Abstract
Introduction:
Abnormal morphologic findings in imaging were thought to explain the etiology of low back pain (LBP). However, it is now known that variety of morphologic abnormalities is noted even in asymptomatic individuals. Single photon emission computed tomography/computed tomography (SPECT/CT) could be used to differentiate incidental findings from clinically significant findings.
Objective:
This study was performed to define the SPECT/CT patterns in patients with LBP and to correlate these with clinical and magnetic resonance imaging (MRI) findings.
Materials and Methods:
Thirty adult patients with LBP of duration 3 months or more were prospectively evaluated in this study. Patients with known or suspected malignancy, trauma or infectious processes were excluded. A detailed history of sensory and motor symptoms and neurologic examination was performed. All the patients were subjected to MRI and bone scintigraphy with hybrid SPECT/CT of the lumbo-sacral spine within 1 month of each other. The patients were classified into those with and without neurologic symptoms, activity limitation. The findings of clinical examination and imaging were compared. MRI and SPECT/CT findings were also compared.
Results:
Thirty patients (18 men and 12 women; mean age 38 years; range 17-64 years) were eligible for the study. Clinically, 14 of 30 (46%) had neurologic signs and or symptoms. Six of the 30 patients (20%) had positive straight leg raising test (SLRT). Twenty-two of the 30 patients (73%) had SPECT abnormality. Most frequent SPECT/CT abnormality was tracer uptake in the anterior part of vertebral body with osteophytes/sclerotic changes. Significant positive agreement was noted between this finding and MRI evidence of degenerative disc disease. Only 13% of patients had more than one abnormality in SPECT. All 30 patients had MRI abnormalities. The most frequent abnormality was degenerative disc disease and facet joint arthropathy. MRI showed single intervertebral disc abnormality in 36% of the patients and more than one intervertebral disc abnormality in remaining 64% patients. Fifteen of the 30 patients had facet joint arthropathy. 60% of these patients had involvement of more than one level facet joints while 38% had associated inter vertebral disc disease. 83% of the patients with positive SLRT had SPECT and MRI abnormalities. 100% of patients with neurologic symptoms had SPECT and MRI abnormalities.
Conclusion:
Addition of hybrid SPECT/CT data will help differentiate incidental from significant MRI abnormalities as all patients with LBP have MRI abnormalities and most have MRI abnormalities at multiple sites. Tracer uptake in the anterior part of the vertebral body represents degenerative disc disease. MRI is sensitive and SPECT/CT is specific for facet joint arthropathy. Both investigations are best used complementary to each other.
Keywords: Bone scan, low back pain, magnetic resonance imaging, single photon emission computed tomography/computed tomography, straight leg raising test
INTRODUCTION
Almost 80 percent of adults suffer from low back pain (LBP) during some period in their life with the peak prevalence during fifth decade.[1] There are many potential risk factors/indicators.[2] Experimental studies have shown that almost all lumbar structures are capable of producing pain.[3,4] Abnormal morphological findings of the lumbar structures (in particular bones, joints, discs, and muscles) on conventional imaging modalities have often been assumed to be the cause LBP.[5] However, several of such abnormalities have been shown to exist even in asymptomatic individuals.[6] Plain radiography has been relatively insensitive in evaluation. Computed tomography (CT) is extremely good for disorders of bone.
Recent introduction of hybrid single photon emission computed tomography/CT (SPECT/CT) imaging has allowed assessment of both morphology and function in a single study. The morphological information provided by CT scan can also help in providing additional information regarding the etiology of LBP.
Magnetic resonance imaging (MRI) is a non-invasive investigation that is not associated with exposure to ionizing radiation. MRI provides excellent soft-tissue resolution and has become a routine investigation in evaluation of patients with LBP due to its ability to clearly define neurologic and disc degenerative diseases. However, since all of these are based on morphological characters, they are unable to differentiate between incidental and relevant changes. SPECT/CT could potentially be used complimentary to MRI to differentiate incidental from clinically relevant findings.
The purpose of this study was to define the patterns of scintigraphic abnormalities in patients with LBP and to correlate the findings with clinical and MRI findings.
MATERIALS AND METHODS
A prospective study was conducted in 30 consecutive patients fulfilling the eligibility criteria of the study, after obtaining ethical clearance from the institutional Ethics Committee. All subjects were recruited in this study after obtaining written informed consent. Patients having LBP duration of at least 3 months were eligible to be included into the study. Pregnant females, history of previous spinal surgery, suspected or proven spinal tuberculosis, recent trauma, severe medical or surgical illness or psychiatric disorder and patients with diagnosed and/or treated malignancy were excluded from the study. Detailed clinical histories of the symptoms including the onset, progression, nature of the pain, aggravating and relieving factors were noted. History of previous infection, trauma was noted. A thorough physical examination was performed which included inspection and palpation of the lumbo-sacral spine. Patients suspected of connective tissue disorders were subjected to special investigations like C-reactive protein (CRP) assay and human leukocyte antigen (HLA)-B27 assays.
