Abstract
Penile cancer is an uncommon malignancy which of the management depends on the clinical stage and location of the lesion. Positron emission tomography/computerized tomography (PET/CT) is a promising method for detection of distant metastatic lesions and therapeutic strategy planning. Here, we report a case of penile squamous cell carcinoma of 57-year-old male patient, was referred to PET/CT department for investigation of metastases. There were significantly increased fluoro-18 fluorodeoxyglucose activities in supradiaphragmatic and infradiaphragmatic lymphatic stations.
Keywords: Fluorodeoxyglucose, nodal involvement, penile squamous cancer, Positron emission tomography/computerized tomography
INTRODUCTION
Squamous cell carcinoma (SCC) of the penile is an uncommon malignancy. It usually appears in the epithelium of the inner prepuce and glans.[1] Risk factors contain unhygienic conditions such as phimosis and chronic inflammatory disease, sexual history, condylomata history and smoking.[2,3] The management depends on the clinical stage and the location of the lesion. Penile cancer drains principally to the inguinal nodes and then spreads to the pelvic lymph nodes.[4,5]
If tumor-positive inguinal nodes are demonstrated, scanning methods must be used to search pelvic metastases and distant metastases for the increasing risk of further lymphatic spread.[6,7,8] Positron emission tomography/computerized tomography (PET/CT) scanning is a reliable method to determine pelvic and more distant metastases.[9,10] If PET/CT is not available abdominal CT scan and chest x-ray are advisable and in symptomatic M1 patients a bone scan is also advisable.[1] The aim of this case report is to represent the significance of fluoro-18 fluorodeoxyglucose (18F-FDG) PET/CT detected by the metastases in a patient with penile carcinoma [Figures 1 and 2].
Figure 1.
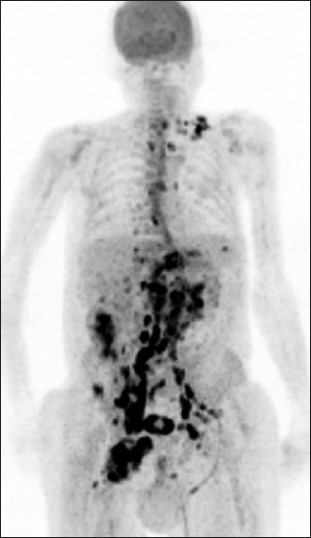
Fluorodeoxyglucose (FDG) PET MIP image showed that intense accumulation of FDG on inguinal lymph nodes and increased FDG uptake was detected on multiple lymphadenomegalies in abdomen-pelvis and the left-inferior jugular region, the left supraclavicular fossa and the mediastinal lymph nodes
Figure 2.
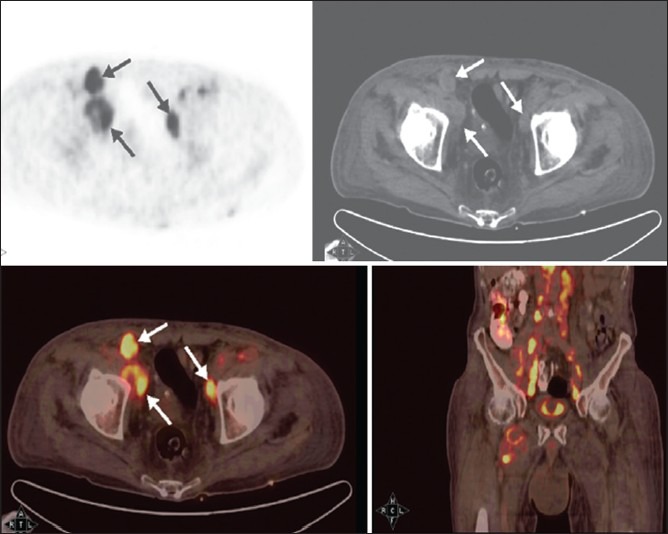
Pelvis axial PET, computed tomography, fusion and coronal fusion images showed multiple lymphadenomegalies in the iliac region
CASE REPORT
We report a case of a 57-year-old male demonstrated inguinal metastases with biopsy then underwent amputation and recognized histopathological grade 2 (moderately differentiated) penile SCC. The patient was referred to our PET/CT department to search for possible further metastatic disease. Following 10 h fasting (serum glucose level 126 mg/dl), the patient was injected with 14.5 mCi F-18 of fluorodeoxyglucose(FDG) intravenously. After 1 h waiting period, whole-body images were obtained on the Siemens HI-REZ PET/CT System. Fused images of metabolic (PET) and anatomic (CT) information were reviewed. PET/CT study showed that intense accumulation of FDG on inguinal lymph nodes. Additionally, increased FDG uptake was detected on multiple lymphadenomegalies in abdomen-pelvis and the left-inferior jugular region, the left supraclavicular fossa and the mediastinal lymph nodes [Figures 1 and 2]. Also, PET images demonstrated a few uptakes in the left axilla and left parasternal lymph nodes. The lung parenchyma, liver and skeletal system demonstrated a physiological distribution of the tracer. Histopathological results showed primary penile SCC carcinoma [Figure 3a] and metastatic inguinal lymph nodes [Figure 3b].
Figure 3a-b.
