Abstract
Infections have almost become an inseparable part of the intensive care units throughout the globe in spite of numerous advancements in diagnostic and therapeutic interventions. With advances in critical care medicine and introduction of broad-spectrum antibiotics, the incidence of invasive fungal infections in intensive care is on the rise, especially in patients with immunosuppression. The aim of this review is to collect recent information about various types of invasive fungal infections prevalent in the intensive care unit, the problems in their diagnosis and recent trends in their management. A thorough literature search was made in PubMed and Google using the following keywords for our search: Invasive fungal infection, antifungal therapy in intensive care unit, candidiasis. The major fungi implicated worldwide are Candida and Aspergillus spp., followed by Cryptococcus, Histoplasma, etc., in endemic areas. These produce a wide variety of infections that are difficult to diagnose as most of the diagnosing tests are non-specific and the culture takes a long time. An early suspicion of fungal infection with institution of appropriate antifungal therapy is mandatory for a positive outcome and to prevent development of invasive fungal infection.
Keywords: Antifungal therapy, Intensive care unit, Invasive fungal infection
Introduction
Infections have almost become an inseparable part of the intensive care units throughout the globe in spite of numerous advancements in diagnostic and therapeutic interventions. The presence of infection in critically ill patients poses unique challenges as it can directly influence the morbidity and mortality. Of the various infections prevalent in an intensive care unit, invasive fungal infection has always been considered to occur infrequently, but, over the past few years, with the surge in broad-spectrum antibiotic usage and improved knowledge of fungal diseases, the incidence has risen. At present, systemic fungal infections constitute a major problem in intensive care units in both developed and developing nations. However, intensivists in tropical developing countries like India face an uphill task during management of this ever-increasing menace of fungal infections. The fungi can survive in extremes of environment, but only 150-200 of over several thousand species of fungi are found to be pathogenic to humans. The incidence of systemic fungal infections is much more in immunocompromised individuals such as organ-transplanted patients, patients with hematologic malignancies and HIV-infected patients. In the United States, the incidence of nosocomial fungal infections has increased from 2 to 3.8 per 1000 discharges.[1] Candida spp. was found to be the most common, accounting for 8-15% of nosocomial blood stream infections and the fourth most common isolate of patients of the intensive care unit.[2]
Among the developing countries, the diverse climatic conditions in India also are well suited for various fungal infections. The incidences of candidemia, systemic aspergillosis, cryptococcosis and zygomycosis in India have shown a steep rise, with emergence of newer fungal infections like Apophysomyces elegans.[3,4,5,6]
Methods of Literature Search
We conducted a systematic literature search using search engines like PubMed and Google with the use of the following single text words and combinations: Fungal infections in ICU, invasive fungal infections, antifungal therapy - recent trends. The PubMed search was made from the year 1989 till date. The references of relevant articles were cross checked and the articles describing various types of fungal infections in the intensive care unit and recent trends in treatment of fungal infections were included.
Common Fungal Infections in the Intensive Care Unit: Etiology and Clinical Scenario
The diagnosis of fungal infections in critically ill patients is an extremely difficult task as the symptoms are invariably masked by the presence of dominant primary pathology. The etiology of fungal infections can be broadly subdivided into systemic infections caused by true pathogenic fungi and infections caused by opportunistic saprophytic fungi.
True pathogenic fungi
Histoplasmosis
Epidemiology and clinical features
It is the most common among endemic mycosis, and is caused by a soil-dwelling dimorphic fungus, Histoplasma capsulatum. It is endemic in most parts of the United States and in many states in India. The portal of entry is respiratory tract, with severity of disease depending on the infecting dose. The spectrum of disease varies from mild pulmonary disease, severe pulmonary disease, chronic pulmonary disease and disseminated histoplasmosis. The chest radiograph may show multilobar infiltrates but is not diagnostic, while in patients with full-blown acquired immunodeficiency syndrome (AIDS), it may show predominantly reticulonodular infiltrates.[7]
Diagnosis
The diagnosis is by a high degree of suspicion, with a positive travel history to the endemic area, while the demonstration of Histoplasma antigen in urine, blood or bronchoalveolar lavage fluid of infected patients is diagnostic and rapid. If disseminated histoplasmosis is suspected, then a bone marrow biopsy may be helpful.
