Abstract
Objectives
The aim of this study was to determine the prevalence of apical periodontitis (AP) detected in cone beam CT (CBCT) images from a database.
Methods
CBCT images of 300 Brazilian patients were assessed. AP images were measured in three dimensions. Age, gender, number and location of total teeth in each patient were considered. AP location was considered according to tooth groups. The extent of AP was determined by the largest diameter in any of the three dimensions. Percentages and the χ2 test were used for statistical analysis.
Results
AP was found in 51.4% of the patients and in 3.4% of the teeth. Higher prevalence of AP was found in 60- to 69-year-olds (73.1%) and in mandibular molars (5.9%) (p < 0.05). Inadequate endodontic treatment presented higher prevalence of AP (78.1%).
Conclusions
AP can be frequently found in CBCT examinations. The presence of AP has a significant association with patients' age, and tooth type and condition. CBCT databases are useful for cross-sectional studies about AP prevalence in a population.
Keywords: cone beam computed tomography, apical periodontitis, cross-sectional studies, epidemiology
Introduction
Apical periodontitis (AP) is a consequence of pulp necrosis caused by micro-organisms within the root canal system.1,2 Chronic inflammation of the periapical tissues frequently develops without the patient experiencing symptoms, and, therefore, examination of images is still fundamental for its detection.3 Panoramic and periapical radiographs are widely used for diagnosis, treatment and follow-up of AP. However, they are two-dimensional (2D) projections of a three-dimensional structure (3D).3-5 There is a lack of information in the buccolingual plane and superimposition of structures. According to previous studies, AP can only be detected in radiographs when the cortical bone is affected by mineral loss.6 AP is generally underestimated and sometimes not detectable in 2D images.7,8
Cone beam CT (CBCT) is a modern technology that is being widely applied in dental practice and research. The possibility of a (3D) view of maxillofacial structures with no superimposition of anatomical landmarks is its main advantage. Many authors have shown that CBCT images are more accurate than 2D dental radiographs for detection of AP3,7,8 since they allow the evaluation of the periapical region through sagittal, coronal and axial sections. Also, AP extension and the size, location and spatial relationship with adjacent structures are properly assessed in CBCT images.7,9 CBCT examination generates radiation exposure to the patient, which is higher than conventional panoramic or periapical radiographs, and lower than medical CT scans.10 The limitations of 2D radiographs and the higher radiation dose of medical CT scanners should be considered in order to respect the ALARA (as low as reasonably achievable) principle and avoid unnecessary radiation exposure without clinical need or benefit. CBCT is a diagnostic tool to be considered for the assessment of AP since its benefits justify the radiation exposure risks.
Nowadays there are many CBCT scanners available on the market. The main differences between them concern field of view (FOV), voxel size and, consequently, image quality and radiation dose.11 Limited FOV scanners acquire volumetric images from a small region (40–80 mm FOV). Medium and large FOV scanners can acquire the entire volume of a single jaw, or both the maxilla and the mandible, and even the full craniofacial region. The advantage of using databases from medium and large FOV CBCT scanners for epidemiological purposes is that the information can be used to assess several oral pathologies that affect the maxillofacial region. This could be difficult to perform using limited FOV databases because multiple exposures are necessary in order to obtain full jaw images.
Several epidemiological studies concerning AP in different populations around the world have been performed using panoramic and/or periapical radiographs. This study was carried out because of the limitations of these radiographic images for the assessment of AP prevalence and features, and the necessity of a new study using CBCT images for epidemiological purposes. Therefore, the aim of the present study was to determine the prevalence of AP in Brazilian subjects and to classify the found AP into patients' age and gender, location and size of AP, and cortical bone and related tooth condition using CBCT images from a database of a large FOV CBCT scanner.
Material and methods
Sample selection
The sample consisted of CBCT images of the maxillofacial region from databases of 300 patients: 280 from a dental school and 20 from a private radiology clinic, both located in Bauru urban area in São Paulo, Brazil. Examinations from patients under 12 years old and from edentulous patients were excluded. In order to be included in the sample, the jaw should present with at least one non-retained tooth. Examinations were obtained using the Classic i-CAT scanner (Imaging Sciences International, Hatfield, PA) with 6, 8 or 13 cm FOV, and 0.25 or 0.3 voxel protocols. Depending on the FOV size, it was possible to visualize the maxilla, the mandible or both. No patient underwent a CBCT scan exclusively for this study. The CBCT scans had been performed for endodontic, periodontal, stomatological, dental implant placement, surgical or orthodontic purposes. The Ethics in Research Committee of the dental school approved this research (082/2009).
