Abstract
In the past three decades, there have been countless advances in imaging modalities that have revolutionized evaluation, management, and treatment of neuro-ophthalmic disorders. Non-invasive approaches for early detection and monitoring of treatments have decreased morbidity and mortality. Understanding of basic methods of imaging techniques and choice of imaging modalities in cases encountered in neuro-ophthalmology clinic is critical for proper evaluation of patients. Two main imaging modalities that are often used are computed tomography (CT) and magnetic resonance imaging (MRI). However, variations of these modalities and appropriate location of imaging must be considered in each clinical scenario. In this article, we review and summarize the best neuroimaging studies for specific neuro-ophthalmic indications and the diagnostic radiographic findings for important clinical entities.
Keywords: Neuroophthalmology, Imaging, Magnetic resonance imaging, Computed tomography
Introduction
Advances in neuroimaging have revolutionized the evaluation, management, and treatment of neuro-ophthalmic disorders. Despite the ever-increasing resolution ability of modern neuroimaging technology, it remains critical that both the ordering eye physician and the interpreting radiologist communicate about the relevant topographical and localizing anatomy, the clinical and radiographic differential diagnosis, and the most likely, single best unifying diagnosis (i.e., “clinical correlation required”). In this paper, we review and summarize the best neuroimaging studies for specific neuro-ophthalmic indications and the diagnostic radiographic findings for important clinical entities.
Computed tomography
The computed tomography (CT) scan obtains image by conventional X-ray technology. The CT X-ray source moves around the patient and the X-ray detectors located on the opposite side of the X-ray source measure the amount of attenuation. Data points analyzed by a computer and attenuation values, in Hounsfield units, are assigned to each pixel, which are then compared to the attenuation value of water (zero) and reconstructed into an array of pixels forming images that we see on the computer screen. By convention, denser materials, such as bone, are displayed bright white, while less dense material, such as air, is displayed darker. Materials with densities between these values are displayed in a gray scale gradient. Iodinated contrast material can be used to improve the sensitivity and specificity of CT scan interpretation in many situations. However, in some situations, contrast material does not add any benefit (e.g., thyroid eye disease), diminishes the ability to detect the lesion of interest (e.g., acute hemorrhage), or might be contraindicated (e.g., iodine allergy).
Magnetic resonance imaging
In contrast to CT scan, which uses conventional X-ray technology, the imaging technique in magnetic resonance imaging (MRI) relies on the interaction of hydrogen atoms, mostly water, with the intense magnetic field generated by the MRI scanner. Thus, as opposed to CT, there is no radiation exposure with MRI. Certain atoms become polarized when subjected to a strong magnetic field, creating a net magnetic vector that is longitudinal to the direction of the magnetic field. Atoms that are misaligned to the magnetic field can be forced to align when they absorb a characteristic frequency (Larmor frequency) that is directly proportional to the strength of the magnetic field that is subjected. This energy is called excitation and it is re-emitted over time as the excited atoms move from the higher to the lower energy state. This process and energy release is known as relaxation.
The basic MRI sequences are T1 and T2 modes. Detailed discussion of the complex physics and the technical parameters of these methods are beyond the scope of this article, but a short and simple description of T1 and T2 might be of value to the ophthalmologist. On a T2 weighted scan, water and fluid containing tissues are bright and fat-containing tissues are dark, and on T1-weighted images, the fluid is dark and the fat is bright. Thus, the T2-weighted imaging is useful in detecting pathologic tissues that tend to develop edema and fluid that can be distinguished from normal tissue. However, the “brightness” of normal structures on T1- and T2-weighted imaging can make it more difficult to detect pathology. In a specialized T2-weighted sequence, fluid attenuated inversion recovery (FLAIR), the free water signal (e.g., in cerebrospinal fluid) can be attenuated and made dark, while water in edematous and pathologic tissue will remain bright. This is particularly useful in demyelinating disease such as multiple sclerosis, which we discuss later in this article. Likewise, in T1-weighted imaging, the normal fat signal is bright and can obscure both pathologic bright T1 signal and also gadolinium contrast enhancement of pathology in the fat-filled orbit. Thus, T1 post-contrast studies with fat suppression sequence of the orbits might be necessary to visualize orbital pathology (e.g., optic nerve sheath meningioma, intraorbital optic neuritis). In addition to fat-suppressed T1 and T2 FLAIR, additional special sequences might be of interest to the ophthalmologist such as diffusion weighted imaging (DWI) and apparent diffusion coefficient (ADC). Diffusion weighted MRI measures aberrancies in expected Brownian motion of free water. A frequent application for DWI/ADC is in acute ischemic strokes where increased restriction of water diffusion can differentiate acute ischemic cytotoxic edema from vasogenic edema. DWI/ADC imaging can show abnormalities within minutes of the onset of stroke symptoms (even before structural CT and conventional MRI show abnormalities) and may remain for up to two weeks. In MRI, gadolinium, as opposed to the iodinated contrast material of CT, is the contrast material. As in CT, however, the administration of gadolinium contrast material increases the sensitivity and specificity of imaging for neuro-ophthalmology and, in general, contrast material should be given for most clinical indications.
