Introduction
The G antigen belongs to the Rh system and is present on most D-positive red blood cells (RBC) and on most C-positive RBC1. For this reason, the true specificity of serum that apparently has anti-D and anti-C specificity when tested with the usual panels for the identification of irregular antibodies could correspond to one of the five possible combinations: anti-D and anti-C (D+C), anti-D and anti-G (D+G), anti-D and anti-C and anti-G (D+C+G), anti-C and anti-G (C+G), and anti-G2.
The correct identification of the specificity and, in particular, the determination of whether anti-D is present or not are of paramount clinical importance in different clinical settings. In pregnant women, the presence of anti-D excludes the need for the administration of prophylactic anti-D immunoglobulin (RhIG). In addition, the exclusion of the presence of anti-D in samples from D-negative women with D-negative partners or from D-negative recipients of D-negative blood components can avoid potential social or medico-legal complications2.
We describe here a simple approach that enables us to determine whether anti-D is present or not in serum presumed to contain anti-D and anti-C specificity. This protocol was employed in the study of 32 samples with presumed anti-D+C specificity confirming the utility of this simple and less time-consuming strategy.
Material and methods
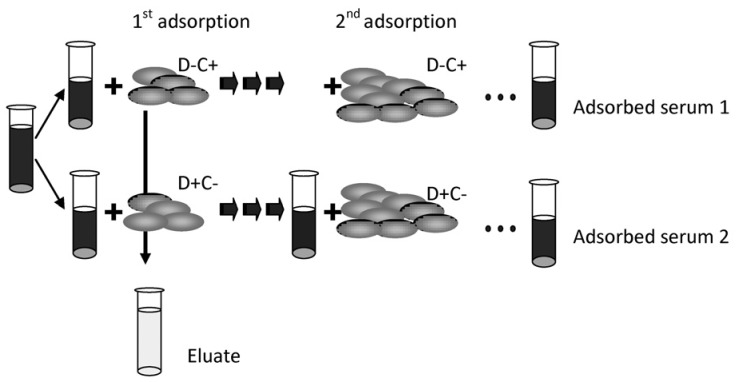
Our main aim was to demonstrate unequivocally the presence of anti-D in samples. To this aim an alternative to the usual protocol was developed (Figure 1). This alternative includes: (i) the adsorption of an aliquot of the serum under investigation with r'r packed RBC (D-negative, C-positive) as many times as is necessary to obtain a serum that is non-reactive with those RBC; (ii) the study of the adsorbed serum (adsorbed serum 1 in Figure 1) with R2R2 and r'r RBC. This procedure is sufficient to immediately confirm or exclude the presence of anti-D in the serum under investigation.
Figure 1.
The new proposed protocol.
If we additionally want to determine whether or not anti-C is present, a second aliquot of the serum under investigation is subjected to a similar procedure, this time using R2R2 or R0r packed RBC (D-positive, C-negative) in the adsorption.
In the cases in which only an anti-D or anti-C is identified or no antibody is identified in the adsorbed serum, the original anti-D and anti-C reactivity should be attributed to the presence of anti-G.
For the purpose of determining whether anti-G is present in a sample with both anti-D and anti-C, an eluate must be prepared (Gamma ELU-KITTM II) from one of the two cells employed in the first adsorption of the two aliquots (e.g. the D-negative and C-positive cells) and then this eluate is studied with R2R2 and r'r cells (examples 1 and 3 in Table I).
Table I.
Detection of anti-D by the new proposed protocol.
| Example | Aliquot 1 (Adsorbed serum with D-C+ cells) | Aliquot 2 (Adsorbed serum with D+C- cells) | Eluate* | Antibodies identified | |||
|---|---|---|---|---|---|---|---|
|
| |||||||
| R2R2 | r'r | R2R2 | r'r | R2R2 | r'r | ||
| 1 | + | 0 | 0 | + | 0 | + | D+C |
| 2 | + | 0 | 0 | 0 | D+G | ||
| 3 | + | 0 | 0 | + | + | + | D+C+G |
| 4 | 0 | 0 | 0 | + | C+G | ||
| 5 | 0 | 0 | 0 | 0 | G | ||
Legend
The eluate had been prepared from the red blood cells used in the first adsorption procedure with the serum under investigation (Aliquot 1).
With the aim of increasing the speed of the adsorptions (especially in the cases in which the titres were equal to or higher than 16), we used three volumes of cells for one volume of serum and the complete adsorption was controlled by the human direct antiglobulin test carried out every 15 minutes. When a 4+ reaction was obtained, the adsorbed serum was separated and moved on to the next adsorption. If the reaction was ≤3+ the adsorption procedure was maintained for 60 minutes.
Alternatively, the adsorption procedure could be performed with PEG. In this case one volume of cells, one of serum and one of PEG were incubated 15 minutes three times. To confirm the complete adsorption the adsorbed serum was tested with the same cells employed in the adsorption. If reactivity persisted the adsorption procedure was continued until a negative result was obtained.
