Abstract
Background
An understanding of the relationships among obesity severity, medical co-morbidities, and psychological complications is important in the design of interventions to encourage overweight youth and families to accomplish healthy lifestyle changes.
Methods
We evaluated associations among psychological status, diagnosed medical co-morbidities consistent with components of the metabolic syndrome, and BMI among 166 obese adolescents (11–18 years) referred for endocrinology consultation. We hypothesized that there would be higher levels of psychological distress among youth with more diagnosed components of the metabolic syndrome (i.e., more medical co-morbidities associated with obesity).
Results
Contrary to expectation, we found that meeting criteria for extreme obesity alone was more predictive of psychological difficulties.
Conclusions
The degree of obesity may be more relevant than the number of associated medical co-morbidities in impacting psychological health. It is important to recognize individual differences between patients in terms of identifying motivating goals for accomplishing weight management.
Introduction
Medical and psychosocial complications associated with pediatric obesity are well established, and include type 2 diabetes, increased cardiovascular risk, sleep problems, musculoskeletal complaints, and mental health challenges.1 The metabolic syndrome is a cluster of obesity-related health risk factors that has risen markedly in prevalence and is currently found among 12.4–44.2% of overweight youth, depending on ethnicity.2 Although there are some distinctions between specific diagnostic criteria employed to define metabolic syndrome, it is generally designated as insulin resistance–related risk factors for the development of type 2 diabetes and/or cardiovascular disease, inclusive of obesity-related lipid abnormalities, hypertension, and hyperglycemia.3–5
An association between the diagnosis of metabolic syndrome and diminished psychological functioning, most often depressed mood, has been found among adults.6 In terms of behavioral considerations for youth, impaired quality of life, depression, and diminished social functioning have been reported among overweight children and adolescents.7 The association between obesity and diminished psychological functioning appears to increase in relation to the degree of overweight status, suggesting that those at the highest end of the obesity spectrum are the most vulnerable to psychological impairment.8 Compared to the relatively well-documented relationship between pediatric obesity and psychological impairment, the relationship between medical co-morbidities, or the number of components of the metabolic syndrome, and psychological functioning is less clear. Lower health-related quality of life was related both to greater number of medical co-morbidities and elevated BMI in prior work with a subsample of this cohort.9 However, more remains to be learned about whether youth psychological functioning is compromised by obesity alone, or by the number of diagnosed medical co-morbidities associated with overweight status. Among adults, depressive symptoms and psychological distress have been linked to components of the metabolic syndrome, such as hypertension and lipid abnormalities.10,11 Emerging data among youth with obesity-related co-morbidities suggest that the dual burden of obesity and medical complications may exacerbate psychological sequelae. For instance, elevated rates of depression, binge eating symptoms, and diminished quality of life have been reported among overweight youth with type 2 diabetes.12
It is important to characterize further whether medical co-morbidities associated with obesity, namely the components of the metabolic syndrome, demonstrate a cumulatively negative impact on psychological functioning. The adolescent patient population is particularly challenging due to a developmental period hallmarked by significant cognitive, emotional and interpersonal changes.13,14 The variability and vulnerability of adolescence underscores the necessity of maximizing our understanding of the factors involved in psychological distress among overweight adolescents. We hypothesized that the extent of psychological distress would directly relate to the number of diagnosed medical co-morbidities among overweight patients referred for endocrinology consultation. We expected that incremental increases in the number of diagnosed components of the metabolic syndrome, rather than obesity alone, would be associated with greater psychological distress. We also conducted exploratory analyses to examine the potential role of demographic variables (age, race/ethnicity, gender) in the relationship among obesity, co-morbidities, and psychological functioning.
