Abstract
Background
Ischemic heart disease (IHD) is the most common cause of heart failure (HF); however, the role of revascularization in these patients is still unclear. Consensus on proper use of cardiac imaging to help determine which candidates should be considered for revascularization has been hindered by the absence of clinical studies that objectively and prospectively compare the prognostic information of each test obtained using both standard and advanced imaging.
Methods/Design
This paper describes the design and methods to be used in the Alternative Imaging Modalities in Ischemic Heart Failure (AIMI-HF) multi-center trial. The primary objective is to compare the effect of HF imaging strategies on the composite clinical endpoint of cardiac death, myocardial infarction (MI), cardiac arrest and re-hospitalization for cardiac causes.
In AIMI-HF, patients with HF of ischemic etiology (n = 1,261) will follow HF imaging strategy algorithms according to the question(s) asked by the physicians (for example, Is there ischemia and/or viability?), in agreement with local practices. Patients will be randomized to either standard (SPECT, Single photon emission computed tomography) imaging modalities for ischemia and/or viability or advanced imaging modalities: cardiac magnetic resonance imaging (CMR) or positron emission tomography (PET). In addition, eligible and consenting patients who could not be randomized, but were allocated to standard or advanced imaging based on clinical decisions, will be included in a registry.
Discussion
AIMI-HF will be the largest randomized trial evaluating the role of standard and advanced imaging modalities in the management of ischemic cardiomyopathy and heart failure. This trial will complement the results of the Surgical Treatment for Ischemic Heart Failure (STICH) viability substudy and the PET and Recovery Following Revascularization (PARR-2) trial. The results will provide policy makers with data to support (or not) further investment in and wider dissemination of alternative ‘advanced’ imaging technologies.
Trial registration
Background
The multifaceted Canada-Finland collaborative research program, Imaging Modalities to Assist with Guiding Therapy and the Evaluation of Patients with Heart Failure (IMAGE-HF), is designed with the following overall objectives: 1) to determine the impact of emerging imaging strategies on relevant clinical outcomes and decision making in patients with HF; 2) to establish standardized quality assurance (QA) measures and central databases in order to achieve reliable outcome driven research; and 3) to apply this as a platform for evaluation of new and emerging imaging and serum biomarkers in HF. The program consists of three separate randomized controlled trials. Project 1A is designed to compare the effect of HF imaging strategies in the evaluation and diagnosis of ischemic heart disease (IHD). Project 1B evaluates the utility of cardiac magnetic resonance (CMR) imaging in addition to standard echocardiography in the evaluation and diagnosis of non-ischemic HF (with either preserved or reduced ejection fraction) in comparison to the standard echocardiography alone. Project 1C is comparing two imaging modalities for the detection of coronary artery disease (standard coronary angiography versus cardiac computerized tomography scans).
Project 1A is the focus of this publication
Despite multiple advances in cardiovascular disease, the morbidity and mortality of patients with heart failure (HF) in the setting of IHD remains high. Although it is believed that most patients with symptoms of significant ischemia may benefit from revascularization, decisions regarding revascularization in those with advanced ventricular dysfunction and no significant ischemia are complex, and the applicability of current clinical trial data is often challenged by limited patient selection. Over the past three decades, information describing cardiac structure, function, perfusion, hemodynamics, and metabolism obtained from noninvasive cardiac imaging studies has been used to guide management decisions for patients with HF. Although this anatomic and physiologic information adds value to clinical care, an accepted strategy is still debated regarding the optimal testing sequence approach to efficiently identify the treatment strategy most likely to improve outcomes. Consensus on proper use of cardiac imaging studies has been hindered by absence of clinical studies that objectively compare the independent treatment-related prognostic information of each test obtained using standardized methods. Uniformity of reporting formats also needs to be improved in order to provide a clearer working scheme for clinicians.
Alternative Imaging Modalities in Ischemic Heart Failure (AIMI-HF) (Project I-A of the Imaging Modalities to Assist with Guiding Therapy and the Evaluation of Patients with Heart Failure, IMAGE-HF program) is a multicenter trial with the primary objective of comparing the effect of HF imaging strategies on the composite clinical endpoint of cardiac death, myocardial infarction (MI), resuscitated cardiac arrest and cardiac re-hospitalization (worsening heart failure, acute coronary syndrome, arrhythmia). Patients with an ischemic heart disease (IHD) etiology will follow HF imaging strategy algorithms according to the question(s) asked by the physicians (for example, is there ischemia and/or viability?), in agreement with their local clinical practices for standard and alternative imaging. Patients will be randomized to either standard imaging modalities for ischemia and/or viability (SPECT) or advanced imaging modalities, namely cardiac magnetic resonance imaging (CMR) or positron emission tomography (PET). Secondary objectives include the effect of HF imaging strategies on the incidence of revascularization procedures, left ventricular remodeling, HF symptoms and quality of life, as well as a health economic evaluation. A biomarker substudy (on renal function, left ventricular remodeling and a selected set of biomarkers), assessing mechanisms underlying specific cardiovascular events, is also planned (see Additional file 1).
Coronary revascularization and ischemic heart failure
Among patients with coronary artery disease (CAD) and heart failure, mortality rates range from 10 to 60% at 1 year [1-11]. CAD is the most common cause of HF, however the role of revascularization in these patients is often unclear. Significant concerns remain about perioperative morbidity and mortality [8,10-14]. The recent Surgical Treatment for Ischemic Heart Failure (STICH) trial [15] did not demonstrate a significant benefit for coronary artery bypass graphing (CABG) surgery compared to medical therapy, for the primary endpoint of all-cause mortality in patients with LV dysfunction (ejection fraction {“EF”} ≤ 35%) and coronary disease eligible for CABG; although there was benefit for secondary endpoints of cardiovascular death and cardiovascular endpoints. STICH focused on IHD rather than on chronic HF with systolic dysfunction, and the outcomes of the many patients who were screened but did not undergo revascularization remain unknown [16]. Unfortunately, the STICH trial has not provided the final answer on the role of revascularization for patients with chronic HF; nor did it evaluate the role of advanced imaging in decision making for revascularization in this patient population.
Imaging in ischemic heart failure
Increasingly over the past three decades, information describing cardiac structure, function, perfusion, hemodynamics, and metabolism obtained from noninvasive cardiac imaging studies has been used to guide management decisions for patients with HF. Although this anatomic and physiologic information adds value to clinical care, an accepted imaging strategy has not evolved that tailors the testing sequence to specific presenting features of individual patients to efficiently identify the treatment strategy most likely to improve outcomes. Consensus on proper use of cardiac imaging studies has been hindered by the absence of clinical studies that objectively compare the independent treatment-related prognostic information of each test obtained using standardized methods.
Observational data has demonstrated that methods to define ischemia, viability and scar can identify high risk patients likely to benefit (or not) from revascularization [17-22].
The long-term impact of newer or alternative imaging strategies used for the revascularization decision processes has not been evaluated prospectively in HF. Revascularization has the potential to restore function to dysfunctional viable myocardium but not scar. Our group and others have shown that patients with dysfunctional but viable hibernating myocardium are at high risk for cardiac events if they do not undergo timely revascularization [20,23].
