Abstract
The primary hypertrophic osteoarthropathy (HOA) (pachydermoperiostosis) is a rare hereditary disease characterized by skin manifestations (pachydermia), digital clubbing and proliferation of periosteum (periostitis) with sub-periosteal new bone formation. We describe here a case who presented with seborrheic dermatitis and joint pain of both hands on work up matched satisfactorily with the complete form of primary HOA. The identification of secondary form being relatively common among clinicians and hence the importance of recognizing the primary form, which is a difficult to treat condition is discussed here.
Keywords: Pachydermoperiostosis, primary hypertrophic osteoarthropathy, Touraine-Solente-Gole syndrome
INTRODUCTION
Pachydermoperiostosis or primary hypertrophic osteoarthropathy (HOA) is a hereditary disease characterized by pachydermia (skin thickening), digital clubbing and periostosis co-existing with variety of clinical manifestations including, palmoplantar hyperhidrosis, joint pain, arthritis, cutis verticis gyrata, ptosis, and hypertrophic gastritis. It was initially described by Friedreich in 1868 and then by Touraine, et al. in 1935 who recognized its’ familial nature and described three forms of presentation: Complete (pachydermia, digital clubbing, and periostosis), incomplete (no pachydermia), and frustre form (prominent pachydermia with few skeletal manifestations).
Pachydermoperiostosis represents 3% of total of HOA but its prevalence is unknown for general population. It has a marked predominance in males and the ratio being 9:1 and has autosomal dominant pattern of inheritance with familial aggregation in 25-38% of cases. The main purpose of these patients consulting the physician are the skin manifestations as well as bone and joint pain the latter two giving us the clue to diagnose this rare but easily recognizable clinical entity. Because of this, we have considered presenting this case report of a middle-aged man with HOA who visited our hospital with dermatological and musculoskeletal complaints.
CASE REPORT
A 44-year-old male presented with complaints of generalized itching for past 5 years. He also had swelling and pain in both knees ankles and small joints of hands with worsening of symptoms following exercise. Fever or other associated rheumatological symptoms were denied. No relevant family history. He also had troublesome dyspepsia for past 6 months with no relief in spite of medications. Physical examination revealed greasy and coarse skin with deep furrowed forehead skin. Examination revealed ptosis of both eyelid, hyperhydrosis of both palms and soles, generalized seborrheic dermatitis and multiple folliculitis in both lower limbs [Figure 1]. The patient showed pandigital clubbing and bulbous deformity of all digits of hand and feet [Figures 2, 3a and b]. Laboratory work up of routine blood and urine investigations including S. VDRL (venereal disease research laboratory) were unremarkable.
Figure 1.
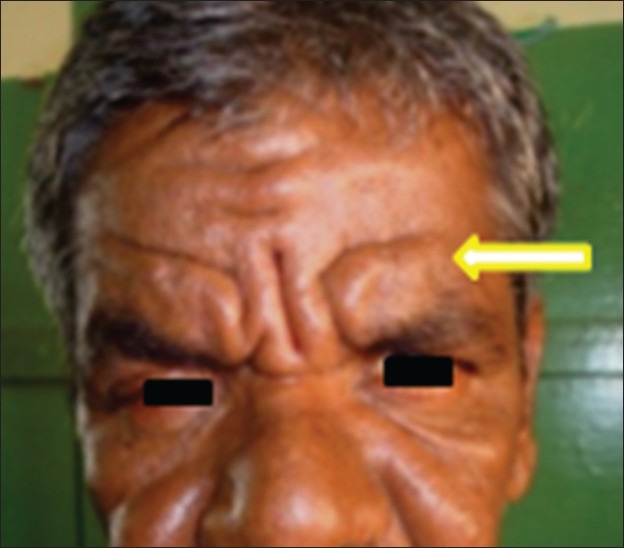
Greasy and coarse skin with deep furrowed forehead skin with ptosis of both eyelid
Figure 2.

Pandigital clubbing of both hands
Figure 3a.

Pandigital clubbing of both feet with bulbous enlargement of all toes
Figure 3b.

