Abstract
The goal of the treatment of patients with glaucoma is to prevent disability or, if disability already exists, to repair the disability or at the least to prevent further disability from developing. To achieve these goals requires knowing what will happen if there is no treatment and what will happen if there is treatment. That is, one must know the possible benefits from the therapy in comparison to the damage caused by the therapy. As we will demonstrate, the classic risk factors do not provide accurate estimates of the development of disability and do not answer these two questions. The most helpful clues are provided by what the patient says, by whether the disc is damaged and by whether the disc is deteriorating.
The severity of disease is best estimated by the nature of the optic disc and how it changes. This report is primarily focused on increasing the skill of the physician in being able to estimate the nature of the optic disc and how that changes. This does not, however, lessen the tremendous importance of careful history-taking and of gonioscopy. In this report, however, we focus on the evaluation of the disc.
Currently disc evaluation is often not adequate because of poor examination techniques, reliance on cup/disc ratios, and reliance on the results of image analyzers. We will present here the Disc Damage Likelihood Scale, which is a user-friendly method which correlates accurately with visual field changes.
Keywords: Glaucoma, Care, Optic disc, DDLS, Cup/disc ratio
1. Introduction
For many years physicians based the diagnosis and management of glaucoma on the level of intraocular pressure. The initial belief was that pressure above 21 mm Hg was abnormal and below 21 mm Hg was normal (Leydhecker et al., 1958). Consequently, glaucoma diagnosis and treatment were simple: people with pressures over 21 mm Hg had glaucoma and were treated, and people with pressures below 21 mm Hg did not have glaucoma and were not treated. We know now this was simplistic, not simple. Ninety-three percent of people with pressures over 21 mm Hg never develop glaucoma damage, and around one third to one half of those with glaucoma have pressures in the normal range (Sommer et al., 1991).
Unfortunately, there is presently a similarly simplistic way of thinking simplistically about glaucoma, specifically to “just lower the intraocular pressure to or below 12 mm Hg.” This belief is based on an incorrect interpretation of the results of the AGIS study (The Advanced Glaucoma Intervention Study (AGIS), 2000). The AGIS study appeared to show that individuals whose pressures were 12 mm Hg or below for seven years failed to have progressive glaucoma damage, whereas those with pressures around 20 developed three out of 20 units of visual field loss.
However, the study did not actually show that. Fourteen percent of individuals in the study whose intraocular pressures were 12 mm Hg or below got worse faster than the subjects whose pressures were 20 mm Hg. This is an important point, because the simplistic misinterpretation of the results of the AGIS study has resulted in many ophthalmologists working to get all patients with glaucoma to pressures of 12 mm Hg or below. The consequence has been a massive overtreatment of many patients with glaucoma. These overtreatments can result in inconvenience, cost, embarrassment, damage to the surfaces of the eye, loss of vision, infection, systemic abnormalities and even death. No treatment is justified unless it is clear that without the treatment the patient will develop some type of disability.
In the Olmsted County Study, around one-third of the patients went blind (Hattenhauer et al., 1998). In our practice at Wills Eye Institute, less than one-tenth percent go blind (Eid et al., 2003). These are, of course, different populations. However, there is a reasonable chance that at least part of the difference in outcome is related to the method in which care is provided including minimizing overtreatment. By and large, the patients in the Olmsted County Study were treated on the basis of pressure. Our patients are treated on the basis of the history and the evaluation of the disc.
At Wills, the essential aspects of the care of patients with glaucoma, in addition to looking at pressure, include (1) a careful history with sufficient information on estimated life expectancy; (2) assessing the anterior chamber angle accurately enough to know its nature; (3) measuring the intraocular pressure with an applanation tonometer; (4) evaluating the optic disc with careful staging of the amount of damage; and (5) considering psychophysical characteristics, such as visual acuity, visual field and contrast sensitivity.
The goal of treatment at Wills is to prevent disability in patients or, if disability already exists, to repair the disability or at the least to prevent further disability from developing. To achieve these goals requires knowing what will happen if there is no treatment and what will happen if there is treatment. That is, one must know the possible benefits from the therapy in comparison to the damage caused by the therapy. The use of the Glaucoma Graph (Fig. 1) is very helpful in this regard (Spaeth and Paulus, 2010).
