Abstract
Nuclear factor κB (NFκB) is a transcription factor that plays an important role in carcinogenesis as well as in the regulation of inflammatory response. NFκB is constitutively expressed in tumours where it induces the expression of genes which promote cell proliferation, apoptotic events, angiogenesis, invasion and metastasis. Furthermore, many cancer cells show aberrant or constitutive NFκB activation that mediates resistance to chemo- and radio-therapy. Therefore, the inhibition of NFκB activity appears a potential therapeutic strategy for cancer treatment. In this review, we focus on the role of NFκB in carcinogenesis and summarize actual inhibitors of NFκB that could be potential therapeutic target in cancer therapy.
Keywords: transcription factors, IκB, GRK5, cancer
I. INTRODUCTION
Human cancer is a complex disease based on multiple etiologies, multiple cell targets, and distinct developmental stages. Cancer cells share common features that regulate cell proliferation and homeostasis [1] including resistance to growth inhibitory signals, self-sufficiency in growth, resistance to apoptosis, extended replication potential, enhanced angiogenic potential, and the ability to invade local tissue and to metastasize to distant sites [1]. Autonomous cell growth characterizes cancer cells and depends on impaired expression of growth factors or growth factor receptors, leading to uncontrolled cell proliferation. Thus, a fairly common mechanism in cancer is the up-regulation of expression of members of the epidermal growth factor receptor family such as EGF receptor or Her2/ErbB2. Furthermore, certain cancer cells produce growth factors such as PDGF and TGF-α, which can promote cell proliferation in an autocrine manner [1,2]. Mutations in proteins that regulate cell proliferation are also relatively common in cancer. For example, resistance to growth inhibitory signals are due to mutations in tumour suppressor genes such as p53, Rb, Arf, and APC, or in receptors such as those for TGFβ. Additionally, up-regulation of expression of cyclin D1 or c-myc, or activating mutations in transcription factors can promote cell proliferation or cell growth [1,2]. A key process in the ability of tumour cells to spread is the suppression of apoptotic potential. Resistance to apoptosis can involve the activation of expression of anti-apoptotic factors, such as Bcl-2 or Bcl-xL, or the loss of expression or mutation of pro-apoptotic factors, such as p53 [2]. Additionally, mutation in tumour suppressors such as PTEN leads to the activation of intracellular signalling pathways (in this case, the PI3 kinase/Akt pathway) that suppress apoptosis [3]. An additional mechanism of suppression of cancer cell apoptosis can be derived from release of cytokines from the tumour stroma [2]. The ability of cancer cells to metastasize depends on angiogenesis which in turn is mediated through a complex interplay of regulatory factors, including vascular endothelial growth factor (VEGF). In fact, many tumors exhibit up-regulation of VEGF [1]. Local invasion is mediated by changes in expression of cell adhesion molecules and integrins, and in changes in expression of extracellular proteases such as MMP-2 and MMP-9. In some situations, the matrix-degrading proteases are produced by the tumour-associated stromal and inflammatory cells [2].
II. TRANSCRIPTION FACTORS AND NFκB
Transcription factors are gene regulatory proteins that bind to the promoter or enhancer regions of target genes and induce either transcriptional repression or activation [4]. The basic structure of a transcription factor mainly contains a DNA-binding domain and an activator domain. DNA-binding motifs include zinc-finger, helix-loop-helix, helix-turn-helix, leucine zipper and high-mobility groups, based on which transcription factors are classified [4,5]. The activator domain of these transcription factors interacts with components of transcription machinery such as RNA polymerases and associated transcription regulators. Transcription factors regulate gene expression in different ways: they stabilize or block the binding of RNA polymerase to DNA; catalyse the acetylation or deacetylation of histone proteins; recruit co-activator or co-repressor proteins to the transcription factor DNA complex [4,6,7]. Transcription factors represent prime targets for disruption in many diseases [8]. In cancer, for instance, a number of oncogenic transcription factors such as activator protein 1 (AP-1), nuclear factor κB (NFκB), and signal transducer and activator of transcription (STAT)-3/STAT5 are constitutively expressed and thus may present promising targets for cancer prevention [9]. Among them, NFκB is an ubiquitously expressed and highly regulated dimeric transcription factor that regulates the expression of genes responsible for innate and adaptive immunity, tissue regeneration, stress responses, apoptosis, cell proliferation, and differentiation [10]. NFκB has now been shown to contribute to the pathogenesis of a large number of diseases including cancer, diabetes, allergy, rheumatoid arthritis, Crohn’s disease, cardiovascular diseases, atherosclerosis, Alzheimer’s disease, muscular dystrophy, cardiac hypertrophy, catabolic disorders, hypercholesterolemia, ischemia/reperfusion [10].
III. NFκB SIGNALLING PATHWAY
NFκB belongs to the Rel family, comprising the following proteins: RelA (p65), c-Rel, RelB, NFκB 1 (p50/p105) and NFκB 2 (p52/100) [10,11]. While RelA, c-Rel and RelB are synthesized as final proteins, p50 and p52 derive from large precursors p105 and p100, respectively, after processing by the proteasome. The nuclear activity of NFκB is controlled by shuttling from the cytoplasm to the nucleus in response to cell stimulation. It has been demonstrated that NFκB activation depends on two different signalling pathways, which can be referred to as canonical and non-canonical pathway [12]. In the canonical pathway, NFκB dimers containing RelA or c-Rel are retained in the cytoplasm through interaction with the inhibitors of NFκB (IκBs). In response to a variety of stimuli, IκBs are phosphorylated (Ser32 and Ser36 for IκBα and Ser19 and Ser21 for IκBβ) by the activated IκB kinase (IKK) complex, followed by rapid ubiquitin-dependent degradation by the proteasome [12,13]. This allows NFκB dimers to translocate to the nucleus, where they stimulate the expression of target genes. IKK is composed of two catalytic subunits, IKKα and IKKβ (also known as IKK1 and IKK2), and an essential regulatory subunit, IKKγ (also known as NEMO) [12]. While IKKβ is mostly required for the canonical NFκB pathway that depends on IκB degradation [14–16], IKKα is involved in a non-canonical NFκB pathway that regulates, at least, the RelB/p52 dimer [17]. In resting cells, RelB is associated with p100 in the cytoplasm. Upon cell stimulation, the IκB-like C terminus of p100 is degraded, and the resulting RelB-p52 dimers translocate to the nucleus [18] (fig 1).
Fig 1.
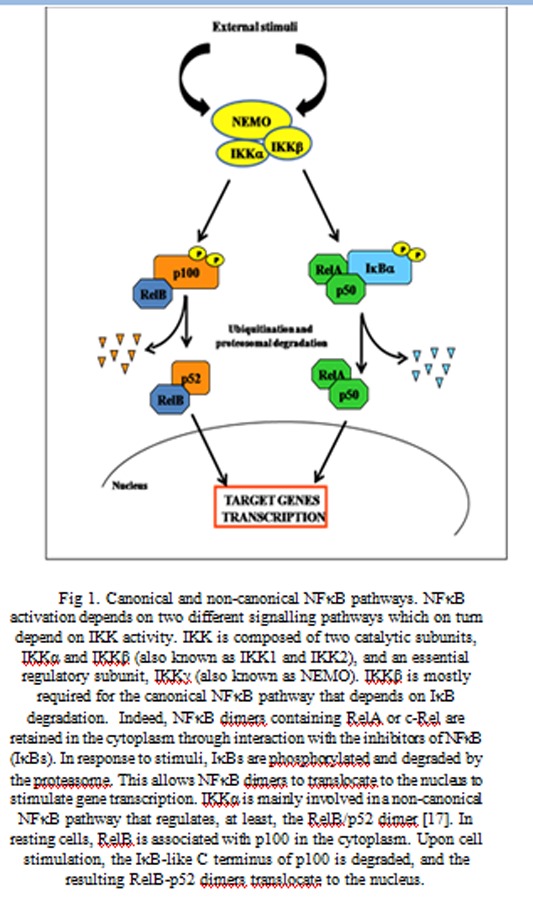
Canonical and non-canonical NFκB pathways. NFκB activation depends on two different signalling pathways which on turn depend on IKK activity. IKK is composed of two catalytic subunits, IKKα and IKKβ (also known as IKK1 and IKK2), and an essential regulatory subunit, IKKγ (also known as NEMO). IKKβ is mostly required for the canonical NFκB pathway that depends on IκB degradation. Indeed, NFκB dimers containing RelA or c-Rel are retained in the cytoplasm through interaction with the inhibitors of NFκB (IκBs). In response to stimuli, IκBs are phosphorylated and degraded by the proteasome. This allows NFκB dimers to translocate to the nucleus to stimulate gene transcription. IKKα is mainly involved in a non-canonical NFκB pathway that regulates, at least, the RelB/p52 dimer [17]. In resting cells, RelB is associated with p100 in the cytoplasm. Upon cell stimulation, the IκB-like C terminus of p100 is degraded, and the resulting RelB-p52 dimers translocate to the nucleus.
IV. NFκB ACTIVATION IN CANCER
Strong evidences suggest a key role of NFκB in cancer. According to Hanahan and Weinberg, the tumour genesis requires six essential alterations to normal cell physiology: self-sufficiency in growth signals; insensitivity to growth inhibition; evasion of apoptosis; immortalization; sustained angiogenesis; and tissue invasion and metastasis [1]. NFκB is able to regulate several of these cellular alterations (fig 2), and has been shown to be constitutively activated in some types of cancer cell [2,19,20].
Fig. 2.
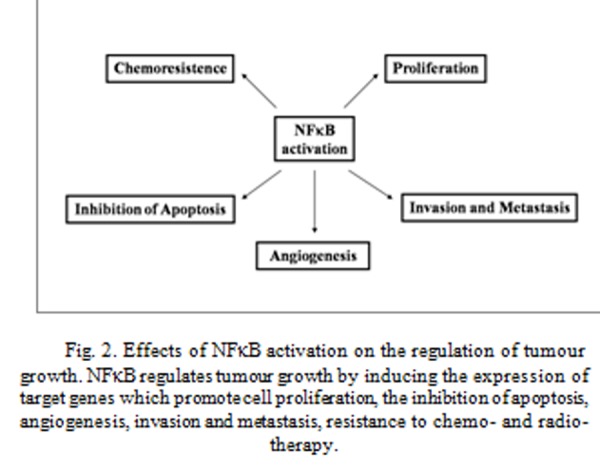
Effects of NFκB activation on the regulation of tumour growth. NFκB regulates tumour growth by inducing the expression of target genes which promote cell proliferation, the inhibition of apoptosis, angiogenesis, invasion and metastasis, resistance to chemo- and radio-therapy.
