Abstract
Purpose
To assess and compare the recurrence rate of pterygium after limbal stem cell transplantation versus amniotic membrane transplantation (AMT) as ocular surface reconstructing measures in recurrent pterygium, also evaluation of the use of antimetabolite drugs as adjunctive therapy for AMT.
Patients and methods
Prospective randomized comparative study included 60 eyes of 48 patients with recurrent pterygia. Informed consents were taken from all patients.
Primary pterygium excision was performed 6–15 months ago; the cases were divided randomly into three equal groups:
Group 1: included 20 eyes with excision of the pterygium and application of limbal stem cell transplantation with conjunctival autograft, group 2: included 20 eyes with excision of the pterygium followed by AMT and group 3: included 20 eyes in which surgical excision of pterygium was followed by intra-operative application of low-dose of MMC (0.05%) for 3 min then using AMT.
Results
The study included 36 males and 12 females of age ranged from 28 to 52 years. The recurrence rate was 2 eyes in group 1 (10%) (limbal stem cell transplantation + conjunctival autograft), 6 eyes in group 2 (30%) (AMT) and 4 eyes (20%) in group 3 (MMC + AMT). The rate of recurrence was significantly different between the three groups (P < 0.001).
Conclusions
Limbal stem cell transplantation together with conjunctival autografting proved to be more effective in prevention of pterygium recurrence and in rapid restoration of normal epithelial morphology. MMC in addition to AMT decreases the incidence of recurrence.
Abbreviations: AMT, amniotic membrane transplantation; MMC, mitomycin C
Keywords: Recurrent pterygium, Stem cells autograft, Amniotic membrane transplantation, Mitomycin C, Ocular surface diseases, Impression cytology
1. Introduction
Pterygium is a common worldwide eye disease affecting population especially in tropical and subtropical areas. Recurrence of pterygium is the most common complication after pterygium excision and recurrent pterygium represents a significant surgical problem (Yaisawang and Piyapattanakrn, 2003). Several techniques have been tried to reduce the fibro vascular activity aiming to reduce rate of recurrence such as B-irradiation, conjunctival and limbal auto-grafting, anti-mitotic drugs and amniotic membrane transplantation (AMT) (Kawasaki et al., 2003).
Limbal auto-grafts have been used successfully to correct limbal dysfunction, acting as a barrier against conjunctival invasion of the cornea and supplying stem cells of the corneal epithelium. Limbal graft can be obtained preferably from the unaffected eye to decrease the incidence of limbal stem cell deficiency (Shimazaki et al., 1996).
The anti-fibrotic effect of anti-metabolites as mitomycin C (MMC) and 5-fluorouracil made them useful tools to be used during surgical excision of pterygium. Concentration of these drugs should be properly adjusted to avoid and prevent serious complications as scleral melting, ulceration or delayed epithelization (Mastropasqua et al., 1996).
Amniotic membrane being a basement membrane acts as a new healthy substrate suitable for proper epithelization, it has a strong antiadhesive effect (Xi et al., 2003) being normally avascular thus inhibit the incursion of new vessels (Dua and Azuara Blauco, 1999).
Impression cytology is a simple, new and reproducible technique which is successful at both removing cell and preserving cytological features of the epithelium, demonstrating any morphological changes and indicating the grade of the dryness (Tseng et al., 1997).
The aim of the current study was to assess and compare the recurrence rate of pterygium after AMT versus limbal stem cell transplantation as ocular surface reconstructing measures in recurrent pterygium, also evaluation of the use of antimetabolite drugs as adjunctive therapy.
2. Patient and methods
The prospective randomized comparative study included 60 eyes of 48 patients with recurrent pterygia.
Primary pterygium excision was performed 6–15 months before selection in our study. Informed consents were taken from all patients. Demographic data are shown in Table 1.
Table 1.