Figure 1.
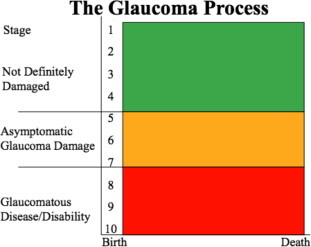
Glaucoma Color Graph. The stage of disease is graded considering the amount of disc damage estimated by DDLS. The optic discs may be graded in three zones: green, yellow or red. In the green zone, which comprises DDLS of 1–4, the patients do not have definite damage. When a patient is in the yellow zone (with a DDLS of 5–7), the optic nerve is definitely damaged, but the person may still be asymptomatic. It is certain that the optic disc is not normal. Finally, when a person is already in the red zone (with a DDLS of 8, 9 or 10), that is, the person already has a disability. The patient may have decreased quality of life or impaired ability to perform the daily activities.
Two important questions are “Who is disabled by glaucoma?” and “Who will become disabled by glaucoma?” As we will demonstrate, the classic risk factors do not provide accurate estimates of the development of disability and do not answer these two questions. The most helpful clues are provided by what the patient says, by whether the disc is damaged, and by whether the disc is deteriorating.
Fig. 2 is a graphic representation of the likelihood that a person will develop visual field loss in association with various risk factors. Note this is not disability but just field loss. The likelihood of developing disability is much lower. Note that even when patients have central corneal thickness less than 550 micra and intraocular pressures above 27 mm Hg, two-thirds of the patients will not develop any visual field loss within seven years (Gordon et al., 2002). On the other hand, if the Disc Damage Likelihood Scale (DDLS) is 5 or greater, 95% of the patients will have worsening of their visual field.
Figure 2.
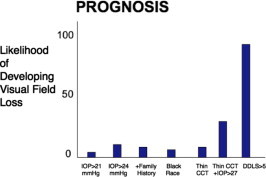
Risks factors and the likelihood of developing visual field loss. CCT = Central corneal thickness; DDLS = Disc Damage Likelihood Scale.
Fig. 3 is an analysis of the AGIS data performed by Joseph Caprioli, in which he found that the major risk factors for the worsening of the visual field were the rate of change of the visual field and the age of the patient (Nouri-Mahdavi et al., 2005). The level of intraocular pressure and the fluctuation of intraocular pressure were not statistically significant in this regard. However, Fig. 4 shows something a little bit different. Fig. 4 illustrates that patients with a rapid rate of field deterioration always have continuing visual field progression. In contrast, age by itself does not predict whether an individual will have progressive glaucoma damage. The oldest patients did not get worse. Even though intraocular pressure was not statistically significant, when the intraocular pressure was markedly elevated, all the patients got worse.
Figure 3.
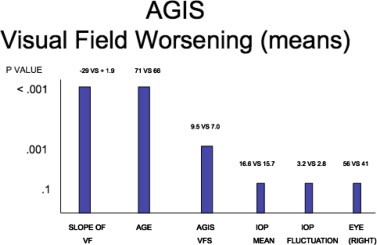
Statistical significance of various characteristics of patients with glaucoma, related to their likelihood of their developing visual field loss as observed in the Advanced Glaucoma Intervention Study (AGIS). The slope of the visual field (VF) refers to the rapidity with which the visual field is worsening in units of visual field loss/years. “AGIS VFS” indicates the amount of visual field loss according to the AGIS system of staging visual fields. IOP mean indicates the mean intraocular pressure in mmHg. IOP fluctuation refers to the fluctuation of intraocular pressure. Eye (right) refers to comparison of the IOP in the right eye versus the left eye. (Histogram created on the basis of data from citation 8.)
Figure 4.