Management
Most infections are self-limited and require no specific treatment. The treatment of severe and disseminated disease involves administration of amphotericin B; both the conventional and the lipid formulations can be used. However, the lipid formulation is found to be less nephrotoxic. Following initial stabilization, oral itraconazole can be added twice daily for at least 12 months.[8] Monitoring of itraconazole serum levels has to be done every 2 weeks with monitoring of liver and renal functions.
Blastomycosis
Epidemiology and clinical features
The incidence of blastomycosis is much less than that of histoplasmosis, and the endemicity exhibit almost similar pattern as of histoplasmosis.[9] The mode of infection is through inhalation of infected particles; however, extrapulmonary involvement is much less as compared with histoplasmosis. The usual clinical presentation is a community-acquired pneumonia not responding to usual antibiotics. It is less common in HIV-infected patients, but, if present, produces widely disseminated disease often involving the meninges. Other sites of infections are skin, bones and genitourinary tract.
Diagnosis
The presumptive diagnosis is made by demonstration of characteristic appearance of the fungus on 10% KOH digest of the respiratory secretions or bronchoalveolar lavage fluid.[10,11] Serologic tests have low sensitivity and hence are seldom used, but an open lung biopsy of the lesion may sometimes be required. Definitive diagnosis requires growth of organism from a clinical specimen.
Management
The treatment for the severe infection causing respiratory distress is by Amphotericin B (both conventional and liposomal), and followed by oral itraconazole twice daily for 12 months after initial stabilization. The meningitis usually responds to Amphotericin B with concurrent or sequential itraconazole or fluconazole.
Coccidioidomycosis
Epidemiology and clinical features
It is caused by the soil-dwelling dimorphic fungus Coccidiodes immitis, which is found to be endemic in the desert-like terrain of America. The portal of entry is by respiratory tract and the usual presentation is community-acquired pneumonia. The most dreaded complication is meningitis, which may or may not be preceded by an acute illness. The patient presents with increasing severity of headache with altered mental status, which may lead on to development of hydrocephalus. Occasionally, it may present as stroke syndrome due to vasculitis of cerebral vessels.[12,13]
Diagnosis
The diagnosis is by demonstration of fungus from culture of respiratory secretions or of cerebrospinal fluid, and is thus more difficult. The serologic tests are usually used to establish the diagnosis. The cerebrospinal fluid analysis in meningeal disease shows predominantly lymphocytic pleocytosis with occasional eosinophils.
Management
The treatment is often difficult as it is less susceptible to antifungal drugs as compared with histoplasmosis or blastomycosis. In severe and disseminated disease, amphotericin B (liposomal or conventional) is still used; however, oral fluconazole or itraconazole is considered the main drug for less-severe disease. There is, however, no consensus for treatment duration.[14] Invasive and disseminated disease in immunocompromised patients is treated with Amphotericin B till clinical improvement, followed by itraconazole or fluconazole for at least 1 year.
These fungal infections may or may not exhibit clinical symptomatology, but their occurrence greatly affect the prognosis and outcome. The most challenging aspect is the timely diagnosis, and by that time it almost causes a great damage to the cellular functions. Once diagnosed, it should be treated as an emergency that can substantially lower the morbidity and mortality among critically ill patients.
Opportunistic fungi
These opportunistic fungal infections pose numerous challenges and difficulties in the management of critically ill patients, especially those who need broad-spectrum antibiotics for their primary pathology. It involves fungi like Candida, Cryptococcus, Aspergillus and Zygomycetes, which are regularly associated with immunocompromised patients such as hematooncological patients, patients undergoing organ transplantation or patients with immunodeficiency syndromes.
Candida SPP
Epidemiology and clinical features
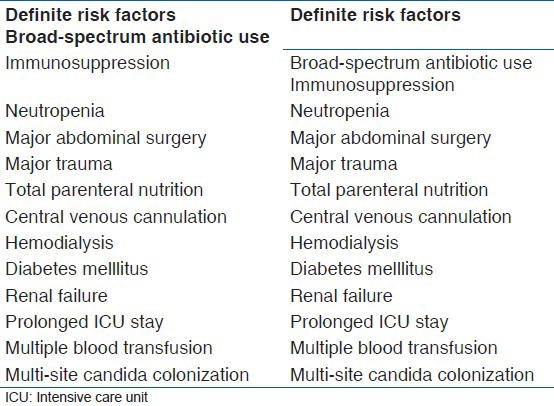
Invasive fungal infections with Candida spp. are the most common systemic fungal infections in the intensive care unit, accounting for 9% of all such infections in the United States.[15] The most common species implicated was C. albicans until recently, when the incidence of non-albicans Candida (NAC) has risen dramatically.[16] In India also, the isolates of NAC range from 52 to 96%, but the predominant species was found to be C. tropicalis instead of C. glabrata or C. parapsilosis in all age groups.[17,18,19] This increased incidence of NAC may be attributed to the increased use of fluconazole prophylaxis in immunocompromised patients, central venous cannulations and prior gastrointestinal surgery, and the mortality due to invasive candidiasis can range from 40 to 60%.[20] The various risk factors associated with the development of systemic candidial infection are summarised in Table 1.[21]
Table 1.