Hypertrophied thumb of this patient in comparison with the normal thumb
Radiograph of both hands and wrists showed increase in soft-tissue around terminal phalanges with hypertrophy of distal tufts and periosteal thickening in all metacarpals including proximal and middle phalanges [Figure 4]. Radiograph of both feet revealed similar changes. X-ray of both forearm showed symmetric exuberant irregular sub-periosteal bone formation with cortical thickening in both radius and ulna. There was interosseus membrane ossification in Lt fore-arm [Figure 5]. X-ray of both tibia and fibula showed gross irregularities and intense periosteal proliferation throughout the shaft including epiphysis and resultant broadening of the epiphysis [Figure 6]. Lateral radiograph of skull revealed normal sella turcica and hyperostosis of skull bones. Chest radiograph was taken to rule out pulmonary causes of HOA which was found to be normal. 99mTc MDP (methylene diphosphonate) bone scintigraphy was performed following standard protocols after i.v administration of 20 mCi activity Figure 7a and b shows diffusely increased and almost symmetrical peri-cortical uptake in the entire skeletal system prominently involving the shaft of all long bones. In view of his troublesome dyspepsia, upper gastro intestinal endoscopy carried out showed hypertrophied mucosal folds involving the entire stomach and antrum. CECT abdomen with negative contrast revealed uniform increase in stomach wall thickness >1 cm.
Figure 4.

Radiograph of both hands and wrists showed increase in soft tissue around terminal phalanges with hypertrophy of distal tufts and periosteal thickening in all metacarpals including proximal and middle phalanges
Figure 5.
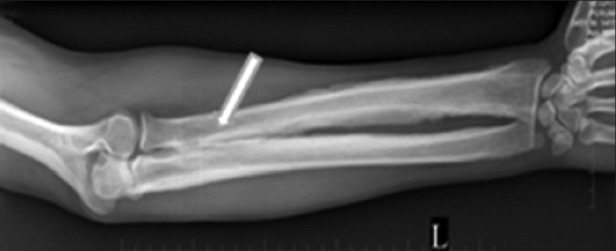
X-ray of both forearm showed symmetric exuberant irregular sub-periosteal bone formation with cortical thickening in both radius and ulna and there is interosseus membrane ossification in Lt forearm
Figure 6.