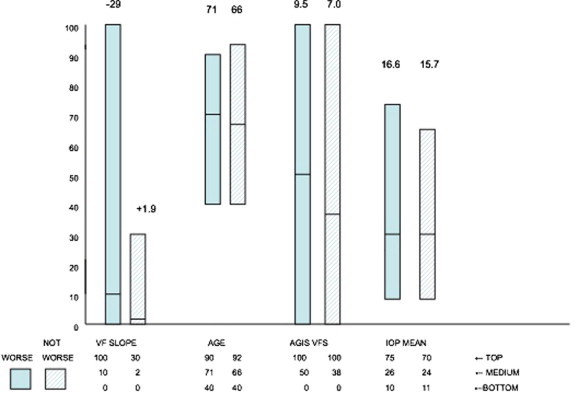
Individual data points from the analysis made by Caprioli in Fig. 3, analyzing those patients whose visual fields got worse and those who did not get worse in four categories, specifically related to the rapidity of worsening visual field, the age of the patient, the amount of visual field loss, and the mean intraocular pressure. The dark bars are those who developed visual field loss, and the light bars those who did not. The figures at the top of each bar are the mean values. The units on the Y-axis represent the ranges, adjusted so as to have a similar denominator. Zero represents the lowest value and 100 the highest.
Risk factors continue to be used in ways that do not make sense. Wilensky, Podos and Becker pointed out in 1974 that “the individual parameters were not good predictive indicators (including intraocular pressure)” (Wilensky et al., 1974). Quigley et al. wrote in 1994, “The relationship of the development of field loss to race, myopia, family history of glaucoma and medical history are more complex than has been presumed” (Quigley et al., 1994).
One of the great errors we make in deciding on treatment is to base the care of individuals on population statistics. Fig. 5, from Caprioli’s study, shows on the left that the cup/disc ratios in patients with glaucoma are larger than cup/disc ratios in patients without glaucoma, on a population basis (Caprioli and Miller, 1988). Yet, on the right looking at the individual patients, one can see that it is not until the cup/disc ratio gets up to about .8 or more that it becomes even a fairly reliable indicator that the patient has glaucoma. Furthermore, the smallest cup/disc ratio occurred in a patient with glaucoma.
Figure 5.
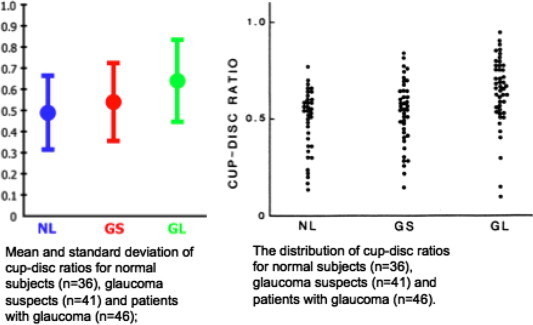
The mean and standard deviations of the cup/disc ratio in normal subjects, glaucoma suspects and those with glaucoma (left). Distribution of cup/disc ratios for the same groups (right). (Modified from citation 11.)
Visual fields are, of course, important in estimating the well-being of patients with glaucoma. However, trying to decide on whether visual fields are actually worsening or whether they represent glaucoma is far more complex than is usually admitted. In 2002, Weinreb wrote that the specific methods to identify true glaucomatous progression have yet to be determined. This situation is still true (Lee et al., 2002).
In any individual, (1) the predictive value of intraocular pressure in determining whether the optic disc and/or visual field will deteriorate is almost non-existent unless the intraocular pressure is in a range which is always abnormal, that is above 35 mm Hg (Foster et al., 2003); (2) there is virtually no predictive value of an individual’s intraocular pressure in determining who will become disabled; (3) we know that it is possible to prevent visual field loss in patients with glaucoma, yet many patients with glaucoma still get progressive visual field loss; (4) visual field changes are often misleading; (5) the significance of glaucoma is a function of the severity of the disease and the duration of the disease; and (6) the likelihood that a patient will become disabled due to glaucoma is (i) a function of the severity and duration of the disease; (ii) the self-care abilities of the patient; (iii) the skill of the physician; and (iv) the adaptability of the patient.
2. Severity of disease
The severity of disease is best estimated by the nature of the optic disc and how it changes. This report is primarily focused on increasing the skill of the physician in being able to estimate the nature of the optic disc and how that changes. This does not, however, lessen the tremendous importance of careful history-taking and of gonioscopy. In this report, however, we focus on evaluation of the disc.