Risk factors associated with systemic candidiasis
Opportunistic candidial infections in patients with AIDS have been reduced due to the advent of highly active antiretroviral therapy (HAART) in developed nations, but it is still high in developing nations like India due to the high cost of such therapy. In intensive care units, catheter-related candida infections account for 30-80% of the proven or suspected cases of invasive candidiasis.[22]
Diagnostic methodologies
According to the European Organisation for Research and Treatment of Cancer/Mycoses Study Group, the diagnosis of candidiasis can be “definitive” or “probable.” The demonstration of Candida in blood and histologic identification in tissues are considered to be definitive, but about 50% of these patients may show false-negative results, and the tissues may not be readily available in an intensive care setting.[23] The use of risk-factor-based prediction of invasive candidial infection has been described, which classified the patients as low risk or high risk depending on the presence or absence of four independent risk factors, namely total parenteral nutrition (1 point), multifocal colonisation sites (1 point), severe sepsis (2 points) and surgery (1 point). Accordingly, a “Candida Score” was calculated and a score of ≥3 predicted invasive candidial disease with a sensitivity of 81% and a specificity of 74%.[24,25]
Laboratory tests can aid in increasing the accuracy of the above tests in diagnosing invasive candidiasis. The various laboratory tests involved are:
Beta-D-Glucan assay: It detects b-D-glucan, an important constituent of the cell wall of pathogenic fungi. It cannot however differentiate between Candida and Aspergillus, and is not helpful in diagnosing infection with Cryptococcus and Zygomycetes.[26] False-positive results may be found in patients receiving beta lactams, albumin and immunoglobulins and patients on hemodialysis with cellulose membrane. A single positive test has low sensitivity for diagnosing invasive candidiasis, and serial measurements may be more sensitive.
Polymerase chain reaction (PCR): It detects fungal nucleic acid and has been found to have a sensitivity of 90.9% with 100% specificity.[27] These results may be highly promising, but their exact utility in clinical settings is questionable.
Management strategies
Pre-emptive treatment: It is considered in those patients who have a high risk of developing candidiasis but lack a definitive diagnosis of infection. Fluconazole in a dose of 400 mg to 800 mg per day is usually used, and this therapy has shown to significantly reduce the incidence of definitive candidiasis.[28] However, no improvement of outcome could be documented so far.
Prophylactic treatment: The prophylactic use of fluconazole is recommended in patients receiving chemotherapy for hematologic malignancies who are expected to be neutropenic, in patients with solid organ transplantation and in patients undergoing bone marrow transplantation. This prophylaxis can also be used in non-neutropenic at-risk intensive care patients.[29] However, no benefit of such prophylaxis could be documented till now.[30]
Definitive treatment: In patients with a definitive diagnosis of candidiasis, all catheters, including the central venous catheter, should be removed and invasive candidiasis such as endophthalmitis should be excluded.
In clinically stable patients, fluconazole is used in a dose of 400 mg to a maximum of 1600 mg per day for at least 2 weeks after the last positive blood culture unless azole resistance is suspected. Echinocandins (caspofungin, micafungin, anidulafungin) should be preferred if NAC such as C. glabrata or C. krusei are suspected.[29]
In unstable and severely ill patients, amphotericin B (conventional or liposomal) alone or in combination with fluconazole, echinocandins (caspofungin, micafungin, anidulafungin), voriconazole or high-dose fluconazole (800 mg per day) may be used.
The duration of therapy should be 14 days after the first negative blood culture and clinical resolution of symptoms in patients with candidaemia. In patients with invasive candidiasis, antifungal treatment has to be given for a longer period of time until clinical and radiological resolution of the disease.
