiety fit the data (Muthèn & Muthèn, 2010, version 6.1). Results indicated the four anxiety items were significantly loaded on one factor. However, the distribution of these data did not meet the asymptotic distribution assumptions of ML, with a resulting poor model fit (Chi-square= 13.08[2], p= 0.001; CFI= 0.849, TLI= 0.546).
However, Bayesian estimation confirmed the existence of a one factor model. A good Markov chain Monte Carlo algorithm convergence was achieved, with a potential scale reduction value of 1.06. In addition, a good model fit, reflected in a posterior predictive p-value of 0.332 was obtained. Based on these results, the four dichotomous items were summed to obtain an overall summary anxiety measure for use in further analyses (range 0 to 4)1.
Depression
Many youths reported experiencing depression. A majority of youths reported experiencing sadness for a two-week period; nearly a third reported crying for several days in a row; and close to forty percent indicated they had trouble sleeping that lasted for many days, see Table 1. Further, one-in-five youths reported thoughts of ending their lives, and eight percent indicated they made attempts to do so in the past.
Confirmatory factor analysis of the depression items
Exploratory factor analysis indicated three questions associated with depression (insomnia, suicidal ideation, and suicide attempts) reflected one underlying factor. Hence, a separate CFA was completed on these three items. As was the case for the anxiety items, a CFA of the items using ML estimation with the variance of the latent variable fixed at 1.0, found the three items to be significantly loaded on one factor. At the same time, the highly skewed data (with only 20% (n=36) and 8% (n=15) of youths indicating “yes” to items 4 and 5, respectively) failed to meet asymptotic distribution assumptions, and the CFA model could not be estimated.
However, a very good one factor fit was obtained using Bayesian estimation. Markov chain Monte Carlo algorithm convergence was achieved, reflected in a potential scale reduction value of 1.06. A posterior predictive p-value of 0.455 indicated a good model fit. Based on these results, the three dichotomous items were summed to obtain an overall summary depression measure for use in further analyses (range 0 to 3)1..
Substance Use by Youth at Baseline
Alcohol use
The ADI alcohol questions probed the youths use of alcohol to the point of experiencing its effects, such as feeling a buzz or getting drunk (Winters & Henly, 1993) and responses were coded as never, 1 to 4 times, or five or more times. The baseline alcohol use questions probed lifetime use up until the time of the baseline interview. Over a third of the youths reported using alcohol five or more times to the point of feeling its effects, while 38% did not report this experience, see Table 2.
Table 2.
Youth Baseline Alcohol/Other Drug Involvement and Diagnosis (Lifetime)
| Variable | Percentage |
|---|---|
| Alcohol use to the point of feeling effects (e.g., intoxicated) | |
| None | 38 |
| 1–4 times | 27 |
| 5 or more times | 35 |
| Marijuana use (Self-Report and Urine Test Results | |
| Denied use and urine test results negative (n = 12) or not provided due to reasons beyond youth's control (n = 2) | 8 |
| Urine test missing or negative, but youth reported use 1–4 times | 18 |
| Urine test missing or negative, but youth reported use 5 or more times | 29 |
| Urine test positive | 45 |
| Other drug use (e.g., hallucinogens, opiates) | |
| None | 79 |
| 1—4 times | 12 |
| 5 or more times | 10 |
| Substance use diagnosis (alcohol or other drugs) | |
| None | 37 |
| Abuse | 35 |
| Dependence | 28 |
Note. N = 183.
Marijuana use
We measured marijuana use through self-report questions on the ADI (Winters & Henly, 1993), and the results of urine tests, both of which were administered at the time of the baseline interview. The ADI questions probed the use of marijuana as: never, less than five times, or five or more times. Ninety-two percent of the youths reported ever using marijuana, and 73% of 119 youths reporting marijuana use indicated they used the substance five or more times in their lifetime.
Other drug use
The youths were also asked about their use of other drugs. These drugs included amphetamines, barbiturates, cocaine, opioids, hallucinogens, PCP, Club Drugs (e.g., Ecstasy), and inhalants. Ten percent of the youths reported 5 or more times of use of one or more of these drugs, and 12 percent claimed to have used them 1 to four times. Barbiturates, followed by hallucinogens and cocaine, were the most frequently reported other drugs.
Urine specimens were also collected to assess recent drug use. The use of four substances was probed using the Onsite CupKit® urine screen procedure (positive threshold levels are noted in parentheses): (1) methamphetamines (1000 nanograms per milliliter [ng/ml] of urine), (2) opiates (300 ng/ml of urine), (3) cocaine (300 ng/ml of urine), and (4) marijuana (THC) (50 ng/ml of urine). No urine testing was done for alcohol use. Following are the surveillance windows for the four drugs: methamphetamines and opiates = 48 hours; cocaine = 72 hours; marijuana: moderate users = 5 days; heavy users = 10 days; chronic users = 20 days. Urine analysis (UA) results were available for 171 (93%) of the youths. Results indicated 48 percent urine tested positive for marijuana. Very few youths were urine test positive for the other drugs tested (amphetamines [4%], cocaine [<1%], and opiates [0%]).
We combined the self-reported marijuana and marijuana urine test data into an overall measure of marijuana use: (1) marijuana use denied, and UA test for marijuana negative; (2) marijuana use denied, and UA test data missing (due to reasons beyond the youth's control [e.g., incarcerated]); (3) UA test data missing and UA sample/specimen refused (not due to reasons beyond the youth's control); (4) UA test missing or negative for marijuana, but youths reported marijuana use one to four times; (5) UA test missing or negative, but youth reported marijuana use five or more times; (6) UA test positive for marijuana. A frequency breakdown of the six marijuana use categories indicated there were no youths in category (2), and only two youths in category (3). None of the youths with positive UA tests denied use. Hence, categories one to three were combined, and the resulting four ordinal category measure used in further analyses, see Table 2. .