Currently disc evaluation is often poor because of poor examination techniques, reliance on cup/disc ratios, and reliance on the results of image analyzers. We will present here the Disc Damage Likelihood Scale, which is a user-friendly method which correlates accurately with visual field changes.
Cup/disc ratios are not satisfactory ways of evaluating the health of the optic nerve. They do not take into account the position of the cup or the size of the disc. Fig. 6 illustrates four discs. Disc A is certainly pathologic. Disc B, which has the same cup/disc ratio as disc A, is probably normal. Disc D, which has much the largest cup/disc ratio, is probably at least as healthy as and perhaps even healthier than disc B.
Figure 6.
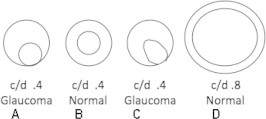
Discs A, B and C are of average size and disc D is of large size. The cup/disc ratios of the three smaller discs are about the same, but disc B is probably healthy and discs A and C are certainly abnormal. The c/d ratio does not tell the well from the sick. Disc D has the biggest cup. It also has the greatest rim area and is likely not to be glaucomatous.
The Disc Damage Likelihood Scale is a method of estimating the health of the disc, based on the width of the neuroretinal rim adjusted for the disc size, or if rim is already absent, the extent of circumferential loss of neuroretinal rim (Bayer et al., 2002). The system is illustrated in Fig. 7.
Figure 7.
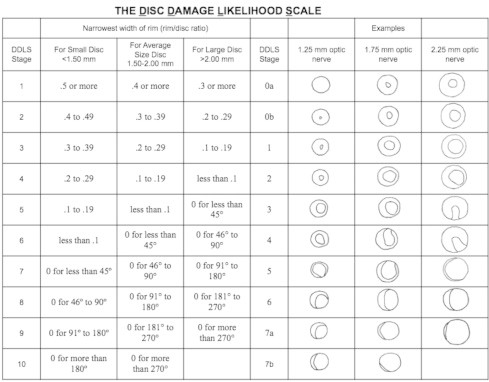
The Disc Damage Likelihood Scale (DDLS). This grading system is based on the radial width of the neuroretinal rim measured at its thinnest point. The unit of measurement is the rim/disc ratio, that is, the radial width of the rim compared to the diameter of the disc in the same axis. When there is no rim remaining, the rim/disc ratio is 0. The circumferential extent of rim absence (0 rim/disc ratio) is measured in degrees. For small discs (diameter <1.50 mm) the DDLS stage should be increased by 1; for large discs (diameter >2.00 mm) the DDLS stage should be decreased by 1.
To determine a score on the Disc Damage Likelihood Scale, the first step is to measure the disc with any of the standard techniques, such as using a high-plus lens or direct ophthalmoscopy. The second step is to identify the narrowest area of the rim in terms of rim/disc ratio. The largest possible rim/disc ratio is 0.5.
It is not true that large cups mean glaucoma. Fig. 8a shows the discs of two different patients, where both discs are very large. Neither patient has glaucoma. Neither patient has visual field loss. These are very large discs with narrow rims but without field loss. The patients have been followed for over ten years each, and there has been no change.
Figure 8.
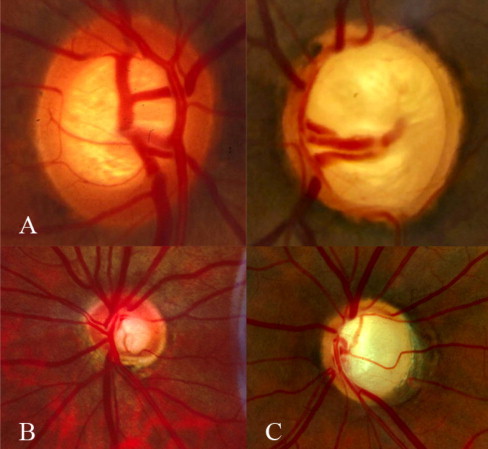
Optic nerves. (A) This illustrates large healthy discs with large cup/disc ratios from patients who have been followed for more than 30 years with no disc change or any other sign of glaucoma. (B) Shows a small glaucomatous optic disc without a large cup/disc ratio, but with an eccentric cup exhibiting an inferior focal notch associated with marked visual field loss. (C) Depicts a large disc with glaucomatous cupping.