Until recently, data from predominantly observational studies had shown that when viability is present, patients have better outcomes with revascularization [24-26]. The PET and Recovery Following Revascularization (PARR-2) trial [27] represents the largest randomized study to evaluate viability imaging in patients with severe LV dysfunction. Overall, there was a trend for benefit for Fluorodeoxyglucose (18F) positron emission tomgoraphy scan (FDG PET) assisted management over standard care. When the adherence to imaging recommendations was considered, there was a significant outcome benefit. A high risk subgroup demonstrated a significant mortality benefit [20,27]. Recently, in a post-hoc analysis a significant reduction in events was observed in a subset of patients at the Ottawa site (Ottawa-FIVE) [28]. The results suggest outcome benefits can be achieved using FDG PET in an experienced center with ready access to FDG and interactions with HF and revascularization teams.
Although PARR2 was unique as a randomized controlled trial for imaging viability, it was underpowered for the primary outcome. Larger prospective randomized studies are needed, although undertaking such studies can be challenging [16,29,30]. The STICH viability study [29] did not include a comparison to late gadolinium enhanced CMR, other modalities, nor evaluate the role of stress induced ischemia. Finally, although care was taken to standardize imaging acquisition and transfer of data, standardization was not as rigorous as has recently been achieved in the CADRE Ontario provincial registry [31].
Results from the STICH Viability substudy [29] suggest that identification of viable myocardium by single photon emission computed tomography (SPECT) or dobutamine stress echocardiography (DSE) do not add value in patients selected for surgical revascularization. The STICH Viability substudy results may be explained by a patient population that was at lower risk, with patients already acceptable for revascularization, having more single vessel disease, infrequent previous CABG, low incidence of renal dysfunction and predominantly without heart failure. For such patients, it may be argued that viability imaging is not needed. This is in contrast to sicker populations in studies such as PARR2 [20,27], where physicians were uncertain about revascularization decisions and, therefore, needed viability assessment. Viability testing was not randomized in STICH [15,16,29]. The authors acknowledged the potential for selection bias [29]. Furthermore, only 19% of patients in the substudy were considered to have nonviable myocardium, which is far less than in most previous studies [29,32,33]. Analyses combining DSE and SPECT results were performed. Ischemia and hibernation imaging were not reported. More advanced (or alternative) ischemia and viability imaging modalities (that is, using PET and CMR) were not evaluated.
Thus the STICH results need to be interpreted cautiously [16,30], and the limitations along with the other observational and randomized data, justify the need for a prospective randomized trial to evaluate imaging strategies in patients with heart failure.
AIMI-HF is a large randomized controlled trial, comparing ‘advanced imaging technologies’ (PET and CMR) to standard imaging (SPECT). The findings will provide policy makers with data to support (or not) further investment in and dissemination of alternative or advanced technologies.
Study hypotheses and objectives
Primary hypothesis
In patients with HF due to IHD with left ventricular ejection fraction (LVEF) ≤ 45%, a management algorithm that applies alternative imaging strategies (PET or CMR) achieves a better clinical outcome measured as the composite clinical endpoint of cardiac death, MI, resuscitated cardiac arrest and cardiac re-hospitalization (hospitalization due to heart failure, acute coronary syndrome or arrhythmia) than an approach with standard care using SPECT imaging.
Secondary hypotheses
1) Compared to standard care, in patients with HF due to IHD with LVEF ≤45% a management algorithm that applies alternative imaging modalities (PET or CMR) achieves: a) more efficient use of revascularization procedures with similar complication rates than standard care imaging strategies; b) better HF and angina symptom reduction; c) better quality of life (QoL), measured using MLHFQ and EQ5D; and d) is cost-effective.
2) In patients with HF due to IHD with LVEF ≤45%, a HF management algorithm that applies PET achieves a better primary (composite clinical endpoint) and secondary outcomes (revascularizations, remodeling, QoL, cost effectiveness) compared to one that applies CMR.
Primary objective
The primary objective of AIMI-HF is to compare the effect of HF imaging strategies on the composite clinical endpoint of cardiac death, MI, resuscitated cardiac arrest and cardiac re-hospitalization (WHF, ACS, and arrhythmia). Patients with HF due to an ischemic heart disease (IHD) etiology of LV dysfunction will follow HF imaging strategy algorithms according to the question(s) asked by the physicians (Is there ischemia and/or viability?), in agreement with their local practices for standard and alternative imaging.
Secondary objectives
To compare the effect of HF imaging strategies on:
1. The incidence of revascularization procedures (percutaneous coronary intervention {PCI}, CABG).
2. LVEF,
3. HF symptoms and New York Heart Association Functional Class (NYHA) class.
4. QOL (Minnesota Living with Heart Failure questionnaire (MLHFQ), the EQ5D).
5. Health economics. Costs will be estimated through regression analysis and cost effectiveness will be assessed through decision modeling.
6. The safety of imaging tests measured by cumulative radiation, adverse reactions to imaging contrast agents and stress testing agents will also be determined.
Methods/Design
The AIMI-HF is a randomized controlled trial to compare the effectiveness of HF imaging strategies in patients with HF due to IHD. Patients enrolled will have LV systolic dysfunction due to IHD where evaluation of ischemia and viability is relevant. Patients will be allocated in a concealed fashion to standard (SPECT) versus advanced (PET or CMR) imaging. In addition, a registry will be maintained of patients undergoing standard or advanced imaging based on clinical decisions.
A survey sent to participating centers revealed that most of them could not provide stress echocardiography consistently within the requested timeframe as per the research protocol. This was especially true for dobutamine stress-echo (DSE) and viability protocols. The decision not to include this method was mainly due to statistical considerations; since if only a few centers elected to use this standard method, there may not be enough patients to adequately compare it with other methods (and site bias might also be involved).
Study participants
Patients with clinical HF (see Table 1 for definition) or severe LV systolic dysfunction who need further definition of ischemia, viability or scar and meet the following inclusion and exclusion criteria, will be considered for entry into this trial. Patients will be prospectively randomized to standard (SPECT) versus advanced (PET or CMR) imaging. Patients who meet inclusion criteria but cannot be randomized due to clinical management decisions, yet undergo standard or advanced imaging, will be entered into a registry.
Table 1.
Criteria for the clinical diagnosis of heart failure
|
At least one of each of the following symptoms and signs in the last 12 months:a | |
|---|---|
| Symptoms | Signs |
| ▪ Paroxysmal nocturnal dyspnea |
▪ Pulmonary rales (post cough) |
| ▪ Orthopnea |
▪ Jugular venous pressure (JVP) ≥5 cm above sternal angle |
| ▪ Dyspnea upon mild or moderate exertion |
▪ Lower extremity oedema |
| ▪ Chest x-ray demonstrating pleural effusion, pulmonary congestion, or cardiomegaly | |
aIf LVEF is 30% or less, no signs or symptoms of HF are required for eligibility.