Aspergillus
Epidemiology and clinical features
Aspergillosis is a serious infection in the intensive care unit, which is difficult to diagnose due to the lack of definitive diagnostic criteria. Majority of infections are caused by A. fumigatus, A. flavus and A. niger. The incidence in western countries was found to be about 15%, with a mortality rate of approximately 80%.[31]
In India, A. flavus is the most common species, followed by A. fumigatus, and A. niger is the third most common species implicated.
The risk factors for development of invasive aspergillosis are similar to that of invasive candidiasis, with the predominance of immunosuppression in aspergillosis. Chronic obstructive pulmonary disease is considered to be an important risk factor for aspergillosis.[32]
The portal of entry is mainly the respiratory tract, both lungs and sinuses. Aspergillosis can be acquired in the intensive care unit through an improperly cleaned ventilation system and contaminated water.
Diagnostic methodologies
The diagnosis of aspergillosis is often difficult, and the following methods are employed:
Culture and histopathology: Identification of the fungus in culture and tissue specimens is the gold standard for diagnosing aspergillosis, but may not be feasible in the intensive care setting due to the long time required and difficulty in obtaining tissue samples in these patients.
Radiology: Computed tomography showing a characteristic “crescent” or “halo” sign is highly suggestive of aspergillosis, especially in neutropenic patients, but only in 5% of non-neutropenic patients.[33] However, there might be many confounding factors that can affect the radiological diagnosis in these patients.
Galactomannan test: It is an important constituent of the cell wall and it can be detected in the serum or bronchoalveolar lavage fluid; however, brochoalveolar lavage is considered to be more sensitive.[34]
PCR: It detects the fungal nucleic acid and is sensitive when combined with other tests.
Combination of bronchoalveolar lavage fluid galactomannan test with the PCR greatly increases the detection of Aspergillus spp. Detection of aspergillus from patients without any risk factors should encourage further diagnostic workup.
Management strategies
Amphotericin B was initially used as the mainstay therapy, but, due to various adverse effects, voriconazole has now become the treatment of choice. The treatment for invasive aspergillosis can be described as:
Primary therapy: Intravenous voriconazole in the dose of 6 mg/kg every 12 hourly followed 24 h later by 4 mg/kg every 12 hourly. This should be followed by oral voriconazole 200 mg twice daily until clinical and radiological stabilization occurs. Alternatively, amphotericin B (liposomal) can be used intravenously in a dose of 3-5 mg/kg/day followed by oral voriconazole (200 mg twice daily) until clinical improvement.
Salvage therapy: Echinocandins are utilized in this therapy when the primary therapy fails. Intravenous Caspofungin in a dose of 70 mg on Day 1, followed by 50 mg per day thereafter is usually used; however, intravenous micafungin can also be used. Recently, oral posaconazole in a dose of 200 mg every 6 hourly, followed by 400 mg twice daily, has been found to be equally effective.[35]
Combination therapy: There has been interest in the combination of various antifungal agents for the treatment of invasive aspergillosis and combination of liposomal amphotericin B and itraconazole as well as combination of voriconazole with caspofungin has been studied and found to be equally effective.[36] However, further studies are required for strongly recommending any such therapies.
The therapy is usually continued for 6-12 weeks. The galactomannan test can be used as a marker of effectiveness of the therapy. The therapy is found to be more effective when the immunosuppression is reversed.
The treatment for other forms of aspergillus infection, such as allergic bronchopulmonary aspergillosis and aspergilloma is usually symptomatic, and surgical resection may be warranted.
Cryptococcus
Epidemiology and clinical features
The most common organism implicated is C. neoformans, and the most common clinical feature is cryptococcal meningitis. It was considered rare before the emergence of AIDS, but now with the AIDS pandemic, its incidence has increased to about 5% in western countries while in Sub-Saharan Africa, its incidence reaches up to 30%.
The usual habitat of C. neoformans is in the bird droppings. The pulmonary manifestations range from pulmonary nodules, interstitial pneumonitis, pleural effusions or adenopathy in immunocompetent individuals to ground glass opacities, consolidation and hilar lymphadenopathy in patients with AIDS.[37,38]
Diagnosis
Diagnosis is delayed due to non-specific symptomatology. Cerebrospinal fluid analysis shows pleocytosis with predominant lymphocytes and elevated proteins with depressed glucose. Serological cryptococcal antigen test of blood and cerebrospinal fluid is indicated in central nervous infections, but are costly and are not preferred in developing countries. Lateral flow assay was introduced recently for diagnosis, and has shown to be equally effective to enzyme immune assay. Demonstration of the fungus in cerebrospinal fluid culture is diagnostic.