With this background information in mind, we will now discuss some specific clinical indications of interest to the ophthalmologist for which neuroimaging might be necessary.
Unilateral or bilateral optic neuropathy
In a patient with an unexplained unilateral or bilateral optic neuropathy (e.g., optic atrophy), a pre- and post-contrast magnetic resonance imaging (MRI) of the head and orbit might disclose a compressive, inflammatory, or infiltrative etiology. As noted above, fat has a very high signal intensity on the conventional T1-weighted MRI and suppression of the fat signal (i.e., fat suppression or fat saturation) is highly recommended for showing intraorbital lesions, especially any enhancing optic nerve (e.g., optic neuritis) or optic nerve sheath (e.g., sheath meningioma) lesions. Imaging along the intraorbital (i.e., MRI of orbit) and intracranial (i.e., MRI of brain) course of the optic nerve is essential to exclude an etiology in the setting of an unexplained optic neuropathy.
Optic neuritis
Acute demyelinating optic neuritis (ON) is a common consideration of acute to subacute painful (pain with eye movement) unilateral vision loss in young adults. Our recommended imaging modality to exclude demyelinating disease in ON is MRI with pre- and post-contrast fat suppression of the orbits to look for enhancement of the optic nerve (Fig. 1) and T2-weighted brain imaging for periventricular demyelinating lesions (including sagittal views of the corpus callosum). As noted above, cerebrospinal fluid (CSF) shows very high signal intensity on T2-weighted MRI and Fluid Attenuation Inversion Recovery (FLAIR) sequences can suppress the normal CSF bright signal on T2 and allow easier detection of demyelinating white matter lesions in ON.1,2 In the Optic Neuritis Treatment Trial (ONTT) patients with ON without demyelinating lesions in the brain have a 22% risk of multiple sclerosis (MS) versus a 78% risk of MS after 15 years with multiple white matter lesions.3 Thus, the MRI is prognostic (but not definitive) for the prediction of future MS in patients with ON.
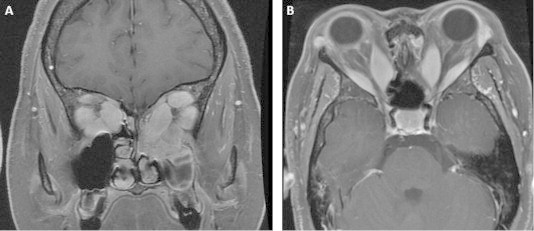
Figure 1.
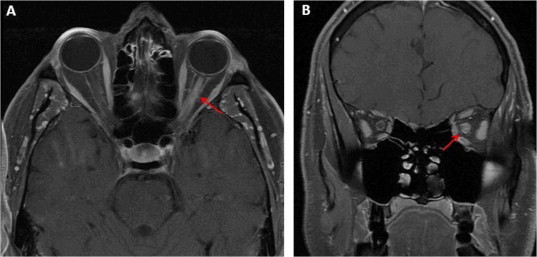
Axial (A) and coronal (B) views of T1 sequence post contrast fat suppression magnetic resonance imaging demonstrating post contrast enhancement of the left optic nerve (arrows).
