Abstract
Purpose
Anorexia nervosa (AN) is a psychiatric disorder characterized by restrictive eating, low body weight, and severe bone loss. Recent data show a deleterious relationship between low circulating sodium levels and bone mass, and relative or absolute hyponatremia is a known complication of AN. Clinical studies of other medical conditions associated with hyponatremia suggest that detrimental effects of low sodium levels on health are seen even within the normal range. We hypothesized that women with AN and relatively low sodium levels would have lower bone mineral density (BMD) than those with higher sodium levels.
Methods
In a cross-sectional study (1997–2009) of 404 women ages 17–54 (mean±SEM age 25.6±0.3 years) who met DSM-IV criteria for AN, we measured BMD using dual energy x-ray absorptiometry (DXA). BMD was compared in women with sodium levels <140 mmol/L (midpoint of normal range) vs. those with sodium levels ≥140 mmol/L, and in women with hyponatremia (sodium <135 mmol/L) vs. those without.
Results
Women with sodium levels <140 mmol/L had lower BMD, T- and Z-scores at the AP spine (Z-scores −1.6±0.1 vs. −1.3±0.1, p=0.004) and total hip (−1.2±0.1 vs. −0.9±0.1, p=0.029) vs. those with sodium levels ≥140 mmol/L. In a model including age, BMI, psychiatric drug use, and disease duration, differences remained significant at the AP spine. Hyponatremic women had lower BMD, T- and Z-scores at the AP spine (Z-scores −2.2±0.3 vs. −1.3±0.1, p=0.009), lateral spine (−2.4±0.4 vs. −1.5±0.1, p=0.031) and total hip (−2.5±0.5 vs. −1.0±0.1, p<0.0001) vs. those without. In a model including age, BMI, psychiatric drug use, and disease duration, differences remained significant at all sites.
Conclusions
These data suggest that relative sodium deficiency may contribute to AN-related osteopenia.
Keywords: Anorexia nervosa, hyponatremia, osteopenia, dual energy x-ray absorptiometry
Introduction
Anorexia nervosa is a psychiatric disorder characterized by restrictive eating, low body weight, and severe bone loss. In a study of 130 women with anorexia nervosa, mean age 24 years old, Grinspoon et al. found that more than 90% had osteopenia and nearly 40% had osteoporosis at one or more skeletal sites (1). Consistent with these data, Miller et al. reported that only 14% of 214 ambulatory young women with anorexia nervosa had normal bone mineral density at all sites, and 30% reported a history of bone fracture (2). The risk of fractures in women with anorexia nervosa is up to 7 times that of age-matched healthy women (3). Anorexia nervosa-induced bone loss in adult women reflects a decrease in bone formation and increase in bone resorption, which has been attributed to nutritional deficiencies and endocrine abnormalities, including hypoestrogenemia, growth hormone resistance, and hypercortisolemia (4). Recent reports indicate that hyponatremia, a complication of anorexia nervosa (2), has deleterious effects on bone (5–10). Verbalis, Barsony et al. demonstrated that experimentally-induced hyponatremia in rats results in a marked reduction in bone mineral density and trabecular and cortical parameters (5). Clinical studies of other medical conditions associated with hyponatremia suggest that detrimental effects of low sodium levels on health are seen even within the normal range (11–14). We hypothesized that women with anorexia nervosa and relatively low plasma sodium levels would have lower bone mineral density than those with higher sodium levels, suggesting that sodium deficiency may contribute to the profound bone loss seen in this disorder.
Methods
Subjects
404 women (18–54 years of age) who completed a screening visit between January 1, 1997 and December 31, 2009 in the Neuroendocrine Unit at the Massachusetts General Hospital for studies involving bone density determinations in adult women with anorexia nervosa were included in the study. Subjects met DSM-IV criteria (intense fear of gaining weight, emphasis on body shape, weight less than 85% of ideal body weight), other than amenorrhea. Women who were pregnant were excluded from the study. Participants were recruited through referrals from local eating disorder providers and on-line advertisements. Subject characteristics, sodium levels, and DXA results have been previously reported in subsets, but the relationship between sodium levels and bone density has not been described (1, 2, 15–21).
Methods
The study was approved by the Partners Institutional Review Board and complied with the Health Insurance Portability and Accountability Act guidelines. Written informed consent was obtained from all participants.