Bone scintigraphy
Three phase bone scintigraphy was performed in every patient. Hybrid SPECT/CT (Infinia Hawkeye 4, GE healthcare, Milwaukee, USA) images of the lumbo-sacral spine including the hips were acquired in all the patients. SPECT images were acquired in 64 × 64 matrix, in a step and shoot method covering 360° in 60 views and 30 s per view. Following the SPECT acquisition, CT was acquired in helical mode and tube current of 2.5 mA covering the lumbo-sacral spine. Three phase scintigraphy and hybrid SPECT/CT images were transferred to Xeleris workstation and examined by evaluating the individual SPECT images, CT images and the fused SPECT/CT images. The sites of increased tracer uptake, localization to the anatomical structures and the corresponding morphological changes in the anatomical structure were also recorded. Abnormalities found on CT images without corresponding changes in SPECT images were also recorded. Patterns of scintigraphic, radiographic, and MRI abnormalities were tabulated. Correlation between clinical symptoms and imaging findings were made.
Magnetic resonance imaging
Patients underwent MRI within 1 month of bone scan. MRI was performed on a 1.5 tesla whole-body scanner (VISION, Siemens AG, Erlangen, Germany). The following MRI parameters were used. All sagittal images had a field of view (FOV) of 320 mm with a slice thickness of 4 mm. Sagittal T1-weighted images [Repetition time (TR), 600 ms; Echo time (TE), 15 ms], with and without fat saturation (TR, 600 ms; TE, 15 ms) before and after Gadolinium diethylene triamine pentaacetic acid (Gd-DTPA) administration (0.1 mmol/kg body weight), sagittal T2-weighted images (TR, 4000 ms; TE, 90 ms), sagittal STIR (short T1 inversion recovery) images (TR, 4200 ms; TE, 70 ms; TI, 150 ms). All axial images had a FOV of 350 mm with a 4-mm-slice thickness to see the whole paravertebral area. Axial T1-weighted images (TR, 600 ms; TE, 15 ms) after contrast administration were acquired. A matrix of 224 × 256 for axial and 330 × 512 for sagittal were used. For interpretation of MRI images, patients were divided into those with or without neurologic symptoms/signs based on the clinical evaluation. Patients were also divided into two groups based on straight leg raising test (SLRT). MRI was examined for curvature of the lumbar spine and presence of osteophytes. Presence of degenerative changes in the intervertebral disc was characterized by a decreased signal in the disc on the T2 weighted images. Presence of disc bulge/protrusion was also noted. Facet joint arthropathy was said to be present in the presence of any of the following findings: Joint space effusion, bony hypertrophy of facet joint, hypertrophy with associated loss of marrow signals. Foraminal stenosis was evaluated and diagnosed when epidural fat was obliterated by disc material of intermediate signal intensity or by osseous material of low signal intensity.
RESULTS
Thirty patients (18 men and 12 women) with chronic LBP were included in the study. The mean age of the patients was 38 years (range 17-64 years). The average duration of LBP was 1.3 years (range 3 months to 4 years).
Clinical characteristics of back pain
All the patients described their pain as constant dull aching type. Walking aggravated the pain in 29 patients. Rest caused significant relief of pain 24 patients. Six patients required medications to control their back pain. Majority of the patients had pain in the region of lower lumbar vertebrae (L4/L5 region) and sacrum. Only one patient had pain in the region of L1 vertebra. Seventeen patients had no radiation of the pain to the lower limbs. Pain was radiating in nature in 13 patients (7 to legs, 5 to thighs and to pubic region in 1 patient). Eight patients had sensory symptoms like paraesthesia in the region of distribution of pain. One patient had motor weakness. Six patients had positive SLRT. Rest of the study group had a negative SLRT.
Enzyme sedimentation rate (ESR) was elevated in five patients. Average ESR value was 27.4 mm Hg/1 h (Range 18-40 mmHg/h). These patients were then subjected to HLA-B27 study. Three were positive for HLA-B27. The visual analogue scale pain scores of these patients and their correlation with activity limitation were also evaluated.
Bone scintigraphy findings
Three phase bone scintigraphy
Three phase bone scintigraphic findings were evaluated qualitatively. It was entirely normal in 9/30 patients while 21 patients had an abnormality on three phase bone scan.
