Abstract
The lateral orbital wall is the strongest among other orbital walls. However, it is commonly fractured in the setting of severe facial trauma. The fracture usually occurs at the sphenozygomatic suture line. In general, patients with lateral wall fractures are commonly young male who may present with mid facial swelling and some degree of deformity. In some cases, lateral orbital wall fracture may be associated with visual loss or change in mental status due to associated intracranial injury. Imaging studies with computed tomography is important in the proper diagnosis and planning of the surgical intervention. Management of intracranial or eye injuries should be undertaken on emergent basis. Thereafter, significantly displaced lateral wall fractures need to be repaired on timely basis. Proper realignment of the plane of the lateral orbital wall at the sphenozygomatic suture along with the other complex articulations of the zygomatic bone is necessary for proper functional and aesthetic outcome.
Keywords: Lateral orbital wall, Fracture, Eye injury, Vision loss, Diagnosis, Management
1. Introduction
Lateral orbital wall fractures are commonly seen with zygomatic malar complex (ZMC) fractures. Lateral orbital wall fractures most frequently occur as a result of road traffic accidents followed by assault, work and sport accidents (Cerulli et al., 2002). In elderly patients, falls are the most common cause (Rehman and Edmondson, 2002). This type of fractures are more frequent in young males and uncommon in children (Ferreira et al., 2004). In the setting of severe facial trauma, lateral orbital wall fracture should be suspected. Imaging studies need to be carried out for diagnostic and management purpose.
1.1. Anatomical consideration
Lateral orbital wall is formed anteriorly by zygomatic bone which manifests itself a prominent anatomic position in the mid face. As such it makes it highly susceptible to external traumas. The greater wing of the sphenoid forms posterior part of the lateral orbital wall along with anterior corner of the middle cranial fossa and the lateral border of orbital fissures. Fracture through the greater wing of the sphenoid is fortunately rare (Unger et al., 1990). Articulation between the zygomatic bone and the great wing of sphenoid is broad. This articulation is the commonest site for lateral orbital wall fractures, which are usually accompanied by disruption of zygomatic bone articulations with the frontal bone, temporal bone, maxillary bone.
1.2. Patient presentation
Patients with lateral orbital wall fractures usually present with periorbital swelling and ecchymosis along with variable degrees of mid facial deformity. A displaced lateral orbital wall has a dramatic effect on the globe position and facial asymmetry. As lateral orbital rim is position approximately at the equator of the globe, inferolateral displacement of the lateral orbital wall will lead to more significant change in the globe position than a simple blow-out floor fracture.
Fortunately, intracranial injury and visual loss rarely occur with isolated lateral orbital wall fracture. However, with the increase in the severity and posterior displacement of the lateral orbital wall fracture, the risk of the life-threatening intracranial injuries, injury to the orbital portion of the cranial nerves, and rupture globe increases. Blindness is a rare complication of facial fracture with reported incidence of 3% (Stanley et al., 1998). Visual loss may occur due to globe injury or injury to optic nerve. Indirect injury to the intracanalicular portion of the optic is most common mechanism of optic nerve related visual loss (Holt and Holt, 1983). Retrobullbar hemorrhage, penetrating foreign body and bony fragment impinging on the optic nerve are other causes of optic nerve injury.
Along with the clinical assessment, orbital computed tomography (CT) plays an important role in diagnosing and determining the extent of the lateral orbital wall fracture. It provides the surgeon with good hints for planning the reduction of the fracture. Management of lateral orbital wall fracture is directed toward early detection and emergent treatment of associated intracranial and eye injuries. This is followed by reduction of significantly displaced lateral orbital wall detected during clinical and radiological assessment.