In an average-sized disc where the rim is extremely narrow, but present, the DDLS is a 5. However, in a small disc this would be a DDLS of 6, and in a large disc it would be a DDLS of 4. Fig. 8b illustrates such a disc, which is small, but in which the rim is very narrow. In an average-sized disc, this would be a 5, but because it is a small disc it is graded as a 6. Fig. 8c illustrates a large disc which, were it an average disc, would be graded as DDLS of 7. However, because it is a large disc, it is a DDLS of 6. It is important to note, then, that the health of the disc in Fig. 8c is no better than the health of the disc in Fig. 8b.
The first challenge, then, is to determine the amount of damage that is present in the disc, that is, what is the stage of the disease. This can be graphed by using the Glaucoma Graph (Fig. 1). This is divided into three zones, the Green Zone, the Yellow Zone and the Red Zone. The DDLS stages 1-4 constitute the Green Zone. When a disc is in this area it is not possible on the basis of one examination to determine whether the disc is abnormal or normal. If the disc is found changed, that is, goes from a DDLS of 1 to a DDLS of 3, then one can say with certainty that the DDLS of 3 is abnormal.
In the Green Zone, patients are asymptomatic and it is not possible to determine whether glaucoma is actually present, unless a change (as just mentioned) has been documented. In the Yellow Zone, however, the patient definitely has some abnormality such as an abnormal visual field, or for purposes of this discussion, a DDLS of 5, 6 or 7. The patient definitely has glaucoma but is still asymptomatic, because the amount of damage is not sufficient to cause symptoms. The fact that a person is in the Yellow Zone and has glaucoma, however, does not necessarily mean that the process is active or that the person needs treatment. At minimum, it does mean that at some time glaucoma damage developed. In the Red Zone, the patient has symptoms and experiences disability such as difficulty in the dark, trouble reading, or one of the many symptoms caused by glaucomatous visual loss.
Thus, the stage of disease is estimated by considering the amount of disc damage as measured by the Disc Damage Likelihood Scale.
Other units could be used for the Y-axis on the Glaucoma Graph, such as the number of ganglion cells. However, at this time it is not feasible to count ganglion cells. Visual fields are also not satisfactory for the Y-axis because they show changes only relatively late in the disease and show high variability. As mentioned, cup/disc ratios or intraocular pressure are not satisfactory for staging of glaucoma.
3. Rate of change
It is not adequate merely to estimate the stage of the disease. It is also necessary to determine the rate at which the disease is changing. This requires establishing serial points, so that these points can be recorded sequentially and compared. The slope of the curve determines whether or not the condition is active or quiescent (in a patient who is not treated).
4. Estimated remaining years
The goal of treatment is to prevent individuals from getting into the Red Zone, or, if in the Red Zone already, to prevent them from developing further disability. When one is considering patients in the Green or the Yellow Zone, one has to know how long the disease will continue to progress as well as the rate of change. For many chronic conditions, including chronic glaucoma, the disease will continue for as long as the person lives. Thus, an estimate of the patient’s remaining years is an essential aspect of proper therapy. Lee has demonstrated that it is possible to predict quite accurately whether an individual will live for four more years (Lee et al., 2006). This can be done by taking into account factors, such as general health, lifestyle and family history. Age is a poor indicator of the remaining years. For example, a 92-year-old healthy woman has only a three percent chance of dying within four years, whereas a 50-year-old overweight male who smokes cigarettes, has a history of a myocardial infarction, and has high blood pressure has only a 50% chance of dying in less than four years. A healthy 96-year-old woman has a 97% chance of living to be 100. A 50-year-old overweight male smoker has no chance of living to be 100 years old.
5. Putting it all together to help patients
Combining a careful history with an accurate evaluation of the disc provides a useful way of directing treatment. Consider a 74-year-old banker in good health who has an estimated 20 remaining years. He has noted deteriorating vision, has a DDLS of 9, and has intraocular pressure on therapy of 13. He is already in the Red Zone. Thus, any further deterioration will result in an increase in his disability. Therefore, the basic approach to his treatment must be to prevent any further damage to his optic nerve. Because he is getting worse with pressures that are presumably somewhere around 13 mm Hg, it is apparent his pressure must be lower than 13 mm Hg. Assuming he is already on maximum medical therapy, he needs either a laser or a filtering procedure with the goal of further IOP reduction.
