Abstract
Primary Diffuse Large B-cell Lymphoma (DLBCL) represents the 2nd most common lymphoma occurring in the orbit, after Mucosal Associated Lymphoid Tissue (MALT) lymphoma. A total of 5 cases of ocular adnexal DLBCL were diagnosed over 25 years of experience at our tertiary eye care center. Two cases involved the lacrimal sac and one case involved the lacrimal gland. In this paper we are presenting the remaining 2 non-lacrimal cases of DLBCL. The first case is a 32 year old male who was referred with a slowly growing, painless mass involving the left medial canthal area as a case of dacryocystitis. The mass was found to be extending into the orbit inferiorly with upward displacement of the left globe. The second case is a 65 year-old lady who presented with unilateral proptosis as a result of a right orbital mass extending to the orbital apex. Histopathologic examination and immunohistochemical analysis of the incisional biopsy in both cases confirmed the diagnosis of Diffuse Large B-cell Lymphoma (DLBCL).
Keywords: B-cell lymphoma, Large cell, Orbit
Introduction
Lymphoproliferative disease of the orbit includes a wide range of disorders including lymphoid hyperplasia and indolent lymphomas. Primary Diffuse Large B-cell Lymphoma (DLBCL) represents the 2nd most common lymphoma occurring in the orbit, after Mucosal Associated Lymphoid Tissue (MALT) lymphoma. The diagnosis requires careful clinical, radiological, histopathological and immunohistochemical examination.1
Five cases of ocular adnexal DLBCL cases were diagnosed in our institution over a 25-year experience. Two cases involved the lacrimal sac, one case involved the lacrimal gland and the remaining last 2 cases showed different non-lacrimal orbital involvement. We are reporting these 2 cases of DLBCL with an overall clinical, histopathologic and radiologic data. Both cases presented initially with ophthalmic manifestations and no history of systemic lymphoma. The mass in the first case involved the inferior orbit with no proptosis but visible extension to left lacrimal sac area and the case was referred as dacryocystitis. The second case presented with a typical right orbital mass resulting in unilateral proptosis. The systemic work up in the first case was completely negative, thus this lesion was considered primary. Work up of the second case revealed mediastinal lymphadenopathy indicating a possible secondary orbital involvement.
Case 1
A 32 year old male was referred by a general ophthalmologist as a non-urgent case of left chronic dacryocystitis. The patient gave a history of tearing and a slowly growing, painless swelling just near the left medial canthal area for several months. There was no history of trauma, blood transfusion or extramarital exposure. No history of fever, weight loss or other systemic symptoms. Past medical and drug history were not significant. Family history was also unremarkable.
On examination, the best corrected visual acuity was 20/20 in both the eyes. The intraocular pressure (IOP) was 16 mmHg in each eye. Examination of the right eye was within normal limit. External examination of the left eye revealed fullness of left lower lid involving the medial canthal area. A palpable tender firm mass was felt extending from the medial canthus to the anterior part of the orbit just inferior to the left globe (Fig. 1a). The globe was displaced upward with no evidence of proptosis. Regurgitation from upper and lower puncta was negative. Ocular motility was full. The remaining ocular examination was within normal limits. His systemic examination revealed no abnormality.
Figure 1a.
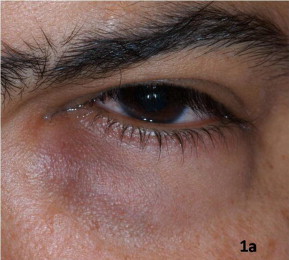
The clinical appearance of the left medial canthal area swelling in case 1.
A Computerized Tomography (CT) scan of the left orbit showed a mass with intermediate attenuation measuring 2.9 × 2.8 cm in the left inner canthus region in close proximity to the lacrimal sac (Fig. 1b). Magnetic Resonance Imaging (MRI) of the left orbit showed a soft tissue mass of intermediate signal intensity on T1 and T2 weighted images in the area of the left lacrimal sac with intra-orbital, extra-conal component, all measuring 3 × 1.8 cm (Fig. 1c). The globe was pushed laterally with abnormal contour of its wall medially. The mass showed mild homogenous contrast enhancement except for a non-enhancing center.