This phenomenon seems to be dependent on several mechanisms in different cancers: aberrant IKK activity, a shorter half-life of IκB in B-cell lymphoma, mutated IκB in Hodgkin’s lymphoma, IL-1β production in acute myelogenous leukaemia, TNF production in cutaneous T-cell lymphoma and Burkitt’s lymphoma [21,22]. It has been shown that the avian REV-T oncovirus produces the constitutively active v-REL oncoprotein, which causes rapidly progressing lymphomas and leukaemias [19,23]. The TAX oncoprotein of human T-cell leukaemia virus (HTLV)-1 has been shown to directly interact with the IKK complex, inducing its constitutively activation which results in the activation of both NFκB signalling pathways [19,24]. Other viral oncoproteins have also been shown to activate NFκB by means of different mechanisms [25]. Moreover, chromosomal amplification, rearrangement and other genetic aberrations of genes coding for NFκB family members are present in many solid tumours and cause NFκB activation [20]. Indeed, cancer-associated genetic modifications of genes encoding for NFκB and IκB proteins induce uncoupling of NFκB factors from their regulators, causing constitutive NFκB activation [19]. Finally, autocrine and paracrine production of pro-inflammatory cytokines, oncogenic activation of upstream signalling molecules and chronic infections have been shown to persistently stimulate IKK activity, which leads to constitutive NFκB activation [19].
V. EFFECTS OF NFκB ACTIVATION ON TUMOUR GROWTH
NFκB activation regulates tumour genesis by inducing the expression of target genes which promote cell proliferation, inhibition of apoptosis, angiogenesis, invasion and metastasis, resistance to chemo- and radio-therapy (fig 2).
A. NFκB and apoptosis
It has been demonstrated that NFκB exerts a dual function on apoptosis, either as an inhibitor or an activator, depending on stimuli, cell type and subunit involved [26–29].
For instance, it is generally accepted that NFκB activation is responsible of induction of apoptosis in cardiac cells [28] and apoptosis resistance in cancer cells [27]. This latter event occurs by inducing the expression of multiple anti-apoptotic proteins and interfering with the expression or activity of pro-apoptotic proteins. Indeed, NFκB may activate the transcription of several genes involved in the suppression of cell death by both mitochondrial (intrinsic) and death receptor (extrinsic) pathways [30]. The release of cytochrome c from mitochondria directly triggers caspase-3 activation through formation of the cytochrome c/Apaf-1/caspase-9-containing apoptosome complex [31]. It has been demonstrated that NFκB activation suppresses mitochondrial release of cytochrome c through the activation of the Bcl-2 family member A1/Bfl-1 [32]. NFκB may up-regulate the expression of proteins that interfere with the death receptor apoptotic pathway such as the FLICE-like inhibitory protein (FLIP) [33,34]. FLIP competes with caspase-8 for the binding to the Death-Inducing Signalling Complex (DISC). Thus, high levels of FLIP prevent caspase-8 recruitment to the DISC. It has been reported an up-regulation of FLIP in many tumours which could explain the resistance to death receptor apoptosis [35–39]. Other proteins, TRAF2 and TRAF6, activated by TNF may also be targets of NFκB and may lead to activation of pro-survival signalling [40]. NFκB also induces the expression of the Inhibitors of Apoptosis (IAPs) [41,42] and some members of the anti-apoptotic Bcl-2 family [43,44]. The IAPs (c-IAP1, c-IAP2, and XIAP) suppress apoptosis through direct inhibition of effector caspases (caspases-3, -6, -7, and 9) [40,45], while the anti-apoptotic members of the bcl-2 family antagonize the function of the pro-apoptotic members A1/BFL1 and Bcl-XL [46].
Furthermore, NFκB may interfere with the transcriptional activity of p53. In healthy cells, the level of p53 remains typically low under the control of Mdm2, which is responsible for p53 ubiquitination leading to its rapid degradation [47]. In turn, synthesis of Mdm2 transcript is controlled by p53 [48], which defines the negative feedback. DNA damage activates the checkpoint proteins, which destabilize Mdm2 and trigger p53 phosphorylation elevating its stability and transcriptional activity [49]. This disturbs the homeostatic balance between Mdm2 and p53 leading to oscillations and/or rise of the p53 level. Activated p53 triggers transcription of groups of genes, products of which are responsible for cell cycle arrest and DNA repair and, if the last fails or takes too long, for initiation of apoptosis. In tumour cells, NFκB inhibits p53-induced apoptosis, by up-regulating anti-apoptotic genes, and down-regulating p53 levels.
B. NFκB and proliferation
Several genes, such as TNF, IL-1β and IL-6, that mediate cell proliferation are under the transcriptional control of NFκB. Besides these growth factors, certain cell cycle regulatory proteins are also regulated by NFκB. In particular, NFκB promotes cell cycle progression, by regulating the expression of cyclins D1, D2, D3, cyclin E 50–53 and c-myc [54–56]. NFκB-induced cyclin D1 expression appears to be a key element in mammary gland development and breast carcinogenesis [57]. It was shown that growth factors like epithelial growth factor and platelet-derived growth factor induce proliferation of tumour cells through activation of NFκB [58]. It has been reported that proliferation of Hodgkin/Reed-Sternberg cells depends on activated NFκB [59,60]. As happens in apoptosis, NFκB exert a reciprocal regulation of cell proliferation by inducing inhibition or stimulation, depending on cell type. For example, NFκB activation can suppress the proliferation of keratinocytes 61 and c-Rel overexpression induces cell cycle arrest in HeLa cells 62. On the other hand, NFκB induces the expression of cell adhesion molecules (ICAM-1, E-selectin), and proteins involved in invasion (matrix metallo-proteinases). However, generally, in tumour cells NFκB induces cell proliferation and the expression of angiogenic factors.
C. NFκB and angiogenesis
Metastasis of cancer cells is a complex process involving multiple steps, including invasion, angiogenesis, trafficking of cancer cells through blood vessels, extravasations, organ specific homing, and growth. Proteins like matrix metalloproteinase 2 (MMP2), MMP9 and serine protease urokinase-type plasminogen activator (uPA) which play an important role in tumour invasion and metastasis, are under the transcription control of NFκB. Indeed, it has been demonstrated that NFκB blockade induces down-regulation of pro-metastatic MMP-9, uPA, and heparanase and reciprocal up-regulation of anti-metastatic TIMP-1 and -2 and PAI 2 [63]. Furthermore, NFκB regulates the expression of intracellular adhesion molecule 1 and vascular cell adhesion molecule 1 that are associated with tumour metastasis [64]. Tumour angiogenesis is regulated by chemokines (monocyte chemo-attractant protein-1, IL-8) and growth factors (TNF, VEGF) produced by macrophages, neutrophils and other inflammatory cells [65]. The production of these angiogenic factors has been shown to be regulated by NFκB activation [66,67]. It has been demonstrated that NFκB promotes breast cancer cell migration and metastasis by inducing the expression of the chemokine receptor CXCR4 [68]. Huang et al reported that blockade of NFκB signalling also inhibits angiogenesis of human ovarian cancer cells by suppressing expression of VEGF and IL-8 [69]. Cyclooxygenase 2, which is up-regulated in more aggressive forms of colorectal cancer, is known to be transcriptionally activated by NFκB and promote angiogenesis [70].
D. NFκB and chemo-resistance
Tumours with constitutive NFκB activation usually show increased resistance to chemotherapy [71]. It has been suggested that NFκB may induce the expression of the multidrug resistance P-glycoprotein, involved in the development of resistance to chemotherapy drugs in many cancers [72]. In some tumours, cells exposed to radiation or certain chemotherapeutic drugs show enhanced activation of NFκB [71]. On the other hand, inhibition of NFκB improves the apoptotic response to radiation therapy [71,73]. For instance, it has been found that inhibition of NFκB activation confers sensitivity to TNF-α by impairment of cell cycle progression in six human malignant glioma cell lines [73]. Inhibitors of NFκB activation can block the neoplastic transformation response. Indeed, inhibition of NFκB through adenoviral delivery of a modified form of IκB, a specific inhibitor of NFκB, has been reported to sensitize chemo-resistant tumours to the apoptotic potential of TNF-α and to the chemotherapeutic compound CPT-11, resulting in tumour regression [74].
VI. INFLAMMATION AND CANCER
A link between inflammation and cancer has been suspected for many years. While acute inflammation is a part of the defence response, chronic inflammation can mediate several diseases, including cardiovascular diseases, cancer, diabetes, arthritis, autoimmune diseases [75]. Since NFκB becomes activated in response to inflammatory stimuli and its constitutive activation has been associated with cancer, NFκB represents the link between these two processes. Indeed, several pro-inflammatory gene products have been associated to tumour genesis and they are all under the transcription control of NFκB. In particular, TNF, interleukins, chemokines, COX-2, 5-LOX, and MMP-9 have all a key role in cancer development [75,76].