Inclusion criteria:
• Age >18 years
and
• Known or highly suspected coronary artery disease (CAD) documented by coronary angiography or by history of previous MI or evidence of moderate ischemia or scar based on prior imaging.
and
• LV dysfunction most likely attributable to ischemic heart disease with EF ≤45% measured by any acceptable means (echo, nuclear RNA, PET or SPECT perfusion, angiography, CMR) within the previous 6 months and NYHA class II to IV symptoms within the past 12 months or
• LV dysfunction most likely attributable to ischemic heart disease with EF ≤30% measured by any acceptable means (echo, nuclear RNA, PET or SPECT perfusion, angiography, CMR) within the previous 6 months AND NYHA class I within the past 12 months.
Exclusion criteria:
• Severe medical conditions that significantly affect the patient's recommended management (for example, severe COPD, active metastatic malignancy) and would preclude revascularization.
• <4 weeks post-ST segment elevation myocardial infarction (STEMI)
• Already identified as not suitable for revascularization
• Emergency revascularization indicated
• Severe valvular heart disease requiring valve surgery
• Pregnancy, breast feeding
• Potential for non-compliance to tests involved in this protocol
• Incapacity to provide informed consent
Randomization
Patients will be randomized according to a pre-defined randomization scheme and availability of imaging procedures at individual participating centers. All eligible patients will be randomized to either standard or advanced imaging modalities for ischemia and/or viability testing. Participating sites with the capability for two advanced imaging modalities will then be further randomized between each modality. If randomization is not possible due to local site factors, the patient can be entered into the registry (Figure 1). The ratio of advanced to standard imaging will be 2:1.
Figure 1.
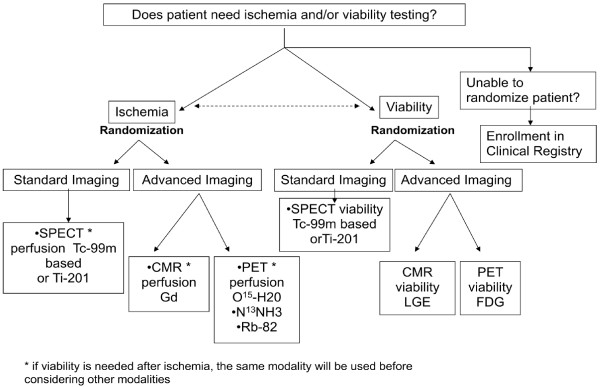
Overall randomization scheme for patients enrolled in Alternative Imaging Modalities in Ischemic Heart Failure (AIMI-HF).
Blinding
The study is not blinded given the nature and purpose of the interventions. Knowledge of imaging results and potential gained from the intervention will need to be considered to implement the appropriate treatment strategy. Therefore, performance bias (that is, systematic differences between groups in the care provided or exposure to factors other than the interventions of interest) and attrition bias (that is, systematic differences between groups in withdrawals from the study) may occur. Detection bias is still a potential concern, but an independent assessor will evaluate the objectively defined primary outcome and an adjudication committee will independently review and adjudicate each clinical event blinded to treatment randomization.
Measurements
Standard imaging protocols have been defined by the IMAGE-HF Standardization team, using nationally recognized protocols (Additional file 2) GFR will be estimated (eGFR) using the Modified Diet in Renal Disease (MDRD) equations based on current recommendations [34-37]. CBC, electrolytes, urea, creatinine will be measured locally on randomization. This creatinine measurement will serve for local eGFR assessment (to ensure CMR eligibility). Further laboratory analyses will be collected and stored for future biomarkers analyses (at baseline and at 1 year in a subgroup of patients; Additional file 1).
Subject evaluation
At baseline, demographic and clinical data will be collected from all participants on standardized case report forms. These data will be collected from the most recent, routine history and physical examination that has been completed by the treating physician. Quality of life questionnaires (EuroQol and Minnesota Living with Heart Failure) will be administered. In addition, the above-mentioned laboratory samples will be collected. To address a secondary objective, whenever possible, an echocardiogram will be performed if LV ejection fraction has not been determined by echocardiography within 6 months prior to randomization. As much as possible, imaging procedures will be performed within 4 weeks after entry into the trial. Subsequent telephone follow-up and repeat blood work will be performed on a predetermined schedule (Table 2). If the patient cannot be reached by telephone for their final assessment, a query will be made at government or national health care resources to verify if any corresponding events have occurred since the last visit (search of corresponding codes for cardiac death, MI, cardiac arrest and cardiac re-hospitalization for WHF, ACS, or arrhythmia). A follow-up echocardiogram will be requested at one year (LV remodeling, LVEF). Within 3 months of the baseline scan the treating physician will be asked to record the HF management plan.
Table 2.
Patient assessment schedule
| Baseline | 3 months | 6 months | 12 months | 18 months | 24 months | 36 months | 48 months | |
|---|---|---|---|---|---|---|---|---|
| Imaging (SPECT, PET or CMR) |
x |
|
|
|
|
|
|
|
| Blood work |
x |
|
|
x |
|
|
|
|
| Demographic and history |
x |
|
|
|
|
|
|
|
| Clinical data collected |
x |
|
|
x |
|
|
|
|
| EuroQol questionnaire |
x |
x |
x |
x |
x |
x |
x |
x |
| MLWHF questionnaire |
x |
x |
x |
x |
x |
x |
x |
x |
| Telephone follow-up | x | x | x | x | x | x | x |
CMR cardiac magnetic resonance, MLWHF Minnesota Living with Heart Failure, PET positron emission tomography, SPECT single photon emission computed tomography.
Safety and ethics
This study was approved by the University of Ottawa Heart Institute Human Research Ethics Board, protocol #2010620-01H. In addition, before study initiation at each site, this protocol, and the informed consent form, as well as any advertisement for subject recruitment, was submitted for review and approval by each local participating site’s ethics committee charged with this responsibility and will be so submitted for future sites. These ethic committees will submit written notification of the approval to the investigator. This study will be conducted according to the Declaration of Helsinki, Good Clinical Practice and the TriCouncil Policy.
Registry
Eligible and consenting patients that could not be randomized but undergo standard or advanced imaging based on clinical decisions, will be included in a registry. Measurement, subject evaluation and safety and ethics as outlined in the previous sections will apply to these registry patients. The registry patients for advanced imaging will be considered in the sample size calculation and data analysis (see below); however, the small number of patients expected to be part of the SPECT registry will not be considered in the primary analysis.
Sample size
For the sample size determination, the estimated occurrence over one year of the composite clinical endpoint of cardiac death, MI, resuscitated cardiac arrest and cardiac re-hospitalization (WHF, ACS, arrhythmia) for PET is 27% and for standard care is 40%, based on the Ottawa-FIVE substudy [28] of the PARR-2 [27] study in which the composite event rates were 19% and 41%, respectively. These estimates were considered reasonable as it reflects the outcome rates that may be achievable at a facility with expertise and access to FDG PET imaging. There are no similar data upon which to draw an estimate for CMR. Considering the Schinkel et al. publication [38], which noted sensitivity of CMR to be between PET and standard care modalities and based on expert consensus from our IMAGE-HF workshop (16 December 2008 in Toronto, Canada), we estimate the event rate for CMR directed care would lie between the above values at 34%. Hence, an overall rate for the alternative (PET, CMR) modalities would be approximately 30%. The rates are considered conservative since the mean duration of follow-up will be 2 years, whereas the PARR-2 study was 1 year.