Methods
Subjects
Patients referred to a pediatric endocrinology clinic by their primary care provider for evaluation of metabolic syndrome based on documented lab abnormalities or hypertension at the Children's Hospital Colorado between 2006 and 2011 were included in the study. The study was approved by the Colorado Multi-institutional Review Board (COMIRB) and written informed consent and assent were obtained from the primary caregiver and patient, respectively. Potential participants were informed about the research project in a confirmation letter prior to their appointment. Detailed information about the project was provided during the clinic visit, and consent was obtained from those interested in participating. Questionnaires were completed independently by the primary caregiver and patient. Additional data were retrieved via chart review following their appointment and completion of all relevant laboratory assays. Eligibility criteria for the current analyses included: (1) Patients 11–18 years of age accompanied by a primary caregiver, (2) completion of a questionnaire packet prior to clinic appointment by at least one respondent (primary caregiver and/or patient), and (3) BMI ≥95th percentile for age and sex and one or more additional medical components of metabolic syndrome [high-density lipoprotein cholesterol ≤40, triglycerides≥150, systolic or diastolic blood pressure >95th percentile for age and/or fasting blood glucose ≥100/mg/dL].15 Exclusion criteria included developmental delays or language barriers that would prevent self-report.
Measures
Demographics
Race and ethnicity were determined by caregiver report. Age and gender were obtained from registration data.
Medical
Height was measured using a wall-mounted stadiometer and weight was measured using a calibrated scale. Blood pressure was taken with the appropriate cuff, and laboratory measurements were obtained by standard assay methods. BMI percentiles and categories were calculated for age and gender according to the CDC. The 99th percentile was used as a cutoff indicative of extreme or morbid obesity.16 Rates of extreme obesity have tripled in the past 25 years, and the 99th percentile has been shown to be a valuable differentiating factor characterizing patients with the most substantial consequences from their overweight status.8,17–19
Psychological
Primary caregivers and patients completed the Strengths and Difficulties Questionnaire (SDQ), a broadly used measure of child mental health status with solid psychometric properties, including demonstrated reliability and validity.20–22 For each item, respondents are asked to indicate how true a series of statements are for them/their child in terms of recent functioning using a Likert-type scale. The total difficulties score, generated by summing the responses to four subscales, including emotional symptoms, conduct problems, hyperactivity/inattention, and peer relationship problems, was used for this analysis. The total difficulties score can range from 0 to 40, with higher scores indicating more difficulties. SDQ scores are often used as continuous variables; however, total difficulties scores have also been classified into the following classification system to assist with interpretation: Scores ranging from 0 to 13 are considered “normal,” scores ranging from 14 to 16 are considered “borderline,” and scores ranging from 17 to 40 are considered “abnormal.” Individual subscale scores were not examined in this analysis to avoid limitations to statistical power secondary to multiple comparisons. The prosocial score, reflecting a youth's strengths and helping behavior, was also evaluated. The prosocial scale consists of five items, and can range from 0 to 10 points, with higher scores indicating more prosocial behaviors. Scores ranging from 6 to 10 are considered to fall in the “normal” range of functioning, 5 is considered “borderline,” and 0 to 4 is considered “abnormal.”
Statistical Analysis
Statistical analyses were performed using SAS software version 9.2 (SAS Institute Inc., Cary, NC). Descriptive statistics were used to describe subject characteristics, and sample generalizability was addressed by comparing the final sample to adolescents from the same clinic with missing SDQ data and by comparing SDQ scores to a national data source.23 Data are reported as mean±standard deviation unless otherwise stated. Multiple regression analysis was used to examine BMI and medical co-morbidities as predictors of psychological functioning as rated by youth and caregiver report on respective versions of the SDQ. For all analyses, BMI was treated as a categorical variable measuring whether or not the adolescent was greater than or equal to the 99th percentile for their age and sex, and co-morbidities were treated as a count of the number of metabolic syndrome components. BMI≥99th percentile was entered first into the regression equation, followed by medical co-morbidities, to examine the unique variance accounted for (R2) by each predictor. Exploratory analyses examined whether the metabolic syndrome components or psychological functioning differed by demographic factors. Specifically, we examined differences in gender or race/ethnicity (independent samples t-tests), or age (Pearson correlations) and whether these demographic variables influenced the effect of BMI or medical co-morbidities on psychological functioning (statistical moderation tested by examining the interaction between each demographic variable with BMI≥99th percentile/co-morbidities).
