Abstract
Background
BMI is often used to evaluate the effectiveness of childhood obesity interventions, but such interventions may have additional benefits independent of effects on adiposity. We investigated whether benefits to health outcomes following the Mind, Exercise, Nutrition…Do It! (MEND) childhood obesity intervention were independent of or associated with changes in zBMI.
Methods
A total of 79 obese children were measured at baseline; 71 and 42 participants were followed-up at 6 and 12 months respectively, and split into four groups depending on magnitude of change in zBMI. Differences between groups for waist circumference, cardiovascular fitness, physical and sedentary activities, and self-esteem were investigated.
Results
Apart from waist circumference and its z-score, there were no differences or trends across zBMI subgroups for any outcome. Independent of the degree of zBMI change, benefits in several parameters were observed in children participating in this obesity intervention.
Conclusion
We concluded that isolating a single parameter like zBMI change and neglecting other important outcomes is restrictive and may undermine the evaluation of childhood obesity intervention effectiveness.
Introduction
Childhood obesity is a serious public health problem adversely affecting children's health.1 Even though there is convergence on the core elements of successful childhood obesity interventions,2–4 there is less consensus about the parameters by which such interventions should be judged as clinically effective. Because childhood obesity affects several body functions and systems, evaluations of interventions should use markers which reflect this diverse range.
Associations between the degree of BMI z-score (zBMI) change and markers of metabolic and cardiovascular health have been used in an attempt to establish thresholds by which an intervention can be claimed as clinically effective.5–8 For example, Ford et al. defined a −0.25 zBMI change as the lowest threshold for achieving clinically significant changes in metabolic health.5
These measures are undoubtedly valuable; however, reliance on a zBMI threshold as a sole measure of an intervention's effectiveness may be too restrictive. The threshold of −0.25 was primarily defined by associations with metabolic health parameters, which although important, represent only one of many body systems affected by obesity. Our aim was to investigate additional benefits associated with different levels of zBMI change in obese children who attended a multicomponent, community-based, childhood obesity intervention.9
Methods
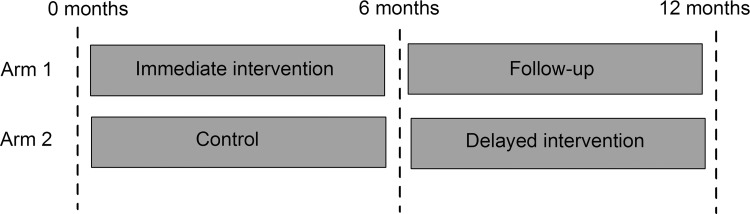
The data presented in this article originated from the Mind, Exercise, Nutrition…Do It! (MEND) randomized controlled trial (RCT) and was approved by the Metropolitan Multi-Centre Research Ethics Committee (Current Controlled Trials ISRCTN 30238779). Consent and assent forms (for parents and children respectively) were signed by researchers and families to confirm trial entry. This family-based intervention consisted of the 9-week MEND program followed by provision of a 12-week free family swim pass. The program consisted of twice-weekly group sessions, including nutrition education, behavior modification, and fun-based physical activity. The intervention took place at five different sites (four urban, one rural) and was delivered to children and their parents by separate teams of health and exercise professionals. The methods and results of the original RCT have been published elsewhere.9 In this study, we only present data from groups when they both served as intervention (i.e., no control data). Therefore, 12-month data were only available for half the sample (Fig. 1).
Figure 1.
Randomized controlled trial (RCT) study design.
Participants
For this study, analyses were carried out on two subsamples of children. The first subsample consisted of a group of 71 participants from both arms of the original RCT who completed the 6-month intervention (Fig. 1). The second subsample was a group of 42 participants from arm 1 only, who were assessed at 12 months (6 months following the intervention). The delayed-intervention design of the original RCT meant that only participants who initially received the intervention (arm 1 or immediate intervention group) were assessed at 12 months (Fig. 1). The analyses were performed using available data, discarding records with missing measurements.
