Abstract
Purpose
To compare central corneal thickness (CCT) measurements taken with Pentacam, noncontact specular microscope (NCSM), and ultrasound pachymetry (US) in normal and post-laser in situ keratomileusis (LASIK) eyes and to assess the agreement between the three devices.
Design
Prospective clinical trial.
Patients and methods
Central corneal thickness (CCT) was measured in 94 eyes of normal volunteer and in 72 eyes of post-LASIK patients. Measurements were made with the three devices.
Results
In normal eyes, the mean (±SD) CCT taken with Pentacam, NCSM, and US was 552.6 ± 36.8 μm, 511.9 ± 38.6 μm, and 533.3 ± 37.9 μm, respectively. The average values of CCT taken with the three instruments were significantly different. In post-LASIK eyes the mean CCT with Pentacam, NCSM, and US was 483.02 ± 6.03 μm, 450.7 ± 5.3 μm, and 469.5 ± 5.8 μm, respectively. The average values of CCT taken were significantly different for Pentacam vs. NCSM (P = 0.046) and Pentacam vs. US (P = 0.02), but not significant for NCSM vs. US (P = 0.352). The Bland and Altman method for assessing clinical agreement between 3 instruments showed that in normal eyes, the mean values and paired differences of the three CCT devices were found to be statistically independent. In post-LASIK eyes, there was significant association between the difference and the mean of the Pentacam and NCSM, and US and NCSM.
Conclusion
The three devices cannot be used interchangeably in normal and post-LASIK eyes. Pentacam tends to give significantly thicker reading than ultrasound pachymetry.
Keywords: Central corneal thickness, Ultrasound pachymetry, Noncontact specular microscopy, Pentacam, Scheimpflug camera
1. Introduction
Corneal thickness measurement is essential factor to assign to corneal status and endothelial pump mechanism (Waring et al., 1982). Evaluation of corneal thickness is important in wide range of disorders. Such as ectatic dystrophies (Insler and Baumann, 1986), contact lenses related complication (Solomon, 1996; Liu and Pflugfelder, 2000), dry eye (Liu and Pflugfelder, 1999), and diabetes mellitus (Larsson et al., 1996). It is also increasingly important procedure in the evaluation of patients with ocular hypertension or glaucoma (Copt et al., 1999).
The outcome and success rate of refractive surgical procedure rely on accuracy of pachymetry measurements (Maldonado et al., 2000). A number of instruments have been developed to determine corneal thickness including ultrasound pachymetry (Salz et al., 1983; Bovelle et al., 1999; Bechmann et al., 2001; Modis et al., 2001a; Fakhry et al., 2002; Suzuki et al., 2003; Rainer et al., 2004; Zhao et al., 2007), optical pachymetry (Salz et al., 1983; Bovelle et al., 1999; Modis et al., 2001a), contact and noncontact specular microscope (Bovelle et al., 1999; Modis et al., 2001a; Zhao et al., 2007), scanning slit topography/pachymetry (Fakhry et al., 2002), corneal confocal microscopy (Li et al., 1997), ultrasound biomicroscopy (Avitabile et al., 1997), partial coherence interferometry (Rainer et al., 2004), and optical coherence tomography (Bechmann et al., 2001).
At present, ultrasound is the most frequently used pachymetry technique and is considered the gold standard because of its high degree of interobserver, and interinstrument reproducibility (Wheeler et al., 1992; Marsich and Bullimore, 2000; Gunvant et al., 2003; Miglior et al., 2004). However, results among observers may vary significantly (Bovelle et al., 1999). It uses high-frequency sound waves to detect the epithelial and endothelial layers. Knowing the velocity of sound in corneal tissue, the distance between the two reflecting surfaces can be calculated (Tam and Rootman, 2003). However, the need for topical anesthesia, contact of the probe with the cornea, risk of epithelial lesion, possible incorrect and unrepeatable probe placement, differences in pressure applied during measurement, lack of a fixation light for gaze control, ill-defined points of reflection of ultrasound within the cornea, and the variability of sound speed in wet and dry tissues result in continuous search for alternative measures (Bechmann et al., 2001; Suzuki et al., 2003; Ucakhan et al., 2006; Javaloy et al., 2004).