Analysis of CBCT examinations
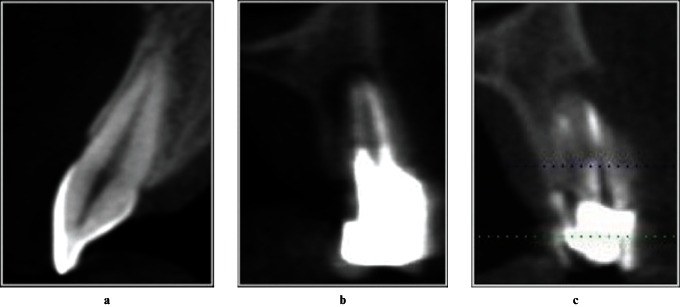
Images were analysed by using the i-CAT Vision software (Imaging Sciences International) installed in a computer running Microsoft Windows XP (Microsoft Corporation, Redmond, WA) with a FlexScan S2000 EIZO (Eizo Nanao Corporation, Ishiwaka, Japan) 20 inch monitor with 1600×1200 pixel resolution, by two calibrated observers, a dentomaxillofacial radiologist and an endodontist. First, the age and gender of each patient was recorded and the purpose of the CBCT scan, by viewing this information in the “preview screen” of the software. The total number of teeth in each jaw was recorded using the panoramic reconstruction. In “implant screen”, each tooth was individually analysed through 0.25 mm or 0.3 mm thickness and step transversal sections. For better visualization, the “sharpen mild” filter and 5×2 display format were used. Figure 1 illustrates the criteria used for determining the absence or presence of AP.
Figure 1.
Illustrative images of the criteria for presence of apical periodontitis (AP) in cone beam CT transversal slices. (a) Healthy tooth with no pathological periapical changes. No hypodense image is observed and the cortical bone is intact. (b) Root-filled tooth with hypodense image of AP between the root limit and periapical bone. (C) Root-filled tooth with hypodense image of AP with buccal cortical destruction
The second part of the work consisted of evaluating different aspects of the found AP. Each AP was evaluated in the “implant screen” and “multiplanar reformatted screen” of the software. The location of AP was determined according to tooth groups (maxillary incisors and canines, maxillary premolars, maxillary molars, mandibular incisors and canines, mandibular premolars, mandibular molars). The extent of AP was established by the largest diameter (mm) in any of the three dimensions (sagittal, coronal, and axial) using the software “measurement tool”, according to the CBCT periapical index (CBCT-PAI).12 AP involvement of the cortical bone was also assessed and classified into no involvement, destruction or expansion of the cortical bone. The AP-related tooth condition was based on the following categories: healthy, remaining root (including filled teeth without coronal restoration), restored teeth with no root filling (RF), adequate RF and inadequate RF (underfilled and overfilled). Adequate RF was considered as a root canal space completely filled, with no voids, and ending 1–2 mm from the apex. Inadequate RF presented root canal space with voids, RF poorly condensed, and RF ending more than 2 mm from the apex (underfilled) or beyond the limit of the apex (overfilled). In multirooted teeth, the worst condition of RF in any of the roots was considered.
Statistical analysis
The results were described as percentages. The χ2 test was applied for the association between variables and significant level was established at 5% (p < 0.05). The interobserver agreement was assessed by kappa statistics. For the verification of AP prevalence in patients we only considered CBCT examinations in which both maxilla and mandible or a single jaw with lesion were visible (n = 214). For the verification of AP prevalence in teeth, we also considered CBCT examinations in which only one jaw with no lesion was visible (n = 300).
Results
A total of 5585 teeth of 300 patients were evaluated. From the total of 214 patients who presented a single jaw with a lesion or both the maxilla and the mandible visible in CBCT examinations, 90 were males and 124 were females (41.5±16.8 years old). AP was detected in 110 patients (51.4%) and in 192 teeth (3.4%). Concerning age, patients under 30 years old presented lower AP prevalence and 60- to 69-year-olds had higher AP prevalence (Table 1, p < 0.05). AP was detected in men and women in a similar way, and the difference is not statistically significant (54.4% and 49.2%, respectively, p > 0.05). The majority of CBCT scans performed for endodontic purposes presented with AP (Table 2).
