Abstract
This is a report of two brothers who underwent bilateral photorefractive keratectomy and developed bilateral peripheral corneal infiltrate on the third day following surgery. The patients were treated with antibiotics and low concentration steroid until negative culture was reported 48 h later, when intensive topical steroid was started. The infiltrate resolved by day 10 with residual subepithelial haze that was apparent 8 months after surgery. Sterile infiltrate has been reported as complication of photorefractive keratectomy and can be managed successfully with excellent outcome. The fact that it happened in two brothers may raise the possibility of genetic predisposition.
Keywords: Photorefractive keratectomy, Corneal infiltrate, Sterile infiltrate, Nonsteroidal anti-inflammatory drug, Bandage contact lenses
1. Introduction
Photorefractive keratectomy (PRK) was the first widely accepted surgical procedure to correct refractive errors in the late 1980s. Since PRK had limitation including discomfort or pain in the first few days, prolonged wound healing and visual rehabilitation, and stromal haze, laser in situ keratomileusis (LASIK) has become the dominant refractive procedure worldwide in the early 1990s. With more cases of keratoectasia following LASIK reported (Randleman, 2006) and the microkeratome related complication (Melki and Azar, 2001), surface ablation treatment using PRK, laser-assisted subepithelial keratomileusis (LASEK), and Epi-LASIK gained the interest of many refractive surgeons. The use of mitomycin (MMC) (Trattler and Barnes, 2008) with surface ablation treatment for moderate to high refractive errors to decrease stromal haze made surface ablation to be a widely accepted procedure for a wide range of refractive error worldwide.
Corneal infiltrate following PRK can be infectious and sterile and may affect the vision. Peripheral sterile corneal infiltrate have been reported following PRK (Teal et al., 1995; Rao et al., 2000), PTK (Teichmann et al., 1996), LASEK (Lifshitz et al., 2005), and LASIK (Lahners et al., 2003; Ambrosio et al., 2003; Yu et al., 2002). Recognition of sterile infiltrate is important to avoid aggressive scraping and it usually ends with an excellent visual outcome. Sterile corneal infiltrate has no definite cause yet. To my knowledge, there are no reported cases of sterile corneal infiltrate in more than one family member following laser refractive surgery.
2. Case reports
2.1. Case 1
Nineteen-year-old man sought refractive surgery to correct myopia. Ocular and medical history was unremarkable. Uncorrected visual acuity was CF in both eyes. Best spectacle-corrected visual acuity was 20/20 in both eyes with refraction of −4.00 D −0.75 D × 105 in the right eye and −4.00 D −0.75 D × 95 in the left eye. Patient has stable refractive error for two years. External eye exam, slit lamp examination and fundus examination were normal. Preoperative corneal topography and elevation map was within normal limit. Corneal pachymetry was 508 μm in the right eye and 514 μm in the left eye. PRK with MMC was offered.
2.2. Case 2
Twenty-two-year-old man sought refractive surgery to correct myopia. Ocular and medical history was unremarkable. Uncorrected visual acuity was 20/200 in both eyes. Best spectacle-corrected visual acuity was 20/20 in both eyes with refraction of −4.00 D −0.25 × 20 in the right eye and −4.00 D −0.5 D × 160 in the left eye. Patient has stable refractive error for three years. External eye exam, slit lamp examination and fundus examination were normal. Preoperative corneal topography and elevation map was within normal limit. Corneal pachymetry was 474 μm in the right eye and 476 μm in the left eye. PRK with MMC was offered.
2.3. Surgical technique
Both patients had uneventful bilateral PRK with MMC. Thirty minutes before surgery, an ofloxacin 0.3% drop was administered three times at 10 min interval. Proparacaine 2% eye drops were used to anesthetize the ocular surface. The patient’s face was prepped with povidone-iodine 10%. The eyelashes were isolated using sterile drape. A 9.0 mm trephine, centered on the pupil was used to mark corneal epithelium. Twenty percent of alcohol was applied using reservoir ring for 30 s then irrigation with balance salt solution (BSS) was done. Corneal epithelium was removed using blunt scraper, and stromal ablation was done using Allegretto Wave Eye-Q Blue Line excimer laser (Wavelight Technologies, Erlangen, Germany), with 6 mm optical zone, 1.25 mm transition zone and 8.5 mm ablation zone. The ablation depth for case 1 was 63 μm in both eyes and for case 2, it was 52 μm in the right eye and 54 μm in the left eye. MMC 0.02% was applied for 10 s using merocel sponge then vigorous irrigation with BSS was done. Soft contact lenses were applied and one drop of diclofenac ophthalmic eye drop and ofloxacin 0.3% was applied.