Noncontact specular microscopy is capable of specular microscopy and pachymetry at the same time. Focusing on the endothelium, this machine provides specular images and measures the focal distance, which can be calculated as corneal thickness. Noncontact specular microscopy reported to have more consistent reading from one operator to another, but gives significantly lower reading than those generated by ultrasound pachymetry (Bovelle et al., 1999; Modis et al., 2001a,b; Fujioka et al., 2007).
The Pentacam instrument uses a rotating Scheimpflug camera system and provides 3-dimensional scanning of the whole anterior segment of the eye. Pentacam can provide information regarding corneal pachymetry, anterior and posterior corneal topography, anterior chamber depth, volume, and angle and lens density (Swartz et al., 2007). The noncontact measuring process with the Pentacam system takes 2 s, performing 12–50 single captures while rotating around the optical axis of the eye. As every slit image consists of 500 true elevation points, the Pentacam system detect, in total, up to 2500 height values, which are processed to a 3-dimensional model of the entire anterior eye segment (Khoramnia et al., 2007). The agreement of the Pentacam system with ultrasound pachymetry in measuring the central corneal thickness is still open to debate.
This prospective study was performed to compare CCT measurements using ultrasound pachymetry (US), noncontact specular microscope (NCSM), and Pentacam system in normal and post-LASIK eyes.
2. Patients and methods
Central corneal thickness was measured in 2 groups of patients. Group I: normal subject: 47 normal volunteers (94 eyes) with average age of 33 years (range 21–46 years). Group II: post-LASIK eyes: 36 post-LASIK patients (72 eyes) with average age of 31 years (range 21–44 years). Detailed history and slit lamp exam was done by single ophthalmologist (Dr. A.M.A). The inclusion criteria for recruiting eyes were having clear cornea, no previous ocular surgery apart from LASIK done in the post-LASIK group, no ocular medication, and no history of contact lens wear for at least one week. For group I, the curvature maps obtained with Pentacam should show no signs of keratoconus or abnormal readings.
All measurements were done at the same time of the day, between 10:00 am and 2:00 pm, at least 3 h after awakening with a 5 min interval between each test. In all subjects, measurements started with Pentacam (Oculus, Wetzlar, Germany), then noncontact specular microscopy (SP-2000P, Topcon Corporation, Tokyo, Japan), and lastly with ultrasound pachymetry (SP-3000, Tomey Corporation, Nagoya, Japan) by masked single experienced technician.
For Pentacam, patient was asked to look at fixation target, the measurement automatically started whenever correct alignment with the corneal apex and focus was achieved. The average of the five readings from central 4 mm of the cornea (inferior, nasal, superior, temporal, and central) was recorded as CCT.
For NCSM, the subject was positioned with his or her chin in a cup and forehead against a headband. Automated mode low flash intensity pictures from the center of the cornea were taken while the subject focused on a fixation light. After the proper position of the alignment dot, circle, and bar on the screen, the picture was captured and printed out with numerical data, including thickness. CCT values were accepted only if the endothelial cells were in clear focus. If the image captured didn’t clearly outline the endothelial cells, patients were asked to remove their head, blink, and a second measurement was performed.
For the ultrasound pachymetry, the cornea was anaesthetized with preservative free oxybuprocaine 0.4% applied 30 s prior to measurement. The subject was seated on the chair and asked to look straight ahead while the pachymeter probe was slightly placed perpendicularly to the central corneal surface, as located visually by the investigator and five consecutive measurements were taken. The mean of the five measurements was used as CCT.
3. Results
3.1. Group I: normal subjects
The study included 47 normal volunteers (94 eyes) with average age of 33 years (range 21–46 years). Fifty-eight percent of the participants were women while 42% were men.
The mean (±SD) CCT (Table 1) was highest with Pentacam followed by US then NCSM. One-way factorial ANOVA showed that the mean values of measurements done significantly differ between Pentacam and US (P = 0.03), between Pentacam and NCSM (P < 0.01), and between NCSM and US (P < 0.01) (Table 2). The paired t test disclosed that the mean difference of CCT measured with Pentacam and NCSM (46.1 ± 53.7 μm), Pentacam and US (19.3 ± 8.85 μm), and US and NCSM (26.8 ± 54.3 μm) was statistically significant (P < 0.01).
Table 1.