Demographic data among the three groups.
| Group 1 (20 eyes) | Group 2 (20 eyes) | Group 3 (20 eyes) | |
|---|---|---|---|
| 1. Sex | |||
| Male | 16 | 18 | 14 |
| Female | 4 | 2 | 6 |
| 2. Age | |||
| Mean ± SD | 45.2 ± 7.3 | 49.1 ± 2.3 | 39.1 ± 13.1 |
| Range | 30–50 | 29–52 | 30–52 |
| 3. Laterality | |||
| Right | 18 | 14 | 12 |
| Left eye | 2 | 6 | 8 |
Exclusion criteria included dry eye syndrome or wound healing problems as ocular cicatricial pemphigoid, immunocompromised patients or use of immunosuppressive drugs, or follow-up less than 6 months postoperatively. For pterygium excision all eyes were operated upon under local anesthesia using a combination of subconjunctival 2 cc of 4%.
Xylocaine and topical Benoxinate Hydrochloride 0.4% eye drops were used as surface anesthesia; a microsponge impregnated with Benoxinate was also applied directly to the pterygium for 2 min for efficient topical anesthesia.
The head of pterygium was shaved from the cornea using 45° super blade then its body was dissected and reflected towards the canthus then excised, and subconjunctival fibrosis was also excised. The cases were divided randomly into three equal groups:
Group 1: included 20 eyes with excision of the pterygium and application of limbal autograft, the conjunctival tissue was taken from upper temporal bulbar conjunctiva 3 mm from the limbus of the affected eye about 3–5 mm in width excluding Tenon’s capsule. The donner site was closed by 10/0 silk sutures. The graft was sutured to the bare sclera with interrupted 10/0 silk sutures.
The globe was rotated infero-medially to expose the supero-temporal conjunctiva. Dimensions were marked with cautery. Free grafts were dissected as thin as possible, taking minimal subconjunctival tissue. The graft was excised such that the cautery marks remained to identify the epithelial surface when the graft was repositioned (Fig. 1, top).
Figure 1.

Top (patient of group 1) – top left: recurrent pterygium and top right: 6 months after limbal autograft. Bottom (patient of group 3) – AMT + MMC after pterygium excision.
Group 2: included 20 eyes with excision of the pterygium followed by AMT. Amniotic membrane was obtained at the time of caesarean section from mothers’ sero-negative for hepatitis B, C and HIV viruses. The membrane was washed several times with physiological saline containing garamycin at a concentration of 3.2/100 ml under complete sterile conditions. The membrane was fashioned into pieces of similar size and shape of the bared scleral area. The amniotic membrane was secured with its basement membrane side up through episcleral tissue to the conjunctiva along the bare scleral border using 10/0 silk sutures (Fig. 2).
Figure 2.
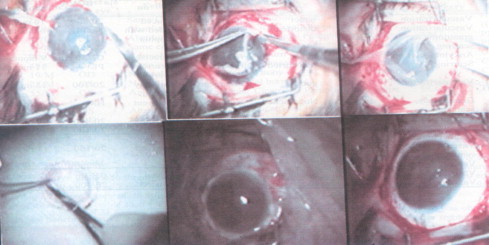
Steps of AMT (patient of group 2).
Group 3: included 20 eyes in which surgical excision of pterygium was followed by intra-operative application of low-dose of MMC (0.05%) for 3 min then using AMT (Fig. 1, bottom).
MMC was prepared in a concentration of 0.05% being diluted by lactated Ringer’s solution. A piece of sponge soaked with MMC was applied to the bare sclera for 3 min. Extensive washing followed using Lactated Ringer’s solution to remove the traces of the drug. The bare sclera was then covered with the AMT using 10/0 silk sutures.
Postoperatively a pressure patch was applied for 24 h and a combination of antibiotic and steroid drops (Tobradex) was used 4 times daily for 2 weeks. Cases were followed-up regarding inflammatory response, healing pattern and recurrence of pterygium as well as complications for 2 years. Recurrence was considered when fibro vascular tissue regrowth over the cornea clinically (Fig. 3, top left).