Data from 79 obese MEND participants [BMI ≥98th percentile,10 mean zBMI 2.75 standard deviation (SD) 0.56] from both groups were used in the analysis. Mean age at baseline was 10.3 years (SD 1.3 years) and 49 participants (62%) were female. Thirty-eight participants (48%) were from minority ethnic groups, 13 (16%) were from low socioeconomic status families, and 20 (25%) were from households where the primary earner was unemployed.
Outcome Measures
Anthropometry (weight, height, BMI, waist circumference), cardiovascular fitness (blood pressure, recovery heart rate following a step test), physical activity, sedentary behaviors, and self-esteem were measured at baseline, 6 and 12 months. Detailed information on the methodology used has been published elsewhere.9
Statistical Analysis
Differences in outcomes after 6 and 12 months from baseline were investigated using a t-test.
Participants were split into four subgroups on the basis of their change in zBMI:
Group A: Participants with an increase in zBMI of >0;
Group B: Participants with a decrease in zBMI of ≥0 to <0.25;
Group C: Participants with a decrease in zBMI of ≥0.25 to <0.5;
Group D: Participants with a decrease in zBMI of ≥0.5.
For all zBMI subgroups and for each outcome variable, preintervention levels and changes between ‘initial’ and ‘final’ measurements were summarized as means and standard errors (Tables 1 and 2).
Table 1.
Change in BMI, Waist Circumference, Blood Pressure, Fitness, Activity, and Self-Esteem with zBMI Change over 6 Months
| |
Change in BMI z-score over 6 months |
|
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| |
Increased |
zBMI decrease >0 to <0.25 |
zBMI decrease ≥0.25 to <0.5 |
zBMI decrease ≥0.5 |
|
|
||||
| |
(n=9) |
(n=29) |
(n=17) |
(n=16) |
|
|
||||
| na | Mean | (SE) | Mean | (SE) | Mean | (SE) | Mean | (SE) | Group comparisonb | Test of linear trendc |
| BMI (kg/m2) | ||||||||||
| Initial mean | 28.6 | (2.6) | 27.2 | (0.7) | 26.3 | (0.6) | 25.9 | (0.9) | 0.5 | |
| Mean change | 1.4 | (0.3) | −0.3 | (0.1) | −1.6 | (0.1) | −3.0 | (0.2) | <0.001 by design | <0.001 by design |
| BMI z-score | ||||||||||
| Initial mean | 2.81 | (0.28) | 2.76 | (0.11) | 2.60 | (0.11) | 2.65 | (0.13) | 0.7 | |
| Mean change | 0.08 | (0.02) | −0.14 | (0.02) | −0.37 | (0.02) | −0.71 | (0.05) | <0.001 by design | <0.001 by design |
| Waist circumference (cm) | ||||||||||
| Initial mean | 80.4 | (3.6) | 82.0 | (1.4) | 80.3 | (1.5) | 79.4 | (1.9) | 0.7 | |
| Mean change | −2.4 | (0.8) | −2.5 | (0.5) | −4.9 | (0.7) | −7.8 | (0.7) | <0.001 | <0.001 |
| Waist circumference z-score | ||||||||||
| Initial mean | 2.79 | (0.24) | 2.93 | (0.09) | 2.70 | (0.12) | 2.75 | (0.13) | 0.7 | |
| Mean change | −0.29 | (0.07) | −0.31 | (0.04) | −0.55 | (0.08) | −0.82 | (0.06) | <0.001 | <0.001 |
| Systolic blood pressure (mmHg) | ||||||||||
| Initial mean | 117.2 | (4.3) | 116.6 | (2.7) | 116.9 | (2.6) | 116.5 | (3.2) | 0.7 | |
| Mean change | −4.6 | (2.7) | −5.7 | (2.5) | −3.2 | (2.7) | −6.0 | (3.0) | 0.9 | 0.4 |
| Diastolic blood pressure (mmHg) | ||||||||||
| Initial mean | 66.9 | (3.0) | 66.1 | (1.8) | 65.3 | (1.9) | 62.9 | (1.8) | 0.6 | |
| Mean change | −5.3 | (3.8) | −3.9 | (2.1) | −2.2 | (1.7) | −6.7 | (1.9) | 0.6 | 0.7 |
| Recovery heart rate (beats/minute) | ||||||||||
| Initial mean | 125 | (12) | 111 | (4) | 115 | (6) | 107 | (6) | 0.99 | |
| Mean change | −28 | (13) | −13 | (5) | −19 | (5) | −21 | (7) | 0.5 | >0.9 |