Table 1. Prevalence of apical periodontitis according to age groups.
| Age group (years) | All patients (n) | Patients with apical periodontitis (n) | Apical periodontitis prevalence (%) |
| 12–19 | 20 | 3 | 15 |
| 20–29 | 46 | 18 | 39.1 |
| 30–39 | 40 | 22 | 55 |
| 40–49 | 28 | 18 | 64.3 |
| 50–59 | 47 | 25 | 53.2 |
| 60–69 | 26 | 19 | 73.1 |
| 70+ | 7 | 5 | 71.4 |
| Total | 214 | 110 | 51.4 |
Table 2. Prevalence of apical periodontitis according to purpose of the cone beam CT scan.
| Purpose | All patients (n) | Patients with apical periodontitis (n) | Apical periodontitis prevalence (%) |
| Endodontics | 38 | 34 | 89.5 |
| Periodontology | 9 | 5 | 55.5 |
| Stomatology | 71 | 41 | 57.7 |
| Implants | 43 | 20 | 46.5 |
| Oral Surgery | 39 | 9 | 23.1 |
| Orthodontics | 14 | 1 | 7.1 |
| Total | 214 | 110 | 51.4 |
192 AP lesions were found. The most frequent location of AP was in mandibular molars (5.9%), followed by maxillary premolars (5.6%) and maxillary incisors and canines (4.6%). AP was less frequently located in mandibular incisors and canines (0.6%) (Table 3, p < 0.05). AP affected the maxilla more frequently than the mandible (4.1% and 2.6%, respectively, p < 0.05). Considering AP extension, most of the lesions were 4–8 mm in diameter (Table 4, kappa = 0.79). The involvement of periapical cortical bone was absent in 76.2% of AP, whereas 17.7% showed cortical destruction and 5.7% showed cortical expansion (kappa = 0.96). Concerning the tooth conditions, AP was more frequently found in endodontically treated teeth with inadequate RF. The prevalence of AP was 78.1% in underfilled teeth and 57.1% in overfilled teeth (Table 5, p < 0.05, kappa = 0.85). The prevalence of endodontically treated teeth in the present study was 415 (7.43% of the sample), of which 298 (71.8%) had adequate RF, 110 (26.5%) were underfilled and 7 (1.7%) were overfilled.
Table 3. Prevalence of apical periodontitis according to tooth groups.
| Tooth groups | All teeth (n) | Teeth with apical periodontitis (n) | Apical periodontitis prevalence (%) |
| Maxillary incisors + canines | 1246 | 58 | 4.6 |
| Mandibular incisors + canines | 1251 | 8 | 0.6 |
| Maxillary premolars | 754 | 42 | 5.6 |
| Mandibular premolars | 716 | 20 | 2.8 |
| Maxillary molars | 908 | 22 | 2.4 |
| Mandibular molars | 710 | 42 | 5.9 |
| Total | 5585 | 192 | 3.4 |
Table 4. Extension of found apical periodontitis according to the CBCT-PAI12.
| Extent of (CBCT-PAI) (mm) | n | Apical periodontitis prevalence (%) |
| 1 (>0.5–1) | 41 | 21.3 |
| 2 (>1–2) | 34 | 17.7 |
| 3 (>2–4) | 35 | 18.2 |
| 4 (>4–8) | 59 | 30.7 |
| 5 (>8) | 23 | 11.9 |
| Total | 192 | 100 |
CBCT–PAI, cone beam CT–periapical index
Table 5. Distribution of apical periodontitis according to related tooth condition.