A. Role of cytokines in cancer
Several inflammatory interleukins, including IL-1, IL-6, IL-8, and IL-18, are associated to tumour genesis. Secretion of IL-1α promotes growth of cervical carcinoma [77] while autocrine production of interleukin IL-1β promotes growth and confers chemoresistance in pancreatic carcinoma cell lines [78]. IL-1β secretion into the tumour milieu also induces several angiogenic factors from tumour and stromal cells that promotes tumour growth through an increase of neovascularization in lung carcinoma growth in vivo [79]. IL-6 acts as a paracrine growth factor for multiple myeloma, non-Hodgkin’s lymphoma, bladder cancer, colorectal cancer, and renal cell carcinoma (RCC) [80–84]. Several evidences underline the key role of TNF-α as mediator of inflammation and cancer [85,86]. Although initially thought to be a product only of macrophages, many malignant tumours are characterized by a constitutive production of TNF-α from the tumour microenvironment and its presence often associates with poor prognosis. Indeed, TNF-α is produced by a wide variety of tumour cells, including those of B cell lymphoma [87], cutaneous T cell lymphoma [88], megakaryoblastic leukaemia [89], adult T cell leukaemia [90], AML [91], CLL [92],ALL [93], breast carcinoma [94], colon carcinoma, lung carcinoma, squamous cell carcinoma, pancreatic cancer [95], ovarian carcinoma [96]. As TNF-α receptors are expressed on both epithelial and stromal cells, TNF-α can directly facilitate cancer development by regulating the proliferation and survival of neoplastic cells; alternatively it can also act on endothelial cells and other inflammatory cells present at the tumour microenvironment [97]. Tumour stromal cells, including macrophages, dendritic cells and fibroblasts, release several inflammatory cytokines, such as TNF-α, IL-1 and IL-6, which attract and recruit more inflammatory cells to the tumour microenvironment to further enhance the proliferation and survival of tumour cells. TNF-α is involved in all steps of tumour genesis, including cellular transformation, promotion, survival, proliferation, invasion, angiogenesis, and metastasis. Indeed, several reports indicate that TNF-α induces cellular transformation, proliferation, and tumour promotion [86,98–101]. First, TNF-α induces tumour initiation and promotion and enhances tumour cell proliferation. All these action are mediated by the activation of NFκB. Indeed, in mouse epidermal JB6 cells, TNF-α treatment increases NFκB activity in a dose dependent manner and TNF-α induced NFκB activation is essential for neoplastic transformation of these cells [102]. TNF-α also promotes tumour cell survival by inducing genes coding for NFκB dependent anti-apoptotic molecules [103]. In addition TNF-α not only acts as an autocrine growth factor but also induces the expression of other growth factors such as amphiregulin, EGFR and TGF-α, leading to increased tumour proliferation. For instance, in cervical cells TNF-α induces amphiregulin, which stimulates cell proliferation [77], whereas in pancreatic cells TNF-α induces the expression of epidermal growth factor receptor (EGFR) and transforming growth factor (TGF-α), which mediates proliferation. Finally TNF-α enhances tumour angiogenesis through different angiogenic factors such as IL-8 and VEGF, and also is a critical regulator of VEGF and jagged-1 expression via a JNK- and AP-1- dependent pathway [104].
It has been demonstrated that tumour necrosis factor (TNF-α) has a therapeutic role when expressed locally by the cells of the immune system [105]. The anti-cancer actions of TNF can be due to direct effects on tumour cells and/or indirect effects on host stroma, and many of these effects are potentiated by IFN-γ. Vascular damage is widely accepted as a mechanism of its anti-tumour effects. In a breast cancer xenograft model, locally injected human TNF resulted in growth inhibition of established tumours. However macroscopic necrosis was observed in these mice when systemic rat IFN-γ, which has no activity alone, was also given. Within 4 h of administration of this cytokine combination, platelet adherence to tumour cells was observed, followed by destruction of the tumour vasculature. Both necrosis and apoptosis of tumour cells was demonstrated and there was up-regulation of mRNA for a range of stromal cytokines and adhesion molecules [106].
TNF-α produced by tumours can act as an endogenous tumour promoter [98]. Komori’s group reported that human TNF-α is 1000 times more effective than the chemical tumour promoters okadaic acid and 12-O-tetradecanoylphorbol-13-acetate in inducing cancer [107]. In most of these cells, TNF-α acts as an autocrine growth factor, however in some cell types TNF-α induces the expression of other growth factors, which mediate proliferation of tumours. TNF-α has been reported to induce angiogenic factor up-regulation in malignant glioma cells [108] which in turn promotes angiogenesis and tumour progression. TNF-α could enhance invasiveness of some carcinomas or stimulate epithelial wound healing in vivo [109] and it has been even reported to mediate macrophage-induced angiogenesis [110].
B. Role of chemokines in cancer
The chemokines are soluble, small proteins that bind to their associate G-protein coupled receptors (GPCRs) to elicit a cellular response [111]. Tumour cells secrete and respond to chemokines, which in turn facilitate cancer growth through means of increased angiogenesis, inflammation, endothelial cell recruitment and cell migration. Furthermore, chemokines regulate the recruitment and trafficking of leukocytes to sites of inflammation. Chemokines are grouped into four classes based on the positions of key cysteine residues: C, CC, CXC, and CX3C. Different classes of chemokines recognize different subset of cells, expressing the corresponding receptor [112] (Table 1).
Table 1.
List of chemokines subfamilies and their specific target cell types
| CHEMOKINES SUBTYPE | TARGET CELL TYPES |
|---|---|
| C | B cells, T cells, natural killer cells, neutrophils |
| CC | Dendritic cells, lymphocytes, macrophages, eosinophils, natural killer cells |
| CXC | Neutrophils, lymphocytes, endothelial and epithelial cells |
| CX3C | Effector T cells |
Tumour cells also release soluble mediators such as VEGF-A (vascular endothelial growth factor-A), TGF-β and TNF-α that act on myeloid and endothelial cells and induce the expression of non-classical chemokines such as the S100 chemokine. Interestingly, S100 chemokines are implicated in targeting of the tumour cells to the pre-metastatic sites rather than the metastatic sites [113,114]. Evidence from murine models and human cancers suggests that CC chemokines are major determinants of macrophage and lymphocyte infiltration in melanoma, ovarian carcinoma, breast, and cervix, and in sarcomas and gliomas [115]. The chemokines elaborated from the tumour and the stromal cells bind to the chemokine receptors present on these cells. The two chemokine receptor–chemokine pairs that are involved commonly in many tumour are CXCR4–CXCL12 and CCR7–CCL21 [112]. Chemokine receptors CXCR4 and CCR7 are highly expressed in human breast cancer cells, malignant breast tumours, and metastasis [116]. Their respective ligands CXCL12/ SDF-1a and CCL21/6Ckine are highly expressed in organs representing the first destinations of breast cancer metastasis. In breast cancer cells, signalling through CXCR4 or CCR7 mediates actin polymerization and pseudopodia formation and subsequently induces chemotactic and invasive responses. In vivo, neutralizing the interactions of CXCL12/CXCR4 significantly impairs metastasis of breast cancer cells to regional lymph nodes and lung. Malignant melanomas show high expression levels of CCR10 in addition to CXCR4 and CCR7. Thus chemokines and their receptors have a critical role in determining the metastatic destination of tumour cells. Melanoma growth stimulatory activity/growth-regulated protein (MGSA/GRO), is a CXC chemokine constitutively expressed in melanoma tumours and is associated with constitutive NFκB activity [117]. Ovarian cancers express CXCR4 chemokine receptors [118]. Its ligand, CXCL12 (stromal cell-derived factor 1), in ovarian cancer cells stimulates cell migration and invasion through extracellular matrix, as well as DNA synthesis and EGFR transactivation [119,120].
C. Role of matrix metallo-proteinases in cancer
NFκB regulates several dependent-matrix metallo-proteinases (MMPs), which are correlated with malignant prognosis of various cancer types including colorectal, breast, and bladder cancers [121]. Indeed, the analyses on the human MMP-9 gene promoter revealed that NFκB is one of major transcription factors responsible for its induction [121]. MMPs are key modulators of many biological processes during pathophysiological events, such as skeletal formation, angiogenesis, cellular migration, inflammation, wound healing, and cancer [122]. By means of in vivo selection, transcriptomic analysis, functional verification and clinical validation, Minn et al have identified a set of genes comprising MMPs, that marks and mediates breast cancer metastasis to the lungs. In particular, MMP-2 acts mainly as virulence gene that may allow tumours to aggressively invade, colonize and grow in the lungs without markedly contributing to primary tumour growth, whereas MMP-1, determine metastatic potential of breast cancer to produce lung metastases [123]. MMP-7 also promotes cancer invasion by proteolytic cleavage of the extracellular matrix substrates and activates other MMPs, such as proMMP-2 and proMMP-9, to facilitate tumour invasion [124]. It has been demonstrated that transgenic mice lacking MMP-9 show reduced keratinocyte hyper proliferation at all neoplastic stages and a decreased incidence of invasive tumours [125]. Yet those carcinomas that do arise in the absence of MMP-9 show a greater loss of keratinocyte differentiation, indicative of a more aggressive and higher grade tumour [125].
VII. NFκB INHIBITION AND CANCER THERAPHY
It is known that a sustained, constitutive activation of NFκB contributes to malignant progression and therapeutic resistance in most of the major forms of human cancer, such as human lymphomas [60], carcinomas of the breast [126], prostate [127], lung [128], colon [129], pancreas [130], thyroid [131], head and neck [132] and cervix [133]. Thus, the modulation of NFκB activity could represent an useful therapeutic strategy for cancer, since NFκB inhibition promotes apoptotic events induced by chemotherapy, reduces the high proliferative rate that characterizes tumour cells and inhibits metastasis [134]. To date, different approaches have been developed to block NFκB in several conditions by regulating different steps in NFκB signalling pathway:
A. IKK inhibition
A protein that disrupts the association of the IKK complex is used to prevent inflammatory bone destruction [135]. Similarly, the inhibition of IκBα phosphorylation by the Bay 11-7082 compound, has been successfully used to prevent tumour growth and leukemic infiltration in a mouse model of adult T cell leukaemia [136]. The IKK inhibitors BAY 11-7082 and BAY 11-7085 also induce the apoptosis of colon cancer cells [137]. Some anti-inflammatory drugs and other substances such as curcumin, trans-resveratrol or parthenolide may inhibit NFκB by interfering with IKK activity [138–142]. Curcumin is a polyphenol derived from the plant Curcuma longa that exerts anti-oxidant, anti-inflammatory, anti-angiogenic and anti-tumoral activity. It was found to suppress COX-2 expression by inhibiting extracellular signal-regulated kinase (ERK) activity and NFκB in phorbol ester-induced mouse skin tumour genesis [143]. Non-steroidal anti-inflammatory agents (NSAIDs), including aspirin, have been shown to suppress NFκB activation by inhibiting IKK activation and IκBα degradation in tumour cells [144]. A small molecule inhibitor of IKK (PS-1145) was found to be selectively toxic for subtypes of diffuse large B-cell lymphoma cells that are associated with NFκB activation [2,145]. This compound was shown to lead to down-regulation of a set of NFκB-dependent genes [2].