| Physical activity (hours/week) | ||||||||||
| Initial mean | 8.8 | (1.8) | 7.8 | (1.0) | 11.4 | (1.6) | 8.1 | (0.9) | 0.2 | |
| Mean change | 1.3 | (2.1) | 5.1 | (1.5) | 2.4 | (2.3) | 6.2 | (1.8) | 0.4 | 0.12 |
| Sedentary activity (hours/week) | ||||||||||
| Initial mean | 20.6 | (2.4) | 22.9 | (1.5) | 17.1 | (1.8) | 20.3 | (2.2) | 0.9 | |
| Mean change | −8.7 | (2.2) | −4.9 | (1.8) | −2.7 | (1.8) | −4.8 | (1.7) | 0.4 | 0.3 |
| Global self-esteem score (range 0–4) | ||||||||||
| Initial mean | 2.8 | (0.3) | 2.8 | (0.2) | 3.2 | (0.1) | 3.0 | (0.1) | 0.7 | |
| Mean change | 0.1 | (0.3) | 0.3 | (0.1) | 0.2 | (0.2) | 0.3 | (0.2) | 0.8 | >0.9 |
n=maximum number of participants per subgroup.
p value obtained from analysis of variance (ANOVA.).
p value obtained from linear regression model fitting zBMI change as continuous explanatory variable and adjusting for randomization group.
SE, standard error.
Table 2.
Change in BMI, Waist Circumference, Blood Pressure, Fitness, Activity, and Self-Esteem with zBMI Change over 12 Months
| |
Change in BMI z-score over 12 months |
|
|
|||||||
|---|---|---|---|---|---|---|---|---|---|---|
| |
Increased |
zBMI decrease >0 to <0.25 |
zBMI decrease ≥0.25 to <0.5 |
zBMI decrease ≥0.5 |
|
|
||||
| |
(n=9) |
(n=18) |
(n=8) |
(n=7) |
|
|
||||
| na | Mean | (SE) | Mean | (SE) | Mean | (SE) | Mean | (SE) | Group comparisonb | Test of linear trendc |
| BMI (kg/m2) | ||||||||||
| Initial mean | 27.5 | (1.4) | 27.4 | (0.8) | 27.4 | (0.9) | 26.4 | (0.6) | 0.9 | |
| Mean change | 1.9 | (0.2) | 0.4 | (0.1) | −0.9 | (0.2) | −3.1 | (0.4) | <0.001 by design | <0.001 by design |
| BMI z-score | ||||||||||
| Initial mean | 2.71 | (0.18) | 2.82 | (0.11) | 3.01 | (0.17) | 2.75 | (0.07) | 0.6 | |
| Mean change | 0.11 | (0.03) | −0.11 | (0.01) | −0.37 | (0.02) | −0.81 | (0.08) | <0.001 by design | <0.001 by design |
| Waist circumference (cm) | ||||||||||
| Initial mean | 81.4 | (2.0) | 83.8 | (2.2) | 80.6 | (2.0) | 80.1 | (2.5) | 0.6 | |
| Mean change | −1.6 | (1.1) | −2.2 | (1.1) | −2.7 | (1.7) | −7.9 | (1.3) | 0.02 | <0.001 |
| Waist circumference z-score | ||||||||||
| Initial mean | 2.89 | (0.12) | 2.99 | (0.12) | 3.08 | (0.14) | 2.86 | (0.16) | 0.7 | |
| Mean change | −0.29 | (0.08) | −0.36 | (0.07) | −0.56 | (0.11) | −0.92 | (0.15) | 0.001 | <0.001 |
| Systolic blood pressure (mmHg) | ||||||||||
| Initial mean | 117.7 | (4.5) | 120.9 | (3.3) | 126.3 | (6.5) | 121.5 | (5.8) | 0.7 | |
| Mean change | −9.3 | (3.4) | −2.7 | (3.5) | −5.7 | (3.9) | −12.9 | (6.2) | 0.3 | 0.2 |
| Diastolic blood pressure (mmHg) | ||||||||||
| Initial mean | 63.7 | (3.9) | 66.3 | (1.9) | 69.3 | (3.2) | 63.8 | (2.5) | 0.6 | |
| Mean change | −6.6 | (4.9) | 0.3 | (1.9) | −3.8 | (2.7) | −2.6 | (3.2) | 0.4 | >0.9 |
| Recovery heart rate (beats/minute) | ||||||||||
| Initial mean | 111 | (8) | 115 | (8) | 115 | (6) | 115 | (12) | 0.9 | |
| Mean change | −12 | (10) | −14 | (8) | 1 | (5) | −22 | (11) | 0.5 | 0.5 |
| Physical activity (hours/week) | ||||||||||
| Initial mean | 5.2 | (0.8) | 8.6 | (1.1) | 7.8 | (1.6) | 6.3 | (1.2) | 0.2 | |
| Mean change | 3.2 | (1.6) | 3.7 | (2.0) | 3.9 | (1.3) | 6.1 | (1.6) | 0.9 | 0.5 |
| Sedentary activity (hours/week) | ||||||||||
| Initial mean | 21.1 | (3.1) | 21.2 | (1.8) | 18.8 | (2.6) | 21.0 | (4.2) | 0.9 | |
| Mean change | −1.4 | (4.1) | −1.5 | (1.2) | −1.6 | (1.1) | −4.3 | (3.4) | 0.9 | 0.8 |
| Global self-esteem score (range 0–4) | ||||||||||