Problem substance use
For youths reporting alcohol, marijuana, or other drug use, five of more times in their lives were asked detailed questions regarding the extent, experiences, and consequences of use for each drug. The responses for each drug were keyed to DSM-IV criteria for a substance use disorder, leading to a classification of each youth as having no diagnosis, a diagnosis of being an abuser, or dependent on the drug. Finally, the diagnostic results for the three categories of drugs (alcohol, marijuana, and other drugs) were combined into an overall measure, based on their most serious diagnostic classification on any of the three mutually exclusive drug categories: 0 = no diagnosis on any of the three categories of drugs, 1 = abuse disorder on any of the drug categories and no dependence disorder on all categories, and 2 = dependence disorder on any of the three categories of drugs. Nearly 3 of 10 youths were classified as being substance dependent, and over a third of the youths substance abusing, see Table 2.
Self-Reported Delinquent Behavior
Based on the work of Elliott, Ageton, Huizinga, Knowles, and Canter (1983), we measured the youths' prior delinquent behavior by asking how many times they engaged in each of 23 delinquent behaviors during the baseline interview. Youths who reported committing an act 10 or more times were also asked to indicate how often they participated in this behavior (once a month, once every two or three weeks, once a week, two to three times a week, once a day, or two to three times a day). Moreover, youths were asked to indicate the age during which a committed act first occurred for each delinquent behavior. Similar to Elliott et al. (1983), we developed five summary indices of delinquent involvement: general theft (e.g., petit theft, vehicle theft/joyriding, burglary); crimes against persons (e.g., aggravated assault, fighting, and robbery); index crimes (similar to UCR Index Part I); drug sales; and total delinquency (i.e., the sum of the 23 delinquent activities).
The youths reported relatively high rates of delinquency during the year prior to their initial interviews (n=183), see Table 3. High prevalence rates were reported for index offenses (48%), crimes against persons (74%), general theft (77%), drug sales (31%), and total delinquency (93%). Further, from 2% to 8% of the youths reported engaging in the offenses (represented by the various indices) 100 times or more; some reported many hundreds of offenses.
Table 3.
Self-Reported Delinquency
| Index/behavior (%) |
||||||||
|---|---|---|---|---|---|---|---|---|
| Frequency | 0 | 1–4 | 5–9 | 30–54 | 55–99 | 100–199 | ≥200 | Total |
| In year before initial interview (N = 183) | ||||||||
| Index offenses | 52 | 29 | 13 | 3 | < 1 | 2 | — | 99 |
| Crimes against persons | 26 | 34 | 27 | 5 | 3 | 2 | 2 | 99 |
| General theft | 23 | 36 | 30 | 7 | 2 | 2 | 2 | 102 |
| Drug sales | 69 | 15 | 9 | 2 | 1 | 2 | 1 | 99 |
| Total delinquency | 7 | 20 | 39 | 13 | 7 | 8 | 8 | 102 |
| Frequency during 3-month follow-up period (n = 139) | ||||||||
| Index offenses | 78 | 17 | 6 | — | — | — | — | 101 |
| Crimes against persons | 56 | 26 | 14 | < 1 | 1 | 1 | — | 98 |
| General theft | 74 | 16 | 8 | — | 1 | — | < 1 | 99 |
| Drug sales | 88 | 4 | 5 | 1 | — | < 1 | — | 98 |
| Total delinquency | 40 | 28 | 21 | 3 | 6 | 1 | < 1 | 99 |
| Frequency during 6-month follow-up period (n = 116) | ||||||||
| Index offenses | 75 | 16 | 6 | 2 | — | — | < 1 | 99 |
| Crimes against persons | 64 | 22 | 11 | < 1 | < 1 | — | < 1 | 97 |
| General theft | 72 | 20 | 6 | — | < 1 | < 1 | < 1 | 98 |
| Drug sales | 84 | 8 | 7 | — | — | — | 2 | 101 |
| Total delinquency | 42 | 29 | 19 | 4 | < 1 | 3 | 2 | 99 |
| Frequency during 12-month follow-up period (n = 72) | ||||||||
| Index offenses | 75 | 14 | 11 | — | — | — | — | 100 |
| Crimes against persons | 69 | 14 | 12 | 1 | 1 | 1 | — | 98 |
| General theft | 65 | 24 | 8 | 3 | — | — | — | 100 |
| Drug sales | 79 | 12 | 7 | — | — | 1 | — | 99 |
| Total delinquency | 42 | 33 | 17 | 1 | 4 | 1 | 1 | 99 |
Compared to their reported delinquency at baseline youths rates of offenses overtime tended to be lower. The rate of index offenses at baseline were 48%, while 3 month (n= 139), 6 month (n = 116) and 12 month (n=72) rates were, 22%, 25%, and 25% respectively. Crimes against persons were 74% at baseline and 44%, 36%, and 31% at the time of the 3, 6, and 12 month follow-up interviews. General theft: was 77% at baseline and 26%, 28%, and 35% overtime; drug sales was 31% at baseline and 12%, 16%, and 21% overtime, while total delinquency was 93% at baseline and 60%, 58%, and 58% over time.
The range of responses to the items comprising the five self-reported delinquency scales was large, ranging from no activity to hundreds (and in few cases thousands), and analysis of the frequency data as an interval scale was not appropriate as a measure of involvement in delinquency/crime. Raw numbers of offenses do form an interval scale, which might be useful if one were predicting crime rates for populations. However, the difference between no offense and 1 offense is not the same as the difference between 99 and 100 offenses in terms of involvement. A transformation was employed so that equal intervals on the transformed scale would represent differences in involvement. We interpreted the differences between 1 and 10, 10 and 100, and 100 and 1,000 offenses as being comparable. Accordingly, we log transformed the number of offenses for each scale to the base 10.