For the primary hypothesis, using the two-sided log-rank test for comparing advanced (PET + CMR) versus standard modalities with a 2:1 patient allocation, a sample size of 495 patients (of which 330 are allocated to the advance modality and 165 are allocated to the standard modality) would be needed in order to detect a difference after 1 year in the composite clinical endpoint of 30% for the advanced modalities (PET, CMR) compared to 40% for standard care modalities (SPECT). This is calculated with a level of significance of 0.05 and power of 80%, and assuming a uniform accrual of patients over the 2.5 year recruitment period, a 1 year minimum follow-up period and a 10% loss from each study group. The difference of 10% was considered to be a minimal clinically important difference based on a consensus of the IMAGE-HF investigators.
For the secondary hypothesis, using the Cox regression model for comparing the advanced modalities PET versus CMR with an approximate 1:1 patient allocation, a sample size of 548 patients per modality is needed considering an anticipated rate for the composite clinical endpoint of 30% after 1 year, a level of significance of 0.05, a power of 80% and a loss to follow-up of 10%. The sample size calculation is complicated by the fact that 766 patients (383 per group) from the registry (in which patients in the registries were clinically directed to PET or CMR) will be combined in the analysis with the 330 patients (165 per group) from the randomized part of the study (in which patients in the randomized study will be randomly allocated to PET versus CMR versus standard modality) for a total of 1096 patients (548 per group). For a sample of 1096 patients, a Cox regression of the log hazard ratio of the composite clinical endpoint on the group allocation variable (PET versus CMR) with a conservative standard deviation of 0.5 (based on an approximate equal allocation to PET and CMR), achieves 80% power at a 0.05 significance level to detect a 40% increase in the hazard ratio to1.4. This increase in the hazard ratio was deemed to be the minimal clinically important difference based on a consensus among the IMAGE-HF investigators. The sample size includes an adjustment to accommodate confounding by indication for allocation patients to PET versus CMR by incorporating a multiple regression of the group allocation variable on the other covariates in the Cox regression model; a conservative estimate of this confounding was considered by taking a value of 0.25 for the multiple correlation coefficient R for the relationship between the group allocation variable and the set of covariates identified.
The total sample size is thus 1,096 + 165 = 1,261.
Statistical analysis
Descriptive statistics will be used to summarize the characteristics of the patients for each imaging technology on demographic, clinical and site-related factors, and differences between these groups will be reviewed for their clinical significance.
Analysis populations
For the purposes of data analysis, three study populations will be considered: Intent-to-treat (ITT) Population, As-Treated Population and Per-protocol Population. The ITT population will be used for the main analysis for all primary and secondary objectives, except for the safety analysis where the as-treated population will be used. As a secondary analysis, the analyses will be repeated for the as-treated and per-protocol populations.
Primary analysis (advanced versus standard imaging)
For the primary analysis, the time-to-event of the composite clinical endpoint of cardiac death, MI, arrest and cardiac re-hospitalization (WHF, ACS, arrhythmia) will be compared between the advanced modality (PET or CMR) to an approach with standard care using SPECT imaging using survival analysis. Kaplan-Meier survival curves of the primary endpoint will be compared between the advanced and standard modalities with the log-rank test. Potential confounding variables of the relationship between the imaging technologies and the primary endpoint will be assessed. In particular, propensity scores based on patient factors (for example, in/outpatient, NYHA class, HF duration, diabetes, atrial fibrillation) and site factors (for example, time-to-imaging, time-to-therapy) will be used in the analysis if necessary to adjust for potential differences. A Cox proportional hazard models will be used to assess the occurrence of the endpoints between the imaging technologies (model will include a group indicator variable) adjusting for any pertinent baseline differences identified. The proportional hazards assumption underlying the Cox model will be assessed.
Secondary outcomes
For the secondary outcomes PCI, CABG, HF symptoms and NYHA class, chi-square tests will be used to compare the advanced and standard imaging technologies; logistic regression analysis will be used for adjusting any pertinent baseline differences identified. For the secondary outcomes LVEF, MLHFQ and EQ5D, analysis of variance will be used to compare trends over time between the advanced and standard technologies. Analysis of covariance will be used for adjusting any pertinent baseline differences identified.
Economic evaluation
For secondary objective 5, a cost-effectiveness analysis of advanced versus standard modality groups will be conducted. Analysis will take the form of a cost-utility analysis with cost effectiveness assessed in terms of the incremental cost per quality life year. Analysis will incorporate data on resource use and patients utility values for the period from initiation of treatment to study termination. Resource use will be assessed through review of patient charts and patient utility values will be derived using the EQ5D and MLHF. A decision model will be created to estimate long-term costs and quality adjusted life years (QALYs) for all comparators. Uncertainty within the analysis will be assessed through Monte Carlo and other simulation techniques.
Safety analysis
For the secondary objective 6, safety will be evaluated by documenting all adverse events. Descriptive statistics (frequency distributions, numerical descriptors) and 95% CIs will be calculated. The as-treated population will be the main analysis population for this safety evaluation.
Secondary analysis (PET versus CMR)
For the secondary analysis, comparing the PET and CMR modalities, potential confounding variables of the relationship between the imaging technologies and the primary endpoint will be assessed. In particular, propensity scores based on patient factors (for example, in/outpatient, NYHA class, HF duration, diabetes, atrial fibrillation) and site factors (for example, time-to-imaging, time-to-therapy) will be used in the analysis if necessary to adjust for potential differences between PET and CMR. A Cox proportional hazard models will be used to assess the occurrence of the endpoints between the imaging technologies (the model will include a group indicator variable) adjusting for any pertinent baseline differences identified. The proportional hazards assumption underlying the Cox model will be assessed. The secondary outcomes will be analyzed in a similar fashion.
Missing data
‘Missingness’ is considered to be missing at random (MAR) and mixed methods repeated measures (MMRM) and multiple imputation techniques will be used for handling missing data. In particular, for continuous outcomes at multiple time points MMRM will be used.
Study management
The IMAGE-HF trial is managed by an Executive Committee consisting of clinicians specialized in diagnostic imaging and/or heart failure and experts in biostatistics, physics and radiochemistry, as well as a larger Steering Committee consisting of members of the Executive Committee and representatives of all the initial study centers. (Table 3) In addition there is an events adjudication committee, which will independently review and adjudicate each clinical event blinded to treatment randomization. Since all the imaging approaches are part of standard clinical practice, no interim analysis is planned, but there will be independent data safety monitoring board (DSMB), which will review the safety data on a periodic basis; the frequency of the meetings and the charter governing the DSMB will be finalized at the first meeting of the DSMB.
Table 3.