Postoperative medications include ofloxacin 0.3% four times/day, fluorometholone four times/day and lubricating eye drops every 2 h.
Patients were seen on day one. They were in severe pain with tearing and photophobia. Visual acuity was 20/100 in the right eye and 20/60 in the left eye for case 1 and 20/20 in the right eye and 20/40 in the left eye for case 2. Slit lamp examination revealed corneal epithelial defect 6–7 mm in both eyes, deep and quite anterior chamber, injected conjunctive and the contact lenses were in place. Diclofenac ophthalmic eye drops, four times/day, were started to decrease pain for both patients. Patients were seen on day three with pain and photophobia. Visual acuity was 20/60 in the right eye and 20/80 in the left eye for case 1 and 20/28.5 in the right eye and 20/28.5 in the left eye for case2. In case 1, slit lamp examination revealed an incomplete ring shaped creamy white infiltrate outside the treatment zone with intact corneal epithelium over the infiltrate and intervening clear zone between the infiltrate and the limbus (Fig. 1), 5.0 mm central corneal epithelial defect, quite anterior chamber, and 2+ conjunctival injection in the right eye. For the left eye, patient had two peripheral creamy white infiltrates inferiorly outside treatment zone with intact corneal epithelium over the infiltrate and intervening clear zone between the infiltrate and the limbus, quite anterior chamber, and 2+ conjunctival injection. In case 2, slit lamp examination revealed an incomplete ring shaped creamy white infiltrate outside treatment zone with intact corneal epithelium over the infiltrate and intervening clear zone between the infiltrate and the limbus, 4.0–5.0 mm central corneal epithelial defect, quite anterior chamber, and 2+ conjunctival injection in the right eye. For the left eye, patient had an incomplete ring shaped creamy white infiltrate outside treatment zone with intact corneal epithelium over the infiltrate and intervening clear zone between the infiltrate and the limbus (Fig. 2), quite anterior chamber and 2+ conjunctival injection. The clinical pictures indicate sterile corneal infiltrate. Corneal scarping was done for the right eye in both cases and specimens were sent for gram and giemsa staining, and bacterial and viral cultures. Ofloxacin 0.3% was increased to every 1 h, fluorometholone and lubricating eye drops were continued four times a day. A Diclofenac ophthalmic drop was stopped. Two days later, culture results came back negative and ofloxacin eye drops were decreased to every 2 h and Prednisolone acetate 1% was started every 1 h. Corneal epithelial defect healed by day six in both eyes in case 1 and by day five in both eyes in case 2 and contact lenses were removed. The infiltrate disappeared after 10 days in cases 1 and 2 leaving anterior stromal haze. Topical ofloxacin was stopped after 2 weeks and the Prednisolone acetate 1% was tapered over 1 month. Eight months after surgery, both patients had uncorrected visual acuity of 20/20 in both eyes. Slit lamp examination revealed faint stromal haze peripherally.
Figure 1.

Case 1: slit lamp photography of the right eye 5 days after PRK. Note the incomplete ring shaped creamy white infiltrate outside treatment zone.
Figure 2.
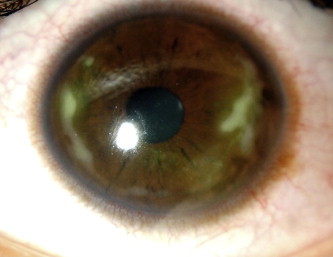
Case 2: slitlamp photography of the left eye 5 days after PRK. Note the incomplete ring shaped creamy white infiltrate outside treatment zone.
