Abstract
Purpose
To estimate the prevalence of acute appendicitis and the relationship between pregnancy and acute appendicitis among South Korean women in 2009.
Methods
This was a cross-sectional study over 1 year period using a national registry data. We analyzed a national patient sample (n = 1,116,040) from a database complied by the South Korean National Health Insurance in 2009.
Results
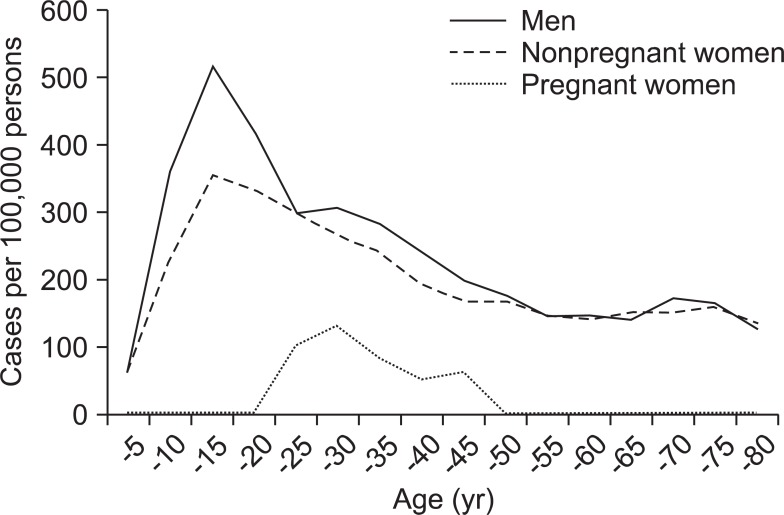
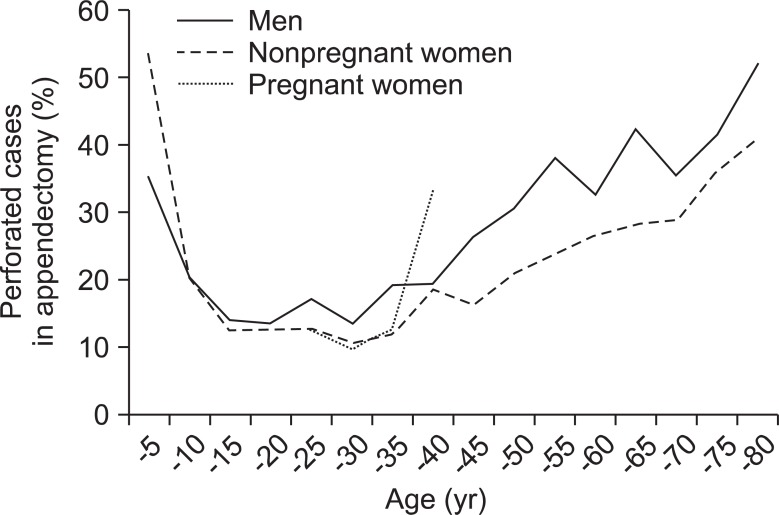
We identified 15,974 cases of acute appendicitis from 2009. The prevalence rate of acute appendicitis was 228 ± 2 per 100,000 persons. The prevalence in men was higher than in women. The peak prevalence of the disease in both genders occurred in patients aged 10 to 14 years. After that, prevalence declined with age. The prevalence of acute appendicitis in women aged 20 to 39 years was negatively associated with age and pregnancy (P < 0.001) but was not associated with socioeconomic status. The prevalence of perforated appendicitis cases by age is represented by a U-shaped curve. The prevalence was highest in people less than five years of age and in people older than 60 years.
Conclusion
We found that the prevalence of acute appendicitis decreased with increasing age after early teens, and that the prevalence of acute appendicitis in pregnant women was lower than in nonpregnant women.
Keywords: Aging, Appendicitis, Pregnancy, Prevalence
INTRODUCTION
Appendicitis is the most common indication in emergency abdominal surgery [1]. The appendix is a diverticulum of the cecum; appendicitis is inflammation of the appendix. Acute appendicitis is thought to occur as a result of an obstruction of the appendiceal lumen. Obstruction is most commonly caused by a fecalith, which results from accumulation and inspissation of fecal material and inorganic salts within the appendiceal lumen [2-4].