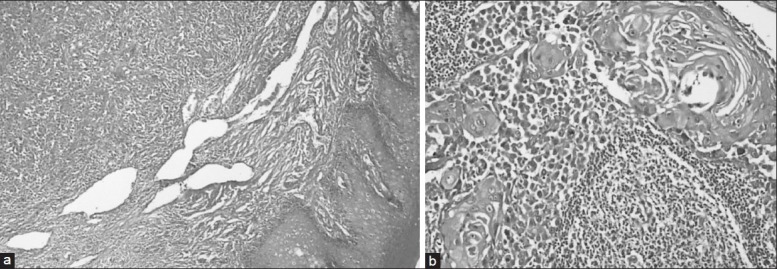
Histopathological examination showed well differentiated squamous cells with keratinization and transition zone which is concordant with primary penile squamous cancer and squamous cells with central keratinization in inguinal metastatic lymph node (H and E, ×100)
DISCUSSION
Penile carcinoma has a lymphogenic pattern of metastases and the firstly drain inguinal lymph nodes and subsequently pelvic nodes. The detection of pelvic metastases and more distant metastases has a considerable impact on therapy and prognosis.[4,5]
Initial F-18 FDG-PET scanning is a promising method on detecting loco regional lymph node metastases and distant metastases in the stage of penile cancer. However, conventional imaging techniques such as CT scans are insufficient to detect pelvic nodal involvement in penile cancer patients.[9,10] FDG-PET with low-dose CT scanning provide to scan whole body and also give functional, anatomic information on one image. Correct staging is crucial in the selection of appropriate treatments and the follow-up the patients. The use of PET/CT provides considerable much knowledge of TNM clinical classification of penile cancer.
Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Pizzocaro G, Algaba F, Horenblas S, Solsona E, Tana S, Van Der Poel H, et al. EAU penile cancer guidelines 2009. Eur Urol. 2010;57:1002–12. doi: 10.1016/j.eururo.2010.01.039. [DOI] [PubMed] [Google Scholar]
- 2.Dillner J, von Krogh G, Horenblas S, Meijer CJ. Etiology of squamous cell carcinoma of the penis. Scand J Urol Nephrol Suppl. 2000;205:189–93. doi: 10.1080/00365590050509913. [DOI] [PubMed] [Google Scholar]
- 3.Daling JR, Madeleine MM, Johnson LG, Schwartz SM, Shera KA, Wurscher MA, et al. Penile cancer: Importance of circumcision, human papillomavirus and smoking in in situ and invasive disease. Int J Cancer. 2005;116:606–16. doi: 10.1002/ijc.21009. [DOI] [PubMed] [Google Scholar]
- 4.Daseler EH, Anson BJ, Reımann AF. Radical excision of the inguinal and iliac lymph glands; a study based upon 450 anatomical dissections and upon supportive clinical observations. Surg Gynecol Obstet. 1948;87:679–94. [PubMed] [Google Scholar]
- 5.Leijte JA, Valdés Olmos RA, Nieweg OE, Horenblas S. Anatomical mapping of lymphatic drainage in penile carcinoma with SPECT-CT: Implications for the extent of inguinal lymph node dissection. Eur Urol. 2008;54:885–90. doi: 10.1016/j.eururo.2008.04.094. [DOI] [PubMed] [Google Scholar]
- 6.Horenblas S, van Tinteren H. Squamous cell carcinoma of the penis. IV. Prognostic factors of survival: Analysis of tumor, nodes and metastasis classification system. J Urol. 1994;151:1239–43. doi: 10.1016/s0022-5347(17)35221-7. [DOI] [PubMed] [Google Scholar]
- 7.Lont AP, Kroon BK, Gallee MP, van Tinteren H, Moonen LM, Horenblas S. Pelvic lymph node dissection for penile carcinoma: Extent of inguinal lymph node involvement as an indicator for pelvic lymph node involvement and survival. J Urol. 2007;177:947–52. doi: 10.1016/j.juro.2006.10.060. [DOI] [PubMed] [Google Scholar]
- 8.Zhu Y, Zhang SL, Ye DW, Yao XD, Jiang ZX, Zhou XY. Predicting pelvic lymph node metastases in penile cancer patients: A comparison of computed tomography, Cloquet's node, and disease burden of inguinal lymph nodes. Onkologie. 2008;31:37–41. doi: 10.1159/000112462. [DOI] [PubMed] [Google Scholar]
- 9.Graafland NM, Leijte JA, Valdés Olmos RA, Hoefnagel CA, Teertstra HJ, Horenblas S. Scanning with 18F-FDG-PET/CT for detection of pelvic nodal involvement in inguinal node-positive penile carcinoma. Eur Urol. 2009;56:339–45. doi: 10.1016/j.eururo.2009.05.016. [DOI] [PubMed] [Google Scholar]
- 10.Schlenker B, Scher B, Tiling R, Siegert S, Hungerhuber E, Gratzke C, et al. Detection of inguinal lymph node involvement in penile squamous cell carcinoma by 18F-fluorodeoxyglucose PET/CT: A prospective single-center study. Urol Oncol. 2012;30:55–9. doi: 10.1016/j.urolonc.2009.10.012. [DOI] [PubMed] [Google Scholar]