Management
Treatment in immunocompetent patients includes fluconazole or itraconazole for mild pulmonary disease and intravenous amphotericin B with or without flucytosine for the initial 2 weeks followed by fluconazole or itraconazole for a further 10 weeks.
In immunocompromised patients, treatment of pulmonary disease consists of fluconazole or itraconazole continued for 6-12 months, followed by secondary prophylaxis, while in that of central nervous system infections, the treatment consists of intravenous amphotericin B with Flucytosine for the initial 2 weeks followed by fluconazole for the next 8 weeks and then continuing with secondary prophylaxis. The secondary prophylaxis consists of fluconazole, and can be continued till the highly active antiretroviral therapy is instituted.[39]
Zygomycetes
Epidemiology and clinical features
Zygomycosis is another opportunistic nosocomial infection commonly found in patients with uncontrolled diabetes and other forms of metabolic acidosis, like burns and hematological malignancies. The incidence is difficult to predict due to difficulties in antemortem diagnosis.
The common species implicated are Rhizopus arrhizus, R. microsporus, Lichtheimia corymbifera, etc., These produce spores that are commonly found in soil, dead organic matter and hospital environment. These may be found in dead necrotic tissues in the body.
Management
Treatment includes high-dose liposomal amphotericin B plus/minus posaconazole. Debridement or surgical removal of dead necrotic tissue may be required.
Pneumocystis
This is an important opportunistic fungus that causes pneumonia in immunocompromised patients, especially in patients with AIDS. Pneumonia is caused by Pneumocystis jiroveci, which is commonly present in the environment but is non-infectious in healthy individuals.[40]
The infection usually starts with fever and non-productive cough, gradually progressing to shortness of breath and hypoxia. Pneumothorax is a well known complication and should be suspected in acute chest pain with breathlessness with unilateral reduced breath sounds. It mainly involves the interstitial fibrous tissue of the lungs, leading to thickening and impaired oxygenation.
Diagnosis
The diagnosis of P. jiroveci infection is usually made by characteristic appearance of widespread pulmonary infiltrates on chest radiograph in an immunocompromised patient. The diagnosis is confirmed by histological demonstration of organism in sputum or bronchoalveolar lavage fluid, by staining showing characteristic cysts. PCR can also be used to detect the DNA.
Treatment
Primary prophylaxis is indicated in patients with AIDS with CD4 cell counts less than 200 cells/μl, patients on chronic steroid therapy, patients with malignancy on cytotoxic drug therapy and patients with organ transplantation. Co-trimoxazole is the first choice drug while dapsone, atovaquone and aerosolized pentamidine may be used as second-line drugs.[41]
The treatment of established infection is by co-trimoxazole in divided doses for at least 3 weeks. The other drugs that may be used as second choice are dapsone, atovaquone, clindamycin, primaquine and pentamidine. Adjunctive steroids are usually indicated in moderate to severe disease to prevent inflammation and worsening of symptoms due to the treatment of infection.
