Abstract
Purpose
To study the utility of meibography for the morphology of meibomian glands in normal eyelids and in various eyelid diseases.
Design
A cross-sectional study.
Methods
A newly designed transilluminator, fitting both the upper along with lower eyelids, and an infrared camera were used to obtain video clips of the meibomian glands for 60 asymptomatic subjects with normal eyelid margin. Parameters studied included, ocular surface, Schirmer test, and tear breakup time (TBUT). The meibomian glands of patients with meibomian glands’ abnormality secondary to infectious, inflammatory, malignant, congenital, or post-radiation therapy disease related etiologies were compared with normal patients. Still pictures were extracted from the video clips to evaluate the meibomian glands for gland dropout and gross morphological changes.
Results
In normal subjects, meibomian glands appeared to be thinner and longer in the upper eye lids than in the lower eye lids. Gland dropout occured with increased age, more in the lower eye lid and in females. Excessive gland drop out (> 75%) was seen in patients with history of trachoma, Stevens Johnson syndrome, severe blepharitis, and post-radiation for orbital tumors. Variable gland drop out was noticed in patients with floppy eyelid syndrome, and blepharitis. In patients with congenital distichiasis, partial or complete gland drop out at the part of the eyelid margins affected by distichiasis was noticed.
Conclusions
The newly designed transilluminator permitted the examination of both upper and lower eye lid meibomian glands with minimal discomfort. Evaluating the anatomical changes involving meibomian glands with meibography may help increase our understanding of the meibomian gland-related diseases, monitor the effects of treatment, and provide helpful information for patient education.
Keywords: Meibography, Meibomian glands, Dry eye, Blepharitis, Trachoma, Radiation, Chalazion, Distichiasis
1. Introduction
Healthy tear film is vital for vision clarity and eye comfort. Meibomian glands, which are specialized pilosebaceous units, play an important role in the health of tear film through their lipid secretion. The lipid component of the tear film maintains stability and prevents the premature evaporation of the aqueous tear component. Abnormalities in the lipid production of meibomian glands lead to chronic irritation of and to damage to the ocular surface epithelium.
Examination of meibomian glands ranges from the simple slit-lamp evaluation of meibomian gland orifices and lid margin anatomy to more advanced testing methods such as meibometry, which measures lipid secretion by the glands, and meibography, which provides images of the meibomian glands with infrared light.
Infrared photography and imaging of meibomian glands (meibography) were originally described by Tapie (1977). In its early stages, meibography was performed with infrared film and was considered a costly and time-consuming procedure. The introduction of video meibography transformed this costly and time-consuming procedure into an inexpensive, noninvasive, immediate evaluation of the anatomy of meibomian glands during the clinic visit. Several studies have described the appearance of meibomian glands in normal lower eyelids, meibomian gland dysfunction, blepharitis, and chalazion (Den et al., 2006; Mathers and Choi, 2004; Robin et al., 1985; Goto et al., 2002). Although meibography has been around for 30 years, it has not gained popularity in clinical practice. We propose that modifying the instrumentation and interpretation of meibography will improve its assessment of meibomian glands.
Based on the principle of infrared video meibography described by Mathers et al. (1994), we made modifications in instrumentation, with the aim of evaluating the meibomian glands of eye lids during the clinical visit in a shorter period of time with minimal patient discomfort. Our objectives were to study the appearance of meibomian glands of eyelids in subjects with normal eyelids of different age groups, and in patients suffering from a variety of eyelid diseases presenting with ocular irritation, eyelid swelling, and followed by eyelid reconstruction.
2. Methods
After obtaining the approval of the Institution Review Board, the anatomy of meibomian glands with video meibography was studied in a group of 60 subjects. We included only asymptomatic subjects without history of contact lens wearing and topical eye medication. Before enrollment, the subjects were assessed to ensure a normal slit-lamp examination of the eyelids and ocular surface. In addition, the tear breakup time (TBUT) test (10 s or more) and the Schirmer test (10 mm or more) 2 min after applying topical anesthetic eye drops were performed. These subjects were randomly recruited from patients, patient companions, and employees from the Department of Ophthalmology, University of Iowa Hospitals and Clinics, Iowa City, Iowa, United States. In the second group, patients with a variety of eyelid diseases presented to oculoplastic clinic were studied.
Written informed consent was obtained from each patient prior to enrollment into the study. After obtaining ophthalmic history and conducting a through slit-lamp examination to rule out eyelid and ocular surface abnormalities, TBUT as well as the Schirmer test with topical anesthesia (proparacaine hydrochloride 0.4%; Akorn, Buffalo Grove, Ill) were performed.