2. Clinical evaluation
Facial trauma may be associated with life threatening injuries. Once the patient’s general condition is stable, a detailed history regarding the type and the severity of the trauma should be obtained. Careful evaluation should be directed to role out injury to the globe and intracranial trauma. Injury to the globe has been reported in up to 30% of orbital fractures (Koo et al., 2007). In the awake patient, inquiring about vision loss, double vision, and the presence of eye pain will help in the ophthalmic assessment. The patient may have numbness of the forehead and/or cheek. The patient may also have pain with opening the mouth (trismus). A review of patient’s past ocular and medical history is important. Currently many surgeons do not routinely use sutures to close clear corneal incisions after uncomplicated cataract surgery. One should be aware that such wounds are not healed fully even after several months following their surgery. Chronic medical conditions affecting the soft tissue and bone healing such as diabetes mellitus and smoking should be noted and considered during surgical planning.
Accurate visual acuity assessment should be performed at the initial examination of the patient (Fig. 1). Pupillary examination is very useful especially in uncooperative and unconscious patients. Pupils need to be examined for both relative afferent pupillary defect and efferent pupillary defect. When the light is directed to one pupil and then quickly switched to the other, both pupils constrict equally without evidence of pupillary re-dilation. Since light in one pupil causes both pupils to constrict, quickly switching from one eye to the other will give a “relative” indication of the functioning of optic nerves. The light can be switched back and forth between the two pupils till proper pupillary evaluation is achieved. In relative afferent pupillary defect, both pupils constrict equally when the light is directed into the unaffected pupil. However, the affected pupil dilates after the light stimulus is moved from the unaffected eye to the affected one which indicates injury to optic nerve (afferent limb of pupil reflex) in the affected eye. In efferent pupillary defect, the affected pupil dilates and the unaffected pupil constricts when the light is shined into the unaffected pupil. When the light stimulus is moved from the unaffected eye to the affected one, the affected pupil will continue being dilated and the unaffected pupil will continue being constricted. This indicates injury to oculomotor nerve (efferent limb of pupillary reflex) or traumatic injury to pupillary muscle of the affected eye.
Figure 1.
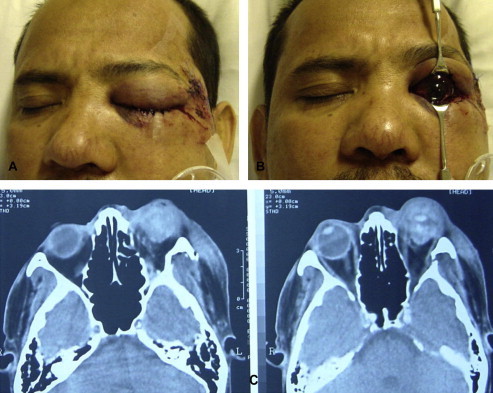
External photograph of a 32-years-old male who suffered a severe left sided facial trauma. Patient was referred after repair of his facial skin lacerations. The patient had complete loss of vision from his left eye along with proptosis and inability to mobilize his left eye (A, B). Axial CT-scan revealed evidence of blow-in fracture of his lateral orbital wall (C).
(Courtesy of Imtiaz A. Chaudhry, MD PhD FACS, King Khaled Eye Specialist Hospital)
Measurement of intraocular pressure, slit-lamp, and dilated fundus examination are important parts of evaluation to asses open globe injury. If the patient comes with proptosis, retrobulbar hemorrhage must be considered and emergent canthotomy and cantholysis should be done to lower the orbital pressure if there is any evidence of optic nerve compression. Ocular motility disturbance may present with orbital wall fractures. In the absence of open globe trauma, forced duction test needs to be performed to exclude extraocular muscle entrapment. However, oculomotor nerve injury or contusion of the muscles should be considered in the setting of impaired ocular motility.
Patients with facial trauma usually present with significant soft tissue swelling and may be associated with superficial lacerations. Displaced lateral wall fracture causes recession of the malar eminence and lateral canthal dystopia (Fig. 2). Presence of point tenderness and boney step off should be evaluated with palpation of the orbital rim. Enophthalmos and hypoglobus may be noted at initial presentation. Hertel exophthalmometer may give inaccurate reading with displaced lateral orbital rim about the eye position. Naugle orbitometer is a good alternative in the presence of intact inferior orbital rim since it rests on the superior and inferior orbital rims (Shere et al., 2004). Clinical photographs are important parts of the evaluation (Box 1).