B. IκB upregulation
The inhibition of NFκB activation by expression of a degradation, increased NFκB dependent apoptosis to stimuli such as TNFα [146]. Zhou et al, transfected the dominant-negative mutant inhibitor of NFκB (IκBm) into an acute lymphoblastic leukaemia (ALL) cell line with constitutive NFκB activation [147]. Overexpression of IκBm simultaneously down-regulates NFκB activation and sequesters p53 in the cytoplasm, thus enhancing NFκB-regulated apoptosis but blocking p53-dependent apoptosis [147]. We have demonstrated that in vitro, adenovirus mediated overexpression of the RH domain of GRK5 (AdGRK5-NT) in human tumour cells (KAT-4) induces IκB accumulation and inhibits NFκB transcriptional activity leading to apoptotic events 27. In BALB/c nude mice harbouring KAT-4 induced neoplasias, intra-tumour delivery of AdGRK5-NT reduces in a dose-dependent fashion tumour growth, with the highest doses completely inhibiting it. This phenomenon is paralleled by a decrease of NFκB activity, an increase of IκB levels and apoptotic events [27]. To move towards a pharmacological setup, we synthesized the TAT-RH protein. In cultured KAT-4 cells, different dosages of TAT-RH reduced cell survival and increased apoptosis. In BALB/c mice, the anti-proliferative effects of TAT-RH appear to be dose-dependent and highest dose completely inhibits tumor growth [27] (fig 3).
Fig 3.
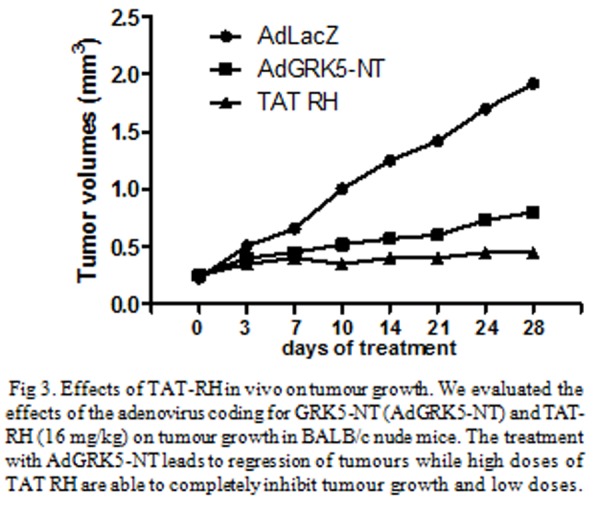
Effects of TAT-RH in vivo on tumour growth. We evaluated the effects of the adenovirus coding for GRK5-NT (AdGRK5-NT) and TAT-RH (16 mg/kg) on tumour growth in BALB/c nude mice. The treatment with AdGRK5-NT leads to regression of tumours while high doses of TAT RH are able to completely inhibit tumour growth and low doses.
C. Proteasome inhibition
Another way to approach NFκB inhibition is to target the process of proteasome degradation. Proteasome inhibitors prevent NFκB activation by blocking the degradation of IκBs, NFκB1/p105 or NFκB2/p100. A successful strategy is using a proteasome inhibitor, Bortezomib or PS-341, to treat patients with refractory or resistant multiple myeloma [148]. Bortezomib is a dipeptidyl boronic acid that specifically inhibits 26S proteasome, the principal regulator of intracellular protein degradation like IκB. The treatment with this compound alone or in combination with other drugs, inhibits proliferation and induces apoptosis in several solid tumours [149–153], and is currently approved for treatment of multiple myeloma [152]. The importance of NFκB in multiple myeloma is suggested from its involvement downstream of CD40, the TNF receptor family member that is expressed in a variety of B-cell malignancies and which is associated with multiple myeloma homing. Consistent with this, monoclonal antibodies to CD40 block CD40L-induced NFκB activation as well as IL-6 and VEGF secretion in cultures of multiple myeloma cells and bone marrow-derived stromal cells. Other haematological malignancies are susceptible to NFκB inhibition. Proteasome inhibition blocks cell growth and induces apoptosis in adult T-cell leukaemia, an NFκB-relevant malignancy, correlated with stabilized IκBα and inhibited NFκB [2,153].
All these approaches open new fields for the management of NFκB-associated diseases like cancer. Clinical trials are being performed with some of the above described drugs and more other compounds that are able to block NFκB activity but the most significant clinical data comes from studies with the protease inhibitor bortezomib.
VIII. CONCLUSIONS AND FUTURE PROSPECTS
It is now well established that NFκB has a key role in carcinogenesis and that the inhibition of NFκB is a promising strategy for cancer therapy. Therefore, an increasing number of compounds able to block NFκB activity at different stages of its signalling pathway have been tested. Most of these drugs have given promising results in preclinical models of tumour (pancreas, lung, colon, ovarian and breast cancer), but failed in the clinical efficacy. Actually, the only pharmacological inhibitors of NFκB approved for clinical use are proteasome inhibitors for treatment of multiple myeloma or adult T-cell leukaemia, for whose pathogenesis it has been clearly demonstrated the key role of NFκB. The difficulty to find an efficient drug for cancer treatment is due to the fact that these drugs are able to block not only the oncogenic activity of NFκB but also its physiological roles in immunity, inflammation and cellular homeostasis. Moreover, the treatment is not specifically targeted on tumour cells thus affecting also healthy cells. Finally, these drugs induce many highly toxic side effects. In the future, new drugs might be designed that should be more specific in their function, in order to avoid affecting the induction of genes that are required for immunity, and in cell targeting, in order to protect normal cells from death.
REFERENCES
- [1].Hanahan D, Weinberg RA. The hallmarks of cancer. Cell. 2000 Jan 7;100(1):57–70. doi: 10.1016/s0092-8674(00)81683-9. [DOI] [PubMed] [Google Scholar]
- [2].Kim HJ, Hawke N, Baldwin AS. NF-kappaB and IKK as therapeutic targets in cancer. Cell Death Differ. 2006 May;13(5):738–747. doi: 10.1038/sj.cdd.4401877. [DOI] [PubMed] [Google Scholar]
- [3].Downward J. PI 3-kinase, Akt and cell survival. Semin Cell Dev Biol. 2004 Apr;15(2):177–182. doi: 10.1016/j.semcdb.2004.01.002. [DOI] [PubMed] [Google Scholar]
- [4].Latchman DS. Transcription factors: an overview. Int J Biochem Cell Biol. 1997 Dec;29(12):1305–1312. doi: 10.1016/s1357-2725(97)00085-x. [DOI] [PubMed] [Google Scholar]
- [5].Vaquerizas JM, Kummerfeld SK, Teichmann SA, Luscombe NM. A census of human transcription factors: function, expression and evolution. Nat Rev Genet. 2009 Apr;10(4):252–263. doi: 10.1038/nrg2538. [DOI] [PubMed] [Google Scholar]
- [6].Narlikar GJ, Fan HY, Kingston RE. Cooperation between complexes that regulate chromatin structure and transcription. Cell. 2002 Feb 22;108(4):475–487. doi: 10.1016/s0092-8674(02)00654-2. [DOI] [PubMed] [Google Scholar]
- [7].Xu L, Glass CK, Rosenfeld MG. Coactivator and corepressor complexes in nuclear receptor function. Curr Opin Genet Dev. 1999 Apr;9(2):140–147. doi: 10.1016/S0959-437X(99)80021-5. [DOI] [PubMed] [Google Scholar]
- [8].Engelkamp D, van Heyningen V. Transcription factors in disease. Curr Opin Genet Dev. 1996 Jun;6(3):334–342. doi: 10.1016/s0959-437x(96)80011-6. [DOI] [PubMed] [Google Scholar]
- [9].Nebert DW. Transcription factors and cancer: an overview. Toxicology. 2002 Dec 27;181–182:131–141. doi: 10.1016/s0300-483x(02)00269-x. [DOI] [PubMed] [Google Scholar]
- [10].Ghosh S, Karin M. Missing pieces in the NF-kappaB puzzle. Cell. 2002 Apr;109(Suppl):S81–96. doi: 10.1016/s0092-8674(02)00703-1. [DOI] [PubMed] [Google Scholar]
- [11].Baldwin AS. The NF-kappa B and I kappa B proteins: new discoveries and insights. Annu Rev Immunol. 1996;14:649–683. doi: 10.1146/annurev.immunol.14.1.649. [DOI] [PubMed] [Google Scholar]
- [12].Lin A, Karin M. NF-kappaB in cancer: a marked target. Semin Cancer Biol. 2003 Apr;13(2):107–114. doi: 10.1016/s1044-579x(02)00128-1. [DOI] [PubMed] [Google Scholar]
- [13].Karin M, Ben-Neriah Y. Phosphorylation meets ubiquitination: the control of NF-[kappa]B activity. Annu Rev Immunol. 2000;18:621–663. doi: 10.1146/annurev.immunol.18.1.621. [DOI] [PubMed] [Google Scholar]
- [14].Li ZW, Chu W, Hu Y, et al. The IKKbeta subunit of IkappaB kinase (IKK) is essential for nuclear factor kappaB activation and prevention of apoptosis. J Exp Med. 1999 Jun 7;189(11):1839–1845. doi: 10.1084/jem.189.11.1839. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [15].Li Q, Van Antwerp D, Mercurio F, Lee KF, Verma IM. Severe liver degeneration in mice lacking the IkappaB kinase 2 gene. Science. 1999 Apr 9;284(5412):321–325. doi: 10.1126/science.284.5412.321. [DOI] [PubMed] [Google Scholar]
- [16].Tanaka M, Fuentes ME, Yamaguchi K, et al. Embryonic lethality, liver degeneration, and impaired NF-kappa B activation in IKK-beta-deficient mice. Immunity. 1999 Apr;10(4):421–429. doi: 10.1016/s1074-7613(00)80042-4. [DOI] [PubMed] [Google Scholar]
- [17].Senftleben U, Li ZW, Baud V, Karin M. IKKbeta is essential for protecting T cells from TNFalpha-induced apoptosis. Immunity. 2001 Mar;14(3):217–230. doi: 10.1016/s1074-7613(01)00104-2. [DOI] [PubMed] [Google Scholar]