Summary of CCT in normal and post-LASIK patients.
| Test | Mean CCT ± SD (μm) |
|
|---|---|---|
| Normal patients | Post-LASIK patients | |
| Pentacam | 552.6 ± 36.8 | 483.02 ± 6.03 |
| Ultrasound | 533.3 ± 37.9 | 469.5 ± 5.8 |
| Specular microscopy | 511.9 ± 38.6 | 450.7 ± 5.3 |
CCT = central corneal thickness; SD = standard deviation.
Table 2.
Summary of one way factorial ANOVA in normal and post-LASIK patients.
| Test |
P value |
|
|---|---|---|
| Normal patients | Post-LASIK patients | |
| Pentacam vs. ultrasound | 0.03 | 0.02 |
| Pentacam vs. specular microscopy | <0.01 | 0.046 |
| Specular microscopy vs. ultrasound pachymetry | <0.01 | 0.352 |
Pearson’s correlation coefficient test showed good correlation between each instrument; with NCSM and US (r = 0.974), Pentacam and US (r = 0.972) and Pentacam and NCSM (r = 0.966).
Fig. 1 shows Bland–Altman plots of agreement on CCT measured with the three methods. The 95% limits of agreement were 1.67–37.1 μm between Pentacam and US, 20.8–60.5 μm between Pentacam and NCSM, and 3.62–38.9 μm between US and NCSM. All three graphs show more or less similar range of differences. The last graph comparing means to differences of ultrasound and specular microscopy shows less bias and more consistency. However, graphs do not provide any form of clear relationship. There was no significant association between the difference and the mean of each pair of three CCT devices.
Figure 1.
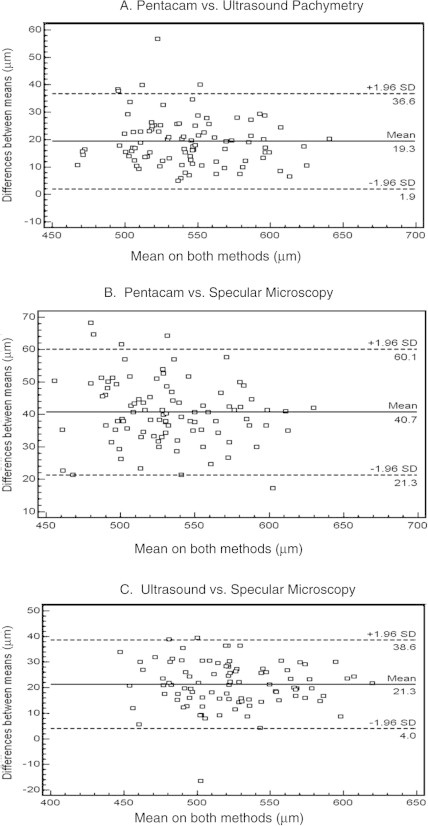
Bland–Altman plot comparing mean CCT and CCT difference in normal eyes for all the three instruments.
3.2. Group II: post-LASIK subject
The study included 36 post-LASIK patients (72 eyes), with average age of 31 years (range 21–44 years). Sixty-eight percent of the participants were women and 32% were men.
The mean CCT (Table 1) was highest with Pentacam followed by US then NCSM. One-way factorial ANOVA showed that the mean values of measurements done significantly differ between Pentacam and US (P = 0.02), between Pentacam and NCSM (P = 0.046), but not between NCSM and US (P = 0.352) (Table 2). The paired t test disclosed that the mean difference of CCT measured with Pentacam and NCSM (32.25 ± 10.83 μm), Pentacam and US (13.52 ± 11.6 μm), and US and NCSM (18.73 ± 11.73 μm) was statistically significant (P < 0.01).
Pearson’s correlation coefficient test showed good correlation between each instrument; with NCSM and Pentacam (r = 0.983), Pentacam and US (r = 0.974) and US and NCSM (r = 0.973).
Fig. 2 shows Bland–Altman plots of agreement on CCT measured with the three methods. The 95% (CI) limits of agreement were −9.8 μm to 36.8 μm between Pentacam and US, 10.4–54.0 μm between Pentacam and NCSM, and −4.9 μm to 42.3 μm between US and NCSM. Similar to normal measurements, all graphs show more or less similar ranges of differences with more consistencies and less outliers between ultrasound and specular microscopy measurements. There was significant association between the difference and the mean of the Pentacam and NCSM, and US and NCSM.