Results
Sample Characteristics
Data were analyzed from 166 obese adolescents and their primary caregivers with complete BMI and co-morbidity data and computed total difficulties and prosocial scores on the SDQ. Subject characteristics are shown in Table 1.
Table 1.
Characteristics of the Sample
| Variable | n | Mean (SD) or no. (%) |
|---|---|---|
| Age | 166 | 14.2 (1.8) |
| Gender | 166 | |
| Male | 79 (47.6%) | |
| Female | 87 (52.4%) | |
| Race/ethnicity | 147 | |
| African American | 11 (7.5%) | |
| Hispanic | 43 (29.3%) | |
| Non-Hispanic white | 85 (57.8%) | |
| Other | 8 (5.4%) | |
| BMI (% ≥99th percentile) | 166 | 101 (60.8%) |
| Blood pressure (% >95th percentile for diastolic or systolic) | 166 | 98 (59.0%) |
| Fasting blood glucose (% ≥100 mg/dL)a | 115 | 19 (16.5%) |
| High-density lipoprotein (% ≤40) | 130 | 96 (73.9%) |
| Triglycerides (% ≥150) | 130 | 84 (64.6%) |
| Total difficulties, caregiver-reported | 163 | 13.10 (7.08) |
| Total difficulties, patient-reported | 163 | 12.31 (5.98) |
| Prosocial, caregiver-reported | 160 | 8.19 (2.00) |
| Prosocial, patient-reported | 160 | 8.16 (1.76) |
Calculated as glycated hemoglobin (HbA1c) ≥5.7% in the event of missing fasting blood sugar data (n=32).
SD, standard deviation.
To examine the representativeness of our sample, demographic, obesity, and metabolic syndrome component variables were compared between the n=166 participants with complete data and the n=153 with missing SDQ data seen in our Endocrinology Clinic during the same time period. The most common reason for missing SDQ data was the inability to complete data collection during high patient volume times secondary to limited staff resources. Of eight tests conducted (on three demographic variables and five obesity/metabolic syndrome variables), one significant difference was observed. Caucasian participants were more likely to have complete data (59.03%) as compared to minority participants (44.60%), χ2 (1)=5.89, p=0.015.
Generalizability was also assessed by comparing caregiver-reported SDQ scores from the present sample to normative data obtained from a national sample collected through the National Health Interview Survey.24 These analyses were conducted to determine how our sample compared to the general adolescent population regarding psychological functioning; child-reported SDQ normative values were not available.23 Means from the national data are reported stratified by age (ages 11–14 and ages 15–17). Therefore, also we stratified our data by the same age ranges for these analyses to facilitate comparisons to the national data. Caregiver-reported total difficulties scores were significantly higher in the present sample compared to the national data for both the 11–14 age range (13.02±6.7, n=106 vs. 7.1±6.2, n=2770, t=9.62, p<0.001, Cohen d=0.92) and the 15–17 age range (13.0±8.3, n=44 vs. 6.4±5.2, n=2265, t=8.22, p<0.001, Cohen d=0.95). Prosocial scores were significantly lower in the present sample for the 11–14 age range (8.2±1.97, n=103 vs. 8.7±1.8, n=2770, t=2.76, p=0.006, Cohen d=0.26) and the 15–17 age range (8.1±2.3, n=44 vs. 8.7±1.6, n=2265, t=2.44, p=0.015, Cohen d=0.30). Taken together, these results demonstrated poorer psychological functioning in our sample of obese adolescents relative to the general adolescent population.