- [18].Solan NJ, Miyoshi H, Carmona EM, Bren GD, Paya CV. RelB cellular regulation and transcriptional activity are regulated by p100. J Biol Chem. 2002 Jan 11;277(2):1405–1418. doi: 10.1074/jbc.M109619200. [DOI] [PubMed] [Google Scholar]
- [19].Karin M, Cao Y, Greten FR, Li ZW. NF-kappaB in cancer: from innocent bystander to major culprit. Nat Rev Cancer. 2002 Apr;2(4):301–310. doi: 10.1038/nrc780. [DOI] [PubMed] [Google Scholar]
- [20].Rayet B, Gelinas C. Aberrant rel/nfkb genes and activity in human cancer. Oncogene. 1999 Nov 22;18(49):6938–6947. doi: 10.1038/sj.onc.1203221. [DOI] [PubMed] [Google Scholar]
- [21].Garg A, Aggarwal BB. Nuclear transcription factor-kappaB as a target for cancer drug development. Leukemia. 2002 Jun;16(6):1053–1068. doi: 10.1038/sj.leu.2402482. [DOI] [PubMed] [Google Scholar]
- [22].Lee CH, Jeon YT, Kim SH, Song YS. NF-kappaB as a potential molecular target for cancer therapy. Biofactors. 2007;29(1):19–35. doi: 10.1002/biof.5520290103. [DOI] [PubMed] [Google Scholar]
- [23].Gilmore TD. Multiple mutations contribute to the oncogenicity of the retroviral oncoprotein v-Rel. Oncogene. 1999 Nov 22;18(49):6925–6937. doi: 10.1038/sj.onc.1203222. [DOI] [PubMed] [Google Scholar]
- [24].Xiao G, Cvijic ME, Fong A, et al. Retroviral oncoprotein Tax induces processing of NF-kappaB2/p100 in T cells: evidence for the involvement of IKKalpha. EMBO J. 2001 Dec 3;20(23):6805–6815. doi: 10.1093/emboj/20.23.6805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Mosialos G. The role of Rel/NF-kappa B proteins in viral oncogenesis and the regulation of viral transcription. Semin Cancer Biol. 1997 Apr;8(2):121–129. doi: 10.1006/scbi.1997.0063. [DOI] [PubMed] [Google Scholar]
- [26].Bours V, Bentires-Alj M, Hellin AC, et al. Nuclear factor-kappa B, cancer, and apoptosis. Biochem Pharmacol. 2000 Oct 15;60(8):1085–1089. doi: 10.1016/s0006-2952(00)00391-9. [DOI] [PubMed] [Google Scholar]
- [27].Sorriento D, Campanile A, Santulli G, et al. A new synthetic protein, TAT-RH, inhibits tumor growth through the regulation of NFkappaB activity. Mol Cancer. 2009;8:97. doi: 10.1186/1476-4598-8-97. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Sorriento D, Santulli G, Fusco A, Anastasio A, Trimarco B, Iaccarino G. Intracardiac injection of AdGRK5-NT reduces left ventricular hypertrophy by inhibiting NF-kappaB-dependent hypertrophic gene expression. Hypertension. Oct;56(4):696–704. doi: 10.1161/HYPERTENSIONAHA.110.155960. [DOI] [PubMed] [Google Scholar]
- [29].Puszynski K, Bertolusso R, Lipniacki T. Crosstalk between p53 and nuclear factor-B systems: pro- and anti-apoptotic functions of NF-B. IET Syst Biol. 2009 Sep;3(5):356–367. doi: 10.1049/iet-syb.2008.0172. [DOI] [PubMed] [Google Scholar]
- [30].Fulda S, Debatin KM. Extrinsic versus intrinsic apoptosis pathways in anticancer chemotherapy. Oncogene. 2006 Aug 7;25(34):4798–4811. doi: 10.1038/sj.onc.1209608. [DOI] [PubMed] [Google Scholar]
- [31].Cain K, Bratton SB, Langlais C, et al. Apaf-1 oligomerizes into biologically active approximately 700-kDa and inactive approximately 1.4-MDa apoptosome complexes. J Biol Chem. 2000 Mar 3;275(9):6067–6070. doi: 10.1074/jbc.275.9.6067. [DOI] [PubMed] [Google Scholar]
- [32].Wang CY, Guttridge DC, Mayo MW, Baldwin AS. NF-kappaB induces expression of the Bcl-2 homologue A1/Bfl-1 to preferentially suppress chemotherapy-induced apoptosis. Mol Cell Biol. 1999 Sep;19(9):5923–5929. doi: 10.1128/mcb.19.9.5923. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Kreuz S, Siegmund D, Scheurich P, Wajant H. NF-kappaB inducers upregulate cFLIP, a cycloheximide-sensitive inhibitor of death receptor signaling. Mol Cell Biol. 2001 Jun;21(12):3964–3973. doi: 10.1128/MCB.21.12.3964-3973.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Micheau O, Lens S, Gaide O, Alevizopoulos K, Tschopp J. NF-kappaB signals induce the expression of c-FLIP. Mol Cell Biol. 2001 Aug;21(16):5299–5305. doi: 10.1128/MCB.21.16.5299-5305.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [35].Bullani RR, Huard B, Viard-Leveugle I, et al. Selective expression of FLIP in malignant melanocytic skin lesions. J Invest Dermatol. 2001 Aug;117(2):360–364. doi: 10.1046/j.0022-202x.2001.01418.x. [DOI] [PubMed] [Google Scholar]
- [36].Griffith TS, Chin WA, Jackson GC, Lynch DH, Kubin MZ. Intracellular regulation of TRAIL-induced apoptosis in human melanoma cells. J Immunol. 1998 Sep 15;161(6):2833–2840. [PubMed] [Google Scholar]
- [37].Irisarri M, Plumas J, Bonnefoix T, et al. Resistance to CD95-mediated apoptosis through constitutive c-FLIP expression in a non-Hodgkin’s lymphoma B cell line. Leukemia. 2000 Dec;14(12):2149–2158. doi: 10.1038/sj.leu.2401954. [DOI] [PubMed] [Google Scholar]
- [38].Irmler M, Thome M, Hahne M, et al. Inhibition of death receptor signals by cellular FLIP. Nature. 1997 Jul 10;388(6638):190–195. doi: 10.1038/40657. [DOI] [PubMed] [Google Scholar]
- [39].Panka DJ, Mano T, Suhara T, Walsh K, Mier JW. Phosphatidylinositol 3-kinase/Akt activity regulates c-FLIP expression in tumor cells. J Biol Chem. 2001 Mar 9;276(10):6893–6896. doi: 10.1074/jbc.C000569200. [DOI] [PubMed] [Google Scholar]
- [40].Wang CY, Mayo MW, Korneluk RG, Goeddel DV, Baldwin AS. NF-kappaB antiapoptosis: induction of TRAF1 and TRAF2 and c-IAP1 and c-IAP2 to suppress caspase-8 activation. Science. 1998 Sep 11;281(5383):1680–1683. doi: 10.1126/science.281.5383.1680. [DOI] [PubMed] [Google Scholar]
- [41].Takahashi R, Deveraux Q, Tamm I, et al. A single BIR domain of XIAP sufficient for inhibiting caspases. J Biol Chem. 1998 Apr 3;273(14):7787–7790. doi: 10.1074/jbc.273.14.7787. [DOI] [PubMed] [Google Scholar]
- [42].Deveraux QL, Roy N, Stennicke HR, et al. IAPs block apoptotic events induced by caspase-8 and cytochrome c by direct inhibition of distinct caspases. EMBO J. 1998 Apr 15;17(8):2215–2223. doi: 10.1093/emboj/17.8.2215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Chen QM, Tu VC. Apoptosis and heart failure: mechanisms and therapeutic implications. Am J Cardiovasc Drugs. 2002;2(1):43–57. doi: 10.2165/00129784-200202010-00006. [DOI] [PubMed] [Google Scholar]
- [44].Lee JU, Hosotani R, Wada M, et al. Role of Bcl-2 family proteins (Bax, Bcl-2 and Bcl-X) on cellular susceptibility to radiation in pancreatic cancer cells. Eur J Cancer. 1999 Sep;35(9):1374–1380. doi: 10.1016/s0959-8049(99)00134-3. [DOI] [PubMed] [Google Scholar]
- [45].Chu ZL, McKinsey TA, Liu L, Gentry JJ, Malim MH, Ballard DW. Suppression of tumor necrosis factor-induced cell death by inhibitor of apoptosis c-IAP2 is under NF-kappaB control. Proc Natl Acad Sci U S A. 1997 Sep 16;94(19):10057–10062. doi: 10.1073/pnas.94.19.10057. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Lin EY, Orlofsky A, Berger MS, Prystowsky MB. Characterization of A1, a novel hemopoietic-specific early-response gene with sequence similarity to bcl-2. J Immunol. 1993 Aug 15;151(4):1979–1988. [PubMed] [Google Scholar]
- [47].Haupt Y, Maya R, Kazaz A, Oren M. Mdm2 promotes the rapid degradation of p53. Nature. 1997 May 15;387(6630):296–299. doi: 10.1038/387296a0. [DOI] [PubMed] [Google Scholar]
- [48].Barak Y, Juven T, Haffner R, Oren M. mdm2 expression is induced by wild type p53 activity. EMBO J. 1993 Feb;12(2):461–468. doi: 10.1002/j.1460-2075.1993.tb05678.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [49].Vogelstein B, Lane D, Levine AJ. Surfing the p53 network. Nature. 2000 Nov 16;408(6810):307–310. doi: 10.1038/35042675. [DOI] [PubMed] [Google Scholar]
- [50].Guttridge DC, Albanese C, Reuther JY, Pestell RG, Baldwin AS., Jr NF-kappaB controls cell growth and differentiation through transcriptional regulation of cyclin D1. Mol Cell Biol. 1999 Aug;19(8):5785–5799. doi: 10.1128/mcb.19.8.5785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [51].Hinz M, Krappmann D, Eichten A, Heder A, Scheidereit C, Strauss M. NF-kappaB function in growth control: regulation of cyclin D1 expression and G0/G1-to-S-phase transition. Mol Cell Biol. 1999 Apr;19(4):2690–2698. doi: 10.1128/mcb.19.4.2690. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Hinz M, Loser P, Mathas S, Krappmann D, Dorken B, Scheidereit C. Constitutive NF-kappaB maintains high expression of a characteristic gene network, including CD40, CD86, and a set of antiapoptotic genes in Hodgkin/Reed-Sternberg cells. Blood. 2001 May 1;97(9):2798–2807. doi: 10.1182/blood.v97.9.2798. [DOI] [PubMed] [Google Scholar]