Consider a 64-year-old beautician who is in fair health, with an estimated 10 remaining years. She is quite unhappy with her vision and states she is continually getting worse. However, the history is not reliable; her intraocular pressures are 26 mm Hg in the right eye and 22 mm Hg in the left eye, on no treatment; and various medications have been tried, but each one has caused intolerable symptoms. She has been seen by us because she is referred for surgery. The disc in the left eye is slightly larger than that in the right eye, with a slightly larger cup; but there is good rim tissue in all areas. Both of her discs are DDLS’s of 4. She is in the green zone. It does not seem that she is actually getting worse. There is probably no need for any treatment at this time.
A 72-year-old engineer is referred because of optic nerves, which are believed to be glaucomatous, and intraocular pressures which are believed to be too high. The engineer is in excellent health and has an estimated 20 remaining years. He has no ocular symptoms other than discomfort from the medications that have been tried, he is a reliable historian, and the intraocular pressure on latanoprost and dorzolamide is 19 mm Hg in the right eye and 18 mm Hg in the left eye. His optic discs are extremely large, with very narrow rims which are intact in all areas; it is not surprising he has no visual field loss, because they are DDLS’s of 4 in each eye. He is also in the Green Zone on the Glaucoma Graph and no treatment is necessary. When his topical treatment was stopped, his pressures rose to 21 mm Hg in each eye. He was advised that probably no medications are necessary, and he is now being followed off medications.
A 56-year-old chemist is seen because his wife insisted that he have a second opinion. The chemist works in a pharmaceutical company as a research scientist. He has an estimated remaining 30 years. He believes his vision is still fine, although his wife complains that is now a dangerous driver and that she will no longer ride in the car with him at night. He denies this, but it becomes clear that he probably is not an accurate observer. He was told, by another ophthalmologist whom he consulted because he thought he needed a change in his glasses, that he had glaucoma and was advised to start therapy. The ophthalmologist told him his intraocular pressures were 15 mm Hg in the right eye and 16 mm Hg in the left eye, and because the patient “knew” that those pressures were normal, he also “knew” that he did not have glaucoma. His optic nerves are severely damaged, with a DDLS of 6 in the right eye and 7 in the left. On the Glaucoma Graph, he is in the Yellow Zone. When he was shown the Glaucoma Graph and it was explained to him that nobody starts in the Yellow Zone, and that he had moved from the Green Zone down into the Yellow Zone and would soon be in the Red Zone, he immediately understood that something was seriously wrong and he recognized that treatment was necessary.
In summary, the optic discs are vitally important in diagnosing and managing patients with glaucoma. Cup/disc ratios are not of much help in this regard because they do not take into account the size of the disc or the location of the cup. Therefore, they are not accurate estimates of whether a disc is damaged or not. Thus, cup/disc ratio should NOT be used and is clearly outdated.
There is a little amount of time to spend with each patient, and so it is essential to concentrate on what really counts. The things that really matter are (1) what the patient says; (2) the nature of the anterior chamber angle; (3) intraocular pressures above 35 mm Hg and asymmetry of more than 4 mmHg; (4) the nature of the optic disc; (5) the rate of change of the disc; (6) the estimated remaining years of life; and (7) pertinent socioeconomic factors. In order to provide appropriate care, it is necessary to concentrate on these things; almost everything else is just for refining the impression and the plan.