3. Discussion
Sterile corneal infiltrate has been reported after PRK (Teal et al., 1995; Rao et al., 2000), PTK (Teichmann et al., 1996), LASEK (Lifshitz et al., 2005), and LASIK (Lifshitz et al., 2005; Lahners et al., 2003; Ambrosio et al., 2003; Yu et al., 2002) with no definite cause. The reports of sterile infiltrate after laser refractive surgery appear to describe a similar entity. The typical presentation in these reports is severe pain, ciliary injection, and subepithelial white infiltrates in the treated area or outside treatment zone. The infiltrate occurs on the first to third postoperative day and sometimes associated with immune rings. The reported incidence of sterile infiltrate after PRK is about 1 in 250 cases (Teal et al., 1995). Corneal scrapings are culture negative, and the condition responds to therapy with topical steroids with or without antibiotics. Resolution is usually accompanied by corneal stromal scarring.
The etiology of these sterile infiltrate is unknown. Nonsteroidal anti-inflammatory drugs (NSAIDs), bandage contact lenses, immune reaction, and culture negative infection are possible causes (Haw and Manche, 1999).
Topical NSAIDs may play a role in the development of sterile infiltrate after laser surface ablation. NSAIDs inhibit the cyclooxygenase pathway of arachidonic acid metabolism. The lipoxygenase pathway is still functioning, and this causes excessive production of leukotrienes. These are potent neutrophil chemotactants and result in accumulation of these cells in the corneal stroma, producing infiltrate (Rao et al., 2000; Ku et al., 1986). The use of steroid blocks, the synthesis of the precursor arachidonic acid, and hence the concomitant use of steroid are recommended when NSAIDs are used after excimer surgery (Sher et al., 1994). NSAIDs are not likely to be the cause of the reported sterile infiltrate after laser refractive surgery as sterile corneal infiltrate continued to appear after LASIK (Lifshitz et al., 2005) and PRK (Rao et al., 2000) cases although NSAID was not used.
Contact lenses induced hypoxia can lead to sterile corneal infiltrate (Teal et al., 1995; Donshik et al., 1995; Baum and Dabezies, 2000). Earlier reports of sterile infiltrate after PRK (Teal et al., 1995) proposed that corneal infiltrate might be secondary to the use of contact lenses. However, recent reports of sterile corneal infiltrate after LASIK (Lifshitz et al., 2005) and PRK (Rao et al., 2000) without using contact lenses indicate that contact lenses may not be the cause of the sterile corneal infiltrate after laser refractive surgery.
Rao et al. (2000) proposed that manipulation of lid margin results in an increased expression of meibomian secretions and bacterial toxins which can trigger immunological reaction with an occurrence of infiltration. Since lid inflammation is common and if this theory is true we should see more sterile corneal infiltrate after refractive surgery or any ocular surgery with lid manipulation.
Teichmann et al. (1996) proposed that mammalian tissues and micro-organisms release heat shock proteins (HSPs) when subjected to physical, chemical, or biological stress. They hypothesize that the interaction between circulating antibodies against bacterial HSPs (formed from previous exposure) and corneal HSPs produced after laser treatment can result in corneal infiltration. The fact that sterile corneal infiltrate was reported after LASIK (Lifshitz et al., 2005; Lahners et al., 2003; Ambrosio et al., 2003; Yu et al., 2002), LASEK (Lifshitz et al., 2005), PRK (Teal et al., 1995; Rao et al., 2000), PTK (Teichmann et al., 1996), and Intralase LASIK (Lifshitz et al., 2005) where they all share laser exposure may support the idea of HSPs as the antigen triggering the immune reaction. Since thousands of laser refractive surgeries are done, we rarely see sterile corneal infiltrate although HSPs should be released in all cases. This may indicate that sterile corneal infiltrate may occur in selected patients with sensitive immune system who may develop antibodies against HSPs. The occurrence of sterile corneal infiltrate in brothers after PRK may support the theory of HSPs triggering inflammation in patients who are genetically predisposed. I believe this idea is worth further study to find if people who develop sterile corneal infiltrate are predisposed to other immunogenic reaction following physical or chemical stress.
In conclusion, sterile corneal infiltrate after laser refractive surgery is a rare complication and the exact cause and mechanism are not clear. All the reported cases showed similar signs which can help in early diagnosis. Topical steroid is the treatment of choice and should be initiated early to minimize the residual scar. We elected to do scraping for one eye and not to start intensive topical steroid until culture result was back. We avoided doing aggressive scraping and fortified antibiotic, and we ended with an excellent visual outcome. Topical steroid can be initiated early without corneal scraping once sterile infiltrate is seen. However, we should maintain a high degree of suspicion for infectious cases.