Figure 1b.

Computerized tomography (Axial) of the left orbit with contrast enhancing mass medially (red arrow).
Figure 1c.
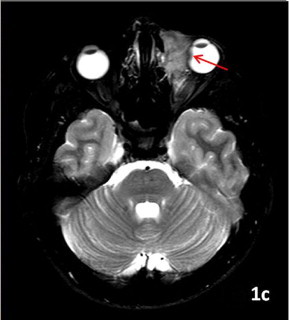
Axial T2 weighed magnetic resonance image of the left orbital lesion. Note the globe indentation by the mass (red arrow).
The patient underwent debulking of the lesion through a lower eyelid incision. The mass was found intra-operatively to be separate from the lacrimal sac. The Histopathologic examination revealed diffuse proliferation of sheets of large lymphocytes with frequent mitotic figures. The cells showed evidence of pleomorphism with vesicular nuclei and prominent nucleoli (Fig. 2a). The immunohistochemical staining showed that the cells were CD20, Bcl2 and Ki-67 positive (Figs. 2b,c,d) while negative to CD10. The differential histopathologic diagnosis based on the morphology included Diffuse Large B-Cell Lymphoma (DLBCL) and Burkitt lymphoma, however the immunohistochemical staining (specifically the strong positivity to CD 20 and the negative CD10) supported the diagnosis of DLBCL. The specimen was also submitted for FISH analysis for c-myc translocation, which was negative, thus ruling out the diagnosis of Burkitt lymphoma.
Figure 2a.
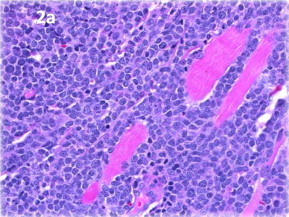
Histopathologic appearance of the diffuse large lymphocytes infiltrating the muscle in case 1, (original magnification ×400, hematoxylin and eosin).
Figure 2b.
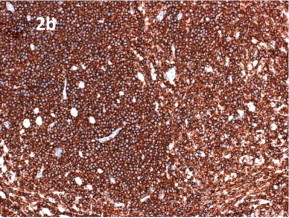
Positive staining of these lymphocytes with CD20 stain (original magnification ×200).
Figure 2c.
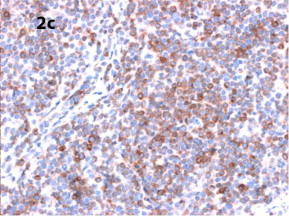
Similar positive staining with Bcl2 (original magnification ×400).
Figure 2d.
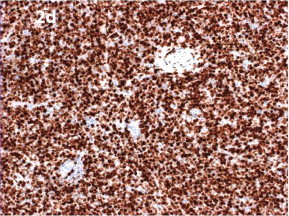
Strong positive staining of the cells with Ki67 (original magnification ×200).
Further systemic workup- including complete blood cell count; CT scan of the head, neck, chest and abdomen; bone marrow aspirate and biopsy – did not reveal any evidence of systemic lymphoma. Thus, this was considered as primary orbital lesion and staged as 1-A. The patient received 3 courses of R-CHOP chemotherapy as a preferred therapy. He tolerated the chemotherapy with good response and no complication (Fig. 1d). The patient is on regular follow-up without evidence of local recurrence or advanced disease up to 15 months after his treatment.
Figure 1d.
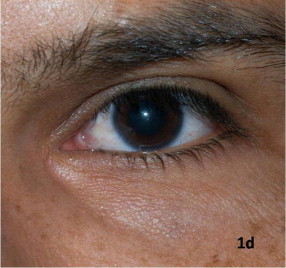
The clinical appearance of the same patient showing resolved swelling following treatment.