SPECT
SPECT findings confirmed the presence of the abnormalites present in 3 phase bone scan in all the patients. Additionaly SPECT lead to better localisation of the lesions. SPECT also identified unidentified lesions in three patients with normal planar study and also enabled exact localisation of the tracer uptake to the parts of vertebra.
Hybrid SPECT/CT
Fusion of SPECT data with CT data improved the anatomical localization of the abnormal foci detected on SPECT. Further, corresponding morphologic changes like osteophytes, sclerotic changes and vacuum phenomenon enabled correct lesion characterization and improved the confidence of interpretation. Figure 1 shows active facet joint arthropathy on SPECT/CT in a patient with chronic low back pain while Figure 2 depicts SPECT/CT findings in degenerative disc disease.
Figure 1.
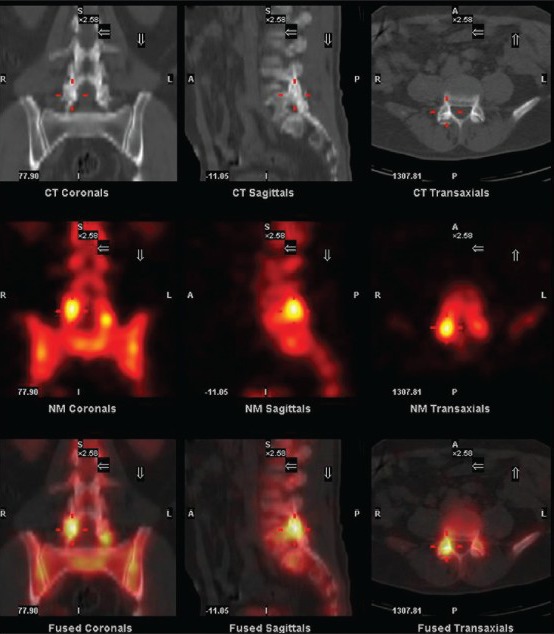
Tc99m single photon emission computed tomography/computed tomography in a patient with chronic low back pain showing pattern of active facet joint arthropathy. Focus of intense tracer activity is noted in the facet joint between L4 and L5 vertebrae
Figure 2.
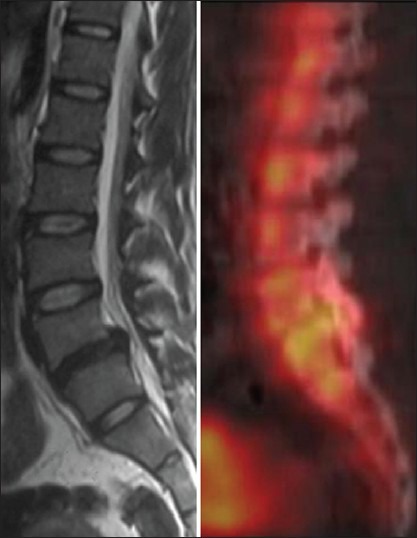
MRI and SPECT/CT findings in a patient with chronic low back pain. MRI image shows thecal indentation in L4/L5 region. Increased tracer activity is noticed in the corresponding site on SPECT/CT imaging
MRI findings
All 30 patients had some identifiable MR abnormalities in the lumbo-sacral region. Summary of CT and MRI findings are tabulated in Tables 1 and 2. All the facet joints were morphologically normal in 15 patients. In three, a single facet joint was involved. In six, two facet joints were involved. In nine patients multiple level facet joints were involved. Single intervertebral disc was diseased in eight of 22 patients. Others had disc disease involving more than one intervertebral disc.
Table 1.
Computed tomography and magnetic resonance imaging findings in all the study group patients. Some patients had more than one finding
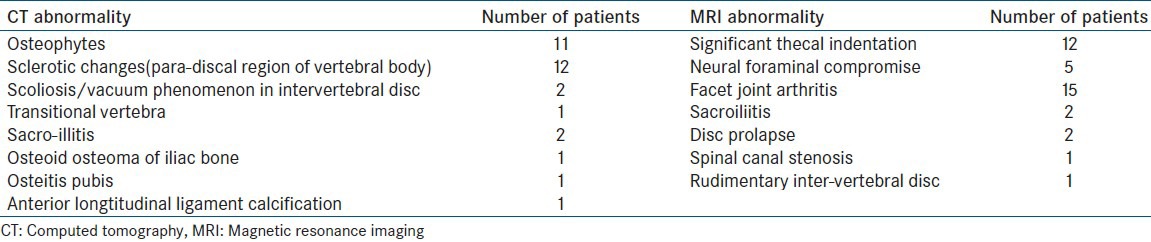
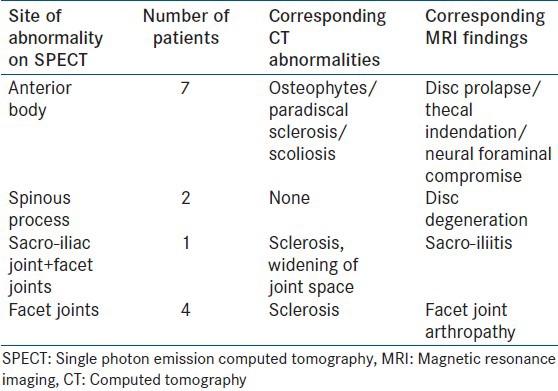
Table 2.