Figure 2.
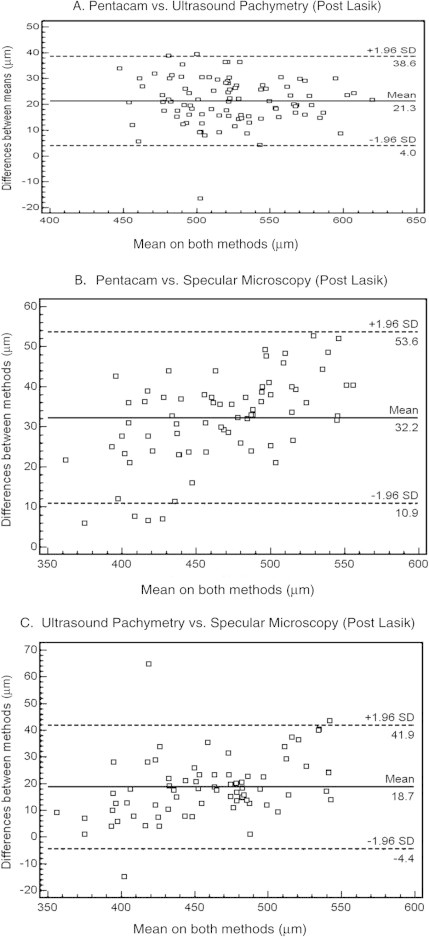
Bland–Altman plot comparing mean CCT and CCT difference in post-LASIK eyes for all the three instruments.
4. Discussion
The current study demonstrated that there were significant differences in the CCT measured with Pentacam, NCSM, and US in normal and post-LASIK eyes. The measurements with Pentacam were significantly thicker than the other two methods in both groups. The measurements with US were significantly thicker than NCSM in normal eyes and not significant in post-LASIK eyes. All the three devices showed good correlation with each other.
Studies done in normal cornea showed close agreement between Pentacam and ultrasound CCT measurements. Lackner et al. (2005), O’Donnell and Maldonado-Codina (2005) and Barkana et al. (2005) found the Pentacam’s CCT measurement to be thinner than ultrasound by 6.0 μm, 9.8 μm, and 6.1 μm, respectively. Ucakhan et al. (2006), Fujioka et al. (2007), Amano et al. (2006) and Al-Mezaine et al. (2008) found the Pentacam’s CCT measurement to be thicker than ultrasound by 2.7 μm, and 6.4 μm, 8.0 μm, and 8.2 μm respectively. Ucakhan et al. (2006) and Fujioka et al. (2007) found that NCSM CCT measurement to be thinner than Pentacam by 21.9 μm and 7.45 μm, respectively. NCSM CCT measurement was thinner than ultrasound pachymetry. Ucakhan et al. (2006), Fujioka et al. (2007), Bovelle et al. (1999) and Modis et al. (2001a) found that NCSM CCT measurements were thinner than US by 19.4 μm, 0.98 μm, 32 μm, and 28 μm, respectively.
Studies done in post-LASIK eyes showed close agreement between Pentacam and ultrasound CCT measurements. Ciolino et al. (2008) found the Petacam’s CCT measurements to be thicker than ultrasound by 1.4 μm.
Zhao et al. (2007) and Kawana et al. (2004) found that ultrasound CCT was thicker than NCSM in post-LASIK eyes. Our results showed that Pentacam’s CCT measurements was thicker than US measurements in normal and post-LASIK eyes by 19.3 μm and 13.5 μm, respectively, which was higher than previous studies (Ucakhan et al., 2006; Fujioka et al., 2007; Amano et al., 2006; Ciolino et al., 2008). The discrepancy between Pentacam and US can be explained by the fact that the ultrasound probe come in touch with the cornea and displace the 7–40 μm thick tear film which may result in thinner CCT measurements. The differences found in our study was bigger than what was found in other studies and this may be related to the corneal hydration following the application of local anesthesia, or to the different US pachymeter models used in different studies. The other possible reason for this discrepancy between studies is the differences in the value of corneal thickness recorded as CCT from the Pentacam pachymetry map. Future studies should specify the time between local anesthesia application and the US measurements, use same US model and avoid differences in the CCT recorded from the Pentacam system.