For any base, logarithms exist for all positive numbers. The choice of base does not matter if the logarithms are analyzed by a statistical procedure invariant under linear transformation, such as analysis of variance, multiple regression, discriminate analysis, or factor analysis. However, regardless of the base, the logarithm of 0 does not exist. Some other method must be employed to determine the score assigned to no offenses. For any base, 0 is the logarithm of the value 1, and 1 is the logarithm of the base. If the difference from “base” offenses (10 in this study) to 1 offense is assigned the difference in logarithm scores of 1 and 0, this provides a unit of measurement for assigning a score even lower than 0 (a negative number) to no offenses. In this study a score of −1 was assigned. This evaluates the difference between no offense and 1 offense as equal in importance as the difference between 1 offense and 10, or between 10 offenses and 100 (Dembo & Schmeidler, 2002).
The correlation between the log transformed measure of total delinquency and the other delinquency measures was sizable and statistically significant at each data collection point (baseline mean correlation= .618; 3 month follow-up mean correlation= .614; 6 month follow-up mean correlation= .697; 12 month follow-up mean correlation= .750). Importantly, the skewness and kurtosis of the log transformed measure of total delinquency were dramatically lower than those of the untransformed measure at each data collection point. Hence, we decided to use the log transformed measure of total delinquency in our analyses.
Time in Secured Settings
Time in a secure setting reduces the likelihood of engaging in risk behavior. Hence, for each youth we determined at each follow-up period from official record data, the number of days he/she spent in a secure facility (e.g., detention center, jail, residential commitment program, detoxification facility, treatment program). Study of the data indicated there was no need to adjust for time at risk in our analyses for three main reasons: (1) relatively few youths were placed in a secure facility during the 3 month, 6 month (a 90 day period) and 12 month (a 180 day period) follow-up periods: (8%, 9% and 19%, respectively), (2) the average number of days placed in a secure facility during each of these follow-up periods were relatively few (1.5 days, 2.8 days, 4.2 days, respectively), and (3) the correlation between the number of the days spent in a secure facility during each follow-up period and the youths' self-reported delinquency during that period was low and non-significant (correlations: 3 month follow-up= .089; 6 month follow-up= .011; 12 month follow-up= .023).
Validity of the Self-Reported Delinquency Data
In order to evaluate the accuracy of the self-reported delinquency data, for each follow-up period correlations were obtained between the youths' self-reported, total delinquency, and official records of number of arrests. Three month follow-up indicated a marginally significant correlation (r=.157, p = .067, two-tailed test), and six month follow-up (r=. 219, p=.018, two tailed test) and twelve month follow-up (r=.331, p=.004, two tailed test) significant relationships, between self-reported, total delinquency and number of official record arrests.
Further, among youths who were not officially charged, the percentages who reported any delinquency were 58%, 55%, and 55% in the three follow-up periods, respectively. Among youths who had official charges, the percentages that denied any delinquency were 20%, 19%, and 32% in the three follow-up periods, respectively. These relatively low rates of denial of officially recorded delinquency compared to the rates of admission for delinquency among youths with no official delinquency record further suggest that most youths reported their delinquency fairly accurately.
Results
Strategy of Analysis
Our analyses proceeded in two steps. First, separate CFAs were completed on the emotional/psychological functioning measures (baseline depression, ADHD, anxiety, and mania) and of the alcohol and other drug use (baseline alcohol use, marijuana use, other drug use, and drug use diagnosis) measures. Next a structural equation analysis was completed to assess the model shown in Figure 1. Because the time of entry into the study determined the number of follow-up interviews each youth and parent/guardian received, the data that are missing are a consequence of the study design. Accordingly, the missing data were replaced in Mplus by a simulated value using a regression-prediction algorithm (Muthèn & Muthèn, 2010).
Confirmatory Factor Analysis of the Emotional/Psychological Functioning Measures
CFA, using Bayesian estimation, indicated the four emotional/psychological measures (depression, ADHD, anxiety, and mania) reflected one underlying factor called “mental health” with each indicator being loaded significantly on the factor. Good Markov chain Monte Carlo algorithm convergence was achieved in this CFA, which indicated a low potential scale reduction value of 1.04. In addition, a very good model fit, reflected in a posterior predictive p-value of 0.607 was obtained1
Confirmatory Factor Analysis of the Substance Use Measures
Bayesian estimation confirmed the four alcohol/other drug involvement measures (baseline alcohol use, marijuana use, other drug use, and drug use diagnosis) reflected one underlying factor called “substance use.” As for the mental health CFA, good Markov chain Monte Carlo algorithm convergence was achieved (potential scale reduction value= 1.07), and quite a good model fit was achieved (posterior predictive p-value= 0.303). Each substance use indicator was loaded significantly on the factor1.
Structural Equation Model Analysis
We next performed a structural equation analysis of the hypothesized model. using Bayesian estimation. Overall convergence and model fit statistics were good (potential scale reduction value= 1.07, and posterior predictive p-value= 0.182). In terms of specific, hypothesized effects, the mental health factor and substance use factor were each significantly and positively related to self-reported delinquency. In addition, mental health was significantly and positively related to delinquency at 6 month follow-up and 12 month follow-up. Further, there were significant, positive relationships between self-reported delinquency at baseline and 3 month follow-up, delinquency at 3 month follow-up and delinquency at 6 month follow-up, and delinquency at 6 month follow-up and delinquency at 12 month follow-up, see Table 4. The results provide considerable support for our hypothesized model.
Table 4.