Comparison of sites of involvement on single photon computed tomography, computed tomography and magnetic resonance imaging
Correlation of SPECT/CT findings with clinical features and MRI findings are depicted in Tables 3 and 4. The agreement between MRI findings and SPECT findings are depicted in Table 5a–b. Thecal indentation in L4/L5 region on MRI and increased tracer activity in the corresponding site on SPECT/CT imaging is depicted in Figure 3.
Table 3.
Correlation of neurologic symptoms with abnormalities on imaging
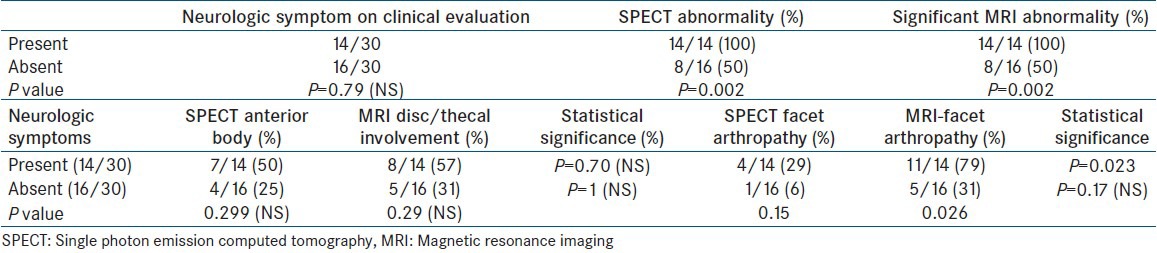
Table 4.
Correlation of straight leg raising test to imaging abnormalities
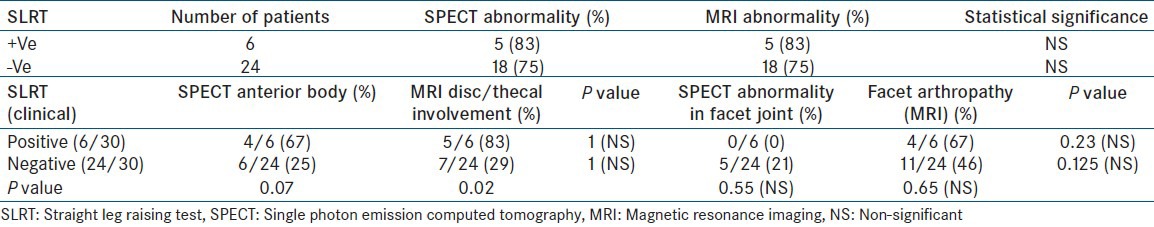
Table 5.
Tests of agreement between single photon emission computed (SPECT) findings and magnetic resonance imaging (MRI).
a: Increased uptake in vertebral body on SPECT versus significant degenerative disc changes on MRI
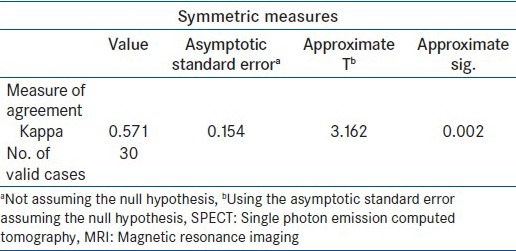
Table 5b.
Facet arthropathy in single photon emission computed tomography versus magnetic resonance imaging
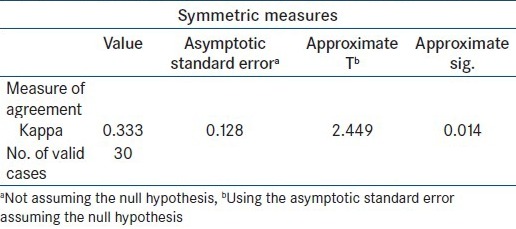
Figure 3.