One study concluded that the highest prevalence of appendicitis was found in persons aged 10 to 19 years, affecting about 233/100,000 people in the population. They also found that males had higher rates of appendicitis than females across all age groups [1].
Diagnosing appendicitis in pregnant women is more challenging than in nonpregnant women [5]. We do not know what causes this difficulty-whether it is physiologic changes or environmental changes associated with pregnancy that instigate the pathogenesis that underlies acute appendicitis. To date, there is a lack of research with a large sample size that explores the relationship between acute appendicitis and pregnancy.
The health insurance system in South Korea is different from that in the United States. All South Koreans are obligated by law to apply to the National Health Insurance Corporation (NHIC, http://www.nhic.or.kr/static/html/wbd/g/a/wbdga0101.html). All medical institutions in South Korea ask NHIC to pay patient medical fees, with the exception of some procedures, such as cosmetic surgery. The Korean Health Insurance Review and Assessment Service (HIRA, http://www.hira.or.kr/eng/) is responsible for reviewing all medical fees sponsored by NHIC. HIRA reviews data for almost all general diseases in South Korea, so the HIRA data that we consulted for our analysis is probably fairly representative of the South Korean disease burden.
The aim of this study is to estimate the prevalence of acute appendicitis and the relationship between pregnancy and acute appendicitis among South Korean women in 2009.
METHODS
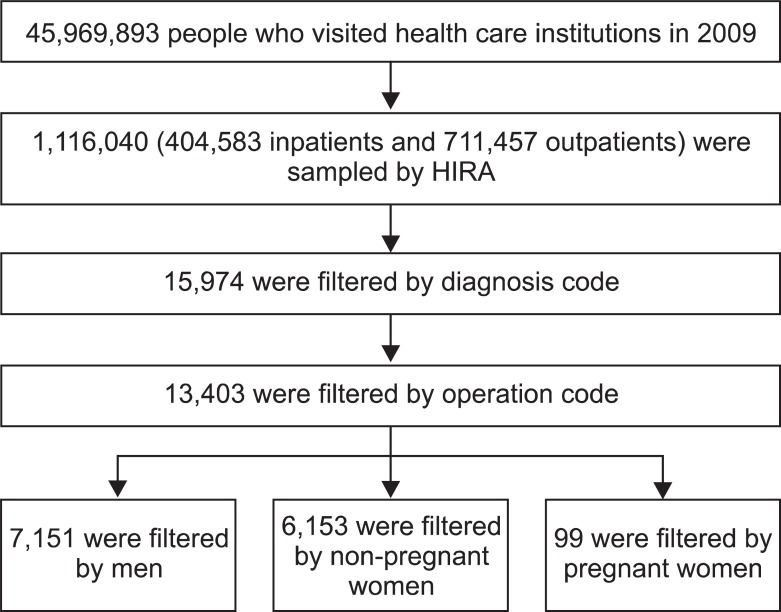
We analyzed data from the National Patients Sample collected by the Korean Health Insurance Review and Assess ment Service (HIRA-NPS) (serial number: HIRA-NPS-2009-0066). The HIRA previously demonstrated the validity of comparing HIRA-NPS and the South Korean population in general [6]. Almost all data (99.9%) were processed electronically [6]. HIRA-NPS used the stratified random sampling method for gender and age from all patients (including inpatients and outpatients, 45,969,893 people) who visited health care insti tutions in 2009. The total sample size from the HIRA-NPS is 1,116,040 people, including 404,583 inpatients (13% of inpatient population) and 711,457 outpatients (1% of outpatient population). This following data are included in HIRA-NPS: diagnosis, surgery or medical therapy, mortality, inpatient or outpatient, type of insurance, medical expenses, operation name, and prescription.