Both protocols allowed us to obtain completely adsorbed serums within 2 to 3 hours depending on the original antibody titre. In addition, they allowed us to determine the titres of anti-D and anti-C in the adsorbed aliquots and to compare them to those in the original sample.
In order to validate this new strategy we studied 32 serum samples, 27 from pregnant women and five from patients in whom an apparent anti-D+C specificity was detected. Two of the pregnant women did not have obstetric or transfusion histories and their partners were D-negative. The transfusion of D-negative blood components was confirmed in four of the five patients.
Results
The presence of anti-D was confirmed in 20 out of the 32 samples, and the following results were obtained: anti-D+C (n=5), anti-D+C+G (n=10), anti-D+G (n=5). Anti-D was excluded in the remaining 12 samples, with the specificities of these samples being anti-C+G (n=10) and anti-G (n=2) (Table II). We demonstrated that anti-D was not present in eight pregnant women, with the result that they were able to receive the corresponding RhIG dose. In addition, we observed that anti-D was always present in the cases in which the foetus was severely affected, and absent when the adverse effects were mild or absent. Finally, the neonates of the two mothers in which only anti-G was identified did not have haemolytic disease.
Table II.
Results obtained in the study of 32 serum samples with a presumed anti-D and anti-C specificity.
| D+C | D+G | D+C+G | C+G | G | |
|---|---|---|---|---|---|
| Pregnant women 27 |
5 | 5 | 9 | 6 | 2 |
| Patients 5 |
0 | 0 | 1 | 4 | 0 |
| HDN | Severe (1) | Severe (4) | Severe (3) | Mild (1) | Absent |
Legend HDN: haemolytic disease of the newborn.
We confirmed that the partners of two out of 27 pregnant women were D negative but with an r'r (dCe/dce) phenotype. Likewise, we confirmed that four out of five transfused patients had received some r'r phenotype blood components. In these six cases an anti-G and an anti-C were identified, and the absence of anti-D was demonstrated.
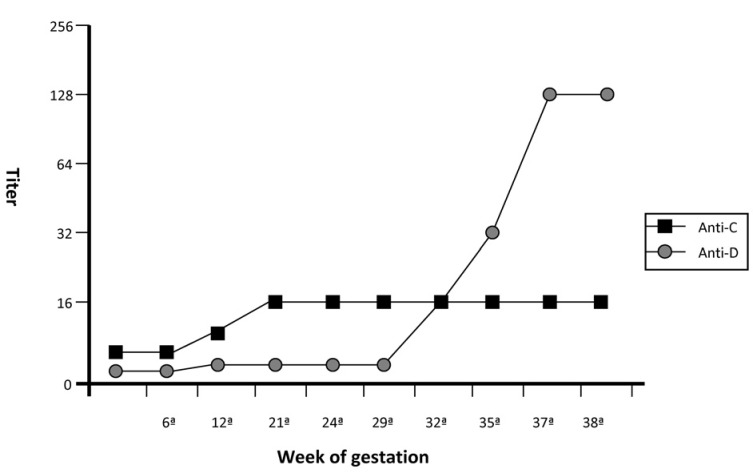
In the course of the study, we also had the opportunity to encounter a peculiar situation related to one of the pregnant women. In an early phase of the pregnancy, we demonstrated the presence of anti-D and anti-G in the serum sample mimicking anti-D+C specificity. In the first 29 weeks of pregnancy the presumed anti-C titre was higher than the anti-D titre (Figure 2). According to the literature, the presence of an anti-G should be considered in such cases. However, this does not exclude the possible coexistence of an anti-D in the sample. From the 29th week of gestation onwards, the woman's anti-D titre started to increase until it reached a critical level of 128. This resulted in severe haemolytic disease of the newborn and in the need for several blood transfusions because of recurrent anaemia. It should be noted that the pregnant woman did not receive the prophylactic dose of RhIG during her pregnancy.
Figure 2.
Titre of the presumed antibodies in a woman with anti-D+G. The titre of the presumed anti-C was higher than the titre of anti-D until the 29th week of gestation.
Discussion
The G antigen is present on almost all D-positive or C-positive red cells and absent from those that are D-negative or C-negative. CDE-negative, G-negative individuals exposed to D-negative, C-positive and G-positive (rarely C-negative and G-positive) RBC may produce an antibody which serologically resembles anti-D+C1. The correct identification of antibodies in samples apparently containing anti-D+C can distinguish several usual antibody combinations: anti-D+C+G, anti-D+G, anti-C+G, anti-G and anti-D+C2. Anti-D is known to be the most clinically important antibody, capable of causing severe haemolytic disease of the newborn and haemolytic transfusion reactions3,4. Anti-C, on the other hand, usually induces less severe disease, and the role of anti-G is still controversial3,5,6. It is, therefore, of paramount importance to confirm the presence of anti-D in samples from antenatal patients and in pre-transfusion testing of samples that apparently have anti-D+C specificity. Prophylaxis with RhIG should be limited to D-negative pregnant women who have not been sensitised to the D antigen3,7. Moreover, for medico-legal reasons, it may be necessary to exclude the presence of anti-D in pregnant women with D-negative partners, or in D-negative patients previously transfused with D-negative blood components2.