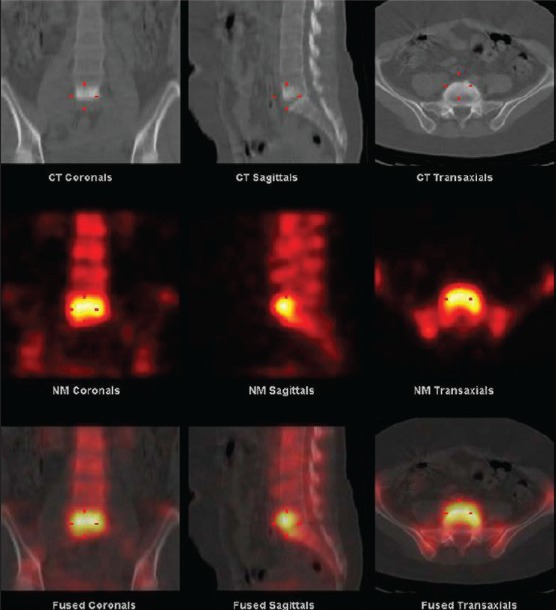
Tc99m single photon emission computed tomography/CT image showing pattern of degenerative disc disease. Increased tracer uptake is noticed in the anterior part of the vertebral body with evidence of sclerosis of the vertebral body in CT
DISCUSSION
LBP is a common disorder with a point prevalence ranging from 6.8% to upto 28% in different populations.[7,8] Six month prevalence of LBP has been reported to have affected 42.6% of patient population.[9] Radiological investigations like skeletal radiography, CT, and MRI are being used in evaluation of patients with LBP. Radiography is universally available and inexpensive investigation for the initial evaluation of patient with LBP. However, the value of radiography has been questioned. Up to 75% of the radiographs yield no useful investigation.[10] CT is a highly sensitive investigation for evaluation of the skeletal system. However, its role in evaluating the soft tissues has been limited. MRI is an excellent non-invasive investigation for evaluation of LBP. It provides superior soft tissue contrast resolution. MRI being an anatomical imaging modality is unable to differentiate between incidental findings from functionally significant findings.
Scintigraphy could be an extremely useful complementary imaging modality to MRI in evaluation of LBP. Availability of hybrid SPECT/CT, apart from accurately localizing the site of abnormality, also allows characterizing sites of functional activity by depicting the morphological changes. The present study was performed in 30 patients with LBP to describe the patterns of scintigraphic abnormalities on SPECT/CT and to correlate the findings with clinical features and MRI findings. The age group (mean age 38 years) and male preponderance (18 male, 12 female) in our study is consistent with the studies done by Pople and Griffith.[11] The mean age of lumbar disc herniation[12] is slightly higher than in our patient group. This may be explained by the fact that most of the patients in our study group were manual laborers. Similarly the prevalence of neurologic symptoms in our patient group is comparable to that reported in literature.[13] However, our study had fewer patients with motor symptoms. This is probably due to the fact that patients presented early in the course of their disease and hence had lesser degree of neurologic impairment. Only 17% of our patients had significant reduction in their functional capacity.
On a total of 30 patients (70%) 21 patients had a scintigraphic abnormality on planar imaging. SPECT imaging of the spine identified extra lesions in these patients. Additionally, one patient with normal planar study was found to have abnormality on SPECT imaging. Without SPECT imaging, three additional lesions could have been missed in our study. Increased tracer uptake in the anterior part of the vertebral body most was the most frequent scintigraphic pattern. This pattern was noted in 45% of those with SPECT abnormality. Our finding is consistent with a previously reported study.[14] The facet joints were the next most common site of abnormality (22% of SPECT positive group) with L3/L4 and L4/L5 sites being involved. The prevalence and distribution of facet joint arthropathy in our study group is consistent with the reported literature.[15,16] The involvement of disc space and isolated spinous process was noted in four patients. Sacroiliitis was noted in two patients. Both the patients had increased erythrocyte sedimentation rate and CRP levels, hence suggesting a diagnosis of inflammatory arthritis. In both these patients, lumbar facet joints were also involved. This is consistent with the fact that zygo-apophyseal joints are affected in a major way in inflammatory arthritis like ankylosing spondylitis.[17] Morphologic changes obtained from CT allowed for improving the specificity of SPECT abnormalities. The most frequent morphologic abnormalities in these patients were osteohphytes and para-discal sclerotic changes noted in 76% of the patients. These findings, in the presence of SPECT abnormality in the anterior part of the vertebral body, secured the diagnosis of degenerative changes as the cause of LBP. CT helped in identifying an osteoid osteoma in one of the patients. The improvement of specificity of SPECT findings is correlating with variety of published literature on this new modality.[18,19]
CT images of the lumbar spine allowed accurate co-registration of the SPECT data. This greatly improved the localization of the lesion. Corresponding morphological changes also allowed for lesion characterization. Similar utility of the CT data in hybrid SPECT/CT has also been reported by other studies.[20,21] In four patients with SPECT abnormality no morphologic abnormality was detected on CT. This is explained by the fact that scintigraphic techniques identify pathology earlier than morphologic changes are evident. Ryan et al.[22] also noted similar findings in their study where 21% of the patients failed to show morphologic changes in spite of having SPECT abnormality.