| Condition | All teeth (n) | Teeth with apical periodontitis (n) | Apical periodontitis prevalence (%) |
| Healthy | 3419 | 6 | 0.2 |
| Remaining root | 62 | 19 | 30.7 |
| Restored with no root filling | 1689 | 20 | 1.2 |
| Restored with adequate root filling | 298 | 57 | 19.1 |
| Restored with inadequate root filling (underfilled) | 110 | 86 | 78.1 |
| Restored with inadequate root filling (overfilled) | 7 | 4 | 57.1 |
| Total | 5585 | 192 | 3.4 |
Discussion
This study is the first cross-sectional assessment of AP prevalence using CBCT images of Brazilian subjects. The literature shows that CBCT images are superior for the detection of AP than conventional radiographs.3,7,8,12,13 Also, kappa values of interobserver reliability show excellent agreement, which demonstrates that CBCT is a useful tool for cross-section studies about AP prevalence. In this study, we used CBCT images only. The majority of the authors used panoramic14-18 or full-mouth periapical radiographs17,19-24 in their epidemiologic studies. In our research, we excluded 86 CBCT examinations in which the maxilla or mandible were isolated due to the scanning protocol (smaller FOV) and did not present AP for the determination of AP prevalence in patients. This procedure was necessary considering that these examinations did not provide information about the opposite jaw, which could also present with AP. Therefore, for the observation of AP prevalence in patients, it is recommended to have images of both the maxilla and the mandible, as in panoramic or full-mouth periapical radiographs. However, for the assessment of AP prevalence in teeth, it is possible to include isolated jaws, since the total number of teeth is known.
The prevalence of AP in patients and teeth found in this study was lower than in most epidemiological studies that used periapical or panoramic radiographs from different countries. This may be because of the age of the assessed patients, the sample of patients and the method of assessment.
In our study, the minimum age was 12 years old, and the average was 41.5±16.8 years old. Other studies concerning the prevalence of AP and root canal treatment usually include patients aged 15 years or more,15 16 years or more,21,25 18 years or more14,18-20,24 or 20 years or more.17,22 We decided to include teenagers since information about the condition of their teeth is important. AP was more prevalent in the group aged over 30 years . This result confirmed that AP prevalence increases with age, which is in accordance with the literature.18,22
The sample of patients is another important factor for the results of this study. The majority of authors in the literature selected patients who came to their dental schools or offices for the first time.15,19,20,24,25 Panoramic radiographs or/and full-mouth periapical radiographs are the correct choice for a preliminary image examination of a patient who comes for the first time and usually needs primary dental treatment. However, a CBCT scan is not a simple and routine examination, since it exposes the patient to higher radiation. In our study, the patients underwent CBCT scan because their referral professional needed further information for a specific purpose. Therefore, the patients were already under treatment in our university and not being seen for the first time, which could reflect a general better oral condition at the time of the scanning than those patients not under treatment. On the other hand, we also observed that a percentage of CBCT scans performed for periodontal, surgical or dental implant placement purposes presented AP in their images (55.5%, 23.1%, 46.5%, respectively).
Men and women presented similar AP prevalence and the difference was not statistically significant, which means that AP is not dependent on gender, confirming what has been previously reported.17-19,21,24,25 Concerning AP location, posterior teeth presented significantly higher prevalence, and the maxilla was affected more than the mandible (4.1% and 2.6%, respectively, p < 0.05). This fact can be related to the complex anatomy of these teeth,25 which contributes to a higher risk of dental caries due to plaque accumulation, and also difficulty in proper cleaning, shaping and filling during root canal treatment.
Considering AP extension and cortical bone condition, we observed that the majority of the lesions were 4–8 mm in size (CBCT-PAI score 3) followed by 0.5–1 mm (CBCT-PAI score 1). An important observation of this study is that periapical cortical bone was not affected in 76.2% of the cases. Only 5.7% of AP presented cortical destruction. According to previous studies, AP can only be detected in radiographs when the cortical bone is affected by mineral loss.6 Therefore, we can suggest that many incidences of AP that were identified in this study would be missed in conventional radiographic assessment. Also, the condition of periapical cortical bone can be properly assessed only through CBCT slices, since the transversal plane is not visible in 2D images.