| Initial mean | 2.9 | (0.3) | 2.7 | (0.2) | 2.7 | (0.3) | 3.1 | (0.2) | 0.7 | |
| Mean change | 0.3 | (0.3) | 0.4 | (0.2) | −0.1 | (0.3) | 0.5 | (0.2) | 0.5 | 0.6 |
n=maximum number of participants per subgroup.
p value obtained from analysis of variance (ANOVA) test.
p value obtained from linear regression model fitting zBMI change as continuous explanatory variable.
SE, standard error.
Differences in outcomes across the four zBMI subgroups were investigated at two time points—at 6 and 12 months from baseline. For each of the two time points, analysis of variance (ANOVA) was performed to investigate whether there were significant differences in the ‘initial’ means and the mean change in outcomes, across the four zBMI subgroups.
A test of linear trend in the change of outcome variables after baseline using linear regression was performed at 6 and at 12 months postintervention to assess whether zBMI change as a continuous variable predicted outcome change. The assumptions of normality and homogeneity were assessed post hoc looking at QQ plots of the residuals of the fitted models. Statistical significance was set at p<0.05 two-tailed. All analyses were conducted using SPSS 18.0 for Windows (SPSS, Chicago, IL).
Results
The initial mean and mean changes 6 and 12 months after baseline for these subgroups are shown in Tables 1 and 2, respectively. Waist circumference and its z-score over 6 and 12 months showed significant differences between the four zBMI subgroups and positive linear trends between reduction and zBMI loss (Tables 1 and 2). However, for the remaining variables, there were no statistically significant differences or trends across the zBMI subgroups at 6 or 12 months from baseline (Tables 1 and 2).
Discussion
In this study, the benefits of a childhood obesity intervention on cardiovascular fitness, physical activity, sedentary activities, and self-esteem over 6 and 12 months did not differ according to the degree of zBMI reduction. Notably, even children who increased their zBMI showed improvement in the majority of outcomes (Tables 1 and 2). The only parameters associated with the degree of zBMI reduction were waist circumference and its z-score. This was an expected finding because BMI and waist circumference are correlated,11 both being measures of body composition. Overall, the results suggest that regardless of the magnitude and direction of change in zBMI, the intervention had beneficial effects on important health outcomes.
These results are supported by previous studies. More precisely, a 3-month physical activity intervention in obese prepubertal children has been shown to improve blood pressure at 6 months, regardless of body weight or fat reduction.12 Another intervention targeting obese children did not have a significant effect on zBMI, but resulted in significant improvements in objectively measured physical activity and sedentary behaviours.13 Nowicka et al.14 found positive effects on self-esteem of 6- to 17-year-old obese children who attended a low-intensity family therapy intervention and achieved a mean zBMI change of −0.12. The authors stated that the beneficial effect on self-esteem was not correlated with the degree of zBMI reduction. Hence, in line with findings from this study, Nowicka et al. found that psychological status was positively affected by the intervention, regardless of the degree in zBMI change.