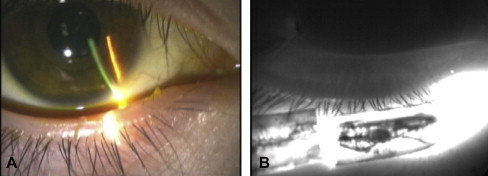
Meibography video clips were recorded with a black and white Ultracon camera (RCA TC2012/U tube), sensitive to visible and near infrared light (>50% efficiency at 900 nm). The camera was equipped with a macro/zoom lens (Javelin 99035J, 18–108 mm, f2.5; Javelin Electronics, Torrance, Calif). A cylindrical probe (measuring 25 mm in length and 1.5 mm in diameter) attached to a halogen Finhoff transilluminator (Welch Allyn) was used as a light source (Fig. 1A). The halogen Finhoff transilluminator produces a mixture of visible and infrared light. The size and the shape of the transilluminator allowed evaluation of meibomian glands of both eyelids. The transilluminator was positioned against the skin of the lower lid and was used to evert the lid over it. For the upper lid, the transilluminator was placed on the eyelid skin, and the eyelid was then everted over the transilluminator (Fig. 1B). The focus and magnification were then adjusted to obtain optimal images of the meibomian glands. The images were recorded with a 0.75-in videocassette machine (Sony U-matic V05600; Sony Corp of America, Teaneck, NJ). High-quality video meibography images were obtained in 2 min for each eye lid for almost all subjects. Subject discomfort and inconvenience were minimal.
Figure 1.
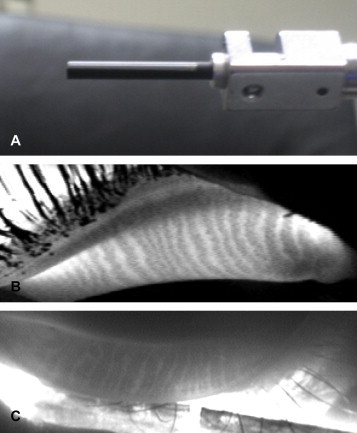
(A) Close-up picture of the transilluminator cylindrical probe (measuring 25 mm in length and 1.5 mm in diameter); (B) Meibography image of the upper eyelid; meibomian glands are the broad dark vertical lines seen in the image. (C) Meibography image of the lower eyelid.
Recorded video meibography images of each individual were used to evaluate the appearance of the meibomian glands and the presence of gland dropout.
2.1. Correlation of meibography with histopathology
We performed meibography for a patient with floppy eyelid syndrome prior to a full-thickness wedge resection of the upper eye lid. A correlation between the meibography image and the low-power histopathological magnification of the resected tarsus was made.
3. Results
3.1. Normal eyelids
Of the 60 subjects (age range 20–80 years) studied, 24 (40%) were males, with a mean age of 48.8 years, and 36 (60%) were females, with a mean age of 50.2 years. Meibography revealed that meibomian glands of the upper eyelids appeared thinner and longer as compared with the lower eyelids.
3.1.1. Gland dropout
No significant gender differences (P > 0.70) were detected. The age effect on gland dropout was not significant in the upper eye lid in males (P > 0.99). In females, the odds ratio for gland dropout in the upper eye lid was 1.25 (95% CI, 0.95–1.65; P = 0.18) per 5-year increase in age. For the lower lid, the odds ratio for gland dropout was 1.74 (95% CI, 0.79–3.81; P = 0.31) per 5-year increase in age for males and 1.20 (95% CI, 0.93–1.54; P = 0.29) for females. For eye lid effects, no significant difference was found in the occurrence of gland dropout in the lower and upper eyelids among males and females (P = 0.31 and 0.12, respectively).
3.1.2. Correlation of meibography with histopathology
A reasonable correlation between the meibography image of meibomian glands and the lower power examination of the same tarsal segment (Fig. 2A and B) on histopathology was noted.
Figure 2.
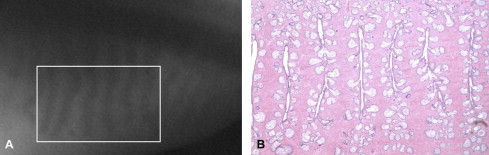
(A) Meibography image of the upper eyelid for a patient with a floppy eyelid syndrome. The image was taken shortly before he underwent wedge resection of the left upper eyelid. (B) Histopathological picture of the resected tarsus of the same patient showed a reasonable correlation with the meibography image (hematoxylin and eosin stain, 10×).