Subjects had a complete medical history and physical exam performed by a physician, physician’s assistant or nurse practitioner at the Massachusetts General Hospital Clinical Research Center. Height was measured as the average of three readings on a single stadiometer. Elbow breadth was measured using calipers and compared to norms based on NHANES-I data (for estimation of frame size). Participants were weighed on an electronic scale while wearing a hospital gown. Body mass index (BMI) was calculated using the formula [weight (kg)/height (meter)2] and percent ideal body weight was calculated based on 1983 Metropolitan Life Height and Weight Tables (22). Bone mineral density at the anterior-posterior (AP) spine (L1–L4), lateral spine (L2–L4) and total hip was determined using dual energy x-ray absorptiometry (DXA) (Hologic QDR 4500, Waltham, MA). This technique has a precision of 0.01 g/cm2 at the lumbar spine (23). Plasma sodium levels were measured by the MGH clinical pathology laboratories using a Roche/Hitachi fully automated chemistry analyzer [Roche Diagnostics, Indianapolis, IN] (normal range 135–145 mmol/L) and closely monitored for consistency over the study timeframe (24).
Data Analysis
JMP Statistical Discoveries (Version 9.0.0; SAS Institute, Inc., Cary, NC) was used for statistical analyses. Clinical characteristics and measures of bone mineral density were compared using the Student t-test. Multivariable least-squares analyses were constructed to control for potential confounders. Statistical significance was defined as a two-tailed P-value < 0.05. Data are reported as mean ± SEM.
Results
Subject Characteristics: Women with sodium levels at or above vs. below 140 mmol/L
Subject characteristics are presented in Table I. Mean age of subjects was 25.6±0.3 years. 23% of the AN reported binge/purge activity. Sodium levels did not differ between those who purged and those who did not (140.6±0.3 vs. 140.6±0.2 mmol/L, p=NS). 117 of the 404 women had sodium levels below 140 mmol/L (the midpoint of the normal range). Women with sodium levels below 140 mmol/L were older and reported greater duration of anorexia nervosa than those with sodium levels at or above 140 mmol/L. A greater percentage of the women with sodium below 140 mmol/L reported current psychiatric medication use than those with sodium levels at or above 140 mmol/L (66% vs. 49%, p=0.002). 50% of subjects with sodium levels below 140mmol/L were on SSRI’s compared to 37% of those at or above 140 mmol/L (p=0.01). The percentage of subjects on antipsychotics (16% vs. 13%, p=NS) did not differ between those with sodium levels below 140 mmol/L and those at or above 140 mmol/L. BMI, age of diagnosis, estrogen use (oral or transdermal), and age at menarche did not differ between the groups. 64% of those with sodium levels greater than or equal to 140 mmol/L and 64% of those with sodium levels less than 140 mmol/L were ammenorrheic (p=NS).
Table I.
Clinical characteristics and differences in bone mineral density based on plasma sodium
| Na cutoff at midpoint of normal | Na cutoff at low end of normal | |||||
|---|---|---|---|---|---|---|
| Na<140 N=117 |
Na≥140 N=287 |
p-value | Na<135 N=12 |
Na≥135 N=392 |
p-value | |
| Clinical Characteristics | ||||||
| Age (years) | 27.5±0.7 | 24.8±0.4 | 0.0005 | 31.3±1.9 | 25.4±0.3 | 0.004 |
| Body mass index (kg/m2) | 16.9±0.1 | 17.2±0.1 | NS | 15.4±0.6 | 17.2±0.1 | 0.0009 |
| Height (cm) | 164.2±0.7 | 164.7±0.4 | NS | 164.1±2.4 | 164.5±0.3 | NS |
| Age of diagnosis (years) | 20.3±0.6 | 20.0±0.4 | NS | 21.6±1.9 | 20.0±0.3 | NS |