Imaging Modalities to Assist with Guiding Therapy and the Evaluation of Patients with Heart Failure (IMAGE-HP) participating
|
IMAGE-HF Participating Sites |
|
|---|---|
| Investigator | Role |
|
University of Ottawa Heart Institute |
|
| R Beanlands |
Co-Principal Investigator IMAGE-HF, Canada |
| G. A. Wells |
Principal Investigator CRMC |
| R. deKemp |
Principal Investigator QA Program |
| D. Birnie |
Co-Principal Investigator Project IIA |
| L. Mielniczuk |
Co-Principal Investigator Project IA |
| K. Chan |
Site Principal Investigator |
| B. Chow |
Principal Investigator Project IC |
| L. Garrard |
Project Management |
| R. Hessian |
Investigator |
| T. Ruddy |
Investigator |
| RA Davies |
Investigator |
| H. Haddad |
Investigator |
| A. Dick |
Investigator |
| C. Dennie |
Investigator |
| D. Coyle |
Investigator |
| B. McArdle |
Investigator |
| T. Dowsley |
Investigator |
| G. Dwivedi |
Investigator |
| J. DaSilva |
Investigator |
| C. Kelly |
Research Coordinator |
| E. Moga |
Research Coordinator |
| R. Klein |
Core Lab Manager |
| K. Williams |
Statistician |
| R. Fleming |
Research Coordinator |
| M. Boomgaardt |
Research Coordinator |
|
Montreal Heart Institute-Université de Montréal |
|
| JC Tardif |
Investigator |
| E. O'Meara |
Co-Principal Investigator Project IA |
| M. Friedrich |
Investigator |
| J. Rouleau |
Investigator |
| T. Heinonen |
Investigator |
| F. Marcotte |
Investigator |
| N. Racine |
Investigator |
| H. Q Ly |
Investigator |
| J. Morrissette |
Research Coordinator |
| H. Brown |
Research Coordinator |
|
University of Alberta |
|
| I. Paterson |
Principal Investigator Project IB |
| L. Lalonde |
Investigator |
| J. Ezekowitz |
Investigator |
| M. Irwin |
Research Coordinator |
|
University of Turku |
|
| J. Knuuti |
Co-Principal Investigator IMAGE-HF, Finland |
| H. Ukkonen |
Investigator |
| S. Yla-Herttuala |
Investigator |
| H. Leskinen |
Investigator |
| A. Saraste |
Investigator |
| T. Vasankari |
Research Coordinator |
| K. Lahtonen |
Research Coordinator |
| M. Tarkia |
Site Project Manager |
|
University Central Hospital, Helsinki |
|
| M. Laine |
Site Principal Investigator |
| H. Hanninen |
Investigator |
| M. Pietila |
Research Coordinator |
|
University of Kuopio |
|
| J. Hartikainen |
Site Principal Investigator |
| S. Karkkainen |
Investigator |
| I. Kaivonurmi |
Research Coordinator |
| M. Sutinen |
Research Coordinator |
|
Sunnybrook Health Sciences Centre |
|
| G. Wright |
Site Co-Principal Investigator |
| K. Connelly |
Site Co-Principal Investigator |
| R. Myers |
Investigator |
| C. Cunningham |
Investigator |
| E. Crystal |
Investigator |
| A. Leber |
Investigator |
| M. Mohammed |
Research Coordinator |
| J. Malko |
Research Coordinator |
|
University of Calgary |
|
| A. Howarth |
Site Co-Principal Investigator |
| T. Anderson |
Site Co-Principal Investigator |
| A. Krysk |
Investigator |
| S. Hutchison |
Investigator |
| N. Merchant |
Investigator |
| S. Weeks |
Investigator |
| R. Sandonato |
Research Coordinator |
| S. Rivest |
Research Coordinator |
| J. Veenhuyzen |
Research Coordinator |
| M. Seib |
Research Coordinator |
| B. Madden |
Research Coordinator |
| D. Durand |
Research Coordinator |
|
London Health Sciences |
|
| M. Arnold |
Site Principal Investigator |
| G. Wisenberg |
Investigator |
| T. Lee |
Investigator |
| F. Prato |
Investigator |
| J. White |
Co-Principal Investigator Project IIA |
| K. Carter |
Research Coordinator |
|
Laval University |
|
| E. Larose |
Site Principal Investigator |
| P. Pibarot |
Investigator |
| B. Cantin |
Investigator |
| J. Carange |
Research Coordinator |
| K. Bibeau |
Research Coordinator |
|
St. Michael's Hospital |
|
| M. Freeman |
Site Co-Principal Investigator |
| K. Connelly |
Site Co-Principal Investigator |
| H. Leong-Poi |
Investigator |
| G. Moe |
Investigator |
| A. Al-Hesayen |
Investigator |
| J. Sloninko |
Research Coordinator |
|
Hamilton |
|
| V. Tandon |
Site Principal Investigator |
| K. Gulenchyn |
Investigator |
| F. Spence |
Investigator |
| A. Khoorshed |
Research Coordinator |
|
Sherbrooke |
|
| E. Turcotte |
Site Principal Investigator |
| S. Lepage |
Investigator |
| Paul Farand |
Investigator |
| S. Joncas |
Resident, recruitment |
| E. Lavallee |
Research Coordinator |
|
Halifax |
|
| M. Rajda |
Site Principal Investigator |
| R. Stewart |
Investigator |
| J. Clarke |
Investigator |
| S. Burrell |
Investigator |
| B. Clarke |
Investigator |
| S. Yarn |
Research Coordinator |
| M. MacFarlane |
Research Coordinator |
|
Winnipeg |
|
| M. Kass |
Site Principal Investigator |
| J. Tan |
Investigator |
| T. Moore |
Research Coordinator |
| A. Munoz |
Research Coordinator |
|
QA Core Labs |
|
| R. Klein |
Core Lab Manager (Ottawa) |
| R. deKemp |
PET, SPECT QA Core Lab Team Leader (Ottawa) |
| B. McArdle |
PET, SPECT QA Core Lab (Ottawa) |
| J. Renaud |
PET, SPECT QA Core Lab (Ottawa) |
| K. Chan |
ECHO QA Core Lab Team Leader (Ottawa) |
| J. White |
CMR QA Core Lab 1A Team Leader (London) |
| I. Pauchard |
CMR QA Core Lab 1A (London) |
| I. Patterson |
CMR QA Core Lab 1B Team Leader (Edmonton) |
| P. L’Allier |
ICA QA Core Lab Team Leader (Montreal) |
| B. Chow |
CTA QA Core Lab Team Leader (Ottawa) |
|
Steering Committee |
|
| R. Beanlands |
|
| G. A. Wells |
|
| J. Knuuti |
|
| M. Friedrich |
|
| G. Wright |
|
| M. Arnold |
|
| J.C. Tardif |
|
| P. Pibarot |
|
| S. Ylä-Herttuala |
|
| R. deKemp |
|
|
DSMB |
|
| A. Krahn, Chair |
|
| J. Fallavollita |
|
| L. Thabane |
|
|
Events |
|
| H. Haddad, Chair |
|
| D.S. Beanlands |
|
| L. Duchesne |
|
| J. Ezekowitz |
|
| R. A. Davies |
Blood samples for the biomarkers ancillary study will be stored at the Montreal Heart Institute central laboratory for analyses to be performed after study completion.