We used the Korean Standard Classification of Diseases, 5th edition and the Health Insurance Medical Care Expenses (HIMCE, 2012) to determine the total number of acute appendicitis cases. Procedure codes for acute appendicitis, based on HIMCE, include: Q2861, simple appendectomy; Q2862, perforated appendectomy; Q2863, removal of appendiceal abscess with periappendiceal abscess drainage. Women in the HIRA-NPS dataset who were given a procedure code of Q2861-Q2863 were counted as a case of acute appendicitis. Pregnant women were identified by one of several antenatal care codes: Z34, supervision of normal pregnancy; Z35, supervision of high-risk pregnancy; Z36, antenatal screening. Pregnant women with acute appendicitis were defined as women who were treated for acute appendicitis within 60 days of receiving antenatal care. Individuals in our study who, according to the Korean Medical Care Act, had either type 1 or type 2 forms of National Health Insurance (similar to receiving Medicaid in the United States) were classified as being in a low socioeconomic state.
The Institutional Review Board of Korea University Guro Hospital approved this study on the 4th Oct 2012 (reference number: KUGH12147). All patients in our dataset have an anonymous ID created by The Korean Health Insurance Review and Assessment Service.
SAS (Enterprise Guide ver.4.3, SAS Institute Inc., Cary, NC, USA) was used for data mining. R ver. 2.12.2 (R Foundation for Statistical Computing, Vienna, Austria) was used for all statistical analyses including a weighted analysis. All statistical tests were two-tailed, and results were considered significant at P < 0.05. Chi-square test for proportions was performed for comparing the prevalence of acute appendicitis. Multivariate logistic regression analysis was used to evaluate the association of our chosen variables (age, pregnancy, and socioeconomic status) with the likelihood of developing acute appendicitis.
RESULTS
The total sample size was 1,116,040 people. Demographics showed Table 1. We identified 15,974 acute appendicitis cases and 160 cases of acute appendicitis in pregnant women during 2009 (Fig. 1). The mean age across the appendicitis sample was 31.8 ± 0.2 years (Table 2). The proportion of women who were pregnant was 3.3%. The prevalence of acute appendicitis among all Koreans was 224 ± 2 per 100,000 persons. The prevalence of acute appendicitis in men was higher than that in women (P < 0.001). In particular, the prevalence of acute appendicitis in pregnant women (96 ± 97 per 100,000 persons) was significantly lower than that in non-pregnant women (206 ± 3 per 100,000 persons) (P < 0.001) (Table 2). Multivariate analysis was performed, adjusting for age, pregnancy, and socioeconomic status. According to the logistic regression models, age and pregnancy were negatively associated with acute appendicitis in women aged 20 to 39 years (age: odds ratio [OR], 0.972; 95% confidence interval [CI], 0.975 to 0.978; pregnancy: OR, 0.376; 95% CI, 0.307 to 0.461; P < 0.001) (Fig. 2). Low socioeconomic status was not significantly associated with acute appendicitis. The peak age group in prevalence of acute appendicitis was early teens. After the early teens, prevalence in both genders declined with increasing age (Fig. 2).
Table 1.
Demograghics
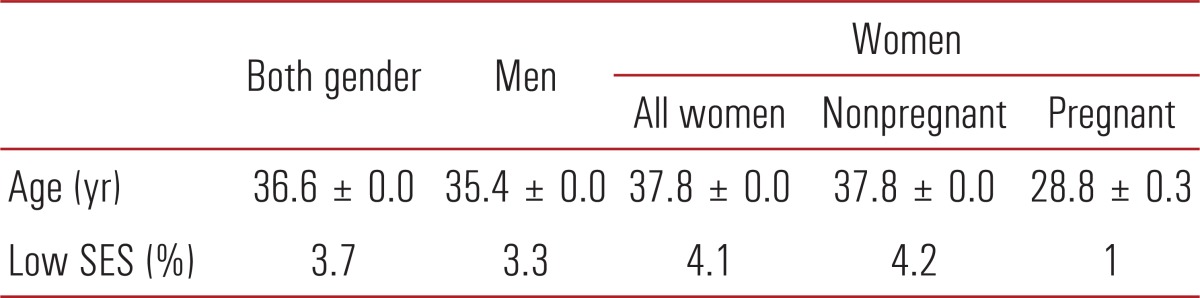
Values are presented as mean ± standard error of the mean.
SES, socioeconomic status.
Fig. 1.
Filtering of data. HIRA, Health Insurance Review and Assessment Service.
Table 2.