All 30 patients had some MRI abnormality. After exclusion of minor disc abnormalities, 22 of the 30 patients (73%) were noted to have significant MRI abnormalities. MRI detected 29 facet joint lesions in 15 patients with 60% of the patients having abnormality in multiple level facet joints. SPECT revealed active facet joint disease in only 15 of these sites. Only one patient had multiple sites of increased tracer uptake. Hence, rest of the abnormalities detected on MRI, in these patients, are most likely non-significant findings. This is further strengthened by the fact that, despite presence of MRI abnormalities, none of the patients with normal SPECT had any neurologic symptom or significant reduction in functional capacity. The difference in incidence of neurologic symptoms and reduction in functional capacity between SPECT positive and negative patients was statistically significant (P = 0.002). Specificity of SPECT findings to identify active disease was further confirmed by Dolan[23] who noted that there is 95% response rate after injection therapy of SPECT positive facets. Pneumaticos in a recent study,[24] proved that significant improvement in back pain is noted only when SPECT positive facet joints are subjected to injection therapy. Hence, the results from SPECT/CT could potentially be used for selection of facet joints for treatment.
MRI finding of facet joint abnormalities were significantly more common in the group with neurologic symptoms than in those without symptoms (79% vs. 31%; P = 0.026) Similarly, MRI identified significantly more facet abnormalities than SPECT (79% vs. 29%; P = 0.023). This correlates with the fact that MRI has high sensitivity in identifying facet joint abnormalities. It would be difficult to attribute the cause of neurologic symptoms to facet joint arthropathy as all but one patient had associated disc degeneration in MRI. Clinically, it is impossible to differentiate pain caused due to facet abnormalities from other etiologies. Another prospective study has also confirmed this finding.[25] There was statistically significant difference in the prevalence of SPECT/MRI abnormalities between patients with and without reduced functional capacity due to LBP. The findings between SPECT and MRI were concordant, with MRI showing more abnormalities. SPECT helped identify the site of MRI abnormality that is clinically significant.
Sixty-seven percent of the patients having positive SLRT had SPECT abnormality localized to the anterior part of the vertebral body. Though prevalence of this abnormality was only 25% in those with negative SLRT, the difference did not reach statistical significance (P = 0.07). On MRI, disc degeneration was noted in 83% of them. Only 29% of those without positive SLRT had this abnormality and this difference was statistically significant (P = 0.02). Two of these patients also had disc abnormality at other vertebral levels and four of these six patients had facet joint arthropathy. However, none of these patients had facet abnormality on SPECT imaging. The significance of each of the abnormalities detected with MRI would have been impossible without correlative findings on SPECT.
There was statistically significant agreement between disc degenerative changes on MRI and tracer uptake in the anterior part of the vertebral body. The uptake in the anterior part of the vertebral body, with extension beyond the vertebral body, is most likely to represent the MRI equivalent of disc degeneration. This pattern is consistent with previously reported SPECT equivalents of degenerative disc disease in MRI.[22] There was no significant agreement between the facet joint disease identified by MRI and SPECT. MRI detected significantly more disease than SPECT. This is in agreement with the fact that SPECT is more specific than MRI.
MRI revealed multiple abnormalities in most of the patients. Maeseneer[26] concluded that scintigraphy may be used to determine the precise cause of symptoms in patients with multiple abnormalities at other imaging studies. We, in our study, have noted that SPECT is extremely useful in localizing the precise cause when multiple abnormalities are present in MRI. The utility of SPECT to determine the precise cause of symptoms has been extensively used in osteoporotic patients with LBP.[27] Cook, in his review article,[28] concluded that scintigraphy has been valuable in identifying unsuspected osteoporotic fracture, assess the age of the fracture and excluding fracture as the cause of LBP. A similar wider application of SPECT/CT, as a complementary investigation to MRI in LBP, is foreseen in our study.
The study suffers from a few limitations. The study utilized low dose CT for registration with the SPECT images. Addition of high dose diagnostic quality CT could have allowed for identification for early morphololgic changes and potentially improved lesion characterization. Sites of increased uptake in SPECT images were considered to be the actual cause of the back pain. No active clinical intervention was attempted in any of the patients to confirm the actual cause of the back pain.