Figure 3.
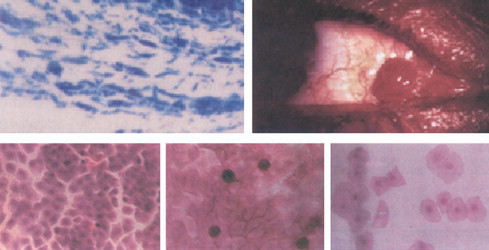
Top left: Cytological changes of recurrence; top right: conjunctival granuloma. Down left: Stage II squamous metaplasia; down middle: stage I squamous metaplasia; down right: stage III squamous metaplasia.
Postoperative examination included full ophthalmic evaluation with slit-lamp examination, fluorescein corneal staining, IOP measurement and recording of any complication. The main outcome measures were the recurrence rate and the postoperative complications. Sutures were removed at 3rd week.
Impression cytology was done to all cases in 3rd day postoperatively, using cellulose acetate filter paper with 0.025 μm pore size to allow more pick of epithelial sheets of cells. This was done periodically till the sixth month postoperatively for evaluation of healing and recurrence.
The filter paper was cut into triangular strips, when applied to the eye the apex is towards the corneal side and the base is towards the conjunctival part of the operated surface.
The sample was preserved in ethanol 70% until laboratory examination.
The samples were stained Haematoxylin & Eosin, Papanicolaou stain and Periodic acid Schiff then fixed with Xylene to be examined on a slide with light microscopy regarding the progression of wound healing and acceptance of amniotic membrane graft.
Complete healing was considered when impression cytology showed complete cytological healing with normal nuclear/cytoplasmic ratio 1:1, normal density of epithelial cells, cell size and nuclear size and clinically with negative fluorescein staining (Tseng et al., 1997).
Data were extracted and transposed onto a data sheet, which was entered into a computer programmed with the SPSS 17/PC Software Package (SPSS Inc., Chicago, IL, USA) until data of 60 eyes in 48 patients had been accumulated. Record was made of each patient’s name, age, hospital number, and globe axial length, type of management and duration of previous surgery, recurrence and follows up. Demographic data, recurrence and other complications were compared using analysis of variance, P < 0.05 was regarded as significant and highly significant if P < 0.001.
3. Results
-
•
The prospective randomized comparative study included 60 eyes of 48 patients with recurrent pterygia. They were 36 males and 12 females whose age ranged between 28–52 years (mean 45.2 ± 3.7 years). During follow-up period, the recurrence rate was 2 eyes in group 1 (10%) (limbal stem cell transplantation + conjunctival autograft), 6 eyes in group 2 (30%) (AMT) and 4 eyes (20%) in group 3 (MMC + AMT). The rate of recurrence was significantly different between the three groups (P < 0.001), and it was statistically significant better with limbal stem cell transplantation with conjunctival autograft in group 1 (Fig. 4).
-
•
Conjunctival irritation was significant in cases where MMC was used. No cases of scleral thinning or necrosis was recorded; 4 eyes showed transient superficial keratitis in group 3 that had delayed healing without residual complications; conjunctival granuloma (Fig. 3, top right) was recorded in 4 eyes in group 2 (AMT) (Table 2).
-
•
The difference in progression of healing process between the three groups was significantly different (P < 0.001).
-
•
The duration of complete epithelial healing (cytologically) was 40 days in group 1, 6 months in group 2, and 10 months in group 3 as shown by impression cytology.
-
•
In group 1, impression cytology revealed the presence of granulation tissue reaction, epithelial intracellular edema (as empty spaces inside the cells), mononuclear inflammatory cells and fibroblasts were predominant. Stage II squamous metaplasia (absent goblet cells in the conjunctiva, enlargement of epithelial cells with nuclear/cytoplasmic ratio 1:4) was the predominant stage in this group (Fig. 3, bottom left).