The US CCT measurements was thicker than NCSM CCT measurements in normal and post-LASIK eyes by 26.8 μm and 18.7 μm, respectively, which does agree with previous studies (Bovelle et al., 1999; Modis et al., 2001a; Zhao et al., 2007; Ucakhan et al., 2006; Fujioka et al., 2007; Kawana et al., 2004). These differences are attributable to the different operating principles. NCSM depend on the reflection of light, and the US pachymetry depend on the reflection of ultrasonic from the anterior and posterior corneal surfaces. In ultrasonic pachymetry, the exact posterior reflection point is not known; it may be located between Descemet’s membrane and the anterior chamber. If the reflection point is located at the anterior chamber, this will cause overestimation of the corneal thickness.
There are several limitations to this study including its modest size, also, enrolment of both eyes of each patient. The study would have greater statistical inference if we could include the right eye or left eye from the sample population. For post-LASIK eyes, our study was limited to those eyes with no complications. It will be more informative to include those eyes with post-LASIK haze as well as to record pre-LASIK refractive error and look at its relation with the variation in post-LASIK corneal thickness.
In conclusion, all the three devices correlate well with each other in normal and post-LASIK eyes. The three devices cannot be used interchangeably since there was statistically significant variation. Pentacam’s CCT measurements tend to be thicker than ultrasound pachymetry and noncontact specular microscope. We should be cautious when we use the Pentacam as pachymetry tool for refractive surgery screening since it tends to give significantly thicker reading than ultrasound pachymetry. We suggest that all patients with borderline Pentacam pachymetry reading should have their corneal thickness measured using ultrasound pachymetry. Further studies with greater sample size are needed to compare the corneal thickness using Pentacam and ultrasound before we can totally depend on Pentacam pachymetry for refractive surgery screening. The US pachymeter as the gold standard for pachymetry measurement deserve to be re-examined as many new pachymetry devices are giving different reading.
Conflict of interest
The authors do not have any commercial or proprietary interest in any product or company.
References
- Al-Mezaine H.S., Al-Amro S.A., Kangave D. Comparison between central corneal thickness measurements by oculus Pentacam and ultrasonic pachymetry. Int. Ophthalmol. 2008;28:333–338. doi: 10.1007/s10792-007-9143-9. [DOI] [PubMed] [Google Scholar]
- Amano S., Honda N., Amano Y. Comparison of central corneal thickness measurements by rotating Scheimpflug camera, ultrasonic pachymetry, and scanning-slit corneal topography. Ophthalmology. 2006;113:937–941. doi: 10.1016/j.ophtha.2006.01.063. [DOI] [PubMed] [Google Scholar]
- Avitabile T., Marano F., Uva M.G., Reibaldi A. Evaluation of central and peripheral corneal thickness with ultrasound biomicroscopy in normal and keratoconic eyes. Cornea. 1997;16:639–644. [PubMed] [Google Scholar]
- Barkana Y., Gerber Y., Elbaz U. Central corneal thickness measurement with the Pentacam Scheimpflug system, optical low-coherence reflectometry pachymeter, and ultrasound pachymetry. J. Cataract Refract. Surg. 2005;31:1729–1735. doi: 10.1016/j.jcrs.2005.03.058. [DOI] [PubMed] [Google Scholar]
- Bechmann M., Thiel M.J., Neubauer A.S. Central corneal thickness measurement with a retinal optical coherence tomography device versus standard ultrasonic pachymetry. Cornea. 2001;20:50–54. doi: 10.1097/00003226-200101000-00010. [DOI] [PubMed] [Google Scholar]
