Abstract
Due to the current economic environment, many local and state health departments are faced with budget reductions. Health department administrators and public health laboratory (PHL) directors need to assess strategies to ensure that their PHLs can provide the same level of service with decreased funds. Exploratory case studies of interorganizational partnerships among local PHLs in California were conducted to determine the impact on local PHL testing services and capacity. Our findings suggest that interorganizational forms of cooperation among local PHLs can help bolster laboratory capacity by capturing economies of scale, leveraging scarce resources, and ensuring access to affordable, timely, and quality laboratory testing services. Interorganizational partnerships will help local and state public health departments continue to maintain a strong and robust laboratory system that supports their role in communicable disease surveillance.
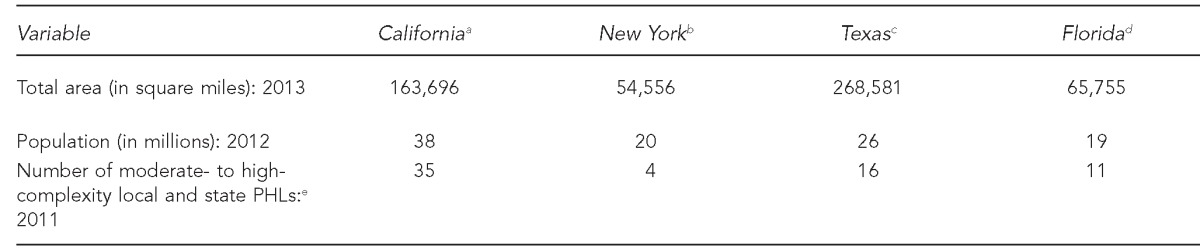
California has a decentralized public health laboratory (PHL) system consisting of one state PHL and multiple local PHLs (LPHLs) serving 61 health jurisdictions. The establishment of LPHLs began in the early 1950s. By the 1970s, 39 LPHLs were established across California. Four laboratories have since shut down in Mendocino, Napa, Yolo, and Marin counties. The Napa, Yolo, and Marin county PHLs consolidated with the Solano County PHL in 1999, 2011, and 2013, respectively. The Mendocino County health department is contracting for laboratory services with the Sonoma County PHL. As of July 2013, there were 35 LPHLs in operation in California. The cost of establishing and maintaining a PHL is borne by the city or county. Thus, the LPHLs operate fairly independently from each other and the state PHL. Table 1 provides a comparison of the number of PHLs in California with states that have a comparable population or land mass.1–5
Table 1.
Comparison of land mass, population, and number of moderate- to high-complexity PHLs within the PHL systems in California, New York, Texas, and Florida: 2012–2013a
aCensus Bureau (US). State and county quickfacts: California, 2012 [cited 2012 Jul 15]. Available from: URL: http://quickfacts.census.gov/qfd/states/06000.html
bCensus Bureau (US). State and county quickfacts: Florida, 2012 [cited 2012 Jul 15]. Available from: URL: http://quickfacts.census.gov/qfd/states/12000.html
cCensus Bureau (US). State and county quickfacts: New York, 2012 [cited 2012 Jul 15]. Available from: URL: http://quickfacts.census.gov/qfd/states/36000.html
dCensus Bureau (US). State and county quickfacts: Texas, 2012 [cited 2012 Jul 15]. Available from: URL: http://quickfacts.census.gov/qfd/states/48000.html
eHsieh K. California's public health laboratories: inter-organizational cooperation models to bolster laboratory capacity. 2011 [cited 2012 Jul 15]. Available from: URL: http://digitalassets.lib.berkeley.edu/etd/ucb/text/Hsieh_berkeley_0028E_11865.pdf
PHL = public health laboratory
Multiple economic and regulatory constraints are impacting the sustainability of LPHLs and the state PHL in California and across the nation. Increased commercial laboratory competition in past years has reduced the volume of tests being sent to PHLs.6 Prior to and during the 2008 economic recession, budgetary pressures decreased funding allocations for health departments and, ultimately, the laboratories.7,8 In addition to economic pressures, regulatory pressures have impacted the sustainability of PHLs. The PHL director (PHLD) workforce has been affected since the introduction of the federal Clinical Laboratory Improvement Amendments in 1988. These federal amendments mandate that PHLDs have a doctoral degree and a board certification to supervise an accredited moderate- to high-complexity PHL.9 In California, a qualified PHLD must meet federal and state requirements. The California requirements include obtaining a post-baccalaureate-level public health microbiologist certification and four years of training in a PHL. A limited number of qualified applicants are able to meet both federal and state requirements. As the current PHLDs retire, there is an anticipated shortage of individuals to fill the pipeline.5 The compounding nature of the workforce shortage and economic environment is affecting the sustainability of PHLs across California.