Bitemporal hemianopsia
Bitemporal hemianopsia most commonly occurs as a result of lesions of the optic chiasm. Although compressive lesions are typical causes for a bitemporal hemianopsia, uncommonly, demyelinating (i.e., chiasmal neuritis) and inflammatory (e.g., sarcoid) lesions can occur and might demonstrate enlargement or enhancement in the chiasm on neuroimaging. Common tumors causing compression of the optic chiasm include pituitary adenoma, craniopharyngioma, meningioma, or dysgerminoma in adults and optic pathway glioma in children. In addition, internal carotid artery aneurysm can also present with sellar symptoms and signs. MRI of the sella with and without contrast can help to differentiate between these pathologies4 (Fig. 2). In the acute setting, CT scan of the sella might be useful for hemorrhage (e.g., pituitary apoplexy) and CT might also be useful for demonstrating calcification in a suprasellar lesion or hyperostosis of bone in meningioma.
Figure 2.
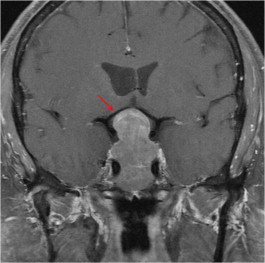
MRI of the sella in coronal image of post contrast T1 sequence shows pituitary macroadenoma compressing chiasm from below (arrow).
Homonymous hemianopsia (or cortical blindness)
Any type of intracranial lesion of the retrochiasmal visual pathways (i.e., lesions of the optic tract, the lateral geniculate nucleus, the optic radiations, and the occipital cortex) can cause a homonymous hemianopia. The preferred imaging study for homonymous hemianopsia is a cranial MRI with and without contrast with attention to the contralateral retrochiasmal pathway. Patients who present acutely (e.g., possible stroke) or who have high suspicion for intracranial hemorrhage (e.g., hemorrhagic stroke, pituitary apoplexy, ruptured aneurysm or arteriovenous malformation) might undergo an initial head CT scan without contrast. In general, however, even if the initial CT is negative, a follow up MRI is recommended for acute or chronic ischemic lesions producing a homonymous hemianopsia. Diffusion weighted imaging (DWI) is a special MR imaging technique that is very helpful to differentiate the various phases of cerebral infarction (e.g., hyperacute, acute, subacute or chronic) and, in conjunction with apparent diffusion coefficient technique (ADC), can demonstrate restricted diffusion consistent with ischemia. In the acute setting DWI and ADC MRI sequences can discriminate reversible vasogenic edema (bright signal on T2 and FLAIR, but no restricted diffusion on DWI/ADC), as seen in posterior reversible encephalopathy syndrome (PRES), from less reversible cytotoxic edema in ischemic stroke (bright signal on T2 and FLAIR with restricted diffusion on DWI/ADC). In vasogenic edema the diffusion of water molecules is increased, so the ADC is elevated and the DWI shows iso- or hypo-intense signal. In contrast, in cytotoxic edema the movement of water from the extracellular to the intracellular compartment produces restricted diffusion, so the ADC is decreased and the DWI appears hyperintense5–10 (Fig. 3). The clinical importance for the ophthalmologist is that DWI/ADC imaging of homonymous hemianopsia or cortical blindness in patients with PRES may be prognostic for recovery (i.e., the deficit is reversible), whereas ischemic infarction with restricted DWI/ADC might not recover.
Figure 3.
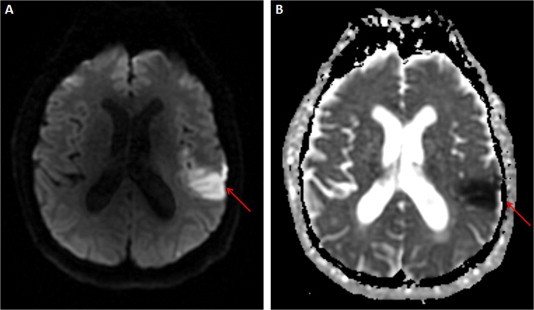
(A) Hyperintensity in DWI due to acute infarct in the left MCA distribution caused right homonymous hemianopsia (arrow). (B) Hypointensity in ADC due to acute infarct of left MCA distribution (arrow).
Cranial nerve palsy
Ocular motor cranial neuropathies (e.g., third, fourth, or sixth nerve palsy) typically are best imaged with cranial pre- and post-contrast MRI following the course of the involved nerve(s). Newer MRI sequences, such as CISS (constructive interference in steady-state) and FIESTA (fast imaging employing steady-state acquisition), have been deployed to better demonstrate the cranial nerves and might be particularly useful for smaller intrinsic lesions of the nerve (e.g., oculomotor nerve schwannoma).11 The sixth cranial nerve runs along the clivus to either side of the midline and CT scan, in conjunction with cranial MRI, might show any lesion involving bone or sinus disease better (Fig. 4).