Prevalence of acute appendicitis by gender
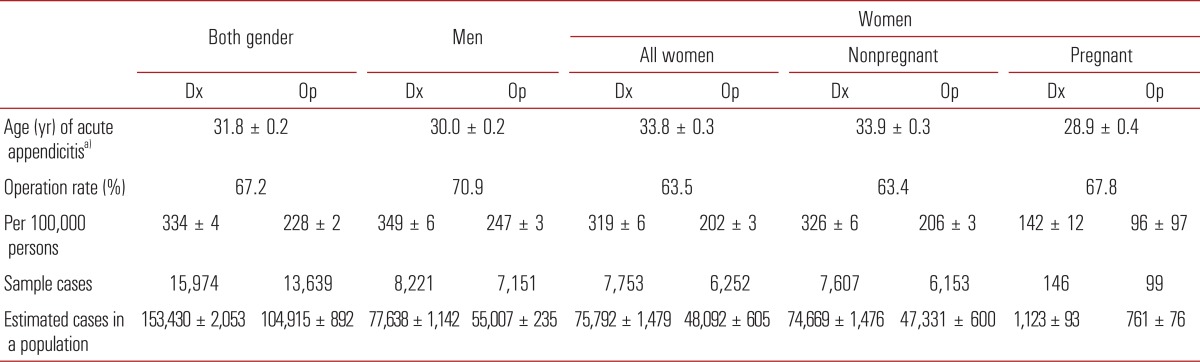
Values are presented as mean ± standard error of the mean.
Dx, diagnosis by diagnosis code; Op, appendectomy by procedure code.
a)Estimated by procedure code.
Fig. 2.
Prevalence rate in acute appendicitis according to 5-year increments.
Simple acute appendicitis was the most common appendicitis diagnosis, based on procedure code. Perforated appendicitis was the next most common diagnosis (Table 3).
Table 3.
Estimated diagnosis cases in a population according to procedure code
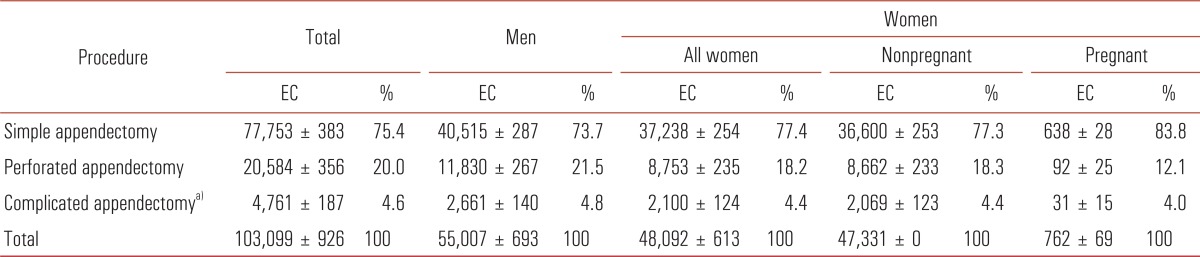
Values are presented as mean ± standard error of the mean.
EC, estimated cases in a population.
a)Removal of appendiceal abscess with periappendiceal abscess drainage.
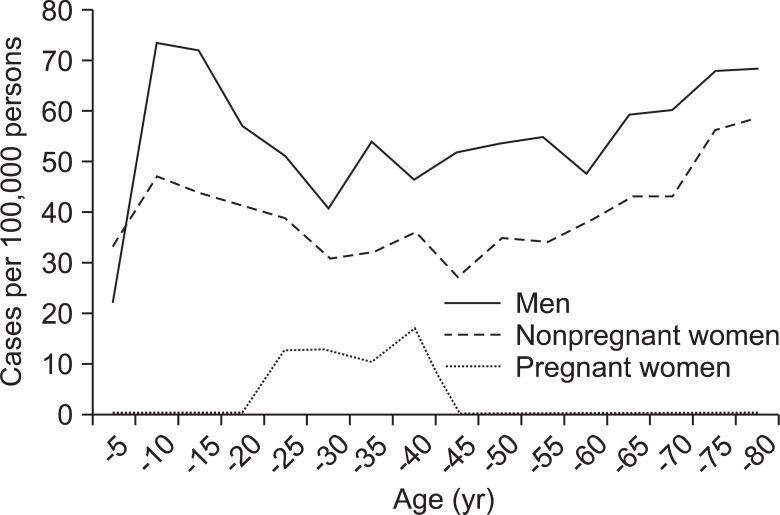
The prevalence of perforated appendicitis peaked among children younger than five years, and the lowest prevalence of perforated appendicitis was among people aged 25 to 29 years (Fig. 3). After the age of 30 years, the prevalence of perforated appendicitis increased with age (P < 0.001), giving the graph of perforated appendicitis prevalence by age a U-shaped distribution (Fig. 4).