Structural Equation Model Estimation Results
| 95% C. I. |
|||||
|---|---|---|---|---|---|
| Posterior | One-Tailed | Lower | Upper | ||
| Variable | Estimate | SD | p Value | 2.5% | 2.5% |
| Substance Use Factor | |||||
| Alcohol Use | 1.000 | 0.000 | 0.000 | 1.000 | 1.000 |
| Marijuana Use | 1.108 | 0.274 | 0.000 | 0.618 | 1.695 |
| Other Drugs | 2.602 | 0.953 | 0.000 | 1.701 | 5.277 |
| Substance Use Diagnosis | 4.087 | 1.108 | 0.000 | 2.183 | 6.210 |
| Mental Health Factor | |||||
| Depression | 1.000 | 0.000 | 0.000 | 1.000 | 1.000 |
| ADHD | 0.438 | 0.136 | 0.000 | 0.233 | 0.749 |
| Anxiety | 0.514 | 0.323 | 0.017 | 0.031 | 1.341 |
| Mania | 0.448 | 0.135 | 0.000 | 0.244 | 0.750 |
| Total Delinquency 3-month on | |||||
| Substance Use Factor | 0.272 | 0.211 | 0.086 | −0.113 | 0.699 |
| Mental Health Factor | −0.021 | 0.366 | 0.478 | −0.670 | 0.727 |
| Total Delinquency 6-month on | |||||
| Substance Use Factor | 0.229 | 0.195 | 0.116 | −0.151 | 0.617 |
| Mental Health Factor | 0.718 | 0.313 | 0.000 | 0.209 | 1.452 |
| Total Delinquency 12-month on | |||||
| Substance Use Factor | −0.022 | 0.250 | 0.457 | −0.502 | 0.479 |
| Mental Health Factor | 1.049 | 0.536 | 0.002 | 0.271 | 2.388 |
| Total Delinquency 3-month on | |||||
| Total Delinquency Baseline | 0.531 | 0.140 | 0.000 | 0.251 | 0.795 |
| Total Delinquency 6-month on | |||||
| Total Delinquency 3-month | 0.540 | 0.083 | 0.000 | 0.373 | 0.707 |
| Total Delinquency 12-month on | |||||
| Total Delinquency 6-month | 0.391 | 0.121 | 0.001 | 0.145 | 0.612 |
| Substance Use Factor and | |||||
| Total Delinquency Baseline | 0.160 | 0.046 | 0.000 | 0.081 | 0.262 |
| Mental Health Factor and | |||||
| Total Delinquency Baseline | 0.179 | 0.064 | 0.000 | 0.090 | 0.328 |
| Substance Use Factor | 0.009 | 0.032 | 0.392 | −0.049 | 0.076 |
| Total Delinquency Baseline (M) | 1.081 | 0.064 | 0.000 | 0.957 | 1.210 |
Demographic Predictors of the Structural Equation Model Variables
We examined the relationship between the demographic characteristics of age, gender, being African American, and Hispanic ethnicity, and each of the latent (i.e., mental health and substance use) and observed variables (i.e., self-reported delinquency at each of the four time points) in the model we tested. Several significant, but not patterned effects were found: (1) at baseline, older youths reported fewer mental health problems and more substance use than younger youth; (2) girls reported less delinquent behavior at 6 month follow-up than males; (3) at baseline, African American youth reported less substance use and less delinquent behavior than non-African American youth; and (4) Hispanic youth reported fewer mental health problems than non-Hispanic youth at baseline1.
The Effect of the BI Intervention on Delinquency Over Time
We assessed the direct effect of the intervention on self-reported delinquency at each of the three follow-up time points. Since we had a relatively small sample size, for each analysis we combined the Brief Intervention -Youth + Brief Intervention-Youth-Parent conditions, and compared them with the Standard Truancy Services (with a referral service overlay) condition. The effect of the brief intervention on self-reported delinquency was as follows: 3-month follow-up: −0.249 (p = 0.067, one tailed), 6-month follow-up: 0.197, and 12-month follow-up: −0.356 (p = 0.051, one tailed). These results reflect a marginally significant BI effect on self-reported delinquency at 3 month follow-up, and a near significant intervention effect on self-reported delinquency at 12 month follow-up. Table 5 reports the mean values for these log transformed measures, discussed in the self-reported delinquent behavior section, by intervention condition across the three follow-up periods.
Table 5.
Self-Reported Delinquency (and Standard Deviations) at Three-, Six-, and Twelve-Month Follow-ups by Intervention Condition
| Mean () Self-Reported Delinquency |
|||
|---|---|---|---|
| Intervention condition | 3 mos (n = 138) | 6 mos (n = 116) | 12 mos (n = 72) |
| Brief Intervention Groupa | .039 (1.020) n = 93 |
.094 (1.056) n = 80 |
−.033 (0.954) n = 52 |
| Standard Truancy Services Group | .226 (.037) n = 45 |
−.096 (1.010) n = 36 |
.140 (1.134) n = 20 |
Includes subjects from both groups of participants receiving the Brief Intervention, that is, the youth only group and the youth and parent group.
Mediated Effects of the Brief Intervention on Delinquency
For each follow-up time point, we examined for possible mediating effects of the Brief Intervention. Again, since we had a relatively small sample size, for each analysis we combined the Brief Intervention-Youth + Brief Intervention-Youth-Parent conditions, and compared them with the Standard Truancy Services condition. For each mediation model, we specified a direct effect of the recoded intervention variable on delinquency and a mediated effect on delinquency via the influence of the recoded intervention variable on the youths' reported delinquency during the prior time period. None of the indirect effects were statistically significant, implying that the effect of the intervention on reported delinquent behavior was primarily direct1.
Conclusion
The main purposes of the present study were to: (1) estimate a structural equation model, reflecting a developmental damage view, of the impact truant youths' mental health, substance use, and delinquency at first interview on their delinquent behavior over a one year follow-up period involving three data collection time points; and (2) to assess the effect of a Brief Intervention on the youths' delinquency over time. Results of our Bayesian estimation analyses provided support for the model. Analyses of a BI effect indicated a marginally significant, treatment effect on the youths' delinquency at 3 month follow-up, and a near significant BI effect at 12 month follow-up. Future analyses, involving a larger data set now being collected, should provide a more definitive conclusion on this issue.