Regression Analysis
Table 2 shows the results of the regression analyses testing the effect of BMI ≥99th percentile and the number of medical co-morbidities on SDQ scores. Higher BMI was predictive of higher total difficulties scores (both caregiver-reported and patient-reported) and of lower prosocial scores (patient-reported). BMI accounted for 4% of the variance in caregiver-reported and 5% of the variance in patient-reported difficulties scores, and 2% and 3%, respectively, for prosocial scores. In contrast, having a greater number of medical co-morbidities was not predictive of any of the four outcomes and did not account for a meaningful level of variance in outcomes (0.01–1%). These results demonstrate that BMI was more predictive of and accounted for more variance in psychological functioning than the number of co-morbidities. Supplementary analyses tested for an interaction between BMI and co-morbidities to determine whether the impact of BMI on outcomes depended on the number of co-morbidities. No significant interactions were observed, indicating that the effects of BMI on outcomes were independent of the number of co-morbidities.
Table 2.
Results of Multiple Regression Analyses Testing the Impact of BMI and Co-Morbidities on SDQ Scores
| |
BMI ≥99th percentile |
Co-morbidities |
||
|---|---|---|---|---|
| B (SE), t value | R2 | B (SE), t value | R2 change | |
| Difficulties, caregiver-reported | 2.90 (1.28) | 0.04 | 0.88 (0.70) | 0.01 |
| t=2.27, p=0.025 | t=1.25, p=0.21 | |||
| Difficulties, patient-reported | 2.87 (1.06) | 0.05 | 0.72 (0.59) | 0.01 |
| t=2.69, p=0.008 | t=1.24, p=0.22 | |||
| Prosocial, caregiver-reported | −0.58 (0.36) | 0.02 | 0.02 (0.20) | 0.0002 |
| t=−1.60, p=0.11 | t=0.15, p=0.88 | |||
| Prosocial, patient-reported | −0.62 (0.32) | 0.03 | 0.02 (0.18) | 0.0001 |
| t=−1.95, p=0.05 | t=0.10, p=0.92 | |||
SDQ, Strengths and Difficulties Questionnaire; SE, standard error.
Demographic Subgroup Analyses
Males scored significantly higher than females on the number of co-morbidities (2.28±0.97 compared to 1.74±0.73, t=3.58, p<0.001) and on mean BMI percentile (99.11±0.83 compared to 98.67±1.07, t=3.008, p=0.003), but there were no gender differences on any of the SDQ subscales or in terms of scoring greater than or equal to the 99th percentile for BMI. Ethnic/racial minority participants scored significantly lower than nonminority participants on the patient-reported prosocial subscale (7.63±1.70 compared to 8.59±1.63, t=3.37, p=0.001). There were no other ethnic/racial differences on the SDQ subscales, BMI percentile, or the number of co-morbidities. Higher adolescent age was associated with more co-morbidities (r=0.19, p=0.028) but not with any other key variables.
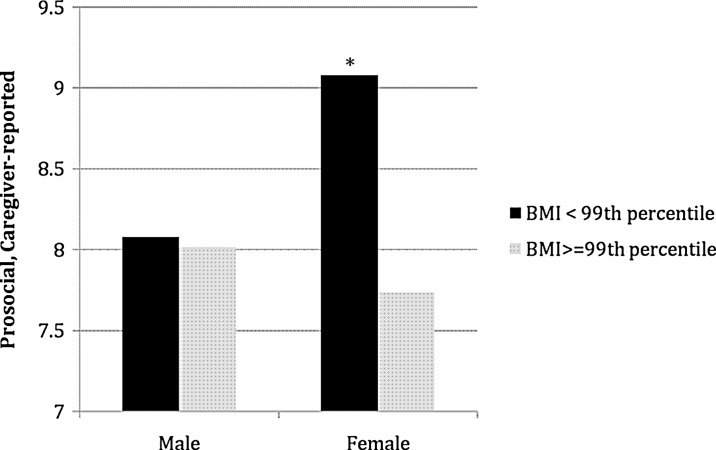
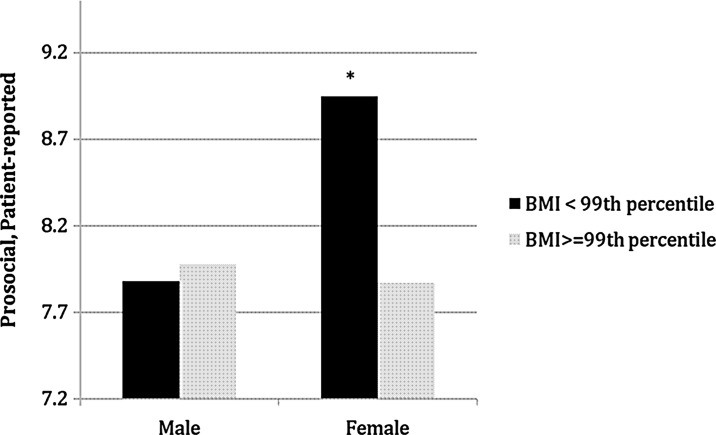
Gender, race/ethnicity, and age were then explored as moderators of the effect of BMI on SDQ scores (i.e., to test for subgroup differences in this effect). Moderation was examined by testing the significance of the statistical interaction among each demographic variable and BMI. Of 12 tests conducted (three demographic variables by four outcomes), the only evidence for significant moderation was for gender, where the effects of BMI on psychological functioning were stronger for females than for males. Specifically, significant interactions were observed for caregiver-reported prosocial scores [B=1.28 (standard error, SE=0.64), t=1.99, p=0.048] and patient-reported prosocial scores [B=1.18 (SE=0.57), t=2.09, p=0.039], but were not observed for caregiver-reported difficulties scores [B=3.28 (SE=2.25), t=1.46, p=0.15] or patient-reported difficulties scores [B=0.82 (SE=1.91), t=0.43, p=0.67]. This indicates that the impact of BMI on prosocial scores was observed among females only, but that the impact of BMI on difficulties scores was stable across genders. Figures 1 and 2 depict the pattern of means for these two interaction effects. The previously observed effects of BMI on psychological functioning were stable across racial/ethnic groups and adolescent age.