Concerning the AP-related condition of the teeth, we observed that inadequate RF teeth presented higher AP prevalence (78.1% underfilled and 57.1% overfilled, p < 0.05). It is known that root canal treatment involves proper cleaning, shaping and filling procedures, and it is not possible to judge the quality of treatment using images. This is a limitation of cross-sectional studies that use radiographic images, since information regarding biological factors and conditions of clinical treatment are unknown.4,21 However, our results are in accordance with other studies and confirm that teeth with inadequate RF present a higher risk of AP occurrence or maintenance, since bacteria can remain within the root canal system in filled teeth.2 It is interesting to observe that our study sample presented a low prevalence of endodontically treated teeth (7.43%) and high prevalence of adequate RF (71.8%), which may contribute to a lower prevalence of AP than in other epidemiologic studies. However, the sample of teeth is not independent, and clusters, such as teeth from the same patient, that may have been treated by the same dentist are not considered by the statistical analysis chosen for epidemiologic studies. These facts can limit the extrapolation of the results, particularly concerning the prevalence of AP related to treated-tooth condition. On the other hand, this clustering in the sample does not impair the conclusion about AP prevalence in this subpopulation.
Clinical examination and intraoral radiographs are better methods to evaluate the marginal quality of coronal restorations.5 However, restored teeth were considered in this study and some interesting data were found. The presence of restored teeth without endodontic treatment showed AP prevalence of 1.2%, which is low. Adequate RF in restored teeth showed AP prevalence of 19%. In contrast, inadequate RF in the presence of a restoration showed a prevalence of 78.1%. Although the design of the study does not allow conclusions about the influence of the quality of the coronal restoration to be reached, AP was more prevalent when an inadequate RF was present. It was not possible to reach a conclusion about overfilling cases due to the low incidence (seven cases).
According to Tsuneishi et al,22 AP prevalence depends on the patient's age, tooth type and quality of root canal treatment, which was confirmed by the present study. It is important to highlight that our findings do not represent a random sample of the Brazilian population, which is a country of continental dimensions. However, it provides useful information about AP prevalence and illustrates general dental condition in a subpopulation, which can help to define new strategies for treatment and prevention of periapical disease. Furthermore, this study contributes to future applications of CBCT images in epidemiological studies.
It can be concluded that AP prevalence in our study is lower than in the epidemiological studies. Also, older patients, and teeth with complex anatomy and inadequate endodontic treatment are more likely to present AP.
Acknowledgments
The authors thank Dr Silvio Garcia Meira Junior from the “Imagem Diagnósticos Médicos” and Prof. Luis Casati Alvares and Dr Roberta Heiffig Handem for helping in recording DICOM data.
Footnotes
This study was supported by CAPES.
References
- 1.Abbott PV. Classification, diagnosis and clinical manifestations of apical periodontitis. Endod Topics 2004;8:36–54. [Google Scholar]
- 2.Nair PNR. Pathogenesis of apical periodontitis and the causes of endodontic failures. Crit Rev Oral Biol Med 2004;15:348–381. [DOI] [PubMed] [Google Scholar]
- 3.Lofthag-Hansen S, Huumonen S, Grondahl K, Grondahl HG. Limited cone-beam CT and intraoral radiography for the diagnosis of periapical pathology. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2007;103:114–119. [DOI] [PubMed] [Google Scholar]
- 4.Huumonen S, Orstavik D. Radiological aspects of apical periodontitis. Endod Topics 2002;1:3–25. [Google Scholar]
- 5.Tyndall DA, Rathore S. Cone-beam CT diagnostic applications: caries, periodontal bone assessment, and endodontic applications. Dent Clin North Am 2008;52:825–841. [DOI] [PubMed] [Google Scholar]
- 6.Bender IB. Factors influencing the radiographic appearance of bony lesions. J Endod 1982;8:161–170. [DOI] [PubMed] [Google Scholar]