Figure 4.
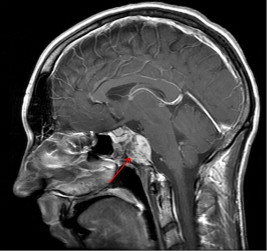
MRI of brain (sagittal, T1, post contrast) shows a clival chondroma (arrow) in a 29 year-old patient with a left 6th nerve palsy.
Although typically MRI is the superior imaging strategy for ocular motor cranial neuropathy, when a patient presents with an acute third nerve palsy (especially with pupil involvement) the most emergent diagnosis is a posterior communicating artery aneurysm. Patients may present with ptosis, anisocoria, diplopia and headache. Severe headache (e.g., “worst headache of my life”), nausea, and/or vomiting might indicate a ruptured aneurysm with subarachnoid hemorrhage. In this setting, the initial imaging modality of choice is typically an emergency non-contrast CT of the head to look for subarachnoid hemorrhage followed by a contrast computed tomography angiogram (CTA) for aneurysm. In many institutions, CTA offers faster and better results than MRA for detection of aneurysm, but the ordering clinician should discuss the pros and cons of each study with their institutional neuroradiologist in advance to design the best imaging strategy for third nerve palsy.
Nystagmus
Nystagmus is a rhythmic oscillating movement of the eyes.12 Brainstem imaging, typically with cranial MRI, is the best initial study for any unexplained nystagmus. Although most forms of nystagmus require brainstem imaging, a few types of nystagmus localize to other specific locations. For example, see-saw nystagmus may be seen in lesions that involve the midbrain or parasellar region (e.g., pituitary tumor or craniopharyngioma)13 and spasmus nutans in children might be associated with an optic pathway glioma. Downbeat nystagmus and periodic alternating nystagmus may be seen in disorders affecting the cervicomedullary junction14 (e.g., Arnold-Chiari malformation15, skull base tumors, spinocerebellar degenerations16 and toxic metabolic syndromes).17 Convergence retraction nystagmus may be seen in the setting of the dorsal midbrain syndrome.18 Oculopalatal myoclonus is a pendular vertical nystagmus associated with compromised pathway between the inferior olive, dentate nucleus of the cerebellum, and red nucleus due to olivary hypertrophy following stroke, multiple sclerosis, or head trauma.19,20 Thus, in general, pre- and post-contrast cranial MRI is the imaging study of choice for unexplained nystagmus.
Proptosis
Proptosis is a condition where the globe abnormally protrudes anteriorly. The most common cause of unilateral or bilateral proptosis in adults is thyroid ophthalmopathy.
Computed tomography (CT) and MRI of the orbit, without contrast, are both neuroimaging studies that can be used to make the diagnosis of thyroid eye disease (TED) (Fig. 5). Contrast is typically not necessary however because of the intrinsic contrast provided by fat in the orbit. In addition, for CT orbit iodinated contrast material might potentiate iodine-induced thyrotoxicosis. CT is also superior to MRI for evaluating sinus disease and for bone especially before and after orbital decompression in TED. Thus, our recommendation for TED is CT rather than MRI of the orbit. Other causes for proptosis include: orbital cellulitis, orbital inflammatory disease (e.g., idiopathic, Wegener granulomatosis, systemic lupus erythematosus) and neoplasm (e.g., meningioma, glioma, hemangioma21, lymphangioma22, metastasis, or lymphoma23). In children unilateral proptosis is commonly due to orbital cellulitis24 and subperiosteal abcess6, and in bilateral cases neuroblastoma25 and leukemia26 are the most likely causes. CT scan of the orbit is recommended for the initial evaluation of acute onset proptosis (Fig. 6A). CT is faster than an MRI and can be useful for defining orbital cellulitis, orbital abscess, idiopathic orbital inflammation, thyroid orbitopathy with compressive optic neuropathy or vision threatening proptosis, and post-surgical or spontaneous retrobulbar hemorrhage.27 For more chronic lesions, orbital fat-suppressed post-contrast MRI (Fig. 6B) may be required to obtain more detailed imaging of the lesion of interest.