Fig. 3.
Prevalence rate in perforated acute appendicitis according to 5-year increments.
Fig. 4.
Proportion of perforated acute appendectomy cases.
DISCUSSION
We found that pregnancy is a protective factor against acute appendicitis. In our study, the prevalence of acute appendicitis in pregnant women was lower than that men or nonpregnant women. Several factors could explain the protective effect of pregnancy against appendicitis. First, T2 helper cells might proliferate during pregnancy [7,8]. Second, circulating estrogen, androgen and progesterone during pregnancy might change T cell response behavior [9]. These immune reaction changes during pregnancy may influence the onset of acute appendicitis [8,10,11]. Our study findings were consistent with those of another study [10]. A particular strength of our study design is that it intuitively shows the relationship between acute appendicitis prevalence among men, nonpregnant women, and pregnant women.
The prevalence of acute appendicitis in South Korea was higher than that found in other countries (110-120/100,000 person-year) [1,12]. This difference could be due to different diagnostic defining criteria (i.e., we used operation code, but other studies defined cases histologically). Even with these different methodologies, the prevalence of acute appendicitis in pregnant women was similar across all studies (range, 66-130/100,000 pregnant women-year) [13-15].
The peak age group in prevalence of acute appendicitis was early teens for both men and women. After the early teens, prevalence in both genders declined with age. Other studies found a comparable prevalence across age groups [1,12-15]. Lymphoid follicular hyperplasia may be the main cause of acute appendicitis in young adults. At around the same age that risk for acute appendicitis decreases, lymphoid follicular hyperplasia begins to decrease [16].
The prevalence of perforated appendicitis by age has a U-shaped pattern; prevalence was highest in children younger than five years and adults older than 60 years. Late presentation and delayed diagnosis may be associated with the high proportion of appendicitis due to perforation among all acute cases in patients younger than five and older 60 years [17,18].
Our study has one main limitation. Diagnosis of acute appendicitis was not confirmed by biopsy. Instead, we estimated the number of cases using a diagnosis code or procedure code. Previous studies have found that confirmed cases by biopsy only account for 64-85% of total actual cases [1,19-21]. Therefore, if this ratio is also true in our study, our study is comparable to other studies, especially regarding prevalence pattern.
In summary, we found that the prevalence of acute appendicitis decreased by increasing age after the early teen years, and that the prevalence of acute appendicitis in pregnant women was lower than those in men and nonpregnant women.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Addiss DG, Shaffer N, Fowler BS, Tauxe RV. The epidemiology of appendicitis and appendectomy in the United States. Am J Epidemiol. 1990;132:910–925. doi: 10.1093/oxfordjournals.aje.a115734. [DOI] [PubMed] [Google Scholar]
- 2.Birnbaum BA, Wilson SR. Appendicitis at the millennium. Radiology. 2000;215:337–348. doi: 10.1148/radiology.215.2.r00ma24337. [DOI] [PubMed] [Google Scholar]
- 3.Nitecki S, Karmeli R, Sarr MG. Appendiceal calculi and fecaliths as indications for appendectomy. Surg Gynecol Obstet. 1990;171:185–188. [PubMed] [Google Scholar]