Undoubtedly, there is evidence supporting the notion that zBMI reduction is associated with metabolic benefits that have important positive effects on children's health.5–8 A few studies have tried to quantify the magnitude of zBMI reduction required to positively influence obese children's metabolic health.5,6,8 Reinehr et al.7 published results suggesting that a 0.5 reduction in zBMI was required for improved metabolic health 1 year after an obesity intervention. Ford et al.5 subsequently examined the effects of different levels of zBMI reduction in obese children on several cardiovascular disease risk factors. They showed that metabolic benefits were seen with a zBMI reduction of 0.25 units, therefore suggesting this as the minimum for metabolic benefits.5
Despite these interesting findings, research in this area is still inconclusive. Other studies have shown similar metabolic benefits, with smaller reductions in zBMI. The Kolsgaard et al. family intervention study15 reported improvements in lipid profile and insulin resistance, even though the average zBMI reduction was only −0.13. In a similar study by Kirk et al.,16 a significant percentage of children with abnormal values for lipid and glucose metabolism indicators moved to normal while experiencing only a modest reduction in zBMI (−0.15). Pedrosa et al.17 showed that a 1-year intervention for overweight and obese prepubertal children reduced zBMI modestly (−0.18), yet improved metabolic syndrome indicators. Similar benefits in lipid profile and insulin resistance indicators such as glucose and insulin levels and homeostasis model assessment (HOMA) have also been reported with only moderate or no decrease in zBMI.15,18,19
Therefore, it seems premature to recommend zBMI thresholds to define intervention effectiveness, especially in the light of several studies suggesting that improvements in glucose and lipid profile and positive metabolic effects can be achieved with smaller reductions or even maintenance of zBMI.12–18
A strength of the current study was the variety of outcomes used to assess intervention effectiveness. Moreover, the intervention design fulfilled the prerequisites of a successful childhood obesity program.2–4 One limitation was that the study was not originally powered to detect differences in outcomes according to different levels of zBMI change. However, there was sufficient power to show the trend for waist circumference and its z-score. A related limitation was that, due to loss of follow-up data, the number of participants per group was in some cases small. Lastly, the lack of dietary data in the present study was also a limitation, while blood sample collection was not part of the study design and physical activity level was assessed using a nonvalidated tool.
It should also be acknowledged that another important reason behind the variation in zBMI between studies and its association with outcomes is the use of different growth charts; for example, in the current study the British growth charts were used,10 whereas in US studies CDC growth charts are implemented.20 When available, country-specific growth charts are used in national studies because they provide better comparisons of the study population with the country's general population. As growth charts differ in construction methodology, sample size, and sample characteristics, direct comparisons of zBMI changes between studies using different charts is inherently problematic. Equivalent changes in absolute BMI do not equate to equivalent changes in zBMI between charts. Additionally, the age and severity of obesity of the sample affects interpretation of the magnitude of zBMI change. Within charts, zBMI scales attenuate absolute BMI change,21 such that children with higher baseline zBMI require greater changes in absolute BMI to produce equivalent changes in zBMI. This issue is particularly pronounced in the CDC growth charts due to the Box–Cox transformation used to account for skewness.22,23 These limitations further support the premise that caution must be used in using zBMI to determine the clinical effectiveness of an obesity intervention.
Conclusion
In conclusion, our findings indicate that benefits in several important parameters of health occurred in children participating in this obesity intervention, regardless of the degree of zBMI change. On the basis of these results, it is apparent that setting a zBMI reduction cutoff to assess the effectiveness of childhood obesity interventions can be misleading, considering the value of other outcomes that may improve in the absence of zBMI change. We cannot yet be certain of the best outcomes to assess such interventions' effectiveness,24,25 and focusing on a single outcome such as zBMI is premature.
Acknowledgments
The MEND research team would like to thank all the children and parents who participated in this trial.