Trial status
At the time of this manuscript preparation, the IMAGE IA trial is currently in the second year of active enrollment. We have enrolled a total of 249 patients, representing 20% of anticipated total enrollment. The study is active in a total of 13 sites across Canada and Finland. We anticipate study completion of enrollment by December 2015.
Abbreviations
AIMI-HF: Alternative Imaging Modalities in Ischemic Heart Failure; CABG: Coronary artery bypass graphing; CAD: Coronary artery disease; CKD: Chronic kidney disease; CMR: Cardiac magnetic resonance imaging; DSE: Dobutamine stress echocardiography; DSMB: Data safety monitoring board; EF: Ejection fraction; eGFR: Estimated glomerular filtration rate; FDG PET: Fluorodeoxyglucose (18F) positron emission tomgoraphy scan; HF: Heart failure; IHD: Ischemic heart disease; IMAGE-HF: Imaging Modalities to Assist with Guiding Therapy and the Evaluation of Patients with Heart Failure; ITT: Intent-to-treat; JVP: Jugular venous pressure; LVEF: Left ventricular ejection fraction; MAR: Missing at random; MDRD: Modification of Diet in Renal Disease; MI: Myocardial infarction; MLWHF: Minnesota Living with Heart Failure; MMRM: Mixed methods repeated measures; NYHA: New York Heart Assocation Functional Class; PARR-2: PET and Recovery Following Revascularization; PCI: Percutaneous coronary interventsion; PET: Positron emission tomography; QA: Quality assurance; QALYS: Quality adjusted life years; SOPs: Standard operating procedures; SPECT: Single photon emission computed tomography; STEM: Segment elevation myocardial infarction; STICH: Surgical treatment for ischemic heart failure.
Competing interests
The following authors have competing interests to disclose; R Beanlands is a consultant for Lantheus Medical Imaging, DraxImage; and has research funding from Lantheus Medical Imaging, GE, and MDS Nordion E O’Meara has research funding from Johnson & Johnson for the Cardiorenal-anemia syndrome in HF. R deKemp is a consultant for Jubilant DraxImage; and has research funding from the following: Lantheus Medical Imaging, GE, MDS Nordion. He also receives revenues from rubidium generator technology licensed to Jubilant DraxImage, and receives revenues from FlowQuant software sales. R Klein is a consultant for Jubilant DraxImage. He receives revenues from rubidium generator technology licensed to Jubilant DraxImage and hereceives revenues from FlowQuant software sales. T Ruddy has Research funding from Nordion, Inc, GE Healthcare and Atreus, Inc. For all other authors, there are no competing interests.
Authors’ contributions
RB, EO, LMM, GAW, JK conceived the study, participated in its design and coordination, and helped to draft the manuscript. EO and LMM are co-principle investigators of this project. LG is involved in the study design and project management and helped to draft the manuscript. RdK and RK established and will monitor the standardization of the imaging modalities. DC designed and will coordinate the economic evaluation. The following contributed to design of trial and will be involved with conducting the trial: BMcA, IP, JAW, MA, MF, PP, AD, EL, BC, CD, HH, TR, HU,GW, BC,MGF, ET, KC, JC, NR, JCT, JR. All authors read and approved the final manuscript.
Supplementary Material
Left ventricular remodeling and biomarkers ancillary study – a synopsis.
Standardization and quality assurance (IMAGE-QA).
Contributor Information
Eileen O’Meara, Email: eileen.omeara@umontreal.ca.
Lisa M Mielniczuk, Email: lmielniczuk@ottawaheart.ca.
George A Wells, Email: gawells@ottawaheart.ca.
Robert A deKemp, Email: radekemp@ottawaheart.ca.
Ran Klein, Email: rklein@ottawaheart.ca.
Doug Coyle, Email: dcoyle@uottawa.ca.
Brian Mc Ardle, Email: bmcardle@ottawaheart.ca.
Ian Paterson, Email: ip3@ualberta.ca.
James A White, Email: jwhite@imaging.robarts.ca.
Malcolm Arnold, Email: malcolm.arnold@lhsc.on.ca.
Matthias G Friedrich, Email: matthias.friedrich@icm-mhi.org.
Eric Larose, Email: eric.larose@criucpq.ulaval.ca.
Alexander Dick, Email: adick@uottawaheart.ca.
Benjamin Chow, Email: bchow@ottawaheart.ca.
Carole Dennie, Email: cdennie@toh.on.ca.
Haissam Haddad, Email: hhaddad@ottawaheart.ca.
Terrence Ruddy, Email: truddy@ottawaheart.ca.
Heikki Ukkonen, Email: heikki.ukkonen@tyks.fi.
Gerald Wisenberg, Email: gerald.wisenberg@lawsonimaging.ca.
Bernard Cantin, Email: clajoie@sympatico.ca.
Philippe Pibarot, Email: philippe.pibarot@med.ulaval.ca.
Michael Freeman, Email: freemanm@smh.toronto.on.ca.
Eric Turcotte, Email: e.turcotte@usherbrooke.ca.
Kim Connelly, Email: connellyk@smh.ca.
James Clarke, Email: james_clarke@ns.sympatico.ca.
Kathryn Williams, Email: kwilliams@cheo.ca.
Normand Racine, Email: normand.racine@icm-mhi.org.
Linda Garrard, Email: lgarrard@ottawaheart.ca.
Jean-Claude Tardif, Email: jean-claude.tardif@icm-mhi.org.
Jean DaSilva, Email: jdasilva@ottawaheart.ca.
Juhani Knuuti, Email: juhani.knuuti@utu.fi.
Rob Beanlands, Email: rbeanlands@ottawaheart.ca.
Acknowledgements
AIMI-HF is supported by the IMAGE HF Team Grant funded by Canadian Institute of Health Research CIHR (team grant # CIF 99470). R.B. is a Career Investigator supported by the Heart and Stroke Foundation of Ontario and Tier 1 Research Chair supported by the University of Ottawa. E.O. is sponsored by les Fonds de Rercherche en Santé du Québec (Junior 2 researcher grant 2011-2015) for research on biomarkers and imaging in heart failure and chronic kidney disease. B.M. is supported in part by the MFI HSFO Program Grant (HSFO Grant #PRG6242) and the University of Ottawa Heart Institute’s Whit & Heather Tucker Endowed Research Fellowship in Cardiology.