| Years of AN | 6.9±0.7 | 4.9±0.4 | 0.007 | 9.7±2.0 | 5.3±0.4 | 0.022 |
| Age at menarche (years) | 13.4±0.2 | 13.4±0.1 | NS | 13.7±0.6 | 13.4±0.1 | NS |
| Bone mineral density | ||||||
| AP Spine | ||||||
| BMD | 0.850±0.011 | 0.891±0.007 | 0.002 | 0.774±0.035 | 0.883±0.006 | 0.002 |
| T-Score | −1.8±0.1 | −1.4±0.1 | 0.004 | −2.6±0.4 | −1.5±0.0 | 0.002 |
| Z-Score | −1.6±0.1 | −1.3±0.1 | 0.004 | −2.2±0.3 | −1.3±0.1 | 0.009 |
| Lat Spine | ||||||
| BMD | 0.657±0.010 | 0.675±0.006 | 0.095 | 0.581±0.029 | 0.673±0.005 | 0.002 |
| T-Score | −2.0±0.1 | −1.8±0.1 | 0.093 | −3.2±0.5 | −1.8±0.1 | 0.0008 |
| Z-Score | −1.6±0.1 | −1.5±0.1 | NS | −2.4±0.4 | −1.5±0.1 | 0.031 |
| Total Hip | ||||||
| BMD | 0.790±0.013 | 0.832±0.113 | 0.002 | 0.630±0.036 | 0.825±0.006 | <0.0001 |
| T-Score | −1.2±0.1 | −0.9±0.1 | 0.009 | −2.6±0.5 | −1.0±0.1 | <0.0001 |
| Z-Score | −1.2±0.1 | −0.9±0.1 | 0.029 | −2.5±0.5 | −1.0±0.1 | <0.0001 |
Mean±S.E.M. Na, sodium (mmol/L).
Subject Characteristics: Women with vs. without hyponatremia
12 of the 404 women were hyponatremic (sodium less than 135 mmol/L). Women with hyponatremia were older, had lower BMI, and reported greater duration of anorexia nervosa than those without hyponatremia. A greater percentage of the women with hyponatremia reported current psychiatric medication use than those without hyponatremia (83% vs. 53%, p=0.04). The percentage of subjects on SSRI’s (58% vs. 40%, p=NS) and antipsychotics (33% vs. 13%, p=0.08) did not significantly differ between those with hyponatremia and those without. Age of diagnosis, estrogen use (oral or transdermal), and age at menarche did not differ between the groups. 75% of those with hyponatremia and 64% of those without were amenorrheic (p=NS).
Bone Mineral Density: Women with sodium levels at or above vs. below 140 mmol/L
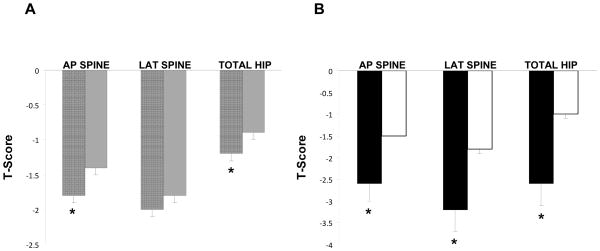
Table I and Figure I present differences in bone mineral density, T- and Z-scores based on plasma sodium levels. Women with sodium levels below 140 mmol/L had lower BMD, T- and Z-scores at the AP spine and total hip compared to those with sodium levels at or above 140 mmol/L. There was a trend toward lower BMD and T-scores at the lateral spine in those with sodium levels below 140 mmol/L compared to those at or above 140 mmol/L. In a model including age, BMI, psychiatric drug use, and disease duration, differences remained significant at the AP spine. When SSRI and antipsychotic use was substituted for psychiatric drug use in the model, the findings were similar.
Figure 1. Differences in bone mineral density (BMD) based on level of plasma sodium.
T-scores were lower in women with anorexia nervosa with plasma sodium levels A) less than 140 (black stripes) compared to those equal to or greater than 140 (gray) and B) less than 135 (black) compared to those equal to or greater than 135 mmol/L (white), *p<0.01. Mean±S.E.M. AP, anterior-posterior.
Bone Mineral Density: Women with vs. without hyponatremia
Hyponatremic women had lower BMD, T- and Z-scores at every site compared to those without hyponatremia (Table I, Figure I). In a model including age, BMI, psychiatric drug use, and disease duration, differences remained significant at all sites. When SSRI and antipsychotic use was substituted for psychiatric drug use in the model, the findings were similar.
Discussion
In this cross-sectional study of more than 400 women with anorexia nervosa, we found that those with lower plasma sodium levels had more severe bone loss, independent of age, BMI, psychiatric medication use and disease duration. Notably, these differences were evident within the normal sodium range.