References
- Ambrosio R.J., Periman L.M., Netto M.V., Wilson S.E. Bilateral marginal sterile infiltrates and diffuse lamellar keratitis after laser in situ keratomileusis. J. Refract. Surg. 2003;19:154–158. doi: 10.3928/1081-597X-20030301-11. [DOI] [PubMed] [Google Scholar]
- Baum J., Dabezies O.H., Jr. Pathogenesis and treatment of “sterile” midperipheral corneal infiltrates associated with soft contact lens use. Cornea. 2000;19(6):777–781. doi: 10.1097/00003226-200011000-00003. [DOI] [PubMed] [Google Scholar]
- Donshik P.C., Suchecki J.K., Ehlers W.H. Peripheral corneal infiltrates associated with contact lens wear. Trans. Am. Ophthalmol. Soc. 1995;93:49–60. discussion 4. [PMC free article] [PubMed] [Google Scholar]
- Haw W.W., Manche E.E. Sterile peripheral keratitis following laser in situ keratomileusis. J. Refract. Surg. 1999;15:61–63. doi: 10.3928/1081-597X-19990101-11. [DOI] [PubMed] [Google Scholar]
- Ku E.C., Lee W., Kothari H.V., Scholer D.W. Effect of diclofenac sodium on the arachidonic acid cascade. Am. J. Med. 1986;80(4B):18–23. doi: 10.1016/0002-9343(86)90074-4. [DOI] [PubMed] [Google Scholar]
- Lahners W.J., Hardten D.R., Lindstorm R.L. Peripheral keratitis following laser in situ keratomileusis. J. Refract. Surg. 2003;19:671–675. doi: 10.3928/1081-597X-20031101-10. [DOI] [PubMed] [Google Scholar]
- Lifshitz T., Levy J., Mahler O., Levinger S. Peripheral sterile corneal infiltrates after refractive surgery. J. Cataract Refract. Surg. 2005;31:1392–1395. doi: 10.1016/j.jcrs.2004.12.057. [DOI] [PubMed] [Google Scholar]
- Melki S.A., Azar D.T. LASIK complications: etiology, management, and prevention. Surv. Ophthalmol. 2001;46:95–116. doi: 10.1016/s0039-6257(01)00254-5. [DOI] [PubMed] [Google Scholar]
- Randleman J.B. Post-laser in-situ keratomileusis ectasia: current understanding and future directions. Curr. Opin. Ophthalmol. 2006;17:406–412. doi: 10.1097/01.icu.0000233963.26628.f0. [DOI] [PubMed] [Google Scholar]
- Rao S.K., Fogla R., Rajagopal R. Bilateral corneal infiltrates after excimer laser photorefractive keratectomy. J. Cataract Refract. Surg. 2000;26:456–459. doi: 10.1016/s0886-3350(99)00348-x. [DOI] [PubMed] [Google Scholar]
- Sher N.A., Krueger R.R., Teal P. Role of topical corticosteroids and nonsteroidal antiinflammatory drugs in the etiology of stromal infiltrates after excimer photorefractive keratectomy. J. Refract. Corneal Surg. 1994;10:587–588. [PubMed] [Google Scholar]
- Teal P., Breslin C., Arshinoff S., Edmison D. Corneal subepithelial infiltrates following excimer laser photorefractive keratectomy. J. Cataract Refract. Surg. 1995;21:516–518. doi: 10.1016/s0886-3350(13)80208-8. [DOI] [PubMed] [Google Scholar]
- Teichmann K.D., Cameron J., Huaman A. Wessely-type immune ring following phototherapeutic keratectomy. J. Cataract Refract. Surg. 1996;22:142–146. doi: 10.1016/s0886-3350(96)80284-7. [DOI] [PubMed] [Google Scholar]
- Trattler W.B., Barnes S.D. Current trends in advanced surface ablation. Curr. Opin. Ophthalmol. 2008;19:330–334. doi: 10.1097/ICU.0b013e3283034210. [DOI] [PubMed] [Google Scholar]
- Yu E.Y.W., Rao S.K., Cheng A.C.K. Bilateral peripheral corneal infiltrates after simultaneous myopic laser in situ keratomileusis. J. Cataract Refract. Surg. 2002;28:891–894. doi: 10.1016/s0886-3350(01)01095-1. [DOI] [PubMed] [Google Scholar]