Figure 5.
A 30 year old female with thyroid eye disease status post left orbital wall decompression. The T1 weighted MRI sequence of coronal (A) and axial (B) views show markedly enlarged extraocular muscles.
Figure 6.
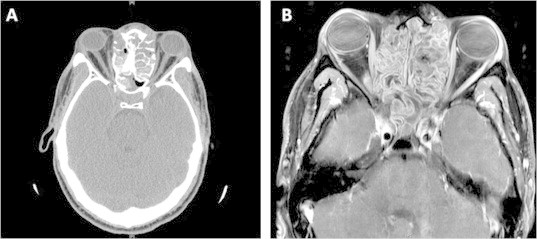
A 20 year old male with allergic fungal sinusitis with severe expansion of the ethmoid sinus pressing on the medial rectus and pushing the orbital content anteriorly. The CT scan (A) shows great details of the bony structure, while the T1sequence MRI with fat suppression (B) shows the great details of the soft tissue in orbit and sinus.
Horner’s syndrome
A Horner syndrome (HS) is characterized clinically by ipsilateral ptosis and miosis with anisocoria greater in the dark. HS can be divided into three types, depending on where the disruption lies along the oculosympathetic pathway: central, preganglionic and postganglionic.28
Central causes of HS are typically recognized based on the accompanying neurologic signs and symptoms that indicate involvement of the hypothalamus, brainstem or cervicothoracic spinal cord (e.g., ataxia, diplopia, hemisensory or hemimotor loss). Most commonly, central HS is of vascular etiology leading to lateral medullary syndrome, but other causes include tumors, trauma, demyelination, and arteriovenous malformations. MRI of the head and neck to the second thoracic vertebra (T2) with and without gadolinium is probably the single best mode of imaging for HS. In the acute setting, a painful HS is commonly caused by internal carotid artery (ICA) dissection (Fig. 7). A T1-weighted MRI of the neck with contrast and fat suppression, in addition to MR angiography (MRA) of the neck, might be diagnostic. The diagnostic MRI sign is a crescent of hyperintense signal intensity on T1 surrounding the typically hypointense normal carotid artery flow void. CT and CTA of the neck might also be diagnostic for a carotid dissection, has some advantages over conventional MRI and MRA of the neck, and at some institutions, may be the initial evaluation of choice in acute HS.
Figure 7.
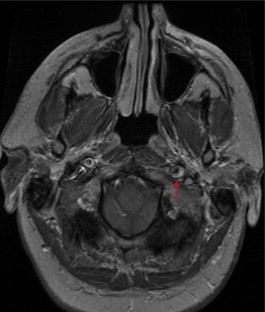
A 46 year old white male presenting with left ptosis and anisocoria from left Horner’s syndrome. Patient had left carotid artery dissection. T1 weighted sequence with contrast in axial view shows classic “crescent sign” (arrow) in distal portion of the left internal carotid artery.
Papilledema
Papilledema is optic disc swelling caused by an increased intracranial pressure. Patients usually present with headache, blurred vision, or diplopia (from a non-localizing sixth nerve palsy), or may even be asymptomatic. Although CT scan might be useful in acute or emergent setting, our definitive imaging recommendation for papilledema is MRI of the brain and orbits with and without contrast, with fat suppression of the orbit, and MRV of the head. The MRI might show an etiology for increased intracranial pressure including meningeal disease, hydrocephalus, or space-occupying lesions, or may show radiographic signs of idiopathic intracranial hypertension (IIH), such as an empty sella, fluid in the optic nerve sheath and posterior indentation of the globe. The MRV of the head might show sinus stenosis or venous sinus thrombosis.