Case 2
A 65-year old Saudi lady presented with the history of painless progressive proptosis of her right eye over 3 months. There was no history of trauma or significant medical illness. The patient however, noticed weight loss over the last few months. Examination of the right eye showed visual acuity of 20/40 with pinhole with normal anterior segment findings and intraocular pressure of 17 mmHg. External examination revealed 4 mm of right proptosis (by Hertel Exophthalmometer at base 94). Her extraocular motility was full and there was no diplopia in any gaze. Her systemic work up revealed mild anemia.
Her MRI showed a right orbital heterogenous mass measuring 2.5 × 2 cm with low signal intensity on T1 and T2-weighted images. The mass was located between the lateral and inferior recti extending along the lateral orbital wall without extension into the optic canal. There was no globe indentation. The mass showed ring contrast enhancement (Fig. 3a).
Figure 3a.
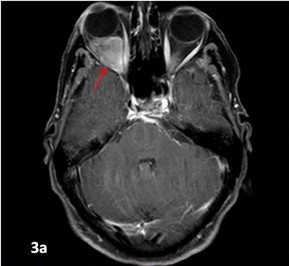
Axial T1 weighed magnetic resonance image of the right orbital mass with the ring of contrast enhancement in the second case (red arrow).
Incisional biopsy of the mass through lateral orbitotomy was performed. The histopathologic examination showed diffuse sheets of large cells with irregular nuclear membrane and prominent nuclei. Numerous mitotic figures and intervening apoptotic cells were also noted. In focal areas, small mature lymphocytes were also observed. The cells infiltrated the orbital fat (Fig. 3b). The cells showed strong positive staining with CD20 (Fig. 3c). Scattered lymphocytes showed positive staining with CD3 (Fig. 3d). Full systemic work up was performed and her final diagnosis was DLBCL possibly secondary in the orbit with mediastinal lymphadenopathy. She was referred for systemic treatment and was started on R-CHOP cycles with no further available follow-up.
Figure 3b.
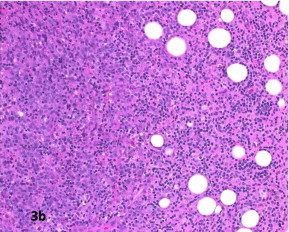
Diffuse large lymphocytes in the histopathologic sections of the lesion in case 2. Note the infiltration of the orbital fat (original magnification ×200, hematoxylin and eosin).
Figure 3c.
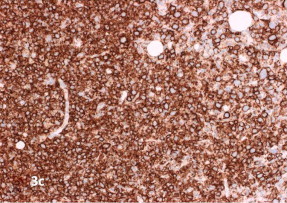
Almost all the cells show positive staining with CD20 (original magnification ×200).
Figure 3d.
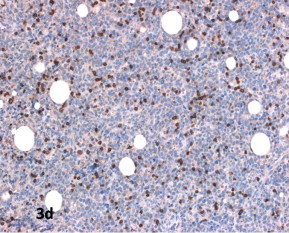
Focal positivity with CD3 (original magnification ×200).
Discussion
Lymphoma is the most frequent malignant tumor in the orbit. It accounts for 11% of all orbital tumors and 55% of malignant tumor.2
Orbital lymphomas are usually primary, however they are rare. Only about 5% of the patients with disseminated non-Hodgkin lymphoma (NHL) have secondary orbital involvement.3
Primary lymphoproliferative disease of the orbit is a heterogeneous condition, representing a spectrum of disease from lymphoid hyperplasia, through indolent lymphomas, such as Extranodal Marginal Zone Lymphoma (EMZL) and follicular lymphoma, to more malignant types, such as diffuse large B-cell lymphoma (DLBCL) and mantle cell lymphoma.1
Primary orbital and periorbital DLBCL is an uncommon form of NHL. DLBCL represents the 2nd most common lymphoma occurring in the orbit, after Mucosal Associated Lymphoid Tissue (MALT) lymphoma.1,2,4 In our institution, only 5 cases were diagnosed over a 25-year period of ophthalmic clinical practice.