X-ray of both tibia and fibula showed gross irregularities and intense periosteal proliferation throughout the shaft including epiphysis and resultant broadening of the epiphysis
Figure 7.
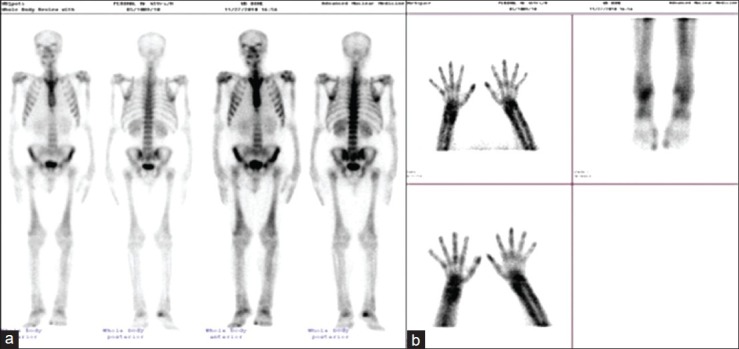
(a, b) 99mTc MDP bone scintigraphy performed following standard protocols after i.v., administration of 20 mCi activity shows diffusely increased and almost symmetrical pericortical uptake in the entire skeletal system prominently involving the shaft of all long bones
His skin biopsy showed thickening and packing of collagen fibres in dermis – Features suggestive of pachydermia. Based on the clino-radiological correlation and after ruling out other secondary causes the diagnosis of Touraine-Solente-Gole syndrome or primary HOA was made.
DISCUSSION
HOA is a syndrome characterized by digital clubbing, periostosis, and arthritis. The disease is classified either as primary (hereditary or idiopathic) or secondary form. The idiopathic form (named pachydermoperiostosis, or primary HOA or Touraine Solente Gole syndrome) is a rare disease with unknown etiology and represents 3-5% of all cases of HOA. The secondary form is associated with several diseases like bronchiectasis, cystic fibrosis, congenital heart diseases, biliary cirrhosis, inflammatory bowel disease etc., and sometimes occurs as a part of paraneoplastic syndrome. Primary HOA is often familial and has autosomal dominant pattern of inheritance. The onset is usually around puberty and presents with enlargement of digits and clubbing. Diagnostic criteria for primary HOA[1] are: Major criteria - pachydermia, periostosis, finger clubbing; Minor criteria - hyperhidrosis, arthralgia, hypertrophic gastritis, ptosis, joint effusion, seborrhea, acne, and flushing.
Touraine et al. proposed a classification for primary HOA[2] where the complete form includes, pachydermia, clubbing and periostosis; the fruste form has prominent pachydermia with minimal skeletal changes; the incomplete form has skeletal changes and no pachydermia. The skin and bone changes become progressively severe for 5-10 years and remain static thereafter. In 30-40% of cases the skin hypertrophy involves eyelids leading to mechanical ptosis.[3] In long standing cases a typical leonine facies develops. The clubbing is a frequent symptom and occurs in 89% of patients with primary HOA. Skeletal findings include, symmetric exuberant sub-periosteal bone formation in long bones of forearm, leg, metacarpals, metatarsals and also the phalanges. The irregular periosteal proliferation affects predominantly the distal ends of long bones including epiphysis in 80-97% of patients.[4] Involvement of epiphysis distinguishes it from the secondary form that typically spares the epiphysis. Bone scintigrapy is very sensitive in detecting HOA and it shows bilateral symmetrical increased uptake of radiopharmaceutical along the cortical margins giving the typical appearance and is known as “tram line” or “double stripe” sign.[4]
In childhood, the clinical presentation being more rheumatoid, this diagnosis should be considered in any child presenting with digital clubbing and joint pains because the periostitis tend to involve the epiphysis causing alteration in growth of long bones leading to growth disturbances. Gastrointestinal involvement in the form of hypertrophic gastropathy occurs in 27% of patients with primary HOA.[5] Our patient had all the dermatoradiological manifestations of the complete form of Touraine-Solente-Gole syndrome. He also had hypertrophic gastropathy which is an infrequent association mentioned in literatures.[5] Myelofibrosis and resultant anemia, chrons disease, acromegaly is known associations with primary HOA. Treatment modalities include, NSAIDS (non-steroidal anti inflammatory drugs), colchicines and course of steroids. Rheumatological symptoms show improvement with intravenous pamidronate a bisphosphonate at the dose of 1 mg/kg. Isotretinoin at the initial dose of 0.5 mg/kg/day[1] gives dramatic improvement of skin symptoms. Plastic surgery may be helpful for complications on the face.
CONCLUSION
The patient studied in this case sought medical help for seborrheic dermatitis and non-specific joint pain and on serial work-up matched satisfactorily with the complete form of primary HOA. Gastric manifestations are events occurring in 27%[6] of patients and our patient has this rare association too. Primary HOA has to be differentiated from secondary form. Table 1 summarizes the main differences between the primary and secondary form; the other differential diagnosis being acromegaly and thyroid acropachy the former has other associated clinical and laboratory evidence and the latter predominantly involves the tubular bones of hand and feet rather than long bones. Pachydermoperiostosis has also been occasionally confused with syphilitic periostitis and leprosy. The latter two needs special mention because their misdiagnosis has widespread social implications in developing countries. This case is presented here because of its typical clinic-radiological spectrum and its close resemblance to various common diseases needs to be recognized by the radiologist to aid easy identification of this rare disorder.
Table 1.
Differences between primary HOA and secondary HOA

Footnotes
Source of Support: Nil
Conflict of Interest: None declared
REFERENCES
- 1.Auger M, stavrianeas N. Auger M, Stavrianeas N, editors. Pachydermoperiostosis. “Pachydermoperiostosis” Orphanet Encyclopedia. 2004. http://www.orpha.net/data/patho/GB/uk-pachydermoperiostosis.pdf .
- 2.Touraine A, Solente G, Gole L. Un syndrome osteo-dermopathique: La pachydermia plicaturee avec pachyperiostose des extremites. Presse Med. 1935;43:1820–4. [Google Scholar]
- 3.Matucci-Cerinic M, Lotti T, Calvieri S, Ghersetich I, Sacerdoti L, Teofoli P, et al. The spectrum of dermatological symptoms of pachydermoperiostosis (primary hypertrophic osteoarthropathy): A genetic, cytogenetic and ultrastructural study. Clin Exp Rheumatol. 1992;10:45–8. [PubMed] [Google Scholar]
- 4.Rosenthall L, Kirsh J. Observations of radionuclide imaging in hypertrophic pulmonary osteoarthropathy. Radiology. 1976;120:359–62. doi: 10.1148/120.2.359. [DOI] [PubMed] [Google Scholar]
- 5.Jajic I, Jajic Z. The spectrum of skeletal visceral abnormalities in 52 patients with primary hypertrophic Osteoarthropathy. Clin Exp Rheum. 1992;10:73. [Google Scholar]
- 6.Lam SK, Hui WK, Ho J, Wong KP, Rotter JI, Samloff IM. Pachydermoperiostosis, hypertrophic gastropathy and peptic ulcer. Gastroenterology. 1983;84:834–9. [PubMed] [Google Scholar]


