Abstract
We report a case of rapid regression of extensive posterior capsule neovascularization in a 67-year-old diabetic male patient, who developed posterior capsule opacity with neovascularization one year post cataract surgery, after a single injection of intravitreal bevacizumab (Avastin) followed by neodymium:YAG capsulotomy. Rapid regression of the posterior capsule neovascularization, and visual improvement was observed 9 days after the intervention. Posterior capsulotomy was performed successfully without bleeding. Prior to posterior capsulotomy, intravitreal bevacizumab can result in rapid and dramatic regression of posterior capsule neovascularization.
Keywords: Anti-vascular endothelial growth factor (VEGF), Bevacizumab, Posterior capsule neovascularization
1. Introduction
Posterior capsule opacification and neovascularization has been reported as a rare condition that can happen in diabetic patients after extracapsular cataract extraction (Ulbig et al., 1993; Eifrig et al., 1990), after pars plana vitrectomy in diabetic patients (Lewis et al., 1987a,b; Ayata et al., 2007), or it can be idiopathic (Dowler et al., 2003). This condition is characterized by peripheral extraretinal vascular proliferation that extends along the anterior hyaloid to the posterior surface of the lens.
Vascular endothelial growth factor (VEGF) has been determined to be a major regulator of pathologic ocular angiogenesis. The treatment of ocular neovascular diseases can be represented by inhibition of VEGF (Boyd et al., 2002).
We report regression of posterior capsule neovascularization in diabetic patient following intravitreal bevacizumab injection.
2. Case report
A 67-year-old male patient was presented to King Khaled Eye Specialist Hospital with a long standing history of diabetes and systemic hypertension. He underwent uncomplicated combined trabeculectomy and phacoemulsification with posterior chamber intraocular lens (IOL) implantation in right eye, and then he received panretinal photocoagulation (PRP) in both eyes for the proliferative diabetic retinopathy, which resulted in regression of new vessels. He was presented one year after the cataract surgery complaining of decrease vision for the last 2 months in the right eye. Examination demonstrated best corrected visual acuity (VA) of 20/400 in the right eye with controlled intraocular pressure (IOP). Gonioscopy showed a normal anterior chamber angle with no angle neovascularization. Anterior segment examination showed no iris neovascularization, a posterior capsule opacity (PCO) with massive neovascularization on the capsule (Fig. 1). Fundus examination revealed neovascularization on the disc with no other retinal neovascularization. PCO precluded the application of panretinal laser photocoagulation. After a lengthy discussion of the potential risks and benefits of off-label bevacizumab use, the patient’s eye was prepped with a topical anesthetic and a drop of antibiotic before the injection. The eyelid margin was prepped with topical povidone and iodine solution. A wire speculum then was placed followed by several drops of diluted povidone and iodine solution to the conjunctiva at the injection site. A pars plana injection of 1.25 mg bevacizumab was injected into the right eye inferotemporally and 3.0 mm from the limbus to the mid-vitreous via a 30-gauge needle.
Figure 1.
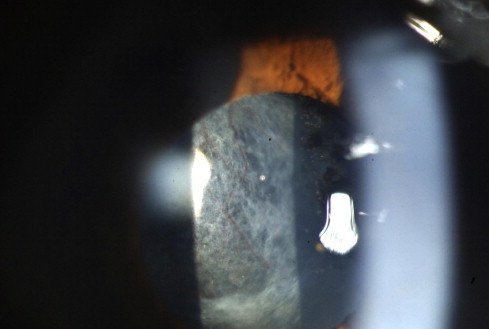
Slitlamp photomicrograph of the involved eye showing posterior capsule opacity with neovascularization.
After 9 days, neovascularization of the posterior capsule had resolved completely (Fig. 2), and the visual acuity was 20/125, with controlled IOP. Nd:YAG capsulotomy was performed followed by an augmentation of PRP in the right eye. Two weeks later, his visual acuity was 20/60 with no recurrence of vascularization was documented.