Figure 1.
Pattern of means for interaction between child gender and BMI ≥99th percentile on caregiver-reported prosocial scores. (Black) BMI <99th percentile; (grey) BMI ≥99th percentile. *p<0.05 for difference between BMI categories within females.
Figure 2.
Pattern of means for interaction between child gender and BMI ≥99th percentile on patient-reported prosocial scores. (Black) BMI <99th percentile; (grey) BMI ≥99th percentile. *p<0.05 for difference between BMI categories within females.
Discussion
Previous research has demonstrated impaired psychological status among overweight youth, and emerging data suggest that having a medical diagnosis related to obesity, such as type 2 diabetes, may exacerbate psychological impact of overweight status.12,25 On the basis of these findings, we expected the number of obesity-related co-morbidities, defined as the number of metabolic syndrome components, would relate to diminished psychological functioning above and beyond BMI. However, BMI above the 99th percentile, rather than the number of medical co-morbidities, more robustly predicted SDQ-assessed psychological difficulties, inclusive of emotional symptoms, behavioral disturbance, and social challenges and diminished prosocial functioning. In prior work with a subsample of this cohort, we found relationships among diminished health-related quality of life and the number of medical co-morbidities, as well as the extent of obesity.9 Taking the current analyses into consideration in comparison to prior work with a subsample, it appears that quality of life and psychological functioning may be operationally distinct in terms of relationships with co-morbidities and BMI severity. It is important to note, however, that methods and sample size differed between the two sets of analyses, and the current study subjects had a higher degree of obesity by implementing the 99th percentile for BMI as a cutoff indicative of morbid obesity.
The co-morbidities that comprise metabolic syndrome may have less impact on psychological functioning than the presence of extreme obesity due to their lack of overt characteristics or intrusive medical management tasks. For example, prediabetes does not require the level of self-care associated with overt type 2 diabetes, and hypertension typically has no symptoms. Instead, the degree of obesity itself may present an overt stressor for youth that takes a toll on psychological functioning. Our findings suggest that the extreme obesity, rather than cumulative number of related co-morbidities, is most impactful on psychological well-being for adolescents. In terms of clinical considerations, these findings suggest that when searching for strategies to motivate patients toward lifestyle change, clinicians may have more impact by addressing emotional experiences associated with obesity compared to emphasizing the urgency associated with metabolic syndrome components as precursors to more significant medical illness. Moreover, our findings underscore the importance of assessing psychological functioning among obese youth, particularly those in the extremely obese range. These youth may experience a more clinically substantial level of psychological dysfunction, suggesting the need for routine screening to identify patients reaching a threshold of distress that warrants clinical intervention.19 In the absence of such screening and treatment when indicated, it is unlikely that lifestyle recommendations in isolation of integrated mental health services will be successful in treating extremely obese patients.