Figure 2.

Left malar recession, and lateral canthal dystopia in young male with displaced lateral wall fracture. The patient had left subconjunctival hemorrhage and eyelids ecchymosis.
Box 1. Examination chart for patients with suspected orbital fracture.
-
–
Vision Assessment
-
–Pupil Exam
-
•Size and shape
-
•Relative afferent pupillary defect (RAPD)
-
•Efferent pupillary defect
-
•
-
–External Eye Exam
-
•Conjunctival hemorrhage, chemosis, laceration
-
•Corneal laceration, epithelial defect
-
•Scleral laceration
-
•Ocular motility, force duction test
-
•
-
–
Intraocular pressure
-
–
Dilated Fundus Exam
-
–External Facial and Periorbital Exam
-
•Ecchymoses, swelling
-
•Lacerations
-
•Enophthalmos, proptosis, lateral canthal dystopia
-
•Palpation for step deformity and subcutaneous emphysema
-
•V2 sensation
-
•Trismus
-
•
3. Imaging
Axial and coronal CT is the gold standard for evaluation of orbital fractures. The Classic ZMC fracture occurs through the sphenozygomatic suture. This suture represents a broad articulation between the two bones and provides a good estimation of the degree of displacement of the lateral wall fracture. ZMC fracture is accompanied with disruption of zygomaticofrontal suture, infraorbital rim, zygomaticomaxillary buttress, and zygomatic arch. Axial CT-scan cuts provide valuable information about the degree of comminution and displacement of ZMC, the gaps along the zygomatic bone articulations and medial orbital walls. Beside their importance in assessing the latera orbital wall and ZMC, coronal orbital CT-scan cuts are quite helpful to assess the orbital floor and roof walls for the presence of fractures and the need to address theses fracture during the surgical repair (Fig. 3A and B). Careful evaluation of the sphenoid bone and optic canal should be done to rule out fractures, signs of compression on the optic nerve, and presence of intracranial injury from lateral wall displacement (Blessmann et al., 2007) (Fig. 4A and B).
Figure 3.
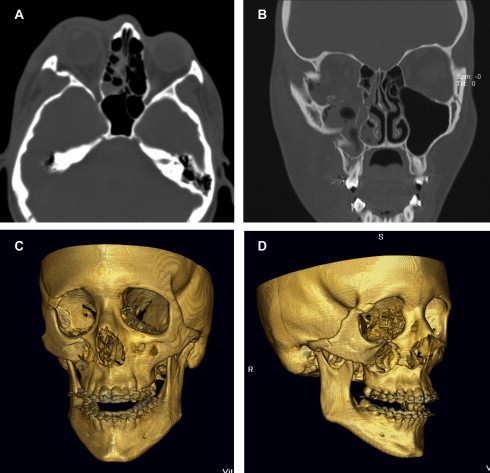
(A) CT axial bone window demonstrating fracture across zygomatic and outward displacement of the right lateral orbital wall. Coronal bone window orbital CT (B) showing the significant displacement of the fractured right lateral orbital wall and zygomatic malar complex (ZMC) along with large right orbital floor defect and maxillary sinus wall fracture. Three-dimensional CT-scans nicely illustrating the right ZMC and lateral wall fracture for the same patient (C) and (D).
Figure 4.

(A) CT axial bone window showing fracture across the left greater wing of the sphenoid with intracranial extension. (B) CT axial soft tissue window demonstrating impinging of the displaced left lateral wall in the lateral rectus muscle. The patient’s vision and motility were normal in the left side.