- [53].Hsia CY, Cheng S, Owyang AM, Dowdy SF, Liou HC. c-Rel regulation of the cell cycle in primary mouse B lymphocytes. Int Immunol. 2002 Aug;14(8):905–916. doi: 10.1093/intimm/dxf055. [DOI] [PubMed] [Google Scholar]
- [54].Chen F, Castranova V, Shi X. New insights into the role of nuclear factor-kappaB in cell growth regulation. Am J Pathol. 2001 Aug;159(2):387–397. doi: 10.1016/s0002-9440(10)61708-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Duyao MP, Kessler DJ, Spicer DB, et al. Transactivation of the c-myc promoter by human T cell leukemia virus type 1 tax is mediated by NF kappa B. J Biol Chem. 1992 Aug 15;267(23):16288–16291. [PubMed] [Google Scholar]
- [56].Thornburg NJ, Pathmanathan R, Raab-Traub N. Activation of nuclear factor-kappaB p50 homodimer/Bcl-3 complexes in nasopharyngeal carcinoma. Cancer Res. 2003 Dec 1;63(23):8293–8301. [PubMed] [Google Scholar]
- [57].Yu Q, Geng Y, Sicinski P. Specific protection against breast cancers by cyclin D1 ablation. Nature. 2001 Jun 28;411(6841):1017–1021. doi: 10.1038/35082500. [DOI] [PubMed] [Google Scholar]
- [58].Jiang T, Grabiner B, Zhu Y, et al. CARMA3 is crucial for EGFR-Induced activation of NF-kappaB and tumor progression. Cancer Res. Mar 15;71(6):2183–2192. doi: 10.1158/0008-5472.CAN-10-3626. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [59].Mathas S, Hinz M, Anagnostopoulos I, et al. Aberrantly expressed c-Jun and JunB are a hallmark of Hodgkin lymphoma cells, stimulate proliferation and synergize with NF-kappa B. EMBO J. 2002 Aug 1;21(15):4104–4113. doi: 10.1093/emboj/cdf389. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Bargou RC, Emmerich F, Krappmann D, et al. Constitutive nuclear factor-kappaB-RelA activation is required for proliferation and survival of Hodgkin’s disease tumor cells. J Clin Invest. 1997 Dec 15;100(12):2961–2969. doi: 10.1172/JCI119849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Hinata K, Gervin AM, Jennifer Zhang Y, Khavari PA. Divergent gene regulation and growth effects by NF-kappa B in epithelial and mesenchymal cells of human skin. Oncogene. 2003 Apr 3;22(13):1955–1964. doi: 10.1038/sj.onc.1206198. [DOI] [PubMed] [Google Scholar]
- [62].Bash J, Zong WX, Gelinas C. c-Rel arrests the proliferation of HeLa cells and affects critical regulators of the G1/S-phase transition. Mol Cell Biol. 1997 Nov;17(11):6526–6536. doi: 10.1128/mcb.17.11.6526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Andela VB, Schwarz EM, Puzas JE, O’Keefe RJ, Rosier RN. Tumor metastasis and the reciprocal regulation of prometastatic and antimetastatic factors by nuclear factor kappaB. Cancer Res. 2000 Dec 1;60(23):6557–6562. [PubMed] [Google Scholar]
- [64].Johnson JP. Cell adhesion molecules in the development and progression of malignant melanoma. Cancer Metastasis Rev. 1999;18(3):345–357. doi: 10.1023/a:1006304806799. [DOI] [PubMed] [Google Scholar]
- [65].Loch T, Michalski B, Mazurek U, Graniczka M. [Vascular endothelial growth factor (VEGF) and its role in neoplastic processes] Postepy Hig Med Dosw. 2001;55(2):257–274. [PubMed] [Google Scholar]
- [66].Chilov D, Kukk E, Taira S, et al. Genomic organization of human and mouse genes for vascular endothelial growth factor C. J Biol Chem. 1997 Oct 3;272(40):25176–25183. doi: 10.1074/jbc.272.40.25176. [DOI] [PubMed] [Google Scholar]
- [67].Huang S, DeGuzman A, Bucana CD, Fidler IJ. Nuclear factor-kappaB activity correlates with growth, angiogenesis, and metastasis of human melanoma cells in nude mice. Clin Cancer Res. 2000 Jun;6(6):2573–2581. [PubMed] [Google Scholar]
- [68].Helbig G, Christopherson KW, Bhat-Nakshatri P, et al. NF-kappaB promotes breast cancer cell migration and metastasis by inducing the expression of the chemokine receptor CXCR4. J Biol Chem. 2003 Jun 13;278(24):21631–21638. doi: 10.1074/jbc.M300609200. [DOI] [PubMed] [Google Scholar]
- [69].Huang S, Robinson JB, Deguzman A, Bucana CD, Fidler IJ. Blockade of nuclear factor-kappaB signaling inhibits angiogenesis and tumorigenicity of human ovarian cancer cells by suppressing expression of vascular endothelial growth factor and interleukin 8. Cancer Res. 2000 Oct 1;60(19):5334–5339. [PubMed] [Google Scholar]
- [70].Tsujii M, Kawano S, Tsuji S, Sawaoka H, Hori M, DuBois RN. Cyclooxygenase regulates angiogenesis induced by colon cancer cells. Cell. 1998 May 29;93(5):705–716. doi: 10.1016/s0092-8674(00)81433-6. [DOI] [PubMed] [Google Scholar]
- [71].Aggarwal BB, Shishodia S, Sandur SK, Pandey MK, Sethi G. Inflammation and cancer: how hot is the link? Biochem Pharmacol. 2006 Nov 30;72(11):1605–1621. doi: 10.1016/j.bcp.2006.06.029. [DOI] [PubMed] [Google Scholar]
- [72].F Thevenod F, Friedmann JM, Katsen AD, Hauser IA. Up-regulation of multidrug resistance P-glycoprotein via nuclear factor-kappaB activation protects kidney proximal tubule cells from cadmium- and reactive oxygen species-induced apoptosis. J Biol Chem. 2000 Jan 21;275(3):1887–1896. doi: 10.1074/jbc.275.3.1887. [DOI] [PubMed] [Google Scholar]
- [73].Otsuka G, Nagaya T, Saito K, Mizuno M, Yoshida J, Seo H. Inhibition of nuclear factor-kappaB activation confers sensitivity to tumor necrosis factor-alpha by impairment of cell cycle progression in human glioma cells. Cancer Res. 1999 Sep 1;59(17):4446–4452. [PubMed] [Google Scholar]
- [74].Wang CY, Cusack JC, Liu R, Baldwin AS. Control of inducible chemoresistance: enhanced anti-tumor therapy through increased apoptosis by inhibition of NF-kappaB. Nat Med. 1999 Apr;5(4):412–417. doi: 10.1038/7410. [DOI] [PubMed] [Google Scholar]
- [75].Aggarwal BB. Nuclear factor-kappaB: the enemy within. Cancer Cell. 2004 Sep;6(3):203–208. doi: 10.1016/j.ccr.2004.09.003. [DOI] [PubMed] [Google Scholar]
- [76].Shishodia S, Aggarwal BB. Nuclear factor-kappaB: a friend or a foe in cancer? Biochem Pharmacol. 2004 Sep 15;68(6):1071–1080. doi: 10.1016/j.bcp.2004.04.026. [DOI] [PubMed] [Google Scholar]
- [77].Woodworth CD, McMullin E, Iglesias M, Plowman GD. Interleukin 1 alpha and tumor necrosis factor alpha stimulate autocrine amphiregulin expression and proliferation of human papillomavirus-immortalized and carcinoma-derived cervical epithelial cells. Proc Natl Acad Sci U S A. 1995 Mar 28;92(7):2840–2844. doi: 10.1073/pnas.92.7.2840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [78].Arlt A, Vorndamm J, Muerkoster S, et al. Autocrine production of interleukin 1beta confers constitutive nuclear factor kappaB activity and chemoresistance in pancreatic carcinoma cell lines. Cancer Res. 2002 Feb 1;62(3):910–916. [PubMed] [Google Scholar]
- [79].Saijo Y, Tanaka M, Miki M, et al. Proinflammatory cytokine IL-1 beta promotes tumor growth of Lewis lung carcinoma by induction of angiogenic factors: in vivo analysis of tumor-stromal interaction. J Immunol. 2002 Jul 1;169(1):469–475. doi: 10.4049/jimmunol.169.1.469. [DOI] [PubMed] [Google Scholar]
- [80].Klein B, Zhang XG, Jourdan M, et al. Paracrine rather than autocrine regulation of myeloma-cell growth and differentiation by interleukin-6. Blood. 1989 Feb;73(2):517–526. [PubMed] [Google Scholar]
- [81].Voorzanger N, Touitou R, Garcia E, et al. Interleukin (IL)-10 and IL-6 are produced in vivo by non-Hodgkin’s lymphoma cells and act as cooperative growth factors. Cancer Res. 1996 Dec 1;56(23):5499–5505. [PubMed] [Google Scholar]
- [82].Okamoto M, Kawamata H, Kawai K, Oyasu R. Enhancement of transformation in vitro of a nontumorigenic rat urothelial cell line by interleukin 6. Cancer Res. 1995 Oct 15;55(20):4581–4585. [PubMed] [Google Scholar]
- [83].Landi S, Moreno V, Gioia-Patricola L, et al. Association of common polymorphisms in inflammatory genes interleukin (IL)6, IL8, tumor necrosis factor alpha, NFKB1, and peroxisome proliferator-activated receptor gamma with colorectal cancer. Cancer Res. 2003 Jul 1;63(13):3560–3566. [PubMed] [Google Scholar]
- [84].Angelo LS, Talpaz M, Kurzrock R. Autocrine interleukin-6 production in renal cell carcinoma: evidence for the involvement of p53. Cancer Res. 2002 Feb 1;62(3):932–940. [PubMed] [Google Scholar]
- [85].Sethi G, Sung B, Aggarwal BB. TNF: a master switch for inflammation to cancer. Front Biosci. 2008;13:5094–5107. doi: 10.2741/3066. [DOI] [PubMed] [Google Scholar]
- [86].Balkwill F. Tumour necrosis factor and cancer. Nat Rev Cancer. 2009 May;9(5):361–371. doi: 10.1038/nrc2628. [DOI] [PubMed] [Google Scholar]