Interpretation of these findings is limited by the heterogeneity of presenting clinical issues of our sample, and a different perspective may be evident when focusing exclusively on a single presenting obesity co-morbidity, such as those with hypertension alone. There are also differences in diagnostic approaches to the metabolic syndrome, and we used the most common clinical parameters with diagnostic potential via clinical exam and laboratory assay. Moreover, rates of complete data were higher among patients from a Caucasian background, potentially interfering with the representativeness of this sample with our larger patient population. In terms of psychological status, reliance on a self-report and parent-report measure of psychological functioning, instead of a clinical interview tool, also has inherent limitations.26 The SDQ has well-established psychometric properties documented extensively in the literature. We anticipate that the measure had equally solid psychometrics in our sample, but we did not do additional tests of psychometrics.
Further research will help identify the optimal strategies for encouraging lifestyle change and accomplishing weight management. It will be important to further characterize the impact of metabolic syndrome by initiating comparisons between different co-morbidities, rather than the cumulative number of medical issues, and also to assess other co-morbidities, such as sleep apnea. We were not statistically powered for such an analytic approach in the current project. Additionally, subsequent analyses should examine demographic distinctions in an a priori fashion, as suggested by our post hoc findings for gender differences in prosocial impairments.
On the basis of our findings, employing a motivational interviewing stance in the treatment of obesity may resonate more than traditional practice. In a traditional anticipatory guidance approach, providers encourage behavior change based on maximizing perceived risk, such as persuading lifestyle modification by underscoring the hazards associated with obesity co-morbidities.27 In contrast, motivational interviewing features a guiding style, rather than a directive approach, that encourages patients to explore and understand their own intrinsic barriers and incentives to change. Motivational interviewing attempts to minimize resistance, and elicits change stemming from patient/family motivation, rather than provider directive.28 On the basis of our findings, it appears that emphasizing the medical co-morbidities related to obesity in an effort to promote adherence to lifestyle modification recommendations may not correspond to the emotional experience of these adolescents. In contrast, asking about each individual's emotional experience related to their obesity may be a more meaningful launching point to fostering behavior change.
Conclusion
Our findings suggest that extreme obesity, rather than the number of identified obesity-related co-morbidities, is more predictive of psychological difficulties. Youth with extreme obesity may require screening for psychological difficulties, and conjoint behavioral health and medical treatment may be more beneficial than medical treatment alone for accomplishing lifestyle changes and weight loss in this cohort of patients. Additionally, our findings emphasize the importance of recognizing individual differences in motivating factors for accomplishing healthy lifestyle goals. Adolescent patients may be more motivated by the degree of their obesity than the number of emerging co-morbidities, suggesting that a motivational interviewing approach that recognizes intrinsic motivational factors may be well-suited for this group of patients.
Acknowledgments
N.W.A., K.J.N., M.M.K., P.Z., K.B., and A.C. were involved in study design, data collection, data analysis, data interpretation, and manuscript writing. N.W.A., A.C., and K.B. were additionally involved in the literature search. S.E. and S.J.S. were involved in dataset management, data analysis, generation of figures, and interpretation of findings. All authors were involved in writing and revision tasks and approved submission of this manuscript.
This research was supported by the Eagle Riders of the Fraternal Order of Eagles Aerie #3324. This research was also supported, in part, by National Institutes of Health/National Center for Advancing Translational Sciences (NIH/NCATS) Colorado CTSI Grant Number UL1 TR000154. Contents are the authors' sole responsibility and do not necessarily represent official NIH views.