Summary
Ophthalmologists should be aware of the specific clinical indications for CT and MRI in neuro-ophthalmology and be prepared to recognize the distinctive radiographic signs for each clinical entity (Table 1). In general, MRI is superior to CT scanning for most intracranial neuro-ophthalmic indications, but CT still has a role in cases of acute hemorrhage, hydrocephalus, bone pathology, trauma, orbital disease, sinus disease, thyroid eye disease and for those patients who are unable to undergo an MR scan. In addition, in some centers CTA may be superior to MRA for some vascular conditions (e.g., carotid dissection or arterial aneurysm). In most cases, contrast material for both CT and MR should be ordered for any neuro-ophthalmic indication unless there is a clear contraindication, but in some cases contrast may not be necessary (e.g., thyroid eye disease). Special MRI sequences of interest to ophthalmology include fat suppression, fluid-attenuated inversion recovery, and DWI/ADC. Finally, we cannot emphasize enough the critical importance for the ordering ophthalmologist to provide the interpreting radiologist with the pertinent clinical information, including the differential diagnosis and the suspected location of a lesion, to obtain the best neuroradiologic interpretation (i.e., “clinical correlation is required”).
Table 1.
Neuro-ophthalmologic indications and recommended imaging study. (modified from Lee et al27 with permission).
| Clinical indication | Preferred imaging study | Contrast material | Comment |
|---|---|---|---|
| Bilateral optic disc swelling | Magnetic resonance imaging (MRI) head with magnetic resonance venogram (MRV) Computed tomography (CT) scan might be first line study in emergent setting. | Yes | Consider concomitant contrast MRV to exclude venous sinus thrombosis, especially in atypical cases of pseudotumor cerebri who are thin, male, or elderly. |
| Transient monocular visual loss (amaurosis fugax) due to ischemia | Magnetic resonance angiogram (MRA) or computed tomography angiogram (CTA) of neck for carotid stenosis or dissection. | Depends on clinical situation | Carotid Doppler study might be first line and may still require follow up catheter angiography. |
| Demyelinating optic neuritis | MRI head and orbit | Yes (enhancing lesions suggest acute disease) | Fluid attenuated inversion recovery (FLAIR) to look for demyelinating white matter lesions. MRI has prognostic significance for development of multiple sclerosis. |
| Inflammatory, infiltrative, or compressive optic neuropathy | MRI head and orbit | Yes | Fat suppression to exclude intraorbital optic nerve enhancement CT is superior in traumatic optic neuropathy for canal fractures. |
| Bitemporal hemianopsia | MRI head (attention to chiasm and sella) | Yes | Consider CT of sella if an emergent scan is needed (e.g. pituitary or chiasmal apoplexy) or if imaging for calcification (e.g., meningioma or craniopharyngioma or aneurysm). |
| Homonymous hemianopsia | MRI head | Yes | Retrochiasmal pathway. Diffusion weighted imaging (DWI) may be useful if acute ischemic infarct or Posterior reversible encephalopathy syndrome (PRES). If structural imaging negative and organic loss consider functional imaging like positron emission tomography (PET) |
| Cortical visual loss or visual association cortex (e.g., cerebral achromatopsia, alexia, prosopagnosia, simultagnosia, optic ataxia, Balint’s syndrome) | MRI head | Yes | Retrochiasmal pathway. Consider DWI in ischemic infarct. If structural imaging negative and organic loss consider functional imaging (e.g., PET, Single photon emission computed tomography (SPECT), or MRI spectroscopy (MRS)). |