We examined the effects of various demographic covariates on the observed and latent variables in the model. Overall, relatively few significant demographic effects were found. Four of the six significant effects pertained to the age of the youth and being African American. Older youth reported fewer mental health problems and more frequent substance use than younger aged youth. African American youth reported less frequent substance use and delinquency at baseline than non-African American youth.
The analyses were guided by a development damage view of problematic behaviors, and results we obtained were consistent with this view, as reflected in the model we tested (Dembo et al., 1992; Grella, et al., 2005; Robertson, et al., 2008). In particular, the youths' interrelated mental health, substance use, and delinquency issues measured at baseline set in motion dynamics which serve to continue their involvement in delinquent behavior over time. Interventions are needed to reduce the adverse, longitudinal effects of these troubled background experiences. The planned accrual of more baseline and follow-ups cases into the study, and extension of our analyses to an 18 month follow-up period, should provide more definitive information on this important issue.
There is a need for future work to pursue a more nuanced approach in understanding the longitudinal relationships between and among specific mental health issues and truant youth psychosocial functioning over time. Our analyses, involving an overall measure of mental health functioning summarizing four key emotional/psychological measures represents a beginning for such efforts.
Consideration of “spillover effects” is also an important consideration for intervention studies. According to the work of Ellickson, McCaffrey, and Klein (2009), drug prevention interventions can have “spillover effects” in reducing sexual risk behavior among youths. In general, among related risk behaviors, it could be expected that reduction in one risk behavior would result in the reduction of another–particularly if these behaviors are believed to reflect a syndrome of problem behavior (LeBlanc and Bouthillier, 2003; Jessor & Jessor, 1977). It is possible that non-specific factors, such as client expectations, readiness for change, and rapport developed between the interventionist and client, may account for at least some of the intervention effect we identified (Stout & Hayes, 2005). Although our examination of several mediation models indicated the effect of the brief intervention on reported delinquent behavior was primarily direct, we were not able to assess possibly important non-intervention specific factors on change in delinquent behavior. It would be important for future intervention research involving truant youth to address this issue.
A main focus of our analyses was to determine if there was a Brief Intervention effect on reducing the youths' delinquency over time. As noted earlier, there is some indication in our data that this is the case. Such a finding, if it holds up as we collect data on more cases, would provide evidence of a “spillover effect” of the BI, which focuses on substance use. These findings also highlight important psychosocial functioning issues that truant youth present, which current sanction-oriented approaches to truancy may not be addressing. There is particular need to utilize problem oriented, rather than sanction-based, responses to the psychosocial issues truant youth are experiencing. Service delivery practices need to be informed by the developing research literature on truant youth. Likewise, future studies should continue to explore alternative interventions for truant youth.
There were several limitations to this study. First, there were limitations due to the nature of the sample, which consisted of truant youth picked up by law enforcement or placed in a diversion program. Hence, the results of the study may not be generalizable to truant youth who do not have such agency contact/involvement. Second, the sample size was relatively small, precluding an examination of the fit of the models across various sociodemographic groups. Third, self-report data were mainly used in the analyses. While every effort was made to ensure data validity (e.g., conducting interviews in private in the youth's home, informed them of our Certificate of Confidentiality), it is possible some self-report bias is reflected in the data. At the same time, there is a consistency and coherence in our findings involving diverse data employed in a longitudinal analysis framework.
As noted earlier, planned, future analyses of our growing data set include replicating our examination of the developmental damage model over a longer time period, and involving more cases. Relatedly, we plan to conduct where feasible, multi-group SEM analyses for gender and race/ethnicity groups.
Footnotes
Results of these analyses are available from the first author.
References
- Abram KM, Teplin LA, McClelland GM, Dulcan MK. Comorbid psychiatric disorders in youth in juvenile detention. Archives of General Psychiatry. 2003;60(11):1097–1108. doi: 10.1001/archpsyc.60.11.1097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Asparouhov T, Muthèn BO. Technical appendix. Muthèn & Muthèn; Los Angeles: 2010. Bayesian analysis using Mplus: Technical implementation. www.statmodel.com. [Google Scholar]
- Baker ML, Sigmon JN, Nugent ME. Juvenile Justice Bulletin. U.S. Department of Justice, Office of Juvenile Justice Delinquency Prevention; Washington DC: 2001. Truancy reduction: Keeping students in school. [Google Scholar]