The California PHL system has been in place for more than 100 years and has been successful in averting public health threats (e.g., the plague, smallpox, 2009 H1N1 pandemic, and, in recent years, Hantavirus and pertussis outbreaks). However, economic pressures are forcing local and state health administrators to assess their laboratory needs. If health department administrators are considering closing a PHL or eliminating and/or outsourcing testing services as a means of cost savings, strategies to ensure seamless provision of quality laboratory testing services are needed. We explored interorganizational partnerships (i.e., a strategic alliance, or formal arrangement, between two or more organizations for the purpose of ongoing cooperation and mutual risk/gain sharing through a long- or short-term contract) as a means of bolstering laboratory capacity and maintaining a robust PHL network in California.10,11
METHODS
We conducted exploratory case studies to highlight different forms of strategic cooperation/partnerships implemented among LPHLs in California to cope with budgetary and regulatory constraints. Factors deemed significant by PHLDs and health administrators for maintaining long-term partnerships are documented across each case study to elucidate criteria necessary for successful interorganizational relationships. As described by Stake and Yin, it is important to understand how different cases perform in different environments; therefore, the evidence from multiple case studies may be more convincing than from a single case study.12,13
We conducted seven in-depth interviews for two case studies. Interviews were conducted either in person or by phone. The interviewees were limited to individuals with specific knowledge of the partnership between laboratories. Information gathered from interviews was written up descriptively. Case studies of the consolidation of the Napa County and Solano County laboratories and the contractual agreement between Sonoma County and Mendocino County are described in the next section.
OUTCOMES
Case one: Napa County and Solano County PHL consolidation
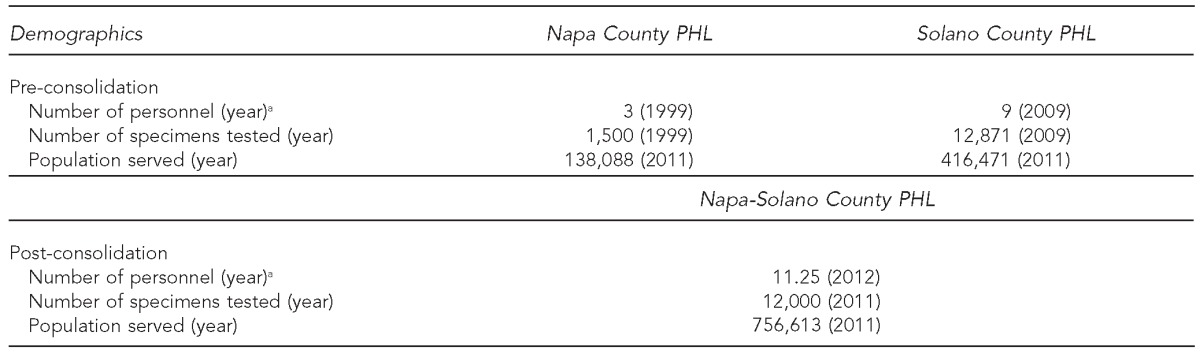
In 1997, the Health and Human Services Agency in Napa County received funding from the county to update its campus. The PHL was located in a trailer and was invited to participate in the campus update. However, after reviewing the cost of building a new laboratory facility and maintaining a PHL, the administration realized that it could not afford to undertake this endeavor. The Napa County health department administrators and PHLD decided to explore the option of consolidating with another PHL to continue provision of laboratory services. The Solano County health department administrators were advocating for obtaining economies of scale with public health programs. Napa and Solano counties were facing major budget deficits and problems with hiring laboratory personnel and decided to engage in a strategic alliance by consolidating their PHLs as a cost-saving measure. Table 2 includes the county demographics and PHL profile of Napa and Solano counties pre- and post-consolidation.
Table 2.
Number of personnel, specimens, and population served by the Napa County and Solano County, California, public health laboratories pre- and post-consolidation
aPersonnel includes technical and clerical categories denoted in full-time equivalents.
PHL = public health laboratory
Initiation of PHL consolidation.
The Napa County health department administrators and PHLD agreed upon two criteria to assess a partnering laboratory: (1) compatibility of testing capabilities and (2) distance of specimen transport. Bids were sent to the neighboring counties of Sonoma, Contra Costa, and Solano. Solano County PHL was chosen as the partnering laboratory due to compatibility of testing capabilities and distance (about 20 miles). In addition, the following two factors were critical in the decision-making process:
Prior working relationship. The Solano County PHL acted as a backup laboratory when Napa County needed assistance with testing. The laboratory personnel at the Solano County PHL were familiar with the procedures and protocols for handling specimens from Napa County. This knowledge streamlined the transition process during the initial phases of the merger.
Use of Napa County personnel at the joint laboratory. The Solano County health department was willing to create an assistant -laboratory -director position in the joint Napa-Solano County PHL for the Napa County PHLD. This staffing solidified and strengthened the partnership as the laboratory directors adjusted to managing a joint PHL.