References
- Bayer A., Harasymowycz P., Henderer J.D., Steinmann W.G., Spaeth G.L. Validity of a new disk grading scale for estimating glaucomatous damage: correlation with visual field damage. Am. J. Ophthalmol. 2002;133:758–763. doi: 10.1016/s0002-9394(02)01422-8. [DOI] [PubMed] [Google Scholar]
- Caprioli J., Miller J.M. Videographic measurements of optic nerve topography in glaucoma. IOVS. 1988;29(8):1294–1298. [PubMed] [Google Scholar]
- Eid T.M., Spaeth G.L., Bitterman A., Steinmann W.C. Rate and amount of visual loss in 102 patients with open-angle glaucoma followed up for at least 15 years. Ophthalmology. 2003;110(5):900–907. doi: 10.1016/S0161-6420(03)00076-9. [DOI] [PubMed] [Google Scholar]
- Foster P.J., Machin D., Wong T.Y., Ng T.P., Kirwan J.F., Johnson G.J. Determinants of intraocular pressure and its association with glaucomatous optic neuropathy in Chinese Singaporeans: the Tanjong Pagar Study. Invest. Ophthalmol. Vis. Sci. 2003;44(9):3885–3891. doi: 10.1167/iovs.03-0012. [DOI] [PubMed] [Google Scholar]
- Gordon M.O., Beiser J.A., Brandt J.D., Heuer D.K., Higginbotham E.J., Johnson C.A. The Ocular Hypertension Treatment Study: baseline factors that predict the onset of primary open-angle glaucoma. Arch. Ophthalmol. 2002;120(6):714–720. doi: 10.1001/archopht.120.6.714. (discussion 829–830) [DOI] [PubMed] [Google Scholar]
- Hattenhauer M.G., Johnson D.H., Ing H.H., Herman D.C., Hodge D.O., Yawn B.P. The probability of blindness from open-angle glaucoma. Ophthalmology. 1998;105(11):2099–2104. doi: 10.1016/S0161-6420(98)91133-2. [DOI] [PubMed] [Google Scholar]
- Lee A.C., Sample P.A., Blumenthal E.Z., Berry C., Zangwill L., Weinreb R.N. Infrequent confirmation of visual field progression. Ophthalmology. 2002;109(6):1059–1065. doi: 10.1016/s0161-6420(02)01043-6. [DOI] [PubMed] [Google Scholar]
- Lee S.J., Lindquist K., Segal M.R., Covinsky K.E. Development and validation of a prognostic index for 4-year mortality in older adults. JAMA. 2006;295(7):801–808. doi: 10.1001/jama.295.7.801. [DOI] [PubMed] [Google Scholar]
- Leydhecker W., Akiyama K., Neumann H.G. Intraocular pressure in normal human eyes. Klin. Monbl. Augenheilkd. Augenarztl. Fortbildl. 1958;33(5):662–670. [PubMed] [Google Scholar]
- Nouri-Mahdavi, K., Hoffman, D., Gaasterland, D., Caprioli, J., 2005. Comparison of methods to predict visual field progression in glaucoma. Invest. Ophthalmol. Vis. Sci. 46 (E-Abstract 3729).
- Quigley H.A., Enger C., Katz J., Sommer A., Scott R., Gilbert D. Risk factors for the development of glaucomatous visual field loss in ocular hypertension. Arch. Ophthalmol. 1994;112(5):644–649. doi: 10.1001/archopht.1994.01090170088028. [DOI] [PubMed] [Google Scholar]
- Sommer A., Tielsch J.M., Katz J., Quigley H.A., Gottsch J.D., Javitt J. Relationship between intraocular pressure and primary open angle glaucoma among white and black Americans. The Baltimore Eye Survey. Arch. Ophthalmol. 1991;109(8):1090–1095. doi: 10.1001/archopht.1991.01080080050026. [DOI] [PubMed] [Google Scholar]
- Spaeth G.L., Paulus A. The colored glaucoma graph and its use in caring for patients with glaucoma: a new system of management presented in three parts. J. Curr. Glaucoma Pract. 2010;4(2):83–90. [Google Scholar]
- The Advanced Glaucoma Intervention Study (AGIS): 7, 2000. The relationship between control of intraocular pressure and visual field deterioration. The AGIS Investigators. Am. J. Ophthalmol. 130(4), 429–440. [DOI] [PubMed]
- Wilensky J.T., Podos S.M., Becker B. Prognostic indicators in ocular hypertension. Arch. Ophthalmol. 1974;91(3):200–202. doi: 10.1001/archopht.1974.03900060208010. [DOI] [PubMed] [Google Scholar]