Conclusion
The recent advances in management of life-threatening infections in intensive care unit with advent of broad-spectrum antibiotics have greatly reduced mortality but have significantly increased the incidence of invasive fungal infections. These invasive fungal infections are often difficult to diagnose and treat in the intensive care setting. With the advances in antifungal therapy, the mortality and morbidity in intensive care can be greatly reduced.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
References
- 1.Beck-Sagué C, Jarvis WR. Secular trends in the epidemiology of nosocomial fungal infections in the United States, 1980-1990: National nosocomial infections surveillance system. J Infect Dis. 1993;167:1247–51. doi: 10.1093/infdis/167.5.1247. [DOI] [PubMed] [Google Scholar]
- 2.Pfaller MA, Diekema DJ. Role of sentinel surveillance of candidemia: Trends in species distribution and antifungal susceptibility. J Clin Microbiol. 2002;40:3551–7. doi: 10.1128/JCM.40.10.3551-3557.2002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Chakrabarti A, Singh K, Narang A, Singhi S, Batra R, Rao KL, et al. Outbreak of pichia anomala infection in the pediatric service of a tertiary care centre in northern India. J Clin Microbiol. 2001;39:1702–6. doi: 10.1128/JCM.39.5.1702-1706.2001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Sharma BS, Khosla VK, Kak VK, Banerjee AK, Vasishtha RK, Prasad KS, et al. Intra-cranial fungal granuloma. Surg Neurol. 1997;47:489–97. doi: 10.1016/s0090-3019(96)00209-1. [DOI] [PubMed] [Google Scholar]
- 5.Chakrabarti A, Das A, Sharma A, Panda N, Das S, Gupta KL, et al. Ten years’ experience in zygomycosis at a tertiary care centre in India. J Infect. 2001;42:261–6. doi: 10.1053/jinf.2001.0831. [DOI] [PubMed] [Google Scholar]
- 6.Chakrabarti A, Ghosh A, Prasad GS, David JK, Gupta S, Das A, et al. Apophysomyces elegans: An emerging zygomycetes in India. J Clin Microbiol. 2003;41:783–8. doi: 10.1128/JCM.41.2.783-788.2003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wheat LJ, Connolly-Stringfield PA, Baker RL, Curfman MF, Eads ME, et al. Disseminated histoplasmosis in the acquired immunodeficiency syndrome; clinical finds, diagnosis and treatment, and review of the literature. Medicine. 1990;69:361–74. doi: 10.1097/00005792-199011000-00004. [DOI] [PubMed] [Google Scholar]
- 8.Johnson PC, Wheat LJ, Cloud GA, Goldman M, Lancaster D, Bamberger DM, et al. Safety and efficacy of liposomal amphotericin B for induction therapy of histoplasmosis in patients with AIDS. Ann Intern Med. 2002;137:105–9. doi: 10.7326/0003-4819-137-2-200207160-00008. [DOI] [PubMed] [Google Scholar]
- 9.Chu JH, Feudtner C, Heydon K, Walsh TJ, Zaoutis TE. Hospitalization for endemic mycoses: Apopulation based national study. Clin Infect Dis. 2006;42:822–5. doi: 10.1086/500405. [DOI] [PubMed] [Google Scholar]
- 10.Lemos LB, Guo M, Baliga M. Blastomycosis: Organ involvement and etiologic diagnosis. A review of 123 patients from Mississippi. Ann Diagn Pathol. 2000;4:391–406. doi: 10.1053/adpa.2000.20755. [DOI] [PubMed] [Google Scholar]
- 11.Martynovicz MA, Prakash UB. Pulmonary blastomycosis: An appraisal of diagnostic techniques. Chest. 2002;121:768–73. doi: 10.1378/chest.121.3.768. [DOI] [PubMed] [Google Scholar]
- 12.Valdivia L, Nix D, Wright M, Lindberg E, Fagan T, Lieberman D, et al. Coccidioidomycosis as a common cause of community-acquired pneumonia. Emerg Infect Dis. 2006;12:958–62. doi: 10.3201/eid1206.060028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnson RH, Einstein HE. Coccidioidal meningitis. Clin Infect Dis. 2006;42:103–7. doi: 10.1086/497596. [DOI] [PubMed] [Google Scholar]
- 14.Galgiani JN, Catanzaro A, Cloud GA, Johnson RH, Williams PL, Mirels LF, et al. Comparison of oral fluconazole and itraconazole for progressive, nonmeningeal coccidioidomycosis: A randomised, double blind trial. Mycoses study group. Ann Intern Med. 2000;133:676–86. doi: 10.7326/0003-4819-133-9-200011070-00009. [DOI] [PubMed] [Google Scholar]