- Bor W, McGee TR, Fagan AA. Early risk factors for adolescent antisocial behavior: An Australian longitudinal study. Australian and New Zealand Journal of Psychiatry. 2004;38(5):365–372. doi: 10.1080/j.1440-1614.2004.01365.x. [DOI] [PubMed] [Google Scholar]
- Browne MW, Cudeck R. Alternative ways of assessing model fit. In: Bollen KA, Long JS, editors. Testing Structural Equation Models. Sage; Beverly Hills, CA: 1993. [Google Scholar]
- Catalano RF, Hawkins JD, Wells EA, Miller J. Evaluation of the effectiveness of adolescent drug abuse treatment, assessment of risks for relapse, and promising approaches for relapse prevention. The International Journal of Addictions. 1991;25:1085–1140. doi: 10.3109/10826089109081039. [DOI] [PubMed] [Google Scholar]
- Clark DB, Winters KC. Measuring risks and outcomes in substance use disorders prevention research. Journal of Consulting and Clinical Psychology. 2002;70(6):1207–1223. doi: 10.1037//0022-006x.70.6.1207. [DOI] [PubMed] [Google Scholar]
- D'Amico EJ, Edelen MO, Miles JNV, Morral AR. The longitudinal association between substance use and delinquency among high-risk youth. Drug and Alcohol Dependence. 2008;93(1–2):85–92. doi: 10.1016/j.drugalcdep.2007.09.006. [DOI] [PubMed] [Google Scholar]
- DeKalb J. Student truancy. ERICClearinghouse on Educational Management; Eugene, OR: 1999. ERIC Digest No. 125. [Google Scholar]
- Dembo R, Briones-Robinson R, Gulledge LM, Ungaro R, Schmeidler J, Belenko S, Winters KC. Emotional, psychological, and related problems among truant youths: An exploratory latent class analysis. Journal of Emotional and Behavioral Disorders. doi: 10.1177/1063426610396221. in press. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dembo R, Gulledge L. Truancy intervention programs: Challenges and innovations to implementation. Criminal Justice Policy Review. 2009;20(4):437–456. doi: 10.1177/0887403408327923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Dembo R, Jainchill N, Turner C, Fong C, Farkas S, Childs K. Levels of psychopathy and its correlates: A study of incarcerated youths in three states. Behavioral Sciences and the Law. 2007;25(5):717–738. doi: 10.1002/bsl.784. [DOI] [PubMed] [Google Scholar]
- Dembo R, Schmeidler J, USF Faculty and University Publications . Family empowerment intervention : An innovative service for high-risk youths and their families. Haworth Press; New York: 2002. [Google Scholar]
- Dembo R, Turner G. A pilot study of truants processed at the Hillsborough County Juvenile Assessment Center. The Journal of At-Risk Issues. 1994;1:38–42. [Google Scholar]
- Dembo R, Williams L, Wothke W, Schmeidler J, Brown CH. The role of family factors, physical abuse, and sexual victimization experiences in high-risk youths' alcohol and other drug use and delinquency: A longitudinal model. Violence and Victims. 1992;7(3):245–266. [PubMed] [Google Scholar]
- Diebolt A, Herlache L. The school psychologist as a consultant in truancy prevention. The annual meeting of the National Association of School Psychologists; Dallas,Texas. 1991. [Google Scholar]
- Dougherty JW. Attending to attendance. Phi Delta Kappa Education Foundation; Bloomington, IN: 1999. Fastback 450. [Google Scholar]
- Egger HL, Costello EJ, Angold A. School refusal and psychiatric disorders: A community study. Journal of the American Academy of Child & Adolescent Psychiatry. 2003;42(7):797–807. doi: 10.1097/01.CHI.0000046865.56865.79. [DOI] [PubMed] [Google Scholar]
- Ellickson PL, McCaffrey DF, Klein DJ. Long-term effects of drug prevention on risky sexual behavior among young adults. Journal of Adolescent Health. 2009;45(2):111–117. doi: 10.1016/j.jadohealth.2008.12.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Elliott DS, Ageton SS, Huizinga D, Knowles BA, Canter RJ. The prevalence and incidence of delinquent behavior: 1976–1980. Behavioral Research Institute; Boulder, CO: 1983. [Google Scholar]
- Farrell AD, Danish SJ, Howard CW. Relationship between drug use and other problem behaviors in urban adolescents. Journal of Consulting and Clinical Psychology. 1992;60(5):705–712. doi: 10.1037//0022-006x.60.5.705. [DOI] [PubMed] [Google Scholar]
- Fergusson DM, Lynskey MT, Horwood LJ. Attentional difficulties in middle childhood and psychosocial outcomes in young adulthood. The Journal of Child Psychology and Psychiatry. 1997;38(6):633–644. doi: 10.1111/j.1469-7610.1997.tb01690.x. [DOI] [PubMed] [Google Scholar]
- Freedman B. Equipoise and the ethics of clinical research. The New England Journal of Medicine. 1987;317(3):141–145. doi: 10.1056/NEJM198707163170304. [DOI] [PubMed] [Google Scholar]
- Frick PJ, White SF. The importance of callous-unemotional traits for the development of aggressive and antisocial behavior. Journal of Child Psychology and Psychiatry. 2008;49(4):359–375. doi: 10.1111/j.1469-7610.2007.01862.x. [DOI] [PubMed] [Google Scholar]
- Garry EM. Juvenile Justice Bulletin. U.S. Department of Justice, Office of Justice Programs, Office of Juvenile Justice and Delinquency Prevention; Washington, DC: 1996. Truancy: First step to a lifetime of problems. [Google Scholar]
- Gelman A, Carlin JB, Stern HS, Rubin DB. Bayesian data analysis. Second edition Chapman & Hall; Boca Raton, FL: 2004. [Google Scholar]
- Gelman A, Meng XL, Stern HS, Rubin DB. Posterior predictive assessment of model fitness via realized discrepancies (with discussion) Statistical Sinica. 1996;6:733–807. [Google Scholar]
- Gelman A, Rubin DB. Inference from iterative simulation using multiple sequences. Statistical Science. 1992;7(4):457–511. [Google Scholar]
- Grella CE, Stein JA, Greenwell L. Associations among childhood trauma, adolescent problem behaviors, and adverse adult outcomes in substance-abusing women offenders. Psychology of Addictive Behaviors. 2005;19(1):43–53. doi: 10.1037/0893-164X.19.1.43. [DOI] [PubMed] [Google Scholar]