In conclusion, all patients with LBP are likely to have some MRI abnormality. Most of the patients are likely to have MRI abnormalities at multiple sites. Addition of SPECT/CT is invaluable in differentiating significant from incidental non-significant findings on MRI. Increased tracer uptake in the anterior part of the vertebral body with associated osteophytes and or sclerotic changes in CT is the SPECT/CT equivalent of intervertebral disc degeneration. This pattern has statistically significant agreement with MRI evidence of intervertebral disc degeneration. SPECT/CT identifies significantly less patients with facet arthropathy as compared to MRI. However, SPECT/CT is likely to be more specific. SPECT/CT is best used complementary to MRI in patients with LBP. SPECT/CT should be considered mandatory before attempting injection therapy of facet joint arthropathy and in patient with multiple abnormalities on MRI.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Spitzer WO, LeBlanc FE, Dupuis MS. Scientific approach to the assessment and management of activity-related spinal disorders. A monograph for clinicians. Report of the Quebec Task Force on Spinal Disorders. Spine (Phila Pa 1976) 1987;12:S1–59. [PubMed] [Google Scholar]
- 2.Harreby M, Neergaard K, Hesselsøe G, Kjer J. Are radiologic changes in the thoracic and lumbar spine of adolescents risk factors for low back pain in adults? A 25-year prospective cohort study of 640 school children. Spine (Phila Pa 1976) 1995;20:2298–302. doi: 10.1097/00007632-199511000-00007. [DOI] [PubMed] [Google Scholar]
- 3.Schwarzer AC, Aprill CN, Derby R, Fortin J, Kine G, Bogduk N. The relative contributions of the disc and zygapophyseal joint in chronic low back pain. Spine (Phila Pa 1976) 1994;19:801–6. doi: 10.1097/00007632-199404000-00013. [DOI] [PubMed] [Google Scholar]
- 4.Schwarzer AC, Wang SC, Bogduk N, McNaught PJ, Laurent R. Prevalence and clinical features of lumbar zygapophysial joint pain: A study in an Australian population with chronic low back pain. Ann Rheum Dis. 1995;54:100–6. doi: 10.1136/ard.54.2.100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.van Tulder MW, Assendelft WJ, Koes BW, Bouter LM. Spinal radiographic findings and nonspecific low back pain. A systematic review of observational studies. Spine (Phila Pa 1976) 1997;22:427–34. doi: 10.1097/00007632-199702150-00015. [DOI] [PubMed] [Google Scholar]
- 6.Deyo RA. Diagnostic evaluation of LBP: Reaching a specific diagnosis is often impossible. Arch Intern Med. 2002;162:1444–7. doi: 10.1001/archinte.162.13.1444. [DOI] [PubMed] [Google Scholar]
- 7.Loney PL, Stratford PW. The prevalence of low back pain in adults: A methodological review of the literature. Phys Ther. 1999;79:384–96. [PubMed] [Google Scholar]
- 8.Cassidy JD, Carroll LJ, Côté P. The Saskatchewan health and back pain survey. The prevalence of low back pain and related disability in Saskatchewan adults. Spine (Phila Pa 1976) 1998;23:1860–6. doi: 10.1097/00007632-199809010-00012. [DOI] [PubMed] [Google Scholar]
- 9.Walker BF, Muller R, Grant WD. Low back pain in Australian adults: Prevalence and associated disability. J Manipulative Physiol Ther. 2004;27:238–44. doi: 10.1016/j.jmpt.2004.02.002. [DOI] [PubMed] [Google Scholar]
- 10.Scavone JG, Latshaw RF, Rohrer GV. Use of lumbar spine films. Statistical evaluation at a university teaching hospital. JAMA. 1981;246:1105–8. [PubMed] [Google Scholar]
- 11.Pople IK, Griffith HB. Prediction of an extruded fragment in lumbar disc patients from clinical presentations. Spine (Phila Pa 1976) 1994;19:156–8. doi: 10.1097/00007632-199401001-00007. [DOI] [PubMed] [Google Scholar]
- 12.Carragee EJ, Kim DH. A prospective analysis of magnetic resonance imaging findings in patients with sciatica and lumbar disc herniation. Correlation of outcomes with disc fragment and canal morphology. Spine (Phila Pa 1976) 1997;22:1650–60. doi: 10.1097/00007632-199707150-00025. [DOI] [PubMed] [Google Scholar]