Hyponatremia, even when mild and asymptomatic, has been associated with increased risk of fractures in older adults (7–10). NHANES III participants 50 years of age or older who had hyponatremia were more likely to have osteoporosis at the femoral neck and total hip than those who had normal sodium levels (5). Using a rat model for the syndrome of inappropriate antiduretic hormone (SIADH), Verbalis, Barsony et al. found that three months of hyponatremia (mean sodium 110±2 mmol/L) resulted in a 30% reduction in bone mineral density compared to normonatremic controls. In addition, cortical and trabecular microarchitectural parameters were severely impaired in the chronically hyponatremic rats. Based on the findings of a five-fold increase in osteoclast number per bone area, suggesting increased resorptive activity, and a relative decrease in concentration of the bone formation marker osteocalcin in hyponatremic rats compared to controls, the authors concluded that chronic hyponatremia leads to bone loss through an uncoupling of bone resorption and formation (5). Cellular and molecular studies have confirmed increased osteoclastic bone resorption in response to low extracellular sodium levels (6). Resorption of sodium from bone is thought to be a mechanism to restore blood sodium levels to normal (5, 6). Recent research has called into question whether the established reference range for sodium is appropriate, given the increased morbidity and mortality seen in patients with relatively low sodium levels in the normal range (11–14).
Women with anorexia nervosa are at risk for hyponatremia due to inappropriate secretion of vasopressin, a posterior pituitary peptide hormone that acts at the kidneys to increase resorption of free water (25). Other contributors to low sodium levels in these women include excessive water consumption, hypovolemia due to inadequate nutrition and purging behaviors, impaired renal sodium reabsorption in the setting of malnutrition, and use of psychotropic medications that result in SIADH or polydipsia (26–29). Given the prevalence of hyponatremia and osteopenia in women with anorexia nervosa, we studied whether relatively low plasma sodium levels in these women were associated with the severity of osteopenia. Whether we used a plasma sodium cutoff at the lower end or middle of the normal range, we found that those women with relatively lower sodium levels had more severe bone loss, independent of potential confounders.
In our study, women with relatively low sodium levels tended to be older with a longer duration of illness and were more likely to report current use of psychiatric medications. Those with frank hyponatremia also had a lower mean BMI. Lower sodium levels may therefore reflect severity of illness in anorexia nervosa and/or use of psychiatric medications. Importantly, differences in bone mineral density were still significant after controlling for these factors.
In summary, we report increased severity of bone loss in patients with lower plasma sodium levels, independent of age, BMI, psychiatric medication use and disease duration. This is a cross-sectional study, and therefore causality cannot be determined. However, these data suggest that relatively low plasma sodium levels may contribute to the severe bone loss seen in women with anorexia nervosa.
Clinical Points.
Women with anorexia nervosa are at risk for hyponatremia and severe osteopenia
Animal models suggest that hyponatremia results in bone loss
Women with anorexia nervosa and lower plasma sodium levels have more severe bone loss than those with higher plasma sodium levels
Relatively low plasma sodium levels may contribute to anorexia nervosa-induced bone loss
Acknowledgments
This work was supported in part by the following grants from the National Institutes of Health: R01 DK052625, DK062249, DK084970, MH083657, ULIRR0257801 and M01 RR01066. We thank the nurses and bionutritionists in the Massachusetts General Hospital Clinical Research Center and the subjects who participated in the study.
Footnotes
The authors have no conflicts to declare.