Three-dimensional CT-scan facilitates evaluation of patients with facial trauma by displaying the spatial orientation of the bone fragments and fracture gaps (Tsai et al., 2005). It gives a three dimensional picture of the change in bony orbital shape in the traumatized side compared with the normal side which facilitates preoperative planning and intraoperative reduction (Fig. 3C and D). Three-dimensional CT-scan provides an excellent tool to educate residents, patients and family members about the fracture and its management.
Displacement along the fractured lateral orbital wall is variable. Depending on the extent of the displacement on orbital imaging, lateral orbital wall fractures can be classified into four types (Unger et al., 1990). In type I fractures, the frontal process of the zygoma is wedged into the orbit between the globe and greater sphenoid wing. In type II fractures, the frontal process of the zygoma is displaced into the temporal fossa, and the orbital plate of the greater wing of the sphenoid bone is fractured free and pushed into the orbit as a “blow-in” fracture. Type III fractures are more severe with the entire greater wing of the sphenoid bone impacting toward the orbital apex, with possible intrusion into the middle cranial fossa. Type IV fractures extend posteriorly where the greater wing is displaced across the orbital apex, with fracture of the optic canal.
4. Management
Most patients with isolated lateral wall fracture come walking to the emergency room. However, life threatening conditions may result from associated traumatic injuries. Once vital signs are stabilized, eyes are examined for the presence of any injury. Repair of open globe injury takes priority over the repair of facial fractures. In these settings, fracture repair can be delayed for several days. If the intraocular pressure is high, a bedside lateral canthotomy and cantholysis may need to be performed emergently to decrease the orbital pressure. If intraocular pressure can not be measured, but there is decrease in vision and the orbit appears to be tight, a lateral canthotomy and cantholysis should be performed. Surgical evacuation of orbital hemorrhage may be indicated if the orbit continues to be tight. If the displaced lateral wall fracture impinges on the orbital part of the optic nerve and compromises its function, urgent reduction of the fracture may be indicated to restore the nerve function and reverse the visual loss (Unger et al., 1990). Management of traumatic optic neuropathy due to indirect insult to the intracanalicular portion of the optic nerve is controversial. These patients may benefit from optic canal decompression or megadose steroid therapy if there is no contraindication (Czerwinski and Lee, 2006).
The management of the lateral orbital wall fracture depends on the degree of displacement and comminution of the fracture, intracranial extension of sphenoid fracture. Non-displaced or mildly displaced fracture may be managed conservatively without surgical repair. If the displaced lateral wall fracture causes visual loss, ocular motility disturbance, enophthalmos or flattening of the malar eminence, fracture repair is indicated. Before resorting to the repair of the fracture, pre-existing corneal incision wounds need to be evaluated for their possible leak during the operation. Although intraocular pressure has been found not to be changed significantly during repair of zygomatic fracture (Dolynchuk et al., 1996), aqueous fluid may leak through the unsecured corneal wounds leading to collapse of the eye globe. Adding corneal suture to the unsecured corneal wounds may be required in these situations. Prior to the surgery, forced duction test should be performed if muscle entrapment is suspected.