- 13.Beattie PF, Meyers SP, Stratford P, Millard RW, Hollenberg GM. Associations between patient report of symptoms and anatomic impairment visible on lumbar magnetic resonance imaging. Spine (Phila Pa 1976) 2000;25:819–28. doi: 10.1097/00007632-200004010-00010. [DOI] [PubMed] [Google Scholar]
- 14.Kanmaz B, Collier BD, Liu Y, Uzum F, Uygur G, Akansel G, et al. SPET and three-phase planar bone scintigraphy in adult patients with chronic low back pain. Nucl Med Commun. 1998;19:13–21. doi: 10.1097/00006231-199801000-00004. [DOI] [PubMed] [Google Scholar]
- 15.Manchikanti L, Manchukonda R, Pampati V, Damron KS, McManus CD. Prevalence of facet joint pain in chronic low back pain in postsurgical patients by controlled comparative local anesthetic blocks. Arch Phys Med Rehabil. 2007;88:449–55. doi: 10.1016/j.apmr.2007.01.015. [DOI] [PubMed] [Google Scholar]
- 16.Manchikanti L, Pampati V, Fellows B, Bakhit CE. Prevalence of lumbar facet joint pain in chronic low back pain. Pain Physician. 1999;2:59–64. [PubMed] [Google Scholar]
- 17.de Vlam K, Mielants H, Veys EM. Involvement of the zygapophyseal joint in ankylosing spondylitis: Relation to the bridging syndesmophyte. J Rheumatol. 1999;26:1738–45. [PubMed] [Google Scholar]
- 18.Buck AK, Nekolla S, Ziegler S, Beer A, Krause BJ, Herrmann K, et al. SPECT/CT. J Nucl Med. 2008;49:1305–19. doi: 10.2967/jnumed.107.050195. [DOI] [PubMed] [Google Scholar]
- 19.Patel CN, Chowdhury FU, Scarsbrook AF. Hybrid SPECT/CT: The end of “unclear” medicine. Postgrad Med J. 2009;85:606–13. doi: 10.1136/pgmj.2008.077859. [DOI] [PubMed] [Google Scholar]
- 20.Even-Sapir E, Flusser G, Lerman H, Lievshitz G, Metser U. SPECT/multislice low-dose CT: A clinically relevant constituent in the imaging algorithm of nononcologic patients referred for bone scintigraphy. J Nucl Med. 2007;48:319–24. [PubMed] [Google Scholar]
- 21.Roach PJ, Schembri GP, Ho Shon IA, Bailey EA, Bailey DL. SPECT/CT imaging using a spiral CT scanner for anatomical localization: Impact on diagnostic accuracy and reporter confidence in clinical practice. Nucl Med Commun. 2006;27:977–87. doi: 10.1097/01.mnm.0000243372.26507.e7. [DOI] [PubMed] [Google Scholar]
- 22.Ryan PJ, Evans PA, Gibson T, Fogelman I. Chronic low back pain: Comparison of bone SPECT with radiography and CT. Radiology. 1992;182:849–54. doi: 10.1148/radiology.182.3.1531544. [DOI] [PubMed] [Google Scholar]
- 23.Dolan AL, Ryan PJ, Arden NK, Stratton R, Wedley JR, Hamann W, et al. The value of SPECT scans in identifying back pain likely to benefit from facet joint injection. Br J Rheumatol. 1996;35:1269–73. doi: 10.1093/rheumatology/35.12.1269. [DOI] [PubMed] [Google Scholar]
- 24.Pneumaticos SG, Chatziioannou SN, Hipp JA, Moore WH, Esses SI. Low back pain: Prediction of short-term outcome of facet joint injection with bone scintigraphy. Radiology. 2006;238:693–8. doi: 10.1148/radiol.2382041930. [DOI] [PubMed] [Google Scholar]
- 25.Jackson RP, Jacobs RR, Montesano PX. Volvo award in clinical sciences. Facet joint injection in low-back pain. A prospective statistical study. Spine (Phila Pa 1976) 1988;13:966–71. doi: 10.1097/00007632-198809000-00002. [DOI] [PubMed] [Google Scholar]
- 26.De Maeseneer M, Lenchik L, Everaert H, Marcelis S, Bossuyt A, Osteaux M, et al. Evaluation of lower back pain with bone scintigraphy and SPECT. Radiographics. 1999;19:901–12. doi: 10.1148/radiographics.19.4.g99jl03901. [DOI] [PubMed] [Google Scholar]
- 27.Ryan PJ, Fogelman I. Osteoporotic vertebral fractures: Diagnosis with radiography and bone scintigraphy. Radiology. 1994;190:669–72. doi: 10.1148/radiology.190.3.8115608. [DOI] [PubMed] [Google Scholar]
- 28.Cook GJ, Hannaford E, See M, Clarke SE, Fogelman I. The value of bone scintigraphy in the evaluation of osteoporotic patients with back pain. Scand J Rheumatol. 2002;31:245–8. doi: 10.1080/030097402320318459. [DOI] [PubMed] [Google Scholar]