- [87].Digel W, Stefanic M, Schoniger W, et al. Tumor necrosis factor induces proliferation of neoplastic B cells from chronic lymphocytic leukemia. Blood. 1989 Apr;73(5):1242–1246. [PubMed] [Google Scholar]
- [88].Giri DK, Aggarwal BB. Constitutive activation of NF-kappaB causes resistance to apoptosis in human cutaneous T cell lymphoma HuT-78 cells. Autocrine role of tumor necrosis factor and reactive oxygen intermediates. J Biol Chem. 1998 May 29;273(22):14008–14014. doi: 10.1074/jbc.273.22.14008. [DOI] [PubMed] [Google Scholar]
- [89].Liu RY, Fan C, Mitchell S, Chen Q, Wu J, Zuckerman KS. The role of type I and type II tumor necrosis factor (TNF) receptors in the ability of TNF-alpha to transduce a proliferative signal in the human megakaryoblastic leukemic cell line Mo7e. Cancer Res. 1998 May 15;58(10):2217–2223. [PubMed] [Google Scholar]
- [90].Tsukasaki K, Miller CW, Kubota T, et al. Tumor necrosis factor alpha polymorphism associated with increased susceptibility to development of adult T-cell leukemia/lymphoma in human T-lymphotropic virus type 1 carriers. Cancer Res. 2001 May 1;61(9):3770–3774. [PubMed] [Google Scholar]
- [91].Stifter G, Heiss S, Gastl G, Tzankov A, Stauder R. Over-expression of tumor necrosis factor-alpha in bone marrow biopsies from patients with myelodysplastic syndromes: relationship to anemia and prognosis. Eur J Haematol. 2005 Dec;75(6):485–491. doi: 10.1111/j.1600-0609.2005.00551.x. [DOI] [PubMed] [Google Scholar]
- [92].Duncombe AS, Heslop HE, Turner M, et al. Tumor necrosis factor mediates autocrine growth inhibition in a chronic leukemia. J Immunol. 1989 Dec 1;143(11):3828–3834. [PubMed] [Google Scholar]
- [93].Elbaz O, Mahmoud LA. Tumor necrosis factor and human acute leukemia. Leuk Lymphoma. 1994 Jan;12(3–4):191–195. doi: 10.3109/10428199409059589. [DOI] [PubMed] [Google Scholar]
- [94].Montesano R, Soulie P, Eble JA, Carrozzino F. Tumour necrosis factor alpha confers an invasive, transformed phenotype on mammary epithelial cells. J Cell Sci. 2005 Aug 1;118(Pt 15):3487–3500. doi: 10.1242/jcs.02467. [DOI] [PubMed] [Google Scholar]
- [95].Schmiegel W, Roeder C, Schmielau J, Rodeck U, Kalthoff H. Tumor necrosis factor alpha induces the expression of transforming growth factor alpha and the epidermal growth factor receptor in human pancreatic cancer cells. Proc Natl Acad Sci U S A. 1993 Feb 1;90(3):863–867. doi: 10.1073/pnas.90.3.863. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [96].Takeyama H, Wakamiya N, O’Hara C, et al. Tumor necrosis factor expression by human ovarian carcinoma in vivo. Cancer Res. 1991 Aug 15;51(16):4476–4480. [PubMed] [Google Scholar]
- [97].Wu Y, Zhou BP. TNF-alpha/NF-kappaB/Snail pathway in cancer cell migration and invasion. Br J Cancer. Feb 16;102(4):639–644. doi: 10.1038/sj.bjc.6605530. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [98].Balkwill F. Tumor necrosis factor or tumor promoting factor? Cytokine Growth Factor Rev. 2002 Apr;13(2):135–141. doi: 10.1016/s1359-6101(01)00020-x. [DOI] [PubMed] [Google Scholar]
- [99].Balkwill F, Mantovani A. Inflammation and cancer: back to Virchow? Lancet. 2001 Feb 17;357(9255):539–545. doi: 10.1016/S0140-6736(00)04046-0. [DOI] [PubMed] [Google Scholar]
- [100].Balkwill F, Coussens LM. Cancer: an inflammatory link. Nature. 2004 Sep 23;431(7007):405–406. doi: 10.1038/431405a. [DOI] [PubMed] [Google Scholar]
- [101].Mantovani A. Cancer: inflammation by remote control. Nature. 2005 Jun 9;435(7043):752–753. doi: 10.1038/435752a. [DOI] [PubMed] [Google Scholar]
- [102].Hsu TC, Nair R, Tulsian P, et al. Transformation nonresponsive cells owe their resistance to lack of p65/nuclear factor-kappaB activation. Cancer Res. 2001 May 15;61(10):4160–4168. [PubMed] [Google Scholar]
- [103].Shishodia S, Aggarwal BB. Nuclear factor-kappaB activation mediates cellular transformation, proliferation, invasion angiogenesis and metastasis of cancer. Cancer Treat Res. 2004;119:139–173. doi: 10.1007/1-4020-7847-1_8. [DOI] [PubMed] [Google Scholar]
- [104].Johnston DA, Dong B, Hughes CC. TNF induction of jagged-1 in endothelial cells is NFkappaB-dependent. Gene. 2009 Apr 15;435(1–2):36–44. doi: 10.1016/j.gene.2009.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [105].Aggarwal BB. Signalling pathways of the TNF superfamily: a double-edged sword. Nat Rev Immunol. 2003 Sep;3(9):745–756. doi: 10.1038/nri1184. [DOI] [PubMed] [Google Scholar]
- [106].de Kossodo S, Moore R, Gschmeissner S, East N, Upton C, Balkwill FR. Changes in endogenous cytokines, adhesion molecules and platelets during cytokine-induced tumour necrosis. Br J Cancer. 1995 Nov;72(5):1165–1172. doi: 10.1038/bjc.1995.481. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [107].Komori A, Yatsunami J, Suganuma M, et al. Tumor necrosis factor acts as a tumor promoter in BALB/3T3 cell transformation. Cancer Res. 1993 May 1;53(9):1982–1985. [PubMed] [Google Scholar]
- [108].Nabors LB, Suswam E, Huang Y, Yang X, Johnson MJ, King PH. Tumor necrosis factor alpha induces angiogenic factor up-regulation in malignant glioma cells: a role for RNA stabilization and HuR. Cancer Res. 2003 Jul 15;63(14):4181–4187. [PubMed] [Google Scholar]
- [109].Yoshida S, Ono M, Shono T, et al. Involvement of interleukin-8, vascular endothelial growth factor, and basic fibroblast growth factor in tumor necrosis factor alpha-dependent angiogenesis. Mol Cell Biol. 1997 Jul;17(7):4015–4023. doi: 10.1128/mcb.17.7.4015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [110].Leibovich SJ, Polverini PJ, Shepard HM, Wiseman DM, Shively V, Nuseir N. Macrophage-induced angiogenesis is mediated by tumour necrosis factor-alpha. Nature. 1987 Oct 15–21;329(6140):630–632. doi: 10.1038/329630a0. [DOI] [PubMed] [Google Scholar]
- [111].Rot A, von Andrian UH. Chemokines in innate and adaptive host defense: basic chemokinese grammar for immune cells. Annu Rev Immunol. 2004;22:891–928. doi: 10.1146/annurev.immunol.22.012703.104543. [DOI] [PubMed] [Google Scholar]
- [112].Raman D, Baugher PJ, Thu YM, Richmond A. Role of chemokines in tumor growth. Cancer Lett. 2007 Oct 28;256(2):137–165. doi: 10.1016/j.canlet.2007.05.013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [113].Hiratsuka S, Watanabe A, Aburatani H, Maru Y. Tumour-mediated upregulation of chemoattractants and recruitment of myeloid cells predetermines lung metastasis. Nat Cell Biol. 2006 Dec;8(12):1369–1375. doi: 10.1038/ncb1507. [DOI] [PubMed] [Google Scholar]
- [114].Rafii S, Lyden D. S100 chemokines mediate bookmarking of premetastatic niches. Nat Cell Biol. 2006 Dec;8(12):1321–1323. doi: 10.1038/ncb1206-1321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [115].Kulbe H, Levinson NR, Balkwill F, Wilson JL. The chemokine network in cancer--much more than directing cell movement. Int J Dev Biol. 2004;48(5–6):489–496. doi: 10.1387/ijdb.041814hk. [DOI] [PubMed] [Google Scholar]
- [116].Muller A, Homey B, Soto H, et al. Involvement of chemokine receptors in breast cancer metastasis. Nature. 2001 Mar 1;410(6824):50–56. doi: 10.1038/35065016. [DOI] [PubMed] [Google Scholar]
- [117].Wang D, Richmond A. Nuclear factor-kappa B activation by the CXC chemokine melanoma growth-stimulatory activity/growth-regulated protein involves the MEKK1/p38 mitogen-activated protein kinase pathway. J Biol Chem. 2001 Feb 2;276(5):3650–3659. doi: 10.1074/jbc.M006115200. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [118].Scotton CJ, Wilson JL, Milliken D, Stamp G, Balkwill FR. Epithelial cancer cell migration: a role for chemokine receptors? Cancer Res. 2001 Jul 1;61(13):4961–4965. [PubMed] [Google Scholar]
- [119].Porcile C, Bajetto A, Barbero S, Pirani P, Schettini G. CXCR4 activation induces epidermal growth factor receptor transactivation in an ovarian cancer cell line. Ann N Y Acad Sci. 2004 Dec;1030:162–169. doi: 10.1196/annals.1329.021. [DOI] [PubMed] [Google Scholar]
- [120].Johrer K, Zelle-Rieser C, Perathoner A, et al. Up-regulation of functional chemokine receptor CCR3 in human renal cell carcinoma. Clin Cancer Res. 2005 Apr 1;11(7):2459–2465. doi: 10.1158/1078-0432.CCR-04-0405. [DOI] [PubMed] [Google Scholar]
- [121].Fukuyama R, Ng KP, Cicek M, et al. Role of IKK and oscillatory NFkappaB kinetics in MMP-9 gene expression and chemoresistance to 5-fluorouracil in RKO colorectal cancer cells. Mol Carcinog. 2007 May;46(5):402–413. doi: 10.1002/mc.20288. [DOI] [PubMed] [Google Scholar]