References
- 1.Grinspoon S, Thomas E, Pitts S, Gross E, Mickley D, Miller K, Herzog D, Klibanski A. Prevalence and predictive factors for regional osteopenia in women with anorexia nervosa. Ann Intern Med. 2000;133:790–794. doi: 10.7326/0003-4819-133-10-200011210-00011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Miller KK, Grinspoon SK, Ciampa J, Hier J, Herzog D, Klibanski A. Medical findings in outpatients with anorexia nervosa. Arch Intern Med. 2005;165:561–566. doi: 10.1001/archinte.165.5.561. [DOI] [PubMed] [Google Scholar]
- 3.Rigotti NA, Neer RM, Skates SJ, Herzog DB, Nussbaum SR. The Clinical Course of Osteoporosis in Anorexia Nervosa. JAMA: The Journal of the American Medical Association. 1991;265:1133–1138. [PubMed] [Google Scholar]
- 4.Lawson EA, Klibanski A. Endocrine abnormalities in anorexia nervosa. Nat Clin Pract Endocrinol Metab. 2008;4:407–414. doi: 10.1038/ncpendmet0872. [DOI] [PubMed] [Google Scholar]
- 5.Verbalis JG, Barsony J, Sugimura Y, Tian Y, Adams DJ, Carter EA, Resnick HE. Hyponatremia-induced osteoporosis. J Bone Miner Res. 2010;25:554–563. doi: 10.1359/jbmr.090827. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Barsony J, Sugimura Y, Verbalis JG. Osteoclast response to low extracellular sodium and the mechanism of hyponatremia-induced bone loss. J Biol Chem. 2011;286:10864–10875. doi: 10.1074/jbc.M110.155002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Gankam Kengne F, Andres C, Sattar L, Melot C, Decaux G. Mild hyponatremia and risk of fracture in the ambulatory elderly. QJM. 2008;101:583–588. doi: 10.1093/qjmed/hcn061. [DOI] [PubMed] [Google Scholar]
- 8.Sandhu HS, Gilles E, DeVita MV, Panagopoulos G, Michelis MF. Hyponatremia associated with large-bone fracture in elderly patients. Int Urol Nephrol. 2009;41:733–737. doi: 10.1007/s11255-009-9585-2. [DOI] [PubMed] [Google Scholar]
- 9.Kinsella S, Moran S, Sullivan MO, Molloy MG, Eustace JA. Hyponatremia independent of osteoporosis is associated with fracture occurrence. Clin J Am Soc Nephrol. 2010;5:275–280. doi: 10.2215/CJN.06120809. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Hoorn EJ, Rivadeneira F, van Meurs JB, Ziere G, Stricker BH, Hofman A, Pols HA, Zietse R, Uitterlinden AG, Zillikens MC. Mild hyponatremia as a risk factor for fractures: the Rotterdam Study. J Bone Miner Res. 2011;26:1822–1828. doi: 10.1002/jbmr.380. [DOI] [PubMed] [Google Scholar]
- 11.Klein L, O’Connor CM, Leimberger JD, Gattis-Stough W, Pina IL, Felker GM, Adams KF, Jr, Califf RM, Gheorghiade M. Lower serum sodium is associated with increased short-term mortality in hospitalized patients with worsening heart failure: results from the Outcomes of a Prospective Trial of Intravenous Milrinone for Exacerbations of Chronic Heart Failure (OPTIME-CHF) study. Circulation. 2005;111:2454–2460. doi: 10.1161/01.CIR.0000165065.82609.3D. [DOI] [PubMed] [Google Scholar]
- 12.Wald R, Jaber BL, Price LL, Upadhyay A, Madias NE. Impact of hospital-associated hyponatremia on selected outcomes. Arch Intern Med. 2010;170:294–302. doi: 10.1001/archinternmed.2009.513. [DOI] [PubMed] [Google Scholar]
- 13.Gheorghiade M, Abraham WT, Albert NM, Gattis Stough W, Greenberg BH, O’Connor CM, She L, Yancy CW, Young J, Fonarow GC. Relationship between admission serum sodium concentration and clinical outcomes in patients hospitalized for heart failure: an analysis from the OPTIMIZE-HF registry. Eur Heart J. 2007;28:980–988. doi: 10.1093/eurheartj/ehl542. [DOI] [PubMed] [Google Scholar]
- 14.Kim WR, Biggins SW, Kremers WK, Wiesner RH, Kamath PS, Benson JT, Edwards E, Therneau TM. Hyponatremia and mortality among patients on the liver-transplant waiting list. N Engl J Med. 2008;359:1018–1026. doi: 10.1056/NEJMoa0801209. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Grinspoon S, Miller K, Coyle C, Krempin J, Armstrong C, Pitts S, Herzog D, Klibanski A. Severity of osteopenia in estrogen-deficient women with anorexia nervosa and hypothalamic amenorrhea. J Clin Endocrinol Metab. 1999;84:2049–2055. doi: 10.1210/jcem.84.6.5792. [DOI] [PubMed] [Google Scholar]