Author Disclosure Statement
No competing financial interests exist.
References
- 1.Lifshitz F. Obesity in children. J Clin Res Pediatr Endocrinol. 2008;1:53–60. doi: 10.4008/jcrpe.v1i2.35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Cook S. Auinger P. Li C, et al. Metabolic syndrome rates in United States adolescents, from the National Health and Nutrition Examination Survey, 1999–2002. J Pediatr. 2008;152:165–170. doi: 10.1016/j.jpeds.2007.06.004. [DOI] [PubMed] [Google Scholar]
- 3.Ford ES. Giles WH. Dietz WH. Prevalence of the metabolic syndrome among US adults: Findings from the third National Health and Nutrition Examination Survey. JAMA. 2002;287:356–359. doi: 10.1001/jama.287.3.356. [DOI] [PubMed] [Google Scholar]
- 4.Executive Summary of The Third Report of The National Cholesterol Education Program (NCEP) Expert Panel on Detection, Evaluation, And Treatment of High Blood Cholesterol In Adults (Adult Treatment Panel III) JAMA. 2001;285:2486–2497. doi: 10.1001/jama.285.19.2486. [DOI] [PubMed] [Google Scholar]
- 5.Grundy SM. Metabolic syndrome: A multiplex cardiovascular risk factor. J Clin Endocrinol Metab. 2007;92:399–404. doi: 10.1210/jc.2006-0513. [DOI] [PubMed] [Google Scholar]
- 6.Goldbacher EM. Matthews KA. Are psychological characteristics related to risk of the metabolic syndrome? A review of the literature. Ann Behav Med. 2007;34:240–252. doi: 10.1007/BF02874549. [DOI] [PubMed] [Google Scholar]
- 7.Vander Wal JS. Mitchell ER. Psychological complications of pediatric obesity. Pediatr Clin North Am. 2011;58:1393–1401. doi: 10.1016/j.pcl.2011.09.008. x. [DOI] [PubMed] [Google Scholar]
- 8.Zeller MH. Roehrig HR. Modi AC, et al. Health-related quality of life and depressive symptoms in adolescents with extreme obesity presenting for bariatric surgery. Pediatrics. 2006;117:1155–1161. doi: 10.1542/peds.2005-1141. [DOI] [PubMed] [Google Scholar]
- 9.Nadeau K. Kolotkin RL. Boex R, et al. Health-related quality of life in adolescents with comorbidities related to obesity. J Adolesc Health. 2011;49:90–92. doi: 10.1016/j.jadohealth.2010.10.005. [DOI] [PubMed] [Google Scholar]
- 10.McCaffery JM. Niaura R. Todaro JF, et al. Depressive symptoms and metabolic risk in adult male twins enrolled in the National Heart, Lung, and Blood Institute twin study. Psychosom Med. 2003;65:490–497. doi: 10.1097/01.psy.0000041545.52924.82. [DOI] [PubMed] [Google Scholar]
- 11.Dunbar JA. Reddy P. Davis-Lameloise N, et al. Depression: An important comorbidity with metabolic syndrome in a general population. Diabetes Care. 2008;31:2368–2373. doi: 10.2337/dc08-0175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson BJ. Edelstein S. Abramson NW, et al. Depressive symptoms and quality of life in adolescents with type 2 diabetes: Baseline data from the TODAY study. Diabetes Care. 2011;34:2205–2207. doi: 10.2337/dc11-0431. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Modi AC. Pai AL. Hommel KA, et al. Pediatric self-management: A framework for research, practice, and policy. Pediatrics. 2012;129:e473–e485. doi: 10.1542/peds.2011-1635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Moreno M. Trainor ME. Adolescence extended: Implications of new brain research on medicine and policy. Acta Paediatr. 2013;102:226–232. doi: 10.1111/apa.12100. [DOI] [PubMed] [Google Scholar]