- [122].Egeblad M, Werb Z. New functions for the matrix metalloproteinases in cancer progression. Nat Rev Cancer. 2002 Mar;2(3):161–174. doi: 10.1038/nrc745. [DOI] [PubMed] [Google Scholar]
- [123].Minn AJ, Gupta GP, Siegel PM, et al. Genes that mediate breast cancer metastasis to lung. Nature. 2005 Jul 28;436(7050):518–524. doi: 10.1038/nature03799. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [124].Ii M, Yamamoto H, Adachi Y, Maruyama Y, Shinomura Y. Role of matrix metalloproteinase-7 (matrilysin) in human cancer invasion, apoptosis, growth, and angiogenesis. Exp Biol Med (Maywood) 2006 Jan;231(1):20–27. doi: 10.1177/153537020623100103. [DOI] [PubMed] [Google Scholar]
- [125].Coussens LM, Tinkle CL, Hanahan D, Werb Z. MMP-9 supplied by bone marrow-derived cells contributes to skin carcinogenesis. Cell. 2000 Oct 27;103(3):481–490. doi: 10.1016/s0092-8674(00)00139-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [126].Sovak MA, Bellas RE, Kim DW, et al. Aberrant nuclear factor-kappaB/Rel expression and the pathogenesis of breast cancer. J Clin Invest. 1997 Dec 15;100(12):2952–2960. doi: 10.1172/JCI119848. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [127].Suh J, Payvandi F, Edelstein LC, et al. Mechanisms of constitutive NF-kappaB activation in human prostate cancer cells. Prostate. 2002 Aug 1;52(3):183–200. doi: 10.1002/pros.10082. [DOI] [PubMed] [Google Scholar]
- [128].Mukhopadhyay T, Roth JA, Maxwell SA. Altered expression of the p50 subunit of the NF-kappa B transcription factor complex in non-small cell lung carcinoma. Oncogene. 1995 Sep 7;11(5):999–1003. [PubMed] [Google Scholar]
- [129].Kojima M, Morisaki T, Sasaki N, et al. Increased nuclear factor-kB activation in human colorectal carcinoma and its correlation with tumor progression Anticancer Res March–Apr2004242B675–681. [PubMed] [Google Scholar]
- [130].Wang W, Abbruzzese JL, Evans DB, Larry L, Cleary KR, Chiao PJ. The nuclear factor-kappa B RelA transcription factor is constitutively activated in human pancreatic adenocarcinoma cells. Clin Cancer Res. 1999 Jan;5(1):119–127. [PubMed] [Google Scholar]
- [131].Pacifico F, Mauro C, Barone C, et al. Oncogenic and anti-apoptotic activity of NF-kappa B in human thyroid carcinomas. J Biol Chem. 2004 Dec 24;279(52):54610–54619. doi: 10.1074/jbc.M403492200. [DOI] [PubMed] [Google Scholar]
- [132].Ondrey FG, Dong G, SunwooJ J, et al. Constitutive activation of transcription factors NF-(kappa)B, AP-1, and NF-IL6 in human head and neck squamous cell carcinoma cell lines that express pro-inflammatory and pro-angiogenic cytokines. Mol Carcinog. 1999 Oct;26(2):119–129. doi: 10.1002/(sici)1098-2744(199910)26:2<119::aid-mc6>3.0.co;2-n. [DOI] [PubMed] [Google Scholar]
- [133].Nair A, Venkatraman M, Maliekal TT, Nair B, Karunagaran D. NF-kappaB is constitutively activated in high-grade squamous intraepithelial lesions and squamous cell carcinomas of the human uterine cervix. Oncogene. 2003 Jan 9;22(1):50–58. doi: 10.1038/sj.onc.1206043. [DOI] [PubMed] [Google Scholar]
- [134].Ross JS, Stagliano NE, Donovan MJ, Breitbart RE, Ginsburg GS. Atherosclerosis: a cancer of the blood vessels? Am J Clin Pathol. 2001 Dec;116(Suppl):S97–107. doi: 10.1309/YNCK-9R19-5JA3-K2K9. [DOI] [PubMed] [Google Scholar]
- [135].Jimi E, Aoki K, Saito H, et al. Selective inhibition of NF-kappa B blocks osteoclastogenesis and prevents inflammatory bone destruction in vivo. Nat Med. 2004 Jun;10(6):617–624. doi: 10.1038/nm1054. [DOI] [PubMed] [Google Scholar]
- [136].Dewan MZ, Terashima K, Taruishi M, et al. Rapid tumor formation of human T-cell leukemia virus type 1-infected cell lines in novel NOD-SCID/gammac(null) mice: suppression by an inhibitor against NF-kappaB. J Virol. 2003 May;77(9):5286–5294. doi: 10.1128/JVI.77.9.5286-5294.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [137].Scaife CL, Kuang J, Wills JC, et al. Nuclear factor kappaB inhibitors induce adhesion-dependent colon cancer apoptosis: implications for metastasis. Cancer Res. 2002 Dec 1;62(23):6870–6878. [PubMed] [Google Scholar]
- [138].Yamamoto Y, Gaynor RB. Role of the NF-kappaB pathway in the pathogenesis of human disease states. Curr Mol Med. 2001 Jul;1(3):287–296. doi: 10.2174/1566524013363816. [DOI] [PubMed] [Google Scholar]
- [139].Yamamoto Y, Yin MJ, Lin KM, Gaynor RB. Sulindac inhibits activation of the NF-kappaB pathway. J Biol Chem. 1999 Sep 17;274(38):27307–27314. doi: 10.1074/jbc.274.38.27307. [DOI] [PubMed] [Google Scholar]
- [140].Yin MJ, Yamamoto Y, Gaynor RB. The anti-inflammatory agents aspirin and salicylate inhibit the activity of I(kappa)B kinase-beta. Nature. 1998 Nov 5;396(6706):77–80. doi: 10.1038/23948. [DOI] [PubMed] [Google Scholar]
- [141].Holmes-McNary M, Baldwin AS. Chemopreventive properties of trans-resveratrol are associated with inhibition of activation of the IkappaB kinase. Cancer Res. 2000 Jul 1;60(13):3477–3483. [PubMed] [Google Scholar]
- [142].Keifer JA, Guttridge DC, Ashburner BP, Baldwin AS. Inhibition of NF-kappa B activity by thalidomide through suppression of IkappaB kinase activity. J Biol Chem. 2001 Jun 22;276(25):22382–22387. doi: 10.1074/jbc.M100938200. [DOI] [PubMed] [Google Scholar]
- [143].Chun KS, Keum YS, Han SS, Song YS, Kim SH, Surh YJ. Curcumin inhibits phorbol ester-induced expression of cyclooxygenase-2 in mouse skin through suppression of extracellular signal-regulated kinase activity and NF-kappaB activation. Carcinogenesis. 2003 Sep;24(9):1515–1524. doi: 10.1093/carcin/bgg107. [DOI] [PubMed] [Google Scholar]
- [144].Takada Y, Bhardwaj A, Potdar P, Aggarwal BB. Nonsteroidal anti-inflammatory agents differ in their ability to suppress NF-kappaB activation, inhibition of expression of cyclooxygenase-2 and cyclin D1, and abrogation of tumor cell proliferation. Oncogene. 2004 Dec 9;23(57):9247–9258. doi: 10.1038/sj.onc.1208169. [DOI] [PubMed] [Google Scholar]
- [145].Lam LT, Davis RE, Pierce J, et al. Small molecule inhibitors of IkappaB kinase are selectively toxic for subgroups of diffuse large B-cell lymphoma defined by gene expression profiling. Clin Cancer Res. 2005 Jan 1;11(1):28–40. [PubMed] [Google Scholar]
- [146].Van Antwerp DJ, Martin SJ, Kafri T, Green DR, Verma IM. Suppression of TNF-alpha-induced apoptosis by NF-kappaB. Science. 1996 Nov 1;274(5288):787–789. doi: 10.1126/science.274.5288.787. [DOI] [PubMed] [Google Scholar]
- [147].Zhou M, Gu L, Zhu N, Woods WG, Findley HW. Transfection of a dominant-negative mutant NF-kB inhibitor (IkBm) represses p53-dependent apoptosis in acute lymphoblastic leukemia cells: interaction of IkBm and p53. Oncogene. 2003 Nov 6;22(50):8137–8144. doi: 10.1038/sj.onc.1206911. [DOI] [PubMed] [Google Scholar]
- [148].Kane RC, Bross PF, Farrell AT, Pazdur R. Velcade: U.S. FDA approval for the treatment of multiple myeloma progressing on prior therapy. Oncologist. 2003;8(6):508–513. doi: 10.1634/theoncologist.8-6-508. [DOI] [PubMed] [Google Scholar]
- [149].Lun M, Zhang PL, Pellitteri PK, Law A, Kennedy TL, Brown RE. Nuclear factor-kappaB pathway as a therapeutic target in head and neck squamous cell carcinoma: pharmaceutical and molecular validation in human cell lines using Velcade and siRNA/NF-kappaB. Ann Clin Lab Sci. 2005 Summer;35(3):251–258. [PubMed] [Google Scholar]
- [150].Bunn PA. The potential role of proteasome inhibitors in the treatment of lung cancer. Clin Cancer Res. 2004 Jun 15;10(12 Pt 2):4263s–4265s. doi: 10.1158/1078-0432.CCR-040011. [DOI] [PubMed] [Google Scholar]
- [151].Sunwoo JB, Chen Z, Dong G, et al. Novel proteasome inhibitor PS-341 inhibits activation of nuclear factor-kappa B, cell survival, tumor growth, and angiogenesis in squamous cell carcinoma. Clin Cancer Res. 2001 May;7(5):1419–1428. [PubMed] [Google Scholar]
- [152].Richardson PG, Hideshima T, Mitsiades C, Anderson K. Proteasome inhibition in hematologic malignancies. Ann Med. 2004;36(4):304–314. doi: 10.1080/07853890410030877. [DOI] [PubMed] [Google Scholar]
- [153].Nasr R, El-Sabban ME, Karam JA, et al. Efficacy and mechanism of action of the proteasome inhibitor PS-341 in T-cell lymphomas and HTLV-I associated adult T-cell leukemia/lymphoma. Oncogene. 2005 Jan 13;24(3):419–430. doi: 10.1038/sj.onc.1208212. [DOI] [PubMed] [Google Scholar]