| Third, fourth, sixth nerve palsy or cavernous sinus syndrome. | MRI head with attention to the skull base. Isolated vasculopathic cranial neuropathies may not require initial imaging. | Yes | Rim calcification in aneurysm, calcification in tumors, and hyperostosis may be better seen on CT. |
| Nystagmus | MRI brainstem | Yes | Localize nystagmus. |
| Horner syndrome: preganglionic | MRI head and neck to second thoracic vertebra (T2) in chest with neck MRA | Yes | Rule out lateral medullary infarct, brachial plexus injury, apical lung neoplasm, carotid dissection, etc. |
| Horner syndrome: post-ganglionic | MRI head and neck to level of superior cervical ganglion (C4 level) with MRA neck | Yes | Rule out carotid dissection. Isolated post-ganglionic lesions are often benign. |
| Thyroid eye disease | CT or MRI of orbit | Iodinated contrast may interfere with evaluation and treatment of systemic thyroid disease. | Bone anatomy is better seen on a CT scan especially if orbital decompression is being considered. |
| Orbital cellulitis and orbital disease secondary to sinus disease | CT orbit and sinuses | Depends on clinical situation | MRI and/or CT with CTA may be useful adjunct to a CT alone; especially if possible concomitant cavernous sinus thrombosis is present. |
| Orbital tumor (e.g., proptosis or enophthalmos, gaze-evoked visual loss) | CT or MRI of orbit | Yes | Include head imaging if lesion could extend intracranially. MRI with contrast is superior at determining intracranial extent of primary optic nerve tumors (e.g., optic nerve glioma or sheath meningioma). CT scan may be superior if looking for hyperostosis or calcification. |
Footnotes
Peer review under responsibility of King Saud University
References
- 1.Gass A., Moseley I.F. The contribution of magnetic resonance imaging in the differential diagnosis of optic nerve damage. J Neurol Sci. 2000;172(Suppl 1):S17–S22. doi: 10.1016/s0022-510x(99)00272-5. [DOI] [PubMed] [Google Scholar]
- 2.Hickman S.J., Toosy A.T., Miszkiel K.A. Visual recovery following acute optic neuritis – a clinical, electrophysiological and magnetic resonance imaging study. J Neurol. 2004;251(8):996–1005. doi: 10.1007/s00415-004-0477-1. [DOI] [PubMed] [Google Scholar]
- 3.Beck R.W., Trobe J.D., Moke P.S. High- and low-risk profiles for the development of multiple sclerosis within 10 years after optic neuritis: experience of the optic neuritis treatment trial. Arch Ophthalmol. 2003;121(7):944–949. doi: 10.1001/archopht.121.7.944. [DOI] [PubMed] [Google Scholar]
- 4.Lee A.G., Hayman L.A., Ross A.W. Neuroimaging contrast agents in ophthalmology. Surv Ophthalmol. 2000;45(3):237–253. doi: 10.1016/s0039-6257(00)00152-1. [DOI] [PubMed] [Google Scholar]
- 5.Barboriak D.P. Imaging of brain tumors with diffusion-weighted and diffusion tensor MR imaging. Magn Reson Imaging Clin North Am. 2003;11(3):379–401. doi: 10.1016/s1064-9689(03)00065-5. [DOI] [PubMed] [Google Scholar]
- 6.Gregory D.G., Pelak V.S., Bennett J.L. Diffusion-weighted magnetic resonance imaging and the evaluation of cortical blindness in preeclampsia. Surv Ophthalmol. 2003;48(6):647–650. doi: 10.1016/j.survophthal.2003.08.008. [DOI] [PubMed] [Google Scholar]
- 7.Kolb S.J., Costello F., Lee A.G. Distinguishing ischemic stroke from the stroke-like lesions of MELAS using apparent diffusion coefficient mapping. J Neurol Sci. 2003;216(1):11–15. doi: 10.1016/s0022-510x(03)00218-1. [DOI] [PubMed] [Google Scholar]
- 8.Romano A., Bozzao A., Bonamini M. Diffusion-weighted MR imaging: clinical applications in neuroradiology. Radiol Med. 2003;106(5–6):521–548. [PubMed] [Google Scholar]
- 9.Stadnik T.W., Demaerel P., Luypaert R.R. Imaging tutorial: differential diagnosis of bright lesions on diffusion-weighted MR images. Radiographics. 2003;23(1):e7. doi: 10.1148/rg.e7. [DOI] [PubMed] [Google Scholar]
- 10.Valentini V., Gaudino S., Spagnolo P. Diffusion and perfusion MR imaging. Rays. 2003;28(1):29–43. [PubMed] [Google Scholar]