Figure 2.

Neovascularization of the posterior capsule had resolved completely – 9 days after intravitreal injection of bevacizumab.
3. Discussion
Posterior capsule neovascularization is a rare complication which can be caused by surgical intervention and systemic or ocular diseases (Ayata et al., 2007). The anterior extraretinal fibrovascular tissue uses the anterior vitreous as a support, extends toward the lens, contracts, and causes peripheral retinal and ciliary body traction detachment (Lewis et al., 1987b).
With intravitreal anti-VEGF therapy, we have obtained a valuable, and most promising, new treatment of ocular neovascularization. Bevacizumab (Avastin) is a humanized, full-length monoclonal antibody that inhibits all isoforms of VEGF. It is approved as an intravenous treatment for metastatic colorectal cancer in February 2004 (Martin et al., 2004). Several case series have shown promising results for using off-label intravitreal bevacizumab for the treatment of exudative age-related macular degeneration (Spaide et al., 2006; Bashshur et al., 2006; Avery et al., 2006; Rosenfeld et al., 2005), proliferative diabetic retinopathy (Spaide and Fisher, 2006), neovascular glaucoma (NVG) (Davidorf et al., 2006; Avery, 2006; Jayter et al., 2006), oedema from retinal vein occlusion (Boyd et al., 2002; Rosenfeld et al., 2005), and one single case of posterior capsule neovascularization (Eren et al., 2007).
In the previous reports about neovascularization of the capsule, other modalities of treatment were applied including argon laser photocoagulation of the vessels in the capsular bag, pars plana vitrectomy with removal of posterior capsule (Eifrig et al., 1990), cryoablation, endophotocoagulation of peripheral retina (Lewis et al., 1987a), membrane dissection with prophylactic placement of encircling band (Lewis et al., 1987b), and photodynamic therapy (Ayata et al., 2007).
The current case demonstrates that a single intravitreal bevacizumab injection may be associated with rapid regression of posterior capsule neovascularization. Very recently, one case report of posterior capsule neovascularization regressed by intravitreal bevacizumab injection was reported (Eren et al., 2007), and the published results are in full accordance with ours.
In conclusion, intravitreal injection of bevacizumab followed by Nd:YAG capsulotomy seemed to be a beneficial treatment modality in our particular patient in whom Nd:YAG capsulotomy alone can not be done due to the risk of bleeding.
References
- Avery R.L. Regression of retinal and iris neovascularization after intravitreal bevacizumab (Avastin) treatment. Retina. 2006;26:352–354. doi: 10.1097/00006982-200603000-00016. [DOI] [PubMed] [Google Scholar]
- Avery R.L., Pieramici D.J., Rabena M.D. Intravitreal bevacizumab (Avastin) for neovascular age-related macular degeneration. Ophthalmology. 2006;113:363–372. doi: 10.1016/j.ophtha.2005.11.019. [DOI] [PubMed] [Google Scholar]
- Ayata A., Unal M., Erşanli D., Gülecek O., Sönmez M. Photodynamic therapy for posterior capsule neovascularization. J. Cataract Refract. Surg. 2007;33:1131–1132. doi: 10.1016/j.jcrs.2007.02.025. [DOI] [PubMed] [Google Scholar]
- Bashshur Z.F., Bazarbachi A., Schakal A. Intravitreal bevacizumab for the management of choroidal neovascularization in age-related macular degeneration. Am. J. Ophthalmol. 2006;142:1–9. doi: 10.1016/j.ajo.2006.02.037. [DOI] [PubMed] [Google Scholar]