- 7.Estrela C, Bueno MR, Leles CR, Azevedo B, Azevedo JR. Accuracy of cone beam computed tomography and panoramic and periapical radiography for detection of apical periodontitis. J Endod 2008;34:273–279. [DOI] [PubMed] [Google Scholar]
- 8.Ordinola-Zapata R, Bramante CM, Duarte MH, Fernandes LMPSR, Camargo EJ, de Moraes IG, et al. The influence of cone-beam computed tomography and periapical radiographic evaluation on the assessment of periapical bone destruction in dog's teeth. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011;112:272–279. [DOI] [PubMed] [Google Scholar]
- 9.Tanomaru M, Lima RKP, Nakazone PA, Tanomaru JMG. Use of computerized tomography for diagnosis and follow-up after endodontic surgery: clinical case report with 8 years of follow-up. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2010;109:629–633. [DOI] [PubMed] [Google Scholar]
- 10.Ludlow JB, Davies-Ludlow LE, Brooks SL, Howerton WB. Dosimetry of 3 CBCT devices for oral and maxillofacial radiology: CB Mercuray, NewTom 3G and i-CAT. Dentomaxillofac Rad 2006;35:219–226. [DOI] [PubMed] [Google Scholar]
- 11.Loubele M, Jacobs R, Maes F, Denis K, White S, Coudyzer W, et al. Image quality vs radiation dose of four cone beam computed tomography scanners. Dentomaxillofac Rad 2008;37:309–318. [DOI] [PubMed] [Google Scholar]
- 12.Estrela C, Bueno MR, Azevedo BC, Azevedo JR, Pecora JD. A new periapical index based on cone beam computed tomography. J Endod 2008;34:1325–1331. [DOI] [PubMed] [Google Scholar]
- 13.de Paula-Silva FWG, Wu MK, Leonardo MR, da Silva LAB, Wesselink PR. Accuracy of periapical radiography and cone-beam computed tomography scans in diagnosing apical periodontitis using histopathological findings as a gold standard. J Endod 2009;35:1009–1012. [DOI] [PubMed] [Google Scholar]
- 14.De Moor RJ, Hommez GM, De Boever JG, Delme KI, Martens GE. Periapical health related to the quality of root canal treatment in a Belgian population. Int Endod J 2000;33:113–120. [DOI] [PubMed] [Google Scholar]
- 15.Kabak Y, Abbott PV. Prevalence of apical periodontitis and the quality of endodontic treatment in an adult Belarusian population. Int Endod J 2005;38:238–245. [DOI] [PubMed] [Google Scholar]
- 16.Loftus JJ, Keating AP, McCartan BE. Periapical status and quality of endodontic treatment in an adult Irish population. Int Endod J 2005;38:81–86. [DOI] [PubMed] [Google Scholar]
- 17.Tercas AG, de Oliveira AE, Lopes FF, Maia Filho EM. Radiographic study of the prevalence of apical periodontitis and endodontic treatment in the adult population of Sao Luis, MA, Brazil. J Appl Oral Sci 2006;14:183–187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Peters LB, Lindeboom JA, Elst ME, Wesselink PR. Prevalence of apical periodontitis relative to endodontic treatment in an adult Dutch population: a repeated cross-sectional study. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011;111:523–528. [DOI] [PubMed] [Google Scholar]
- 19.Boucher Y, Matossian L, Rilliard F, Machtou P. Radiographic evaluation of the prevalence and technical quality of root canal treatment in a French subpopulation. Int Endod J 2002;35:229–238. [DOI] [PubMed] [Google Scholar]
- 20.Jimenez-Pinzon A, Segura-Egea JJ, Poyato-Ferrera M, Velasco-Ortega E, Rios-Santos JV. Prevalence of apical periodontitis and frequency of root-filled teeth in an adult Spanish population. Int Endod J 2004;37:167–173. [DOI] [PubMed] [Google Scholar]
- 21.Georgopoulou MK, Spanaki-Voreadi AP, Pantazis N, Kontakiotis EG. Frequency and distribution of root filled teeth and apical periodontitis in a Greek population. Int Endod J 2005;38:105–111. [DOI] [PubMed] [Google Scholar]
- 22.Tsuneishi M, Yamamoto T, Yamanaka R, Tamaki N, Sakamoto T, Tsuji K, et al. Radiographic evaluation of periapical status and prevalence of endodontic treatment in an adult Japanese population. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2005;100:631–635. [DOI] [PubMed] [Google Scholar]
- 23.Eckerbom M, Flygare L, Magnusson T. A 20-year follow-up study of endodontic variables and apical status in a Swedish population. Int Endod J 2007;40:940–948. [DOI] [PubMed] [Google Scholar]
- 24.Toure B, Kane AW, Sarr M, Ngom CT, Boucher Y. Prevalence and technical quality of root fillings in Dakar, Senegal. Int Endod J 2008;41:41–49. [DOI] [PubMed] [Google Scholar]
- 25.Al-Omari MA, Hazaa A, Haddad F. Frequency and distribution of root filled teeth and apical periodontitis in a Jordanian subpopulation. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2011;111:e59–e65. [DOI] [PubMed] [Google Scholar]