Author Disclosure Statement
Maria Kolotourou is employed part-time at Mytime MEND. Dr. Duncan Radley is employed full-time at Mytime MEND. Dr. Lindsey Smith was employed full-time at MEND at the time of preparation of this publication. Dr. Paul Chadwick is currently a part-time consultant at Mytime MEND. Dr. Venediktos Kapetanakis serves as a consultant statistician at Mytime MEND. Stavros Orfanos, Professor Tim Cole and Professor Atul Singhal have no conflicts of interest. Dr. Paul Sacher is currently employed as a Senior Research Fellow at the UCL Institute of Child Health as well as Consultant Chief Research and Development Officer at Mytime MEND.
Financial and nonfinancial support (e.g., staff and venues) were provided by the following UK organizations: National Institute for Health Research, Sainsbury's Supermarkets Ltd., Bromley Mytime, Bromley Primary Care Trust (PCT), Great Ormond Street Hospital for Children NHS Trust, London Borough of Lewisham, MEND Central Ltd, New Cross Gate New Deal for Communities, Parkwood Leisure, Southwark PCT, The Lewisham Hospital NHS Trust, UCL Institute of Child Health, and Waveney PCT. Tim Cole was funded by MRC grant G0700961.
References
- 1.Abrams P. Levitt Katz LE. Metabolic effects of obesity causing disease in childhood. Curr Opin Endocrinol Diabetes Obes. 2010;18:23–27. doi: 10.1097/MED.0b013e3283424b37. [DOI] [PubMed] [Google Scholar]
- 2.Scottish Intercollegiate Guidelines Network. Management of Obesity: A national clinical guideline. 2011. www.sign.ac.uk/pdf/sign115.pdf. [Jun 1;2013 ]. www.sign.ac.uk/pdf/sign115.pdf
- 3.National Institute for Health and Clinical Excellence (NICE) Obesity. The prevention, identification, assessment, management of overweight, obesity in adults, children. 2006. www.nice.org.uk/cg43. [Jun 1;2013 ]. www.nice.org.uk/cg43 [PubMed]
- 4.American Dietetic Association. Position of the American Dietetic Association: Individual-, family-, school-, and community-based interventions for pediatric overweight. J Am Diet Assoc. 2006;106:925–945. doi: 10.1016/j.jada.2006.03.001. [DOI] [PubMed] [Google Scholar]
- 5.Ford AL. Hunt LP. Cooper A, et al. What reduction in BMI SDS is required in obese adolescents to improve body composition and cardiometabolic health? Arch Dis Child. 2010;95:256–261. doi: 10.1136/adc.2009.165340. [DOI] [PubMed] [Google Scholar]
- 6.Hunt LP. Ford A. Sabin MA, et al. Clinical measures of adiposity and percentage fat loss: Which measure most accurately reflects fat loss and what should we aim for? Arch Dis Child. 2007;92:399–403. doi: 10.1136/adc.2006.103986. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Reinehr T. Andler W. Changes in the atherogenic risk factor profile according to degree of weight loss. Arch Dis Child. 2004;89:419–422. doi: 10.1136/adc.2003.028803. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Reinehr T. de Sousa G. Toschke AM, et al. Long-term follow-up of cardiovascular disease risk factors in children after an obesity intervention. Am J Clin Nutr. 2006;84:490–496. doi: 10.1093/ajcn/84.3.490. [DOI] [PubMed] [Google Scholar]
- 9.Sacher PM. Kolotourou M. Chadwick PM, et al. Randomized controlled trial of the MEND program: A family-based community intervention for childhood obesity. Obesity. 2010;18(Suppl 1):S62–S68. doi: 10.1038/oby.2009.433. [DOI] [PubMed] [Google Scholar]
- 10.Cole TJ. Freeman JV. Preece MA. Body mass index reference curves for the UK, 1990. Arch Dis Child. 1995;73:25–29. doi: 10.1136/adc.73.1.25. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Rudolf MC. Greenwood DC. Cole TJ, et al. Rising obesity and expanding waistlines in schoolchildren: A cohort study. Arch Dis Child. 2004;89:235–237. doi: 10.1136/adc.2002.020552. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Farpour-Lambert NJ. Aggoun Y. Marchand LM, et al. Physical activity reduces systemic blood pressure and improves early markers of atherosclerosis in pre-pubertal obese children. J Am Coll Cardiol. 2009;54:2396–2406. doi: 10.1016/j.jacc.2009.08.030. [DOI] [PubMed] [Google Scholar]