Allen and Tippett1 were the first to recognise the existence of the G antigen on D-negative, C-negative RBC, while Vos8 described the isolation of anti-G by a tedious and relatively complex double adsorption and elution procedure.
Our simpler and less-time consuming strategy enables us to confirm the presence or absence of anti-D with a single adsorption procedure. Anti-C+G or anti-G, without anti-D, was identified in eight out of the 27 pregnant women initially identified as having anti-D+C. Consequently, all these women had received RhIG. Likewise, anti-C+G, without anti-D, was identified in four out of the five patients previously transfused with D-negative blood products.
Anti-G appears to be usually associated with an anti-D and/or an anti-C, although it can also be detected alone as in the two pregnant women in our study in whom anti-G was the only specificity identified. In cases in which anti-D or anti-C is demonstrated, and in cases in which no antibodies are identified, it is possible to deduce the presence of anti-G in the original sample. Likewise, when both anti-D and anti-C are identified, an eluate must be prepared from one of the two cells used for the first adsorption in order to confirm the coexistence of anti-G.
As regards the clinical significance of our findings in the group of 27 pregnant women, we observed severe haemolytic disease only in cases in which anti-D was present. The absence of anti-D seems to be associated with a diminished risk of haemolytic disease of the newborn. However, the clinical significance of anti-G alone still remains controversial5.
It is generally accepted that in samples initially identified as containing anti-D+C, a titre of anti-C higher than anti-D make the presence of anti-G feasible. We cannot confirm this observation in all of our cases and, for this reason, we believe that the presence of anti-G should always be suspected regardless of the titres of anti-D and anti-C found. Likewise, we have provided the example of a pregnant woman in who anti-D and anti-G were identified in an early phase of her pregnancy when the titre of the presumed anti-C was clearly higher than the anti-D titre. However, from the 29th week of gestation onwards, anti-D titre started to increase until it reached a critical level of 128 resulting in severe haemolytic disease of the newborn. This case also illustrates the potential for misleading information and misinterpretation if the analysis of samples from pregnant women initially identified as containing anti-D+C are not regularly examined.
Our approach is rapid and readily accessible to most laboratories. With a few steps it is possible to ascertain whether an anti-D is present or not, and with a few more steps it is possible to confirm the exact composition of the antibodies present in the sample under investigation. For the above reasons, whenever an anti-D and anti-C specificity is detected in the serum of a pregnant woman, a strategy such as the one proposed should be adopted in order to confirm unequivocally the presence or absence of the anti-D specificity.
Footnotes
The Authors declare no conflict of interest.
References
- 1.Allen FH, Tippett PA. A new Rh blood type which reveals the Rh antigen G. Vox Sang. 1958;3:321–30. doi: 10.1111/j.1423-0410.1958.tb04013.x. [DOI] [PubMed] [Google Scholar]
- 2.Palfi M, Gunnarsson C. The frequency of anti-C and anti-G in the absence of anti-D in alloimmunized pregnancies. Transfus Med. 2001;11:207–10. doi: 10.1046/j.1365-3148.2001.00306.x. [DOI] [PubMed] [Google Scholar]
- 3.Shirey RS, Mirabella DC, Lumadue JA, et al. Differentiation of anti-D, -C, and -G: clinical relevance in alloimmunized pregnancies. Transfusion. 1997;37:493–6. doi: 10.1046/j.1537-2995.1997.37597293879.x. [DOI] [PubMed] [Google Scholar]
- 4.Bowman JM, Pollock JM, Manning FA, et al. Severe anti-C hemolytic disease of the newborn. Am J Obstet Gynecol. 1992;166:1239–43. doi: 10.1016/s0002-9378(11)90614-0. [DOI] [PubMed] [Google Scholar]
- 5.Hadley AG, Poole GD, Poole J, et al. Haemolytic disease of the newborn due to anti-G. Vox Sang. 1996;71:108–12. doi: 10.1046/j.1423-0410.1996.7120108.x. [DOI] [PubMed] [Google Scholar]
- 6.Cash K, Brown T, Strupp A, et al. Anti-G in a pregnant patient. Transfusion. 1999;39:531–3. doi: 10.1046/j.1537-2995.1999.39050531.x. [DOI] [PubMed] [Google Scholar]
- 7.Maley M, Babb R, Chapman CE, et al. Identification and quantification of anti-D, -C, -G in alloimmunized pregnant women. Transfus Med. 2001;11:443–6. doi: 10.1046/j.1365-3148.2001.00336.x. [DOI] [PubMed] [Google Scholar]
- 8.Vos GH. The evaluation of specific anti-G (CD) eluate obtained by a double absorption and elution procedure. Vox Sang. 1960;5:472–8. doi: 10.1111/j.1423-0410.1960.tb05226.x. [DOI] [PubMed] [Google Scholar]