- 4.Jones BA, Demetriades D, Segal I, Burkitt DP. The prevalence of appendiceal fecaliths in patients with and without appendicitis: a comparative study from Canada and South Africa. Ann Surg. 1985;202:80–82. doi: 10.1097/00000658-198507000-00013. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Pastore PA, Loomis DM, Sauret J. Appendicitis in pregnancy. J Am Board Fam Med. 2006;19:621–626. doi: 10.3122/jabfm.19.6.621. [DOI] [PubMed] [Google Scholar]
- 6.Kim RY. Introduction to HIRA-NPS. Health Insur Rev Assess Serv. 2012;6:37–47. [Google Scholar]
- 7.Keeling SO, Oswald AE. Pregnancy and rheumatic disease: "by the book" or "by the doc". Clin Rheumatol. 2009;28:1–9. doi: 10.1007/s10067-008-1031-9. [DOI] [PubMed] [Google Scholar]
- 8.Wegmann TG, Lin H, Guilbert L, Mosmann TR. Bidirectional cytokine interactions in the maternal-fetal relationship: is successful pregnancy a TH2 phenomenon? Immunol Today. 1993;14:353–356. doi: 10.1016/0167-5699(93)90235-D. [DOI] [PubMed] [Google Scholar]
- 9.Cutolo M, Capellino S, Sulli A, Serioli B, Secchi ME, Villaggio B, et al. Estrogens and autoimmune diseases. Ann N Y Acad Sci. 2006;1089:538–547. doi: 10.1196/annals.1386.043. [DOI] [PubMed] [Google Scholar]
- 10.Andersson RE, Lambe M. Incidence of appendicitis during pregnancy. Int J Epidemiol. 2001;30:1281–1285. doi: 10.1093/ije/30.6.1281. [DOI] [PubMed] [Google Scholar]
- 11.Somerset DA, Zheng Y, Kilby MD, Sansom DM, Drayson MT. Normal human pregnancy is associated with an elevation in the immune suppressive CD25+ CD4+ regulatory T-cell subset. Immunology. 2004;112:38–43. doi: 10.1111/j.1365-2567.2004.01869.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Anderson JE, Bickler SW, Chang DC, Talamini MA. Examining a common disease with unknown etiology: trends in epidemiology and surgical management of appendicitis in California, 1995-2009. World J Surg. 2012;36:2787–2794. doi: 10.1007/s00268-012-1749-z. [DOI] [PubMed] [Google Scholar]
- 13.Buckius MT, McGrath B, Monk J, Grim R, Bell T, Ahuja V. Changing epidemiology of acute appendicitis in the United States: study period 1993-2008. J Surg Res. 2012;175:185–190. doi: 10.1016/j.jss.2011.07.017. [DOI] [PubMed] [Google Scholar]
- 14.Ohmann C, Franke C, Kraemer M, Yang Q. Status report on epidemiology of acute appendicitis. Chirurg. 2002;73:769–776. doi: 10.1007/s00104-002-0512-7. [DOI] [PubMed] [Google Scholar]
- 15.Primatesta P, Goldacre MJ. Appendicectomy for acute appendicitis and for other conditions: an epidemiological study. Int J Epidemiol. 1994;23:155–160. doi: 10.1093/ije/23.1.155. [DOI] [PubMed] [Google Scholar]
- 16.Petro M, Minocha A. Asymptomatic early acute appendicitis initiated and diagnosed during colonoscopy: a case report. World J Gastroenterol. 2005;11:5398–5400. doi: 10.3748/wjg.v11.i34.5398. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Lunca S, Bouras G, Romedea NS. Acute appendicitis in the elderly patient: diagnostic problems, prognostic factors and outcomes. Rom J Gastroenterol. 2004;13:299–303. [PubMed] [Google Scholar]
- 18.Rothrock SG, Skeoch G, Rush JJ, Johnson NE. Clinical features of misdiagnosed appendicitis in children. Ann Emerg Med. 1991;20:45–50. doi: 10.1016/s0196-0644(05)81117-5. [DOI] [PubMed] [Google Scholar]
- 19.Andersen B, Nielsen TF. Appendicitis in pregnancy: diagnosis, management and complications. Acta Obstet Gynecol Scand. 1999;78:758–762. [PubMed] [Google Scholar]
- 20.Mazze RI, Kallen B. Appendectomy during pregnancy: a Swedish registry study of 778 cases. Obstet Gynecol. 1991;77:835–840. [PubMed] [Google Scholar]
- 21.Mourad J, Elliott JP, Erickson L, Lisboa L. Appendicitis in pregnancy: new information that contradicts long-held clinical beliefs. Am J Obstet Gynecol. 2000;182:1027–1029. doi: 10.1067/mob.2000.105396. [DOI] [PubMed] [Google Scholar]