Fracture repair requires good exposure, proper reduction and securing of the fracture in the reduced position with plates and screws. To expose the fracture sites pre-existing skin laceration or hidden incisions should be utilized as much as possible. Inferior orbital rim can be exposed though either transconjunctival or subciliary skin incision of the lower lid. Exposure of zygomaticofrontal suture can be obtained by lateral upper eyelid crease incision, extension of canthotomy incision or direct lateral brow incision. Trans-mucosal incision in the gingivobucuccal sulcus provides a decent exposure of zygomaticomaxillary buttress. For sphenoid fracture with dislocation of sphenotemporal buttress, significantly comminuted zygomatic complex fracture or panfacial fracture coronal or temporal incision is usually needed (Murray and O’Sullivan, 2007). Once the fracture is well exposed, mobilization and reduction of zygomatic bone can be achieved by inserting an elevator intraorally underneath the posterior aspect of the zygomatic bone. Force is then applied to mobilize the zygoma slowly to gain the proper alignment. T-bar screw is another good way of mobilizing the zygomatic bone (Bilyk and Joseph, 1994). It has a broad horizontal handle to facilitate manipulation and rotation of the zygoma in all direction after drilling an opening in the body of zygoma and firmly embedding the screw in the opening. Use of towel clips, hemostats and clamps may help in the reduction of fracture. Fracture of the great wing of the sphenoid with medial displacement can be reduced after exposure of the lateral wall and reduction of the zygomatic bone (Zhang et al., 2006). Free floating bone fragment from the fracture sphenoid bone may be removed if it is not possible to have it reduced in proper anatomical position. Craniotomy may be needed to reduce the sphenoid fracture associated with dislocation of the sphenotemporal suture and intracranial extension especially near the superior orbital fissure and optic canal (Unger et al., 1990). Displaced fracture across the great wing of the sphenoid bone not causing brain or cranial nerves injury does not need surgical intervention and usually heals without visible deformity (Dolynchuk et al., 1996). If needed, extracranial osteotomy of the sphenozygomatic interface for safe mobilization and aesthetic reduction of the displaced malar eminence can be offered (Czerwinski and Lee, 2006).
Once reduction of zygomatic bone with proper alignment of sphenozygomatic suture, inferior orbital rim, and frontozygomatic suture is achieved, rigid internal fixation is done to maintain the reduction of the fracture. Evaluation of the sphenozygomatic suture alignment necessitates proper visualization of greater wing of the sphenoid which has good stability and broad articulation with zygomatic bone. For non-comminuted fractures, 2-point fixation with rigid titanium miniplate along the inferior orbital rim and frontozygomatic suture may be sufficient (Bilyk and Joseph, 1994). With the increase in comminalty of the zygomatic fracture, additional fixation along the maxillary buttress is usually needed. Reduction and fixation of the zygomatic arch is usually required for very severe comminuted fracture (Murray and O’Sullivan, 2007). Resorbable plates and screws have been found to be effective especially in children with growing facial bones (Chang et al., 2005; Yoshioka et al., 1999).
During repair of the fracture, it is very important to gently handle soft tissue. Using natural plan in dissection such as preseptal dissection of the lower lid to expose the inferior orbital rim decrease the scaring and risk for lid retraction. Wide enough incisions help decrease excessive traction and damaging of the soft tissue. Soft tissue suspension with sutures and closing the periosteum after fixation of the fracture helps maintaining the facial symmetry (Eppley, 2005).
5. Complications
Enophthalmos is one of the main consequences of delayed or inadequate reduction of the ZMC fracture. Enophthalmos is more likely in patients with multiple traumas compared with patients with localized orbital trauma (Bell and Kindsfater, 2006). It is easier to manage enophthalmos shortly after trauma. With time, scaring, bone resorption and malunion of the fracture makes the management more complicated (Patel and Hoffmann, 1998). With the swelling from the injury and operation, the globe in the operated side should project more anteriorly compared with the other side. Post operative enophthalmos is likely to occur if the projection of both globes is symmetrical. Inadequate repair of zygomatic complex fracture can be prevented by good exposure of the lateral orbital wall to assure realignment of sphenozygomatic suture along with alignment of inferior orbital rim, and frontozygomatic suture. Failure to address the associated fracture of the orbital floor and medial wall is another cause of post operative enophthalmos. Loss of malar projection and globe dystopia are other consequences of delayed or inadequate repair of zygomatic complex fracture. Osteotomies to mobilize the zygoma, contour restoration, or both can be used to correct the consequences of delayed or inadequate repair of zygomatic complex fracture. Contour restoration can be performed with onlay grafting or alloplastic implants (Seider et al., 2007).