- Boyd S.R., Zachary I., Chakravarthy U. Correlation of increased vascular endothelial growth factor with neovascularization and permeability in ischemic central vein occlusion. Arch. Ophthalmol. 2002;120:1644–1650. doi: 10.1001/archopht.120.12.1644. [DOI] [PubMed] [Google Scholar]
- Davidorf F.H., Mouser J.G., Derick R.J. Rapid improvement of rubeosis iridis from a single bevacizumab (Avastin) injection. Retina. 2006;26:354–356. doi: 10.1097/00006982-200603000-00017. [DOI] [PubMed] [Google Scholar]
- Dowler J., Mehta J., Landers A. Idiopathic anterior hyaloid vessels. Br. J. Ophthalmol. 2003;87:365–366. doi: 10.1136/bjo.87.3.365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Eifrig D.E., Hermsen V., McManus P., Cunningham R. Rubeosis capsulare. J. Cataract Refract. Surg. 1990;16:633–636. doi: 10.1016/s0886-3350(13)80783-3. [DOI] [PubMed] [Google Scholar]
- Eren E., Küçükerdönmez C., Yilmaz G., Akova Y.A. Regression of neovascular posterior capsule vessels by intravitreal bevacizumab. J. Cataract Refract. Surg. 2007;33:1113–1115. doi: 10.1016/j.jcrs.2007.01.040. [DOI] [PubMed] [Google Scholar]
- Jayter S.P., Rodrigo J., Rogério A.C. Short-term results of intravitreal bevacizumab (Avastin) on anterior segment neovascularization in neovascular glaucoma. Acta Ophthalmol. Scand. 2006;84(4):556–557. doi: 10.1111/j.1600-0420.2006.00731.x. [DOI] [PubMed] [Google Scholar]
- Lewis H., Abrams G., Williams G. Anterior hyaloidal fibrovascular proliferation after diabetic vitrectomy. Am. J. Ophthalmol. 1987;104:607–613. doi: 10.1016/0002-9394(87)90173-5. [DOI] [PubMed] [Google Scholar]
- Lewis H., Abrams G., Foos R. Clinicopathologic findings in anterior hyaloidal fibrovascular proliferation after diabetic vitrectomy. Am. J. Ophthalmol. 1987;104:614–618. doi: 10.1016/0002-9394(87)90174-7. [DOI] [PubMed] [Google Scholar]
- Martin E., Sebastian S., Marc D. Anti-vascular tumor therapy: recent advances, pitfalls and clinical perspectives. Drug Resist. Updates. 2004;7:125–138. doi: 10.1016/j.drup.2004.03.001. [DOI] [PubMed] [Google Scholar]
- Rosenfeld P.J., Moshfeghi A.A., Puliafito C.A. Optical coherence tomography findings after an intravitreal injection of bevacizumab (Avastin) for neovascular age-related macular degeneration. Ophthalmol. Surg. Lasers Imag. 2005;36:331–335. [PubMed] [Google Scholar]
- Rosenfeld P.J., Fung A.E., Puliafito C.A. Optical coherence tomography findings after an intravitreal injection of bevacizumab (Avastin®) for macular oedema from central retinal vein occlusion. Ophthal. Surg. Lasers Imag. 2005;36:336–339. [PubMed] [Google Scholar]
- Spaide R.F., Fisher Y.L. Intravitreal bevacizumab (Avastin) treatment of proliferative diabetic retinopathy complicated by vitreous hemorrhage. Retina. 2006;26:275–278. doi: 10.1097/00006982-200603000-00004. [DOI] [PubMed] [Google Scholar]
- Spaide R.F., Laud K., Fine H.F. Intravitreal bevacizumab treatment of choroidal neovascularization secondary to age-related macular degeneration. Retina. 2006;26:383–390. doi: 10.1097/01.iae.0000238561.99283.0e. [DOI] [PubMed] [Google Scholar]
- Ulbig M.R., Hykin P.G., Foss A.J. Anterior hyaloidal fibrovascular proliferation after extracapsular cataract extraction in diabetic eyes. Am. J. Ophthalmol. 1993;115:321–326. doi: 10.1016/s0002-9394(14)73582-2. [DOI] [PubMed] [Google Scholar]