- Hayatbakhsh MR, Najman JM, Jamrozik K, Al Mamun A, Bor W, Alati R. Adolescent problem behaviors predicting DSM-IV diagnoses of multiple substance use disorder: Findings of a prospective birth cohort study. Social Psychiatry and Psychiatric Epidemiology. 2008;43(5):356–363. doi: 10.1007/s00127-008-0325-1. [DOI] [PubMed] [Google Scholar]
- Henry KL, Huizinga DH. School-related risk and protective factors associated with truancy among urban youth placed at risk. Journal of Primary Prevention. 2007;28(6):505–519. doi: 10.1007/s10935-007-0115-7. [DOI] [PubMed] [Google Scholar]
- Henry KL, Thornberry TP, Huizinga DH. A discrete-time survival analysis of the relationship between truancy and the onset of marijuana use. Journal of Studies on Alcohol and Drugs. 2009;70(1):5–15. doi: 10.15288/jsad.2009.70.5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hill J, Maughan B. Conduct disorders in childhood and adolescence. Cambridge University Press; Cambridge: 2001. [Google Scholar]
- Hu L, Bentler PM. Cutoff criteria for fit indexes in covariance structure analysis: Conventional versus new alternatives. Structural Equation Modeling. 1999;6(1):1–55. [Google Scholar]
- Ingersoll S, LeBoeuf D. Reaching out to youth out of the education mainstream. U.S. Department of Justice, Office of Juvenile Justice and Delinquency Prevention; Washington, DC: Feb, 1997. [Google Scholar]
- Jessor R, Jessor SL. Problem behavior and psychosocial development: A longitudinal study of youth. Academic Press; San Diego, CA: 1977. [Google Scholar]
- Kearney CA, Silverman WK. Family environment of youngsters with school refusal behavior: A synopsis with implications for assessment and treatment. American Journal of Family Therapy. 1995;23(1):59–72. [Google Scholar]
- Kim H, Kim H. Juvenile Delinquency and Youth Crime. Nova Science Publishers, Inc.; New York, N.Y.: 2008. [Google Scholar]
- Lau KL, Chan DW. Family relationship, self-concept, and delinquent behavior among Chinese adolescents in Hong Kong. Education Journal. 1997;25:107–132. [Google Scholar]
- Lahey BB, Applegate B, Barkley RA, Garfinkel B, McBurnett K, Kerdyk L, Greenhill L, et al. DSM-IV field trials for oppositional defiant disorder and conduct disorder in children and adolescents. American Journal of Psychiatry. 1994;151:1163–1171. doi: 10.1176/ajp.151.8.1163. [DOI] [PubMed] [Google Scholar]
- LeBlanc ML, Bouthillier C. A developmental test of the general deviance syndrome with adjudicated girls and boys using hierarchical confirmatory factor analysis. Criminal Behavior and Mental Health. 2003;13(2):81–105. doi: 10.1002/cbm.533. [DOI] [PubMed] [Google Scholar]
- Lin W, Dembo R. An integrated model of juvenile drug use: A cross-demographic groups study. Western Criminology Review. 2008;9(2):33–51. [Google Scholar]
- Loeber R, Farrington DP. Young children who commit crime: Epidemiology, developmental origins, risk factors, early interventions, and policy implications. Development and Psychopathology. 2000;12(4):737–762. doi: 10.1017/s0954579400004107. [DOI] [PubMed] [Google Scholar]
- Lynam DR, Caspi A, Moffitt TE, Loeber R, Stouthamer-Loeber M. Longitudinal evidence that psychopathy scores in early adolescence predict adult psychopathy. Journal of Abnormal Psychology. 2007;116(1):155–165. doi: 10.1037/0021-843X.116.1.155. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lynch S. Introduction to applied Bayesian statistics and estimation for social scientists. Springer; New York, NY: 2010. [Google Scholar]
- Mason WA, Windle M. Reciprocal relations between adolescent substance use and delinquency: A longitudinal latent variable analysis. Journal of Abnormal Psychology. 2002;111(1):63–76. doi: 10.1037//0021-843x.111.1.63. [DOI] [PubMed] [Google Scholar]
- Mannuzza S, Klein RG, Moulton JL., III Lifetime criminality among boys with attention deficit hyperactivity disorder: A prospective follow-up study into adulthood using official arrest records. Psychiatry Research. 2008;160(3):237–246. doi: 10.1016/j.psychres.2007.11.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McCluskey CP, Bynum TS, Patchin JW. Reducing chronic absenteeism: An assessment of an early truancy initiative. Crime and Delinquency. 2004;50(2):214–234. [Google Scholar]
- Moffitt TE, Silva PA. Self-reported delinquency, neuropsychological deficit, and history of attention deficit disorder. Journal of Abnormal Child Psychology. 1988;16(5):553–569. doi: 10.1007/BF00914266. [DOI] [PubMed] [Google Scholar]
- Molina BSG, Pelham WE., Jr. Childhood predictors of adolescent substance use in a longitudinal study of children with ADHD. Journal of Abnormal Psychology. 2003;112(3):497–507. doi: 10.1037/0021-843x.112.3.497. [DOI] [PubMed] [Google Scholar]
- Mulvey EP, Schubert CA, Chassin L. Juvenile Justice Bulletin. U.S. Department of Justice, Office of Juvenile Justice and Delinquency Prevention; Dec, 2010. Substance use and delinquent behavior among serious adolescent offenders. [Google Scholar]
- Muthén B, Asparouhov T. Bayesian SEM: A more flexible representation of substantive theory. 2010 doi: 10.1037/a0026802. Submitted for publication. Available at: www.statmodel.com. [DOI] [PubMed]
- Muthèn BO, Muthèn LK. Mplus User's Guide. Sixth Edition. Muthèn & Muthèn; Los Angeles, CA: 2010. [Google Scholar]
- Paradise MJ, Cauce AM. Substance use and delinquency during adolescence: A prospective look at an at-risk sample. Substance Use & Misuse. 2003;38(3–6):701–723. doi: 10.1081/ja-120017390. [DOI] [PubMed] [Google Scholar]
- Pelkonen M, Marttunen M, Kaprio J, Hurree T, Aro H. Adolescent risk factors for episodic and persistent depression in adulthood: A 16-year prospective follow-up study of adolescents. Journal of Affective Disorders. 2008;106(1):123–131. doi: 10.1016/j.jad.2007.06.001. [DOI] [PubMed] [Google Scholar]