Most of the time spontaneous improvement of the muscle’s function occurs after lateral orbital wall fracture repair and reduction of the bone fragment causing muscle dysfunction. However, muscle surgery needs to be considered 4–6 months later if the patient continues to have diplopia. Lower lid retraction may occur with displaced zygomatic fracture and improves after reduction of the fracture. However, postoperative lid retraction may develop after exposure of inferior orbital rim through lower lid incision. It is thought to occur more after transcutaneous approach compared with transconjunctival approach (Eski et al., 2007). Massage of the lower lid during the early postoperative period may improve the retraction. If the lid retraction continues to be significant with corneal exposure, surgery may be indicated to release the scaring of the orbital septum along with local steroid injection. In severe cases, placement of graft material such as hard palat graft to lengthening the posterior lamella may be considered. If lateral canthotomy and inferior cantholysis have been performed for providing good exposure of the fracture site, simple reattachment of the lower lid with upper lid may be enough. However, fixation of the lower lid to the periosteum of the inner aspect of the lateral rim with help of small curved needle is preferred to maintain the lower lid in good position.
Although it is very rare, visual loss may occur with lateral orbital wall fracture repair (Becelli et al., 2000). Careful manipulation of bone fragment near by the optic nerve and close observation of development of postoperative retrobulbar hemorrhage should be carried out. If orbital implant is used, proper placement away from the optic nerve must be assured.
Acknowledgment
The author would like to thank Dr. Jeffrey A. Nerad for his great help in preparing the manuscript and providing some of the figures for this article.
References
- Becelli R., Renzi G., Perugini M., Iannetti G. Craniofacial traumas: immediate and delayed treatment. J. Craniofac. Surg. 2000;11:265–269. doi: 10.1097/00001665-200011030-00012. [DOI] [PubMed] [Google Scholar]
- Bell R.B., Kindsfater C.S. The use of biodegradable plates and screws to stabilize facial fractures. J. Oral. Maxillofac. Surg. 2006;64:31–39. doi: 10.1016/j.joms.2005.09.010. [DOI] [PubMed] [Google Scholar]
- Bilyk J.R., Joseph M.P. Traumatic optic neuropathy. Semin. Ophthalmol. 1994;9:200–211. doi: 10.3109/08820539409060016. [DOI] [PubMed] [Google Scholar]
- Blessmann M., Pohlenz P., Blake F.A. Validation of a new training tool for ultrasound as a diagnostic modality in suspected midfacial fractures. Int. J. Oral Maxillofac. Surg. 2007;36:501–506. doi: 10.1016/j.ijom.2007.01.016. [DOI] [PubMed] [Google Scholar]
- Cerulli G., Carboni A., Mercurio A. Soccer-related craniomaxillofacial injuries. J. Craniofac. Surg. 2002;13:627–630. doi: 10.1097/00001665-200209000-00006. [DOI] [PubMed] [Google Scholar]
- Chang E.L., Hatton M.P., Bernardino C.R., Rubin P.A. Simplified repair of zygomatic fractures through a transconjunctival approach. Ophthalmology. 2005;112:1302–1309. doi: 10.1016/j.ophtha.2005.01.053. [DOI] [PubMed] [Google Scholar]
- Czerwinski M., Lee C. Intracranial extension of a zygoma fracture: benefits of selective repair. Plast. Reconstr. Surg. 2006;118:10e–13e. doi: 10.1097/01.prs.0000220879.38096.c9. [DOI] [PubMed] [Google Scholar]
- Dolynchuk K.N., Tadjalli H.E., Manson P.N. Orbital volumetric analysis: clinical application in orbitozygomatic complex injuries. J. Craniomaxillofac. Trauma. 1996;2:56–63. [PubMed] [Google Scholar]