- 15.Cook S. Weitzman M. Auinger P, et al. Prevalence of a metabolic syndrome phenotype in adolescents: Findings from the third National Health and Nutrition Examination Survey, 1988–1994. Arch Pediatr Adolesc Med. 2003;157:821–827. doi: 10.1001/archpedi.157.8.821. [DOI] [PubMed] [Google Scholar]
- 16.Ice CL. Murphy E. Cottrell L, et al. Morbidly obese diagnosis as an indicator of cardiovascular disease risk in children: Results from the CARDIAC Project. Int J Pediatr Obes. 2011;6:113–119. doi: 10.3109/17477161003792556. [DOI] [PubMed] [Google Scholar]
- 17.Skelton JA. Cook SR. Auinger P, et al. Prevalence and trends of severe obesity among US children and adolescents. Acad Pediatr. 2009;9:322–329. doi: 10.1016/j.acap.2009.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Skinner AC. Mayer ML. Flower K, et al. Using BMI to determine cardiovascular risk in childhood: How do the BMI cutoffs fare? Pediatrics. 2009;124:e905–e912. doi: 10.1542/peds.2009-0179. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Phillips BA. Gaudette S. McCracken A, et al. Psychosocial functioning in children and adolescents with extreme obesity. J Clin Psychol Med Settings. 2012;19:277–284. doi: 10.1007/s10880-011-9293-9. [DOI] [PubMed] [Google Scholar]
- 20.Goodman R. Psychometric properties of the strengths and difficulties questionnaire. J Am Acad Child Adolesc Psychiatry. 2001;40:1337–1345. doi: 10.1097/00004583-200111000-00015. [DOI] [PubMed] [Google Scholar]
- 21.Becker A. Woerner W. Hasselhorn M, et al. Validation of the parent and teacher SDQ in a clinical sample. Eur Child Adolesc Psychiatry. 2004;13(Suppl 2):II11–II16. doi: 10.1007/s00787-004-2003-5. [DOI] [PubMed] [Google Scholar]
- 22.Stone LL. Otten R. Engels RC, et al. Psychometric properties of the parent and teacher versions of the strengths and difficulties questionnaire for 4- to 12-year-olds: A review. Clin Child Fam Psychol Rev. 2010;13:254–274. doi: 10.1007/s10567-010-0071-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Bourdon KH. Goodman R. Rae DS, et al. The Strengths and Difficulties Questionnaire: US normative data and psychometric properties. J Am Acad Child Adolesc Psychiatry. 2005;44:557–564. doi: 10.1097/01.chi.0000159157.57075.c8. [DOI] [PubMed] [Google Scholar]
- 24.The National Health Interview Survey (NHIS) Normative Data Sample. Strengths and Difficulties Questionnaire Centers for Disease Control and Prevention 2001 NHIS Supplement. www.sdqinfo.org/USnorm.html/ Jan 30, 2004. [Mar 30;2012 ]. www.sdqinfo.org/USnorm.html/
- 25.TODAY Study Group. Wilfley D. Berkowitz R. Goebel-Fabbri A, et al. Binge eating, mood, and quality of life in youth with type 2 diabetes: Baseline data from the today study. Diabetes Care. 2011;34:858–860. doi: 10.2337/dc10-1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Logan DE. Claar RL. Scharff L. Social desirability response bias and self-report of psychological distress in pediatric chronic pain patients. Pain. 2008;136:366–372. doi: 10.1016/j.pain.2007.07.015. [DOI] [PubMed] [Google Scholar]
- 27.Resnicow K. Davis R. Rollnick S. Motivational interviewing for pediatric obesity: Conceptual issues and evidence review. J Am Diet Assoc. 2006;106:2024–2033. doi: 10.1016/j.jada.2006.09.015. [DOI] [PubMed] [Google Scholar]
- 28.Armstrong MJ. Mottershead TA. Ronksley PE, et al. Motivational interviewing to improve weight loss in overweight and/or obese patients: A systematic review and meta-analysis of randomized controlled trials. Obes Rev. 2011;12:709–723. doi: 10.1111/j.1467-789X.2011.00892.x. [DOI] [PubMed] [Google Scholar]