Orbital lymphoma presents clinically as a painless, slowly progressive, unilateral or bilateral mass with a median age of presentation after the 5th decade and a mean age of 60 years at the time of diagnosis. The most frequent clinical presentation includes palpebral or orbital mass and exophthalmos.2 Our second case presented with proptosis at the age of 65 years. The interval between the onset of symptoms and diagnosis of orbital lymphomas was 1–2 months in the cases reported by Rey-Porca.2 Our first case is unique because of earlier presentation in the 3rd decade of life and relatively longer interval of proper diagnosis (7 months) due to the location of the lymphoma which has led to the initial misdiagnosis of chronic dacryocystitis. Nirupma reported a similar case in a young adult with painful progressive proptosis.3
S Morley reported 2 cases of orbital plasmablastic lymphoma (PBL) as a new entity of large cell lymphoma of the orbit which is more rapidly progressive and is associated with wider local disease at presentation. It was suggested in the report that painful proptosis and periocular sensory loss in PBL can possibly be used to differentiate this entity from DLBCL.5 T-cell/histiocyte-rich large B-cell lymphoma is an uncommon variant of DLBCL which has been recently described as a primary orbital lymphoma in a 37 year old male.6
Radiotherapy alone has been commonly used as a treatment modality of ocular adnexal lymphoma, however systemic chemotherapy is favored for orbital/periorbital DLBCL.7 Localized ocular adnexal DLBCL, treated using modern chemotherapy/immunotherapy is generally associated with a good prognosis.1 We have observed a good outcome and disease-free follow-up period of 15 months in our first case.
In conclusion, orbital DLBCL seems to be rare with only few cases encountered in our institution. Further detailed study on the occurrence of ocular adnexal lymphoproliferative disorders in our area is essential. It is important for general ophthalmologist to be familiar with this type of periocular pathology in order to avoid delays in the proper diagnosis. Early detection is also important because it is potentially a curable disease.
Footnotes
This paper is acknowledged by the Research Dept in our institution: ‘‘RP 1123-CR’’.
References
- 1.Madge S.N., McCormick A., Patel I., Hatef E., Menon V., Prabhakaran V.C., Irion L., Bonshek R., Honovar S., Leatherbarrow B., Esmaeli B., Selva D. Ocular adnexal diffuse large B-cell lymphoma: local disease correlates with better outcomes. Eye. 2010;24(6):954–961. doi: 10.1038/eye.2009.283. [DOI] [PubMed] [Google Scholar]
- 2.Rey-Porca C., Pérez-Encinas M., González F. Orbital lymphomas, presentation of nine cases. Arch Soc Esp Oftalmol. 2008;83(2):95–103. doi: 10.4321/s0365-66912008000200007. [DOI] [PubMed] [Google Scholar]
- 3.Lal N., Bisen S., Sucheta V. Primary large B-cell lymphoma of the orbit: a case report and review of literature. Indian J Pathol Microbiol. 2007;50(3):575–576. [PubMed] [Google Scholar]
- 4.Tranfa F., Di Matteo G., Strianese D., Forte R., Bonavolontà G. Primary orbital lymphoma. Orbit. 2001;20(2):119–124. doi: 10.1076/orbi.20.2.119.2633. [DOI] [PubMed] [Google Scholar]
- 5.S Morley A.M., Verity D.H., Meligonis G., Rose G.E. Orbital plasmablastic lymphoma- Comparison of a newly reported entity with diffuse large B-cell lymphoma of the orbit. Orbit. 2009;28(6):425–429. doi: 10.3109/01676830903177427. [DOI] [PubMed] [Google Scholar]
- 6.Kim U.R., Shah A.D., Shanti R., Arora V. Primary T cell/histiocyte-rich large B-cell lymphoma of the orbit. Ophthal Plast reconstr Surg. 2010;0(0):1–2. doi: 10.1097/IOP.0b013e3181c53d23. [DOI] [PubMed] [Google Scholar]
- 7.Esmaeli B., Ahmadi M.A., Manning J., McLaughlin P.W., Ginsberg L. Clinical presentation and treatment of secondary orbital lymphoma. Opthal Plast Reconstr Surg. 2002;18(4):247–253. doi: 10.1097/00002341-200207000-00003. [DOI] [PubMed] [Google Scholar]