3.2. Eyelid disease due to infection/inflammation
3.2.1. Blepharitis
Fourteen patients presented with ocular irritation and signs of chronic blepharitis were studied. Meibography for these patients showed meibomian gland drop out ranging from few gland drop out (1–2) to almost total gland drop out (Fig. 3A and B). The gland drop out distribution appeared to be similar in both upper and lower eyelids.
Figure 3.

(A) Meibography image of the lower eye lid of a patient with mild blephritis showing meibomian glands with normal broad dark vertical lines. (B) Meibography image of lower eye lid of another patient with severe blephritis showing massive gland drop out.
3.2.2. Chalazion
Five patients presented with lid swelling due to chalazion were studied. Meibography showed obscuration of around 5–10 meibomian glands at the site of chalazion. The exact number of obstructed glands was difficult to identify with meibography.
Two patients had surgical drainage of their chalazia more than a year prior to examination with meibography. In one of them, only partially missing gland surrounded by normal appearing glands at the site of drained chalazion was seen. In the other patient, there was only one single missing gland in the eyelid previously harboring the chalazion.
Two patients had chalazia that resolved after medical treatment. One missing gland was seen at the site of the resolved chalazion in one patient and 2 missing glands in the other patient.
3.2.3. Lid swelling simulating chalazion
A 36 years old female presented with left upper eye lid redness, swelling and evidence of previous drainage from the chalazion lesion. Meibography revealed normal appearing meibomian glands next to a depression in the tarsus.
3.2.4. Thyroid eye disease
Meibography was performed on 6 patients with thyroid eye disease and moderate to severe exposure keratopathy. Among these patients, there was no gland drop out in three patients while the rest three had scattered 1–2 glands dropping out throughout the upper and lower eyelids.
3.3. Eyelid disease secondary to conjunctival pathology
3.3.1. Trachoma
Three adult patients, having previous history of trachoma, who presented with ocular irritation were found to have almost complete glands drop out from the upper eye lids (Fig. 4A and B). Only few glands were seen from the lower eye lid.
Figure 4.
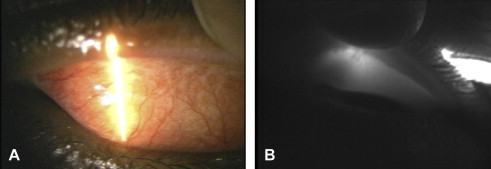
External photographs of the everted upper eye lid palpebral congunctiva of a 45-year-old male with history of trachoma (A). (B) Meibography image of the same eyelid showing almost total gland drop out.
3.3.2. Stevens Johnson syndrome
Meibography of eyelids was performed for two adult patients who had Steven Johnson syndrome as a result of a drug reaction. Both patients had undergone mucous membrane grafting for correction of cicatricial entropion of their left upper eye lids. Meibography of both upper eyelids showed almost total glands drop out. In addition, both patients had undergone their lower eyelid tarsal fracture for entropion correction. Meibography revealed the presence of approximately 25% of meibomian glands between the eyelid margin and the horizontal line of tarsal fracture in both lower eye lids in one patient and in right lower lid in the other patient. No glands were seen proximal to the tarsal fracture line.
3.4. Sebaceous cell carcinoma arising in the meibomian gland
The eyelids of an elderly woman who presented with diffuse redness and swelling of her left upper eye lid. Meibography of the eye lid showed gland drop out of the lateral third of the eye lid with normal meibomian glands in the medial two third. The histopathology showed sebaceous cell carcinoma of the lateral part of the left upper eyelid with pagetoid spread extending over the medial part of the eyelid.
3.5. Following eyelid reconstruction
Three patients who underwent eyelid reconstruction following excision of basal cell carcinoma were examined with meibography. Two of them had a Hughe’s procedure and one had free tarsal graft from the upper eyelid of one eye to the lower lid of the other eye. The remaining part of the tarsus at the donor site maintained normal meibomian glands. However, no glands were seen in the transferred tarsus.
3.6. Post-orbital radiation
The meibomian glands of 4 patients who had unilateral radiotherapy for orbital tumors were examined for presence of meibomian glands. Meibography showed almost complete glands drop out of both upper and lower eye lids for 3 patients and 25% glands drop out in one patient. Meibography of the contralateral non-radiated side was normal for all patients (Fig. 5A and B).
Figure 5.