- Bovelle R., Kaufman S.C., Thompson H.W., Hamano H. Corneal thickness measurements with the Topcon SP-2000P specular microscope and an ultrasound pachymeter. Arch. Ophthalmol. 1999;117:868–870. doi: 10.1001/archopht.117.7.868. [DOI] [PubMed] [Google Scholar]
- Ciolino J.B., Khachikian S.S., Belin M.W. Comparison of corneal thickness measurements by ultrasound and Scheimpflug photography in eyes that have undergone laser in situ keratomileusis. Am. J. Ophthalmol. 2008;145:75–80. doi: 10.1016/j.ajo.2007.08.026. [DOI] [PubMed] [Google Scholar]
- Copt R.P., Thomas R., Mermoud A. Corneal thickness in ocular hypertension, primary open-angle glaucoma, and normal tension glaucoma. Arch. Ophthalmol. 1999;117:14–16. doi: 10.1001/archopht.117.1.14. [DOI] [PubMed] [Google Scholar]
- Fakhry M.A., Artola A., Belda J.I. Comparison of corneal pachymetry using ultrasound and Orbscan II. J. Cataract Refract. Surg. 2002;28:248–252. doi: 10.1016/s0886-3350(01)01277-9. [DOI] [PubMed] [Google Scholar]
- Fujioka M., Nakamura M., Tatsumi Y. Comparison of Pentacam Scheimpflug camera with ultrasound pachymetry and noncontact specular microscopy in measuring central corneal thickness. Curr. Eye Res. 2007;32:89–94. doi: 10.1080/02713680601115010. [DOI] [PubMed] [Google Scholar]
- Gunvant P., Broadway D.C., Watkins R.J. Repeatability and reproducibility of the BVI ultrasonic pachymeter. Eye. 2003;17:825–828. doi: 10.1038/sj.eye.6700485. [DOI] [PubMed] [Google Scholar]
- Insler M.S., Baumann J.D. Corneal thinning syndromes. Ann. Ophthalmol. 1986;18(2):74–75. [PubMed] [Google Scholar]
- Javaloy J., Vidal M.T., Villada J.R. Comparison of four corneal pachymetry techniques in corneal refractive surgery. J. Refract. Surg. 2004;20:29–34. doi: 10.3928/1081-597X-20040101-06. [DOI] [PubMed] [Google Scholar]
- Kawana K., Tokunaga T., Miyata K. Comparison of corneal thickness measurements using Orbscan II, non-contact specular microscopy, and ultrasonic pachymetry in eyes after laser in situ keratomileusis. Br. J. Ophthalmol. 2004;88:466–468. doi: 10.1136/bjo.2003.030361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khoramnia R., Rabsilber T.M., Auffarth G.U. Central and peripheral pachymetry measurements according to age using the Pentacam rotating Scheimpflug camera. J. Cataract Refract. Surg. 2007;33:830–836. doi: 10.1016/j.jcrs.2006.12.025. [DOI] [PubMed] [Google Scholar]
- Lackner B., Schmidinger G., Pieh S. Repeatability and reproducibility of central corneal thickness measurement with Pentacam, Orbscan, and ultrasound. Optom. Vis. Sci. 2005;82:892–899. doi: 10.1097/01.opx.0000180817.46312.0a. [DOI] [PubMed] [Google Scholar]
- Larsson L.I., Bourne W.M., Pach J.M., Brubaker R.F. Structure and function of the corneal endothelium in diabetes mellitus type I and type II. Arch. Ophthalmol. 1996;114:9–14. doi: 10.1001/archopht.1996.01100130007001. [DOI] [PubMed] [Google Scholar]
- Li H.F., Petroll W.M., Møller-Pedersen T. Epithelial and corneal thickness measurements by in vivo confocal microscopy through focusing (CMTF) Curr. Eye Res. 1997;16:214–221. doi: 10.1076/ceyr.16.3.214.15412. [DOI] [PubMed] [Google Scholar]
- Liu Z., Pflugfelder S.C. Corneal thickness is reduced in dry eye. Cornea. 1999;18:403–407. doi: 10.1097/00003226-199907000-00002. [DOI] [PubMed] [Google Scholar]
- Liu Z., Pflugfelder S.C. The effects of long-term contact lens wear on corneal thickness, curvature, and surface regularity. Ophthalmology. 2000;107:105–111. doi: 10.1016/s0161-6420(99)00027-5. [DOI] [PubMed] [Google Scholar]
- Maldonado M.J., Ruiz-Oblitas L., Munuera J.M. Optical coherence tomography evaluation of the corneal cap and stromal bed features after laser in situ keratomileusis for high myopia and astigmatism. Ophthalmology. 2000;107:81–87. doi: 10.1016/s0161-6420(99)00022-6. discussion 88. [DOI] [PubMed] [Google Scholar]