- 15.Wisplinghoff H, Bischoff T, Tallent SM, Seifert H, Wenzel RP, Edmond MB. Nosocomial bloodstream infections in US hospitals: Analysis of 24,179 cases from a prospective nationwide surveillance study. Clin Infect Dis. 2004;39:309–17. doi: 10.1086/421946. [DOI] [PubMed] [Google Scholar]
- 16.Horn DL, Neofytos D, Anaissie EJ, Fishman JA, Steinbach WJ, Olyaei AJ, et al. Epidemiology and outcomes of candidemia in 2019 patients: Data from the prospective antifungal therapy alliance registry. Clin Infect Dis. 2009;48:1695–703. doi: 10.1086/599039. [DOI] [PubMed] [Google Scholar]
- 17.Chakrabarti A, Mohan B, Shrivastava SK, Marak RS, Ghosh A, Ray P. Change in distribution and antifungal susceptibility of Candida species isolated from candidemia cases in a tertiary care center during 1996-2000. Indian J Med Res. 2002;116:5–12. [PubMed] [Google Scholar]
- 18.Rani R, Mohapatra NP, Mehta G, Randhawa VS. Changing trends of Candida species in neonatal septicaemia in a tertiary north Indian hospital. Indian J Med Microbiol. 2002;116:42–4. [PubMed] [Google Scholar]
- 19.Verma AK, Prasad KN, Singh M, Dixit AK, Ayyagari A. Candidemia in patients of a tertiary health care hospital from north India. Indian J Med Res. 2003;117:122–8. [PubMed] [Google Scholar]
- 20.Chow JK, Golan Y, Ruthazer R, Karchmer AW, Carmeli Y, Lichtenberg D, et al. Factors associated with candidemia caused by non- albicans Candida species versus Candida albicans in the intensive care unit. Clin Infect Dis. 2008;46:1206–13. doi: 10.1086/529435. [DOI] [PubMed] [Google Scholar]
- 21.Meersseman W, Lagrou K, Maertens J, Van Wijngaerden E. Invasive aspergillosis in the intensive care unit. Clin Infect Dis. 2007;45:205–16. doi: 10.1086/518852. [DOI] [PubMed] [Google Scholar]
- 22.Lusatia R, Amalfitano G, Lazzarini L, Soldani F, Bellino S, Solbiati M, et al. Nosocomial candidemia in non-neutropenic patients at an Italian tertiary care hospital. Eur J Clin Microbiol Infect Dis. 2000;19:602–7. doi: 10.1007/s100960000325. [DOI] [PubMed] [Google Scholar]
- 23.De Pauw B, Walsh TJ, Donnelly JP, Stevens DA, Edwards JE, Calandra T, et al. European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group. National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Revised definitions of invasive fungal disease from the European Organization for Research and Treatment of Cancer/Invasive Fungal Infections Cooperative Group and the National Institute of Allergy and Infectious Diseases Mycoses Study Group (EORTC/MSG) Consensus Group. Clin Infect Dis. 2008;46:1813–21. doi: 10.1086/588660. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.León C, Ruiz-Santana S, Saavedra P, Almirante B, Nolla-Salas J, Alvarez-Lerma F, et al. A bedside scoring system (“Candida score”) for early antifungal treatment in nonneutropenic critically ill patients with Candida colonization. Crit Care Med. 2006;34:730–7. doi: 10.1097/01.CCM.0000202208.37364.7D. [DOI] [PubMed] [Google Scholar]
- 25.León C, Ruiz-Santana S, Saavedra P, Galván B, Blanco A, Castro C, et al. Usefulness of the “Candida score” for discriminating between candida colonization and invasive candidiasis in non-neutropenic critically ill patients: A prospective multicenter study. Crit Care Med. 2009;37:1624–33. doi: 10.1097/CCM.0b013e31819daa14. [DOI] [PubMed] [Google Scholar]
- 26.Debase Z, Mattiuzzi G, Estey E, Kantarjian H, Saeki F, Ridge RJ, et al. Beta-D-glucan as a diagnostic adjunct for invasive fungal infections: Validation, cutoff development, and performance in patients with acute myelogenous leukemia and myelodysplastic syndrome. Clin Infect Dis. 2004;39:199–205. doi: 10.1086/421944. [DOI] [PubMed] [Google Scholar]
- 27.McMullan R, Metwally L, Coyle PV, Hedderwick S, McCloskey B, O’Neill HJ, et al. A prospective clinical trial of a real-time polymerase chain reaction assay for the diagnosis of candidemia in nonneutropenic, critically ill adults. Clin Infect Dis. 2008;46:890–6. doi: 10.1086/528690. [DOI] [PubMed] [Google Scholar]