- 16.Miller KK, Grinspoon S, Gleysteen S, Grieco KA, Ciampa J, Breu J, Herzog DB, Klibanski A. Preservation of neuroendocrine control of reproductive function despite severe undernutrition. J Clin Endocrinol Metab. 2004;89:4434–4438. doi: 10.1210/jc.2004-0720. [DOI] [PubMed] [Google Scholar]
- 17.Lawson EA, Miller KK, Mathur VA, Misra M, Meenaghan E, Herzog DB, Klibanski A. Hormonal and nutritional effects on cardiovascular risk markers in young women. J Clin Endocrinol Metab. 2007;92:3089–3094. doi: 10.1210/jc.2007-0364. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Miller KK, Lawson EA, Mathur V, Wexler TL, Meenaghan E, Misra M, Herzog DB, Klibanski A. Androgens in women with anorexia nervosa and normal-weight women with hypothalamic amenorrhea. J Clin Endocrinol Metab. 2007;92:1334–1339. doi: 10.1210/jc.2006-2501. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Miller KK, Lee EE, Lawson EA, Misra M, Minihan J, Grinspoon SK, Gleysteen S, Mickley D, Herzog D, Klibanski A. Determinants of skeletal loss and recovery in anorexia nervosa. J Clin Endocrinol Metab. 2006;91:2931–2937. doi: 10.1210/jc.2005-2818. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Lawson EA, Miller KK, Bredella MA, Phan C, Misra M, Meenaghan E, Rosenblum L, Donoho D, Gupta R, Klibanski A. Hormone predictors of abnormal bone microarchitecture in women with anorexia nervosa. Bone. 2009;46:458–463. doi: 10.1016/j.bone.2009.09.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Bredella MA, Fazeli PK, Miller KK, Misra M, Torriani M, Thomas BJ, Ghomi RH, Rosen CJ, Klibanski A. Increased bone marrow fat in anorexia nervosa. J Clin Endocrinol Metab. 2009;94:2129–2136. doi: 10.1210/jc.2008-2532. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Metropolitan height and weight tables. Stat Bull. 1983;64:2–9. [PubMed] [Google Scholar]
- 23.Mazess RB, Barden HS, Bisek JP, Hanson J. Dual-energy x-ray absorptiometry for total-body and regional bone-mineral and soft-tissue composition. Am J Clin Nutr. 1990;51:1106–1112. doi: 10.1093/ajcn/51.6.1106. [DOI] [PubMed] [Google Scholar]
- 24.Kratz A, Ferraro M, Sluss PM, Lewandrowski KB. Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Laboratory reference values. N Engl J Med. 2004;351:1548–1563. doi: 10.1056/NEJMcpc049016. [DOI] [PubMed] [Google Scholar]
- 25.Gold PW, Kaye W, Robertson GL, Ebert M. Abnormalities in plasma and cerebrospinal-fluid arginine vasopressin in patients with anorexia nervosa. N Engl J Med. 1983;308:1117–1123. doi: 10.1056/NEJM198305123081902. [DOI] [PubMed] [Google Scholar]
- 26.Caregaro L, Di Pascoli L, Favaro A, Nardi M, Santonastaso P. Sodium depletion and hemoconcentration: overlooked complications in patients with anorexia nervosa? Nutrition. 2005;21:438–445. doi: 10.1016/j.nut.2004.08.022. [DOI] [PubMed] [Google Scholar]
- 27.Bahia A, Chu ES, Mehler PS. Polydipsia and hyponatremia in a woman with anorexia nervosa. Int J Eat Disord. 2011;44:186–188. doi: 10.1002/eat.20792. [DOI] [PubMed] [Google Scholar]
- 28.Evrard F, da Cunha MP, Lambert M, Devuyst O. Impaired osmoregulation in anorexia nervosa: a case-control study. Nephrol Dial Transplant. 2004;19:3034–3039. doi: 10.1093/ndt/gfh507. [DOI] [PubMed] [Google Scholar]
- 29.Letmaier M, Painold A, Holl AK, Vergin H, Engel R, Konstantinidis A, Kasper S, Grohmann R. Hyponatraemia during psychopharmacological treatment: results of a drug surveillance programme. The International Journal of Neuropsychopharmacology FirstView. 2011:1–10. doi: 10.1017/S1461145711001192. [DOI] [PubMed] [Google Scholar]