-
•
While in group 2, impression cytology showed few inflammatory cells with minimal fibroblasts and stage I squamous metaplasia was the predominant (Fig. 3, bottom middle).
-
•
In group 3, impression cytology showed no evidence of fibroblast with predominance of stage III squamous metaplasia (Fig. 3, bottom right).
Figure 4.
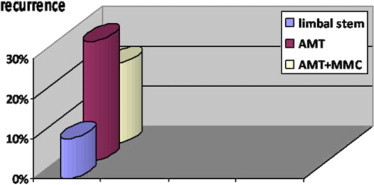
Graph showing comparison of the recurrence incidence in the three groups. Showing highest recurrence with AMT and least recurrence with limbal stem cell transplantation.
Table 2.
Postoperative complications.
| Complications | Group 1 | Group 2 | Group 3 |
|---|---|---|---|
| 1. Recurrence rate | 2 eyes (10%) | 6 eyes (30%) | 4 eyes (20%) |
| 2. Conjunctival irritation | 14 eyes (70%) | ||
| 3. Chemosis | 4 eyes (20%) | 2 eyes (10% | 6 eyes (30%) |
| 4. Transient ++ IOP | 2 eyes (10%) | 2 eyes (10%) | |
| 5. Conjunctival granuloma | 4 eyes (20%) | ||
| 6. Transient superficial keratitis | 4 eyes (20%) |
4. Discussion
Pterygium is a common worldwide external eye disease affecting populations especially in tropical and subtropical areas. It is believed that surgical trauma and subsequent postoperative inflammation activate proliferation of subconjunctival fibroblasts and vascular cells, and deposition of proteins in turn contributes to the pterygium recurrence (Ma et al., 2000).
Simple excision of primary pterygia is associated with a high recurrence rate (33–45%). Removal of recurrent pterygium is more difficult due to corneal thinning, Symblepharon, and extension of the scar tissue to recti muscles (Shimazaki et al., 2003).
The aim of this study was to evaluate different methods of ocular surface reconstruction in recurrent pterygium as regarding rate of epithelial healing and incidence of recurrence.
Our study included 48 patients (60 eyes) with recurrent pterygium, who were divided into three groups. The first group was subjected to limbal autograft and conjunctival transplantation; second group underwent AMT while for the last group we used intra-operative MMC (0.05%) and AMT. During follow-up period, the recurrence rate was 2 eyes (10%) in group, 6 eyes (30%) in group 2, and 4 eyes (20%) in group 3. The rate of recurrence was significantly different between the three groups.
It was least recurrent with limbal stem cells autograft in group 1 as it acts as anatomical and physiological barrier against the recurrence while combination of MMC with AMT in group 3 has more beneficial effect in prevention of recurrence than AMT alone in group 2.
Some authors revealed that the recurrence rate for primary closure varies from 5% to 69%, for sliding conjunctival autograft from 3.2% to 10.7% and for free conjunctival autograft it varies from 0% to 39% among different reports (Adams et al., 1990).
Another study reported the recurrence rates of 10.9% and 2.6% following AMT and conjunctival autograft (Prabhasawat et al., 1997). While another two studies reported recurrence rates 9.4%, 8.3% and 3.8%, 5.4% following AMT and conjunctival autograft, respectively (Gamal, 2001).
In our study, impression cytology revealed the prevalence of grade II squamous metaplasia in group 1 with complete cytological healing after 40 days, in group 2 the predominant stage was grade I and healing was completed after 6 months, finally in group 3 showing the prevalence of grade III squamous metaplasia and complete cytological healing after 10 months.
Mutla et al. (1999) reported that the most frequent complication in limbal conjunctival autograft transplantation was graft edema, whereas that in MMC user as adjunctive therapy group was superficial keratitis. In our study chemosis was present in 20% in group 1, 10% in group 2 and 30% in group 3, while transient superficial keratitis was recorded only in four cases in group 3 (using MMC).