- 11.Glenn L.W. Innovations in neuroimaging of skull base pathology. Otolaryngol Clin North Am. 2005;38(4):613–629. doi: 10.1016/j.otc.2005.03.007. [DOI] [PubMed] [Google Scholar]
- 12.Troost B.T. Nystagmus: a clinical review. Rev Neurol (Paris) 1989;145(6–7):417–428. [PubMed] [Google Scholar]
- 13.Kanter D.S., Ruff R.L., Leigh R.J., Modic M. See-saw nystagmus and brainstem infarction: MRI findings. Neuroophthalmology. 1987;7(5):279–283. doi: 10.3109/01658108708996003. [DOI] [PubMed] [Google Scholar]
- 14.Biller J., Pagano R.J. Downbeat nystagmus and pathology at cervicomedullary junction. Neurology. 1981;31(6):781. doi: 10.1212/wnl.31.6.781. [DOI] [PubMed] [Google Scholar]
- 15.Lyall D.A., Martinek K., Koshy Z. Downbeat nystagmus as the sole sign of Chiari malformation in goldenhar syndrome. J Pediatr Ophthalmol Strabismus. 2010;47(1):61–62. doi: 10.3928/01913913-20100106-15. [DOI] [PubMed] [Google Scholar]
- 16.Castillo L.C., Gracia F., Roman G.C. Spinocerebellar syndrome in patients infected with human T-lymphotropic virus types I and II (HTLV-I/HTLV-II): report of 3 cases from Panama. Acta Neurol Scand. 2000;101(6):405–412. doi: 10.1034/j.1600-0404.2000.80180.x. [DOI] [PubMed] [Google Scholar]
- 17.Hogie M., Guerbet M., Reber A. The toxic effects of toluene on the optokinetic nystagmus in pigmented rats. Ecotoxicol Environ Safety. 2009;72(3):872–878. doi: 10.1016/j.ecoenv.2008.02.016. [DOI] [PubMed] [Google Scholar]
- 18.Sato Y., Maehara F., Utsunomiya H. Convergence and retraction nystagmus in hydrocephalus due to shunt malfunction. Kurume Med J. 1983;30(4):125–128. doi: 10.2739/kurumemedj.30.125. [DOI] [PubMed] [Google Scholar]
- 19.Talks S.J., Elston J.S. Oculopalatal myoclonus: eye movement studies, MRI findings and the difficulty of treatment. Eye (Lond) 1997;11(Pt 1):19–24. doi: 10.1038/eye.1997.4. [DOI] [PubMed] [Google Scholar]
- 20.Lopez L.I., Gresty M.A., Bronstein A.M. Acquired pendular nystagmus: oculomotor and MRI findings. Acta Otolaryngol Suppl. 1995;520(Pt 2):285–287. doi: 10.3109/00016489509125250. [DOI] [PubMed] [Google Scholar]
- 21.Yan J., Wang X. Cavernous hemangioma with rapidly developing proptosis. Int Ophthalmol. 2008;28(2):125–126. doi: 10.1007/s10792-007-9115-0. [DOI] [PubMed] [Google Scholar]
- 22.Hsuan J., Malhotra R., Davis G., Selva D. Orbital decompression for gross proptosis associated with orbital lymphangioma. Ophthal Plast Reconstr Surg. 2004;20(6):463–465. doi: 10.1097/01.iop.0000144790.78416.e7. [DOI] [PubMed] [Google Scholar]
- 23.Vincenti D., Orofino N., Ferrario A. Unilateral exophthalmos and multiple subcutaneous nodules as a result of extranodal marginal zone lymphoma. J Clin Oncol. 2012;30(6):e69–e73. doi: 10.1200/JCO.2011.38.4131. [DOI] [PubMed] [Google Scholar]
- 24.Ho C.F., Huang Y.C., Wang C.J. Clinical analysis of computed tomography-staged orbital cellulitis in children. J Microbiol Immunol Infect. 2007;40(6):518–524. [PubMed] [Google Scholar]
- 25.Cox R.A. Proptosis due to neuroblastoma of the adrenal cortex; Hutchinson’s syndrome; report of a case. Arch Ophthal. 1948;39(6):731–738. doi: 10.1001/archopht.1948.00900020741002. [DOI] [PubMed] [Google Scholar]
- 26.Swinnen S., van Heerden J., Uyttebroeck A. A child with bilateral proptosis: a sign of acute myeloid leukemia? J Pediatr Hematol Oncol. 2012;34(1):35–37. doi: 10.1097/MPH.0b013e3182099302. [DOI] [PubMed] [Google Scholar]
- 27.Lee A.G., Johnson M.C., Policeni B.A., Smoker W.R. Imaging for neuro-ophthalmic and orbital disease – a review. Clin Experiment Ophthalmol. 2009;37(1):30–53. doi: 10.1111/j.1442-9071.2008.01822.x. [DOI] [PubMed] [Google Scholar]
- 28.George A., Haydar A.A., Adams W.M. Imaging of Horner’s syndrome. Clin Radiol. 2008;63(5):499–505. doi: 10.1016/j.crad.2007.12.006. [DOI] [PubMed] [Google Scholar]