- Puzzanchera C, Stahl AL, Finnegan TA, Tierney N, Snyder HN. Juvenile Court Statistics 1998. U.S. Department of Justice, Office of Justice Programs, Office of Juvenile Justice Delinquency Prevention; Washington, DC: 2003. [Google Scholar]
- Robertson AA, Baird-Thomas C, Stein JA. Child victimization and parental monitoring as mediators of youth problem behaviors. Criminal Justice and Behavior. 2008;35(6):755–771. doi: 10.1177/0093854808316096. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rupp AA, Dey DK, Zumbo BD. To Bayes or not to Bayes, from whether to when: Applications of Bayesian methodology to modeling. Structural Equation Modeling. 2004;11(3):424–451. [Google Scholar]
- Salekin RT. Psychopathy and recidivism from mid-adolescence to young adulthood: Cumulating legal problems and limiting life opportunities. Journal of Abnormal Psychology. 2008;117(2):386–395. doi: 10.1037/0021-843X.117.2.386. [DOI] [PubMed] [Google Scholar]
- Satterfield JH, Schell A. A prospective study of hyperactive boys with conduct problems and normal boys: Adolescent and adult criminality. Journal of the American Academy of Child and Adolescent Psychiatry. 1997;36(12):1726–1735. doi: 10.1097/00004583-199712000-00021. [DOI] [PubMed] [Google Scholar]
- Scheines R, Hoijtink H, Boomsma A. Bayesian estimation and testing of structural equation models. Psychometrika. 1999;64(1):37–52. [Google Scholar]
- Slade EP, Stuart EA, Salkever DS, Karakus M, Green KM, Ialongo N. Impacts of age of onset of substance use disorders on risk of adult incarceration among disadvantaged urban youth: A propensity score matching approach. Drug and Alcohol Dependence. 2008;95(1–2):1–13. doi: 10.1016/j.drugalcdep.2007.11.019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Stout CE, Hayes RA, editors. The Evidence-Based Practice: Methods, Models, & Tools for Mental Health Professionals. Wiley; Hoboken, N.J.: 2005. [Google Scholar]
- Teplin LA, Abram KM, McClelland GM, Dulcan MK, Mericle AA. Psychiatric disorders in youth in juvenile detention. Archives of General Psychology. 2002;59(12):1133–1143. doi: 10.1001/archpsyc.59.12.1133. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Teplin LA, Abram KM, McClelland GM, Mericle AA, Dulcan MK, Washburn JJ. Juvenile Justice Bulletin. U.S. Department of Justice, Office of Juvenile Justice and Delinquency Prevention; 2006. Psychiatric disorders of youth in detention. [Google Scholar]
- Teplin LA, Elkington KS, McClelland GM, Abram KM, Mericle AA, Washburn JJ. Major mental disorders, substance use disorders, comorbidity, and HIV-AIDS risk behaviors in juvenile detainees. Psychiatric Services. 2005;56:823–828. doi: 10.1176/appi.ps.56.7.823. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wasserman GA, McReynolds LS, Ko SJ, Katz LM, Carpenter JR. Gender differences in psychiatric disorders at juvenile probation intake. American Journal of Public Health. 2005;95(1):131–137. doi: 10.2105/AJPH.2003.024737. [DOI] [PMC free article] [PubMed] [Google Scholar]
- White JL, Moffitt TE, Caspi A, Bartusch DJ, Needles DJ, Stouthamer-Loeber M. Measuring impulsivity and examining its relationship to delinquency. Journal of Abnormal Psychology. 1994;103(2):192–205. doi: 10.1037//0021-843x.103.2.192. [DOI] [PubMed] [Google Scholar]
- Windle M. A retrospective measure of childhood behavior problems and its use in predicting adolescent problem behaviors. Journal of Studies on Alcohol. 1993;54(4):422–431. doi: 10.15288/jsa.1993.54.422. [DOI] [PubMed] [Google Scholar]
- Windle M, Mason WA. General and specific predictors of behavioral and emotional problems among adolescents. Journal of Emotional and Behavioral Disorders. 2004;12(1):49–61. [Google Scholar]
- Winters KC. Development of an adolescent alcohol and other drug abuse screening scale: Personal Experience Screening Questionnaire. Addictive Behaviors. 1992;17(5):479–490. doi: 10.1016/0306-4603(92)90008-j. [DOI] [PubMed] [Google Scholar]
- Winters KC, Botzet AM, Fahnhorst T, Baumel L, Lee S. Impulsivity and its relationship to risky sexual behaviors and drug abuse. Journal of Child & Adolscent Substance Abuse. 2009;18(1):43–56. doi: 10.1080/15470650802541095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Winters KC, Henly GA. Adolescent Diagnostic Interview Schedule and Manual. Western Psychological Services; Los Angeles: 1993. [Google Scholar]
- Winters KC, Leitten W. Brief intervention for drug-abusing adolescents in a school setting. Psychology of Addictive Behaviors. 2007;21(2):249–254. doi: 10.1037/0893-164X.21.2.249. [DOI] [PubMed] [Google Scholar]
- Winters KC, Stinchfield RD. Adolescent Diagnostic Interview-Parent. University of Minnesota; Minneapolis: 2003. [Google Scholar]
- Van der Laan AM, Veenstra R, Bogaerts S, Verhulst FC, Ormel J. Serious, minor, and non-delinquents in early adolescence: The impact of cumulative risk and promotive factors. The TRAILS study. Journal of Abnormal Child Psychology. 2010;38(3):339–351. doi: 10.1007/s10802-009-9368-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Vermeiren R, De Clippele A, Schwab-Stone M, Ruchkin V, Deboutte D. Neuropsychological characteristics of three subgroups of Flemish delinquent adolescents. Neuropsychology. 2002;16(1):49–55. doi: 10.1037//0894-4105.16.1.49. [DOI] [PubMed] [Google Scholar]
- Yu CY, Muthén BO. Evaluation of model fit indices for latent variable models with categorical and continuous outcomes. University of California, Los Angeles, Graduate School of Education and Information Studies; Los Angeles: 2001. Technical report. [Google Scholar]