- 13.Hughes AR. Stewart L. Chapple J, et al. Randomized, controlled trial of a best-practice individualized behavioral program for treatment of childhood overweight: Scottish Childhood Overweight Treatment Trial (SCOTT) Pediatrics. 2008;121:e539–e546. doi: 10.1542/peds.2007-1786. [DOI] [PubMed] [Google Scholar]
- 14.Nowicka P. Pietrobelli A. Flodmark CE. Low-intensity family therapy intervention is useful in a clinical setting to treat obese and extremely obese children. Int J Pediatr Obes. 2007;2:211–217. doi: 10.1080/17477160701379810. [DOI] [PubMed] [Google Scholar]
- 15.Kolsgaard ML. Joner G. Brunborg C, et al. Reduction in BMI z-score and improvement in cardiometabolic risk factors in obese children and adolescents. The Oslo Adiposity Intervention Study—a hospital/public health nurse combined treatment. BMC Pediatr. 2011;11:47. doi: 10.1186/1471-2431-11-47. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Kirk S. Zeller M. Claytor R, et al. The relationship of health outcomes to improvement in BMI in children and adolescents. Obes Res. 2005;13:876–882. doi: 10.1038/oby.2005.101. [DOI] [PubMed] [Google Scholar]
- 17.Pedrosa C. Oliveira BM. Albuquerque I, et al. Markers of metabolic syndrome in obese children before and after 1-year lifestyle intervention program. Eur J Nutr. 2011;50:391–400. doi: 10.1007/s00394-010-0148-1. [DOI] [PubMed] [Google Scholar]
- 18.Cummings DM. Henes S. Kolasa KM, et al. Insulin resistance status: Predicting weight response in overweight children. Arch Pediatr Adolesc Med. 2008;162:764–768. doi: 10.1001/archpedi.162.8.764. [DOI] [PubMed] [Google Scholar]
- 19.Tompkins CL. Moran K. Preedom S, et al. Physical activity-induced improvements in markers of insulin resistance in overweight and obese children and adolescents. Curr Diabetes Rev. 2011;7:164–170. doi: 10.2174/157339911795843096. [DOI] [PubMed] [Google Scholar]
- 20.Kuczmarski R. Ogden C. Guo S. 2000 CDC Growth Charts for the United States: Methods and development. National Center for Health Statistics. Vital Health Stat. 2002:11. [PubMed] [Google Scholar]
- 21.Cole TJ. Faith MS. Pietrobelli A, et al. What is the best measure of adiposity change in growing children: BMI, BMI %, BMI z-score or BMI centile? Eur J Clin Nutr. 2005;59:419–425. doi: 10.1038/sj.ejcn.1602090. [DOI] [PubMed] [Google Scholar]
- 22.Flegal KM. Ogden CL. Wei R, et al. Prevalence of overweight in US children: Comparison of US growth charts from the Centers for Disease Control and Prevention with other reference values for body mass index. Am J Clin Nutr. 2001;73:1086–1093. doi: 10.1093/ajcn/73.6.1086. [DOI] [PubMed] [Google Scholar]
- 23.Flegal KM. Wei R. Ogden CL, et al. Characterizing extreme values of body mass index-for-age by using the 2000 Centers for Disease Control and Prevention growth charts. Am J Clin Nutr. 2009;90:1314–1320. doi: 10.3945/ajcn.2009.28335. [DOI] [PubMed] [Google Scholar]
- 24.Klesges LM. Williams NA. Davis KS, et al. External validity reporting in behavioral treatment of childhood obesity: A systematic review. Am J Prev Med. 2012;42:185–192. doi: 10.1016/j.amepre.2011.10.014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Oude Luttikhuis H. Baur L. Jansen H, et al. Interventions for treating obesity in children. Cochrane Database Syst Rev. 2009:CD001872. doi: 10.1002/14651858.CD001872.pub2. [DOI] [PubMed] [Google Scholar]