References
- Arnold JM, Liu P, Demers C, Dorian P, Giannetti N, Haddad H, Heckman GA, Howlett JG, Ignaszewski A, Johnstone DE, Jong P, McKelvie RS, Moe GW, Parker JD, Rao V, Ross HJ, Sequeira EJ, Svendsen AM, Teo K, Tsuyuki RT, White M. Canadian Cardiovascular Society consensus conference recommendations on heart failure 2006: diagnosis and management. Can J Cardiol. 2006;22:23–45. doi: 10.1016/S0828-282X(06)70237-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- McKee PA, Castelli WP, McNamara PM, Kannel WB. The natural history of congestive heart failure: the Framingham study. N Engl J Med. 1971;285:1441–1446. doi: 10.1056/NEJM197112232852601. [DOI] [PubMed] [Google Scholar]
- Yatteau RF, Peter RH, Behar VS, Bartel AG, Rosati RA, Kong Y. Ischemic cardiomyopathy: the myopathy of coronary artery disease. Natural history and results of medical versus surgical treatment. Am J Cardiol. 1974;34:520–525. doi: 10.1016/0002-9149(74)90121-0. [DOI] [PubMed] [Google Scholar]
- Alderman EL, Fisher LD, Litwin P, Kaiser GC, Myers WO, Maynard C, Levine F, Schloss M. Results of coronary artery surgery in patients with poor left ventricular function (CASS) Circulation. 1983;68:785–795. doi: 10.1161/01.CIR.68.4.785. [DOI] [PubMed] [Google Scholar]
- Alderman EL, Bourassa MG, Cohen LS, Davis KB, Kaiser GG, Killip T, Mock MB, Pettinger M, Robertson TL. Ten-year follow-up of survival and myocardial infarction in the randomized Coronary Artery Surgery Study. Circulation. 1990;82:1629–1646. doi: 10.1161/01.CIR.82.5.1629. [DOI] [PubMed] [Google Scholar]
- Franciosa JA, Wilen M, Ziesche S, Cohn JN. Survival in men with severe chronic left ventricular failure due to either coronary heart disease or idiopathic dilated cardiomyopathy. Am J Cardiol. 1983;51:831–836. doi: 10.1016/S0002-9149(83)80141-6. [DOI] [PubMed] [Google Scholar]
- Tu JV, Austin PC, Walld R, Roos L, Agras J, McDonald KM. Development and validation of the Ontario acute myocardial infarction mortality prediction rules. J Am Coll Cardiol. 2001;37:992–997. doi: 10.1016/S0735-1097(01)01109-3. [DOI] [PubMed] [Google Scholar]
- Tjan TD, Kondruweit M, Scheld HH, Roeder N, Borggrefe M, Schmidt C, Schober O, Deng MC. The bad ventricle revascularization versus transplantation. Thorac Cardiovasc Surg. 2000;48:9–14. doi: 10.1055/s-2000-8888. [DOI] [PubMed] [Google Scholar]
- Passamani E, Davis KB, Gillespie MJ, Killip T. A randomized trial of coronary artery bypass surgery. Survival of patients with a low ejection fraction. N Engl J Med. 1985;312:1665–1671. doi: 10.1056/NEJM198506273122603. [DOI] [PubMed] [Google Scholar]
- Jones RH. Is it time for a randomized trial of surgical treatment of ischemic heart failure? J Am Coll Cardiol. 2001;37:1210–1213. doi: 10.1016/S0735-1097(01)01123-8. [DOI] [PubMed] [Google Scholar]
- Doenst T, Velazquez EJ, Beyersdorf F, Michler R, Menicanti L, Di Donato M, Gradinac S, Sun B, Rao V. To STICH or not to STICH: we know the answer, but do we understand the question? J Thorac Cardiovasc Surg. 2005;129:246–249. doi: 10.1016/j.jtcvs.2004.07.060. [DOI] [PubMed] [Google Scholar]
- Louie HW, Laks H, Milgalter E, Drinkwater DC Jr, Hamilton MA, Brunken RC, Stevenson LW. Ischemic cardiomyopathy. Criteria for coronary revascularization and cardiac transplantation. Circulation. 1991;84(5 Suppl):III290–III295. [PubMed] [Google Scholar]
- Kron IL, Flanagan TL, Blackbourne LH, Schroeder RA, Nolan SP. Coronary revascularization rather than cardiac transplantation for chronic ischemic cardiomyopathy. Ann Surg. 1989;210:348–352. doi: 10.1097/00000658-198909000-00011. discussion 352–344. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hochberg MS, Parsonnet V, Gielchinsky I, Hussain SM. Coronary artery bypass grafting in patients with ejection fractions below forty percent. Early and late results in 466 patients. J Thorac Cardiovasc Surg. 1983;86:519–527. [PubMed] [Google Scholar]
- Velazquez EJ, Lee KL, Deja MA, Jain A, Sopko G, Marchenko A, Ali IS, Pohost G, Gradinac S, Abraham WT, Yii M, Prabhakaran D, Szwed H, Ferrazzi P, Petrie MC, O'Connor CM, Panchavinnin P, She L, Bonow RO, Rankin GR, Jones RH, Rouleau JL. STICH Investigators. Coronary-artery bypass surgery in patients with left ventricular dysfunction. N Engl J Med. 2011;364:1607–1616. doi: 10.1056/NEJMoa1100356. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fang JC. Underestimating medical therapy for coronary artery disease… Again. N Engl J Med. 2011;364:1671–1673. doi: 10.1056/NEJMe1103414. [DOI] [PubMed] [Google Scholar]
- Beanlands RS, Chow BJ, Dick A, Friedrich MG, Gulenchyn KY, Kiess M, Leong-Poi H, Miller RM, Nichol G, Freeman M, Bogaty P, Honos G, Hudon G, Wisenberg G, Van Berkom J, Williams K, Yoshinaga K, Graham J. CCS/CAR/CANM/CNCS/CanSCMR joint position statement on advanced noninvasive cardiac imaging using positron emission tomography, magnetic resonance imaging and multidetector computed tomographic angiography in the diagnosis and evaluation of ischemic heart disease--executive summa. Can J Cardiol. 2007;23:107–119. doi: 10.1016/S0828-282X(07)70730-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Schinkel AF, Bax JJ, Poldermans D, Elhendy A, Ferrari R, Rahimtoola SH. Hibernating myocardium: diagnosis and patient outcomes. Curr Probl Cardiol. 2007;32:375–410. doi: 10.1016/j.cpcardiol.2007.04.001. [DOI] [PubMed] [Google Scholar]
- Di Carli MF, Davidson M, Little R, Khanna S, Mody FV, Brunken RC, Czernin J, Rokhsar S, Stevenson LW, Laks H, Hawkins R, Schelbert HR, Phelps ME, Maddahi J. Value of metabolic imaging with positron emission tomography for evaluating prognosis in patients with coronary artery disease and left ventricular dysfunction. Am J Cardiol. 1994;73:527–533. doi: 10.1016/0002-9149(94)90327-1. [DOI] [PubMed] [Google Scholar]
- D’Égiodio G, Nichol G, Williams KA, Guo A, Garrard L, deKemp R, Ruddy TD, DaSilva J, Humen D, Gulenchyn KY, Freeman M, Racine N, Benard F, Hendry P, Beanlands RS. PARR-2 Investigators. Increasing benefit from revascularization is associated with increasing amounts of myocardial hibernation: a substudy of the PARR-2 trial. JACC Cardiovasc Imaging. 2009;2:1060–1068. doi: 10.1016/j.jcmg.2009.02.017. [DOI] [PubMed] [Google Scholar]