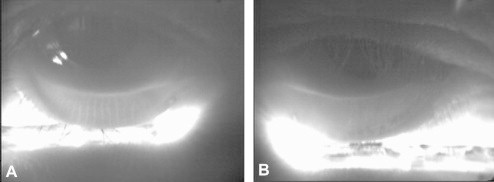
(A) Meibography image of the normal lower eyelid of a 12-year-old boy showing meibomian glands having normal broad dark vertical lines appearance. (B) Meibography image of the left lower eyelid after having undergone radiation for rhabdomyosarcoma, shows massive gland drop out.
3.7. Congenital meibomian gland abnormality – distichiasis
One child and one adult presented with bilateral congenital lower eyelid distichiasis without having any previous surgical intervention. On the child’s eyelids the distichiasis was present only in the medial half of both lower eyelids. Meibography showed partial to complete glands loss in the medial part of both lowers eyelids (Fig. 6A and B). In the adult patient, distichiasis was involving the entire lower of his lids. Meibography revealed total glands drop out from both lower eyelids.
Figure 6.
(A) Slit-lamp photograph of a 11-year-old female child with congenital distichiasis showing presence of extra row of eyelashes medial part of lower eyelid. (B) Meibography image of the same eyelid showing partial missing glands at the involved area of the lid.
4. Discussion
Meibomian glands mainly consist of acini filled with lipids. When near infrared light and infrared light coming from a transilluminator pass through the lipid, the light becomes scattered (van Veen et al., 2005). This scattering gives the meibomian glands a dark appearance compared with the rest of the tarsus when the image is captured with an infrared camera. With the help of an infrared camera and a newly designed transilluminator, one can examine the anatomy of meibomian glands of eyelids.
The number of meibomian glands is higher in the upper eyelid (approximately 30–40 meibomian glands) as compared to the lower eyelid (approximately 20–30 meibomian glands) (Driver and Lemp, 1996). Interestingly, meibography showed the meibomian glands of the upper eyelid were thinner and longer as compared with the lower eyelids. It has been shown that meibomian gland secretion may decrease in quantity but not in quality with age (Hykin and Bron, 1992). However, no significant differences in glands drop out with regard to either age or gender in the present study was detected. Further studies may be required to evaluate structural–functional relationships of meibomian glands in different age groups.
Several changes in the anatomy of meibomian glands have been reported with aging, such as meibomian gland orifice obliteration, pouting, narrowing, and increased gland dropout (Den et al., 2006; Hykin and Bron, 1992; Arita et al., 2008). The occurrence of gland dropout was very low in our normal subject studied, which may be secondary to their having normal TBUT and Schirmer test scores. This may explain the differences between our results and those of a previous study evaluating the association between gland dropout and aging (Den et al., 2006).
Abnormalities in the lipid production of meibomian glands may lead to chronic eye irritation and damage to the ocular surface. Clinical examination alone may not be enough to evaluate the meibmian glands in such patients. Meibography may provides a simple and fast way for meibomian gland morphology evaluation for patients with irritated eyes. In addition to its usage as a diagnostic tool to help physicians, meibography may offer easy demonstration regarding the meibomian glands disease for the patients education. The list of eyelid diseases for which meibography has a potential role for evaluating the extent of meibomian glands involvement is large.
Blepharitis is a common eyelid disease and it varies in the severity in different age groups. Clinical examination alone may not determine the extent of meibomian glands involvement. Meibography may help in assessing the degree of glands drop out in these patients. In patients with severe glands drop out, significant improvement to medical treatment may not be expected.
Visualization of the exact blocked meibomian glands in patients with chalazia may not be possible with meibography due to the inflammatory process in the involved gland and the surrounding area. After resolution of the chalazion, one may see the involved glands by meibography. With availability of different treatment options for chalazion, meibography may offer the chance to image the effect of the treatment used on the area of the eyelid affected.
Trachomatous scarring and orbital radiation may present with eye irritation leading to meibomian glands atrophy (Karp et al., 1979; Al-Rajhi et al., 1993). These patients may show massive glands drop out even with mild eyelid margin abnormalities by meibography.
Eyelid surgery may require incision through the tarsus for eyelid reconstruction or correction of eyelid malposition. Meibography may facilitate evaluation of the impact of the surgery on the meibomian glands. For patients at risk for development of dry eye following eyelid surgery, meibography may help the surgeon to plan the procedure with minimum chance of compromising the normal appearing meibomian glands.