- Eppley B.L. Use of resorbable plates and screws in pediatric facial fractures. J. Oral. Maxillofac. Surg. 2005;63:385–391. doi: 10.1016/j.joms.2004.11.011. [DOI] [PubMed] [Google Scholar]
- Eski M., Sengezer M., Turegun M. Contour restoration of the secondary deformities of zygomaticoorbital fractures with porous polyethylene implant. J. Craniofac. Surg. 2007;18:520–525. doi: 10.1097/scs.0b013e318053432c. [DOI] [PubMed] [Google Scholar]
- Ferreira P., Marques M., Pinho C. Midfacial fractures in children and adolescents: a review of 492 cases. Br. J. Oral Maxillofac. Surg. 2004;42:501–505. doi: 10.1016/j.bjoms.2004.06.006. [DOI] [PubMed] [Google Scholar]
- Holt G.R., Holt J.E. Incidence of eye injuries in facial fractures: an analysis of 727 cases. Otolaryngol. Head Neck Surg. 1983;91:276–279. doi: 10.1177/019459988309100313. [DOI] [PubMed] [Google Scholar]
- Koo L., Hatton M.P., Rubin P.A. Traumatic blindness after a displaced lateral orbital wall fracture. J. Trauma. 2007;62:1288–1289. doi: 10.1097/01.ta.0000235292.16125.fa. [DOI] [PubMed] [Google Scholar]
- Murray D.J., O’Sullivan S.T. Intraocular pressure variations during zygomatic fracture reduction and fixation: a clinical study. Plast. Reconstr. Surg. 2007;120:746–752. doi: 10.1097/01.prs.0000270845.82498.3b. [DOI] [PubMed] [Google Scholar]
- Patel B.C., Hoffmann J. Management of complex orbital fractures. Facial Plast. Surg. 1998;14:83–104. doi: 10.1055/s-0028-1085305. [DOI] [PubMed] [Google Scholar]
- Rehman K., Edmondson H. The causes and consequences of maxillofacial injuries in elderly people. Gerodontology. 2002;19:60–64. doi: 10.1111/j.1741-2358.2002.00060.x. [DOI] [PubMed] [Google Scholar]
- Seider N., Gilboa M., Miller B. Orbital fractures complicated by late enophthalmos: higher prevalence in patients with multiple trauma. Ophthal. Plast. Reconstr. Surg. 2007;23:115–118. doi: 10.1097/IOP.0b013e318032b30e. [DOI] [PubMed] [Google Scholar]
- Shere J.L., Boole J.R., Holtel M.R., Amoroso P.J. An analysis of 3599 midfacial and 1141 orbital blowout fractures among 4426 United States Army Soldiers, 1980–2000. Otolaryngol. Head Neck Surg. 2004;130:164–170. doi: 10.1016/j.otohns.2003.09.018. [DOI] [PubMed] [Google Scholar]
- Stanley R.B., Jr., Sires B.S., Funk G.F., Nerad J.A. Management of displaced lateral orbital wall fractures associated with visual and ocular motility disturbances. Plast. Reconstr. Surg. 1998;102:972–979. doi: 10.1097/00006534-199809040-00006. [DOI] [PubMed] [Google Scholar]
- Tsai H.H., Jeng S.F., Lin T.S. Predictive value of computed tomography in visual outcome in indirect traumatic optic neuropathy complicated with periorbital facial bone fracture. Clin. Neurol. Neurosurg. 2005;107:200–206. doi: 10.1016/j.clineuro.2004.07.015. [DOI] [PubMed] [Google Scholar]
- Unger J.M., Gentry L.R., Grossman J.E. Sphenoid fractures: prevalence, sites, and significance. Radiology. 1990;175:175–180. doi: 10.1148/radiology.175.1.2315477. [DOI] [PubMed] [Google Scholar]
- Yoshioka N., Tominaga Y., Motomura H., Muraoka M. Surgical treatment for greater sphenoid wing fracture (orbital blow-in fracture) Ann. Plast. Surg. 1999;42:87–91. doi: 10.1097/00000637-199901000-00015. [DOI] [PubMed] [Google Scholar]
- Zhang Q.B., Dong Y.J., Li Z.B., Zhao J.H. Coronal incision for treating zygomatic complex fractures. J. Craniomaxillofac. Surg. 2006;34:182–185. doi: 10.1016/j.jcms.2005.09.004. [DOI] [PubMed] [Google Scholar]