- Tillisch J, Brunken R, Marshall R, Schwaiger M, Mandelkern M, Phelps M, Schelbert H. Reversibility of cardiac wall-motion abnormalities predicted by positron tomography. N Engl J Med. 1986;314:884–888. doi: 10.1056/NEJM198604033141405. [DOI] [PubMed] [Google Scholar]
- Kwon DH, Halley CM, Carrigan TP, Zysek V, Popovic ZB, Setser R, Schoenhagen P, Starling RC, Flamm SD, Desai MY. Extent of left ventricular scar predicts outcomes in ischemic cardiomyopathy patients with significantly reduced systolic function: a delayed hyperenhancement cardiac magnetic resonance study. JACC Cardiovasc Imaging. 2009;2:34–44. doi: 10.1016/j.jcmg.2008.09.010. [DOI] [PubMed] [Google Scholar]
- Beanlands RS, Hendry PJ, Masters RG, deKemp RA, Woodend K, Ruddy TD. Delay in revascularization is associated with increased mortality rate in patients with severe left ventricular dysfunction and viable myocardium on fluorine 18-fluorodeoxyglucose positron emission tomography imaging. Circulation. 1998;98(19 Suppl):II51–II56. [PubMed] [Google Scholar]
- Lee KS, Marwick TH, Cook SA, Go RT, Fix JS, James KB, Sapp SK, MacIntyre WJ, Thomas JD. Prognosis of patients with left ventricular dysfunction, with and without viable myocardium after myocardial infarction. Relative efficacy of medical therapy and revascularization. Circulation. 1994;90:2687–2694. doi: 10.1161/01.CIR.90.6.2687. [DOI] [PubMed] [Google Scholar]
- Yoshida K, Gould KL. Quantitative relation of myocardial infarct size and myocardial viability by positron emission tomography to left ventricular ejection fraction and 3-year mortality with and without revascularization. J Am Coll Cardiol. 1993;22:984–997. doi: 10.1016/0735-1097(93)90407-R. [DOI] [PubMed] [Google Scholar]
- Allman KC, Shaw LJ, Hachamovitch R, Udelson JE. Myocardial viability testing and impact of revascularization on prognosis in patients with coronary artery disease and left ventricular dysfunction: a meta-analysis. J Am Coll Cardiol. 2002;39:1151–1158. doi: 10.1016/S0735-1097(02)01726-6. [DOI] [PubMed] [Google Scholar]
- Beanlands RS, Nichol G, Huszti E, Humen D, Racine N, Freeman M, Gulenchyn KY, Garrard L, deKemp R, Guo A, Ruddy TD, Benard F, Lamy A, Iwanochko RM. F-18-fluorodeoxyglucose positron emission tomography imaging-assisted management of patients with severe left ventricular dysfunction and suspected coronary disease: a randomized, controlled trial (PARR-2) J Am Coll Cardiol. 2007;50:2002–2012. doi: 10.1016/j.jacc.2007.09.006. [DOI] [PubMed] [Google Scholar]
- Abraham A, Nichol G, Williams K, Garrard L, Guo A, de Kemp RA, Davies RA, Duchesne L, Haddad H, Ruddy TD, Chow B, DaSilva J, Hendry P, Masters R, Higginson L, Beanlands RS. Ottawa-FIVE: FDG in viability evaluation at an experienced center with ready Access to FDG and integration with management teams. J Nucl Med. 2010;51:567–574. doi: 10.2967/jnumed.109.065938. [DOI] [PubMed] [Google Scholar]
- Bonow RO, Maurer G, Lee KL, Holly TA, Binkley PF, Desvigne-Nickens P, Drozdz J, Farsky PS, Feldman AM, Doenst T, Michler RE, Berman DS, Nicolau JC, Pellikka PA, Wrobel K, Alotti N, Asch FM, Favaloro LE, She L, Velazquez EJ, Jones RH, Panza JA. STICH Trial Investigators. Myocardial viability and survival in ischemic left ventricular dysfunction. N Engl J Med. 2011;364:1617–1625. doi: 10.1056/NEJMoa1100358. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mielniczuk L, Beanlands R. Imaging-guided selection of patients with ischemic heart failure for high risk revascularization improves identification of those with the highest clinical benefit. Circ Cardiovasc Imaging. 2012;5:262–270. doi: 10.1161/CIRCIMAGING.111.964668. [DOI] [PubMed] [Google Scholar]
- Ziadi MC, Garrard L, Beanlands R, Chow B, Hessian R, Ruddy T, Guo A, Williams K, Davies RA, Renaud J, Etele J, DaSilva JN, Ficaro FP, Wisenberg G, Iwanachko M, Marriott C. FDG PET impacts positively management direction and predicts outcomes in a multicentre ‘real world’ setting. Circulation. 2009;120:S349. [abstract] [Google Scholar]
- Liao L, Cabell CH, Jollis JG, Velazquez EJ, Smith WT 4th, Anstrom KJ, Pappas PA, Ryan T, Kisslo JA, Landolfo CK. Usefulness of myocardial viability or ischemia in predicting long-term survival for patients with severe left ventricular dysfunction undergoing revascularization. Am J Cardiol. 2004;93:1275–1279. doi: 10.1016/j.amjcard.2004.01.071. [DOI] [PubMed] [Google Scholar]
- Sawada SG, Dasgupta S, Nguyen J, Lane KA, Gradus-Pizlo I, Mahenthiran J, Feigenbaum H. Effect of revascularization on longterm survival in patients with ischemic left ventricular dysfunction and a wide range of viability. Am J Cardiol. 2010;106:187–192. doi: 10.1016/j.amjcard.2010.03.014. [DOI] [PubMed] [Google Scholar]
- K/DOQI clinical practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Am J Kidney Dis. 2002;39:S1–S266. [PubMed] [Google Scholar]
- Levey AS, Coresh J, Balk E, Kausz AT, Levin A, Steffes MW, Hogg RJ, Perrone RD, Lau J, Eknoyan G. National Kidney Foundation. National Kidney Foundation practice guidelines for chronic kidney disease: evaluation, classification, and stratification. Ann Intern Med. 2003;139:137–147. doi: 10.7326/0003-4819-139-2-200307150-00013. [DOI] [PubMed] [Google Scholar]
- O’Meara E, Chong KS, Gardner RS, Jardine AG, Neilly JB, McDonagh TA. The Modification of Diet in Renal Disease (MDRD) equations provide valid estimations of glomerular filtration rates in patients with advanced heart failure. Eur J Heart Fail. 2006;8:63–67. doi: 10.1016/j.ejheart.2005.04.013. [DOI] [PubMed] [Google Scholar]
- Earley A, Miskulin D, Lamb EJ, Levey AS, Uhlig K. Estimating equations for glomerular filtration rate in the era of creatinine standardization: A systematic review. Ann Intern Med. 2012;156:785–795. doi: 10.7326/0003-4819-156-11-201203200-00391. [DOI] [PubMed] [Google Scholar]
- Schinkel AF, Poldermans D, Elhendy A, Bax JJ. Assessment of myocardial viability in patients with heart failure. J Nucl Med. 2007;48:1135–1146. doi: 10.2967/jnumed.106.038851. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Left ventricular remodeling and biomarkers ancillary study – a synopsis.
Standardization and quality assurance (IMAGE-QA).