- 28.Piarroux R, Grenouillet F, Balvay P, Tran V, Blasco G, Millon L, et al. Assessment of preemptive treatment to prevent severe candidiasis in critically ill surgical patients. Crit Care Med. 2004;32:2443–9. doi: 10.1097/01.ccm.0000147726.62304.7f. [DOI] [PubMed] [Google Scholar]
- 29.Pappas PG, Kauffman CA, Andes D, Benjamin DK, Jr, Calandra TF, Edwards JE, Jr, et al. Infectious Diseases Society of America. Clinical practice guidelines for the management of candidiasis: 2009 update by the Infectious Diseases Society of America. Clin Infect Dis. 2009;48:503–35. doi: 10.1086/596757. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Ostrosky-Zeichner L, Sable C, Sobel J, Alexander BD, Donowitz G, Kan V, et al. Multicenter retrospective development and validation of a clinical prediction rule for nosocomial invasive candidiasis in the intensive care setting. Eur J Clin Microbiol Infect Dis. 2007;26:271–6. doi: 10.1007/s10096-007-0270-z. [DOI] [PubMed] [Google Scholar]
- 31.Meersseman W, Vandecasteele SJ, Wilmer A, Verbeken E, Peetermans WE, Van Wijngaerden E. Invasive aspergillosis in critically ill patients without malignancy. Am J Respir Crit Care Med. 2004;170:621–5. doi: 10.1164/rccm.200401-093OC. [DOI] [PubMed] [Google Scholar]
- 32.Bulpa PA, Dive AM, Garrino MG, Delos MA, Gonzalez MR, Evrard PA, et al. Chronic obstructive pulmonary disease patients with invasive pulmonary aspergillosis: Benefits of intensive care? Intensive Care Med. 2001;27:59–67. doi: 10.1007/s001340000768. [DOI] [PubMed] [Google Scholar]
- 33.Greene RE, Schlamm HT, Oestmann JW, Stark P, Durand C, Lortholary O, et al. Imaging findings in acute invasive pulmonary aspergillosis: Clinical significance of the halo sign. Clin Infect Dis. 2007;44:373–9. doi: 10.1086/509917. [DOI] [PubMed] [Google Scholar]
- 34.Pfeiffer CD, Fine JP, Safdar N. Diagnosis of invasive aspergillosis using a galactomannan assay: A meta-analysis. Clin Infect Dis. 2006;42:1417–27. doi: 10.1086/503427. [DOI] [PubMed] [Google Scholar]
- 35.Walsh TJ, Raad I, Patterson TF, Chandrasekar P, Donowitz GR, Graybill R, et al. Treatment of invasive aspergillosis with posaconazole in patients who are refractory to or intolerant of conventional therapy: An externally controlled trial. Clin Infect Dis. 2007;44:2–12. doi: 10.1086/508774. [DOI] [PubMed] [Google Scholar]
- 36.Marr KA, Boeckh M, Carter RA, Kim HW, Corey L. Combination antifungal therapy for invasive aspergillosis. Clin Infect Dis. 2004;39:797–802. doi: 10.1086/423380. [DOI] [PubMed] [Google Scholar]
- 37.Nadrous HF, Antonios VS, Terrell CL, Ryu JH. Pulmonary cryptococcosis in nonimmunocompromised patients. Chest. 2003;124:2143–7. doi: 10.1016/s0012-3692(15)31671-8. [DOI] [PubMed] [Google Scholar]
- 38.Zinck SE, Leung AN, Frost M, Berry GJ, Muller NL. Pulmonary cryptococcosis: CT and pathologic findings. J Comput Assist Tomogr. 2002;26:330–4. doi: 10.1097/00004728-200205000-00002. [DOI] [PubMed] [Google Scholar]
- 39.Andrew HL, Kenneth SK, George AS, Neil MA, John EB, Antonio C, et al. An Official American Thoracic Society Statement: Treatment of Fungal Infections in Adult Pulmonary and Critical Care Patients. Am J Respir Crit Care Med. 2011;183:96–128. doi: 10.1164/rccm.2008-740ST. [DOI] [PubMed] [Google Scholar]
- 40.Aliouat-Denis C-M, Chabé M, Demanche C, Aliouat el M, Viscogliosi E, Guillot J, et al. Pneumocystis species, co-evolution and pathogenic power. Infect Genet Evol. 2008;8:708–26. doi: 10.1016/j.meegid.2008.05.001. [DOI] [PubMed] [Google Scholar]
- 41.Ledergerber B, Mocroft A, Reiss P, Furrer H, Kirk O, Bickel M, et al. Discontinuation of secondary prophylaxis against Pneumocystis carinii pneumonia in patients with HIV infection who have a response to antiretroviral therapy: Eight European study groups. N Engl J Med. 2001;344:168–74. doi: 10.1056/NEJM200101183440302. [DOI] [PubMed] [Google Scholar]