- Marsich M.M., Bullimore M.A. The repeatability of corneal thickness measures. Cornea. 2000;19:792–795. doi: 10.1097/00003226-200011000-00007. [DOI] [PubMed] [Google Scholar]
- Miglior S., Albe E., Guareschi M. Intraobserver and interobserver reproducibility in the evaluation of ultrasonic pachymetry measurements of central corneal thickness. Br. J. Ophthalmol. 2004;88:174–177. doi: 10.1136/bjo.2003.023416. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Modis L.J., Langenbucher A., Seitz B. Corneal thickness measurements with contact and noncontact specular microscopic and ultrasonic pachymeter. Am. J. Ophthalmol. 2001;132:517–521. doi: 10.1016/s0002-9394(01)01109-6. [DOI] [PubMed] [Google Scholar]
- Modis L., Jr., Langenbucher A., Seitz B. Scanning-slit and specular microscopic pachymetry in comparison with ultrasonic determination of corneal thickness. Cornea. 2001;20:711–714. doi: 10.1097/00003226-200110000-00008. [DOI] [PubMed] [Google Scholar]
- O’Donnell C., Maldonado-Codina C. Agreement and repeatability of central thickness measurement in normal corneas using ultrasound pachymetry and the OCULUS Pentacam. Cornea. 2005;24:920–924. doi: 10.1097/01.ico.0000157422.01146.e9. [DOI] [PubMed] [Google Scholar]
- Rainer G., Findl O., Petternel V. Central corneal thickness measurements with partial coherence interferometry, ultrasound, and the Orbscan system. Ophthalmology. 2004;111:875–879. doi: 10.1016/j.ophtha.2003.09.027. [DOI] [PubMed] [Google Scholar]
- Salz J.J., Azen S.P., Berstein J. Evaluation and comparison of sources of variability in the measurement of corneal thickness with ultrasonic and optical pachymeters. Ophthalmic Surg. 1983;14:750–754. [PubMed] [Google Scholar]
- Solomon O.D. Corneal stress test for extended wear. Clao J. 1996;22:75–78. [PubMed] [Google Scholar]
- Suzuki S., Oshika T., Oki K. Corneal thickness measurements: scanning-slit corneal topography and noncontact specular microscopy versus ultrasonic pachymetry. J. Cataract Refract. Surg. 2003;29:1313–1318. doi: 10.1016/s0886-3350(03)00123-8. [DOI] [PubMed] [Google Scholar]
- Swartz T., Marten L., Wang M. Measuring the cornea: the latest developments in corneal topography. Curr. Opin. Ophthalmol. 2007;18:325–333. doi: 10.1097/ICU.0b013e3281ca7121. [DOI] [PubMed] [Google Scholar]
- Tam E.S., Rootman D.S. Comparison of central corneal thickness measurements by specular microscopy, ultrasound pachymetry, and ultrasound biomicroscopy. J. Cataract Refract. Surg. 2003;29:179–1184. doi: 10.1016/s0886-3350(02)01921-1. [DOI] [PubMed] [Google Scholar]
- Ucakhan O.O., Ozkan M., Kanpolat A. Corneal thickness measurements in normal and keratoconic eyes: Pentacam comprehensive eye scanner versus noncontact specular microscopy and ultrasound pachymetry. J. Cataract Refract. Surg. 2006;32:970–977. doi: 10.1016/j.jcrs.2006.02.037. [DOI] [PubMed] [Google Scholar]
- Waring G.O., 3rd, Bourne W.M., Edelhauser H.F., Kenyon K.R. The corneal endothelium. Normal and pathologic structure and function. Ophthalmology. 1982;89:531–590. [PubMed] [Google Scholar]
- Wheeler N.C., Morantes C.M., Kristensen R.M. Reliability coefficients of three corneal pachymeters. Am. J. Ophthalmol. 1992;113:645–651. doi: 10.1016/s0002-9394(14)74788-9. [DOI] [PubMed] [Google Scholar]
- Zhao M.H., Zou J., Wang W.Q., Li J. Comparison of central corneal thickness as measured by non-contact specular microscopy and ultrasound pachymetry before and post LASIK. Clin. Exp. Ophthalmol. 2007;35:818–823. doi: 10.1111/j.1442-9071.2007.01633.x. [DOI] [PubMed] [Google Scholar]