Limbal stem cell transplantation together with conjunctival autografting proved to be more effective in prevention of pterygium recurrence and in rapid restoration of normal epithelial morphology. MMC addition to AMT decreases the incidence of recurrence.
Financial support
Fund of Ophthalmology Department, Ain Shams University.
No financial interest of authors for any of used materials.
References
- Adams A.P., Starch T., Kenyon K.R. The management of pterygium. Ophthalmol. Clin. North Am. 1990;3:611–623. [Google Scholar]
- Dua H.S., Azuara Blauco A. Amniotic membrane transplantation. Br. J. Ophthalmol. 1999;83:748–752. doi: 10.1136/bjo.83.6.748. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gamal M.A. Comparison of amniotic membrane grafts, conjunctival autograft and intra-operative mitomycin for primary pterygium surgery. Bull. Ophthalmol. Soc. Egypt. 2001;94:69–73. [Google Scholar]
- Kawasaki S., Uno T., Shimamura I., Ohashi Outcome of surgery for recurrent pterygium using intra-operative application of mitomycin C and amniotic membrane transplantation. Jpn. J. Ophthalmol. 2003;47(6):625–626. [PubMed] [Google Scholar]
- Ma D.K., See L., Liau S., Tsai R.J. Amniotic membrane graft for primary pterygium: comparison with conjunctival autograft and topical mitomycin C treatment. Br. J. Ophthalmol. 2000;84:973–978. doi: 10.1136/bjo.84.9.973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mastropasqua L., Carpineto P., Ciancaglini M., Gallenga P.E. Long-term results of intra-operative mitomycin C in the treatment of recurrent pterygium. Br. J. Ophthalmol. 1996;80:288–291. doi: 10.1136/bjo.80.4.288. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mutla F.M., Sobaci G., Tatar T., Yildirim E.A. Comparative study of recurrent pterygium surgery: limbal conjunctival autograft transplantation versus mitomycin C with conjunctival flap. Ophthalmology. 1999;106(4):817–821. doi: 10.1016/S0161-6420(99)90172-0. [DOI] [PubMed] [Google Scholar]
- Prabhasawat P., Barton K., Burkett G., Tseng S.C. Comparison of conjunctival autograft, amniotic membrane grafts and primary closure for pterygium excision. Ophthalmology. 1997;104:974–985. doi: 10.1016/s0161-6420(97)30197-3. [DOI] [PubMed] [Google Scholar]
- Shimazaki J., Yang H.Y., Tsubota K. Limbal autograft transplantation for recurrent and advanced pterygia. Ophthalmic Surg. Lasers. 1996;27:917–923. [PubMed] [Google Scholar]
- Shimazaki J., Kosaka K., Shimmura S., Tuubota K. Amniotic membrane transplantation with conjunctival autograft for recurrent pterygium. Ophthalmology. 2003;110(1):119–124. doi: 10.1016/s0161-6420(02)01453-7. [DOI] [PubMed] [Google Scholar]
- Tseng S.C., Prabhasawat P., Lee S.H. Amniotic membrane transplantation for conjunctival surface reconstruction. Am. J. Ophthalmol. 1997;124:765–774. doi: 10.1016/s0002-9394(14)71693-9. [DOI] [PubMed] [Google Scholar]
- Xi Xh., Jiang D.Y., Tang L.S. Transplantation of amniotic membrane and amniotic membrane combined with limbal autograft for patients with complicated pterygium. Hunan Yi Ke Da Xue Xue Bao. 2003;28(2):149–151. [PubMed] [Google Scholar]
- Yaisawang S., Piyapattanakrn P. Role of postoperative topical corticosteroid in recurrence rate after pterygium excision with conjunctival autograft. J. Med. Assoc. Thai. 2003;86(Suppl. 2):5215–5223. [PubMed] [Google Scholar]