Patients with distichiasis may have abnormal growth of lashes from the orifices of the meibomian glands on the posterior lamella of the tarsal plate which can be congenital or acquired. The congenital distichiasis results from failure of epithelial germ cells of the pilosebaceous units to differentiate completely to meibomian glands (Scheie and Albert, 1966). Meibography may show part of the meibomian glands still present on the part of the eyelid involved by congenital distichiasis.
It is hoped that with the advancement in new imaging techniques, meibography may be a useful tool for the clinical evaluation of patients having meibomian gland dysfunction due to different disease processes.
Conflict of interest
The authors have no conflicts of interest or proprietary interest in any of the instruments or topics presented in this manuscript.
Footnotes
This work was supported in part by an unrestricted educational grant from Research to Prevent Blindness, Inc., NY, and The University of Iowa Department of Ophthalmology and Visual Sciences Resident and Fellow Research Program.
References
- Al-Rajhi A.A., Hidayat A., Nasr A., Al-Faran M. The histopathology and the mechanism of entropion in patients with trachoma. Ophthalmology. 1993;100(9):1293–1296. doi: 10.1016/s0161-6420(93)31485-5. [DOI] [PubMed] [Google Scholar]
- Arita R., Itoh K., Inoue K., Amano S. Noncontact infrared meibography to document age-related changes of the meibomian glands in a normal population. Ophthalmology. 2008;115(5):911–915. doi: 10.1016/j.ophtha.2007.06.031. [DOI] [PubMed] [Google Scholar]
- Den S., Shimizu K., Ikeda T., Tsubota K., Shimmura S., Shimazaki J. Association between meibomian gland changes and aging, sex, or tear function. Cornea. 2006;25(6):651–655. doi: 10.1097/01.ico.0000227889.11500.6f. [DOI] [PubMed] [Google Scholar]
- Driver P.J., Lemp M.A. Meibomian gland dysfunction. Surv. Ophthalmol. 1996;40(5):343–367. doi: 10.1016/s0039-6257(96)80064-6. [DOI] [PubMed] [Google Scholar]
- Goto E., Monden Y., Takano Y., Mori A. Treatment of non-inflamed obstructive meibomian gland dysfunction by an infrared warm compression device. Br. J. Ophthalmol. 2002;86(12):1403–1407. doi: 10.1136/bjo.86.12.1403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hykin P.G., Bron A.J. Age-related morphological changes in lid margin and meibomian gland anatomy. Cornea. 1992;11(4):334–342. doi: 10.1097/00003226-199207000-00012. [DOI] [PubMed] [Google Scholar]
- Karp L.A., Streeten B.W., Cogan D.G. Radiation-induced atrophy of the meibomian gland. Arch. Ophthalmol. 1979;97(2):303–305. doi: 10.1001/archopht.1979.01020010155013. [DOI] [PubMed] [Google Scholar]
- Mathers W.D., Choi D. Cluster analysis of patients with ocular surface disease, blepharitis, and dry eye. Arch. Ophthalmol. 2004;122(11):1700–1704. doi: 10.1001/archopht.122.11.1700. [DOI] [PubMed] [Google Scholar]
- Mathers W.D., Daley T., Verdick R. Video imaging of the meibomian gland. Arch. Ophthalmol. 1994;112(4):448–449. doi: 10.1001/archopht.1994.01090160022008. [DOI] [PubMed] [Google Scholar]
- Robin J.B., Jester J.V., Nobe J., Nicolaides N., Smith R.E. In vivo transillumination biomicroscopy and photography of meibomian gland dysfunction. A clinical study. Ophthalmology. 1985;92(10):1423–1426. doi: 10.1016/s0161-6420(85)33848-4. [DOI] [PubMed] [Google Scholar]
- Scheie H.G., Albert D.M. Distichiasis and trichiasis: origin and management. Am. J. Ophthalmol. 1966;61(4):718–720. doi: 10.1016/0002-9394(66)91209-8. [DOI] [PubMed] [Google Scholar]
- Tapie R. Etude biomicroscopique des glandes de Meibomius. Ann. Oculist. 1977;210:637–648. [Google Scholar]
- van Veen R.L., Sterenborg H.J., Pifferi A., Torricelli A., Chikoidze E., Cubeddu R. Determination of visible near-IR absorption coefficients of mammalian fat using time- and spatially resolved diffuse reflectance and transmission spectroscopy. J. Biomed. Opt. 2005;10(5):054004. doi: 10.1117/1.2085149. [DOI] [PubMed] [Google Scholar]