In 1999, a joint powers agreement (JPA) was created and approved by both the Napa County and Solano County health department administrators and boards of supervisors. A JPA is a contract between a city, a county, and/or a special district in which the city or county agrees to perform services, cooperate with, or lend its powers to the other city, county, or special district.11 The JPA allows a single laboratory to serve multiple adjacent counties and leverage scarce resources to create economies of scale for specimen testing, proficiency testing, supplies, and reducing personnel needs. This agreement resulted in the closure of the Napa County PHL and creation of the joint Napa-Solano County PHL. The employees are hired and paid by Solano County, but Napa County provides financial support to maintain the PHL and continued provision of laboratory services for Napa County. Health department administrators from both counties have deemed this venture successful, as evidenced by the renewal of the JPA in 2005, 2008, and 2010.
Areas of success.
The joint laboratory established a courier service to pick up specimens in Napa County to ensure that samples are transported in a timely manner. If specimens had to be packaged and shipped to a new facility, there would likely be delays in shipment or mishandling of samples. By engaging in a consolidation effort, Napa County is able to offer a broader testing menu to its clients and a faster turnaround time for reporting results. For example, human immunodeficiency virus testing was conducted once a week at the Napa County PHL due to low specimen volume. At the Solano County PHL, the same test is conducted several times a week. Health department administrators from both Napa and Solano Counties are equally invested and responsible for the PHL and work collaboratively to ensure that the needs of both their health departments are met. In addition to enhanced testing services, cost savings have been achieved. Napa County reduced its annual fiscal expenditures by sharing a laboratory facility, and Solano County benefited from increased funding support.
According to health department administrators and the PHLD, an area of implementation that is integral for the success of this partnership is the use of a JPA rather than a contract or memorandum of understanding (MOU). The benefits of the JPA include:
Joint name for the laboratory. The JPA allows the use of a joint name for the laboratory—something that cannot be granted under a contract or an MOU.
Access to government funding. The JPA allows government funding designated for the Napa County PHL to be accessible to the joint PHL. If the agreement was contractual, Solano County would not have access to funding designated for Napa County.
Equal footing and responsibility for the PHL. The counties jointly operate the laboratory, and both counties' health officers function in an advisory capacity for decisions relating to the laboratory. This equality provides assurance to the Napa County health department that the Solano County health department cannot make changes to the PHL without its involvement.
Points of improvement.
This partnership has many successful components; however, one improvement to the agreement has been suggested—allowing greater flexibility with funding. With the renewal of the 2010 JPA, health administrators from both counties have agreed to detach funding to a specific position and allow the use of funds for any laboratory-associated needs. In addition, a new provision to the JPA was added to link Napa County's financial contribution to the consumer price index to reflect inflation. Prior to the 2010 agreement, Solano County did not request an increase in financial support from the Napa County health department even though operating costs have gone up considerably over the years. By leveraging partnerships, both Napa and Solano counties are able to obtain economies of scale for the provision of laboratory services.
The consolidation of these two PHLs has been very successful. As one Napa County health officer put it: “The whole process really worked because of the people involved. Everyone had the same goal in mind, which was to strengthen the laboratory services in both counties and become more efficient and cost-effective, and that was accomplished and is still being accomplished with this agreement.”
Case two: contractual agreement for laboratory services in Mendocino County
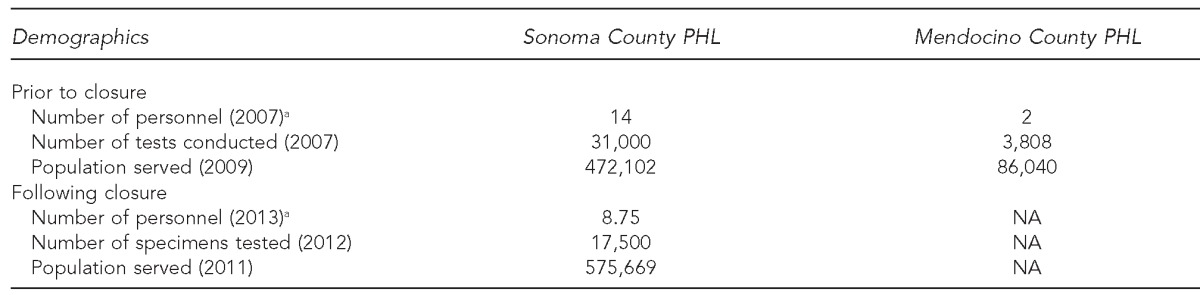
The Mendocino County health administration was unable to recruit a qualified candidate for its PHLD position when its director retired. An alternative solution was to contract for the services of a PHLD to meet federal regulations for operation. An agreement was established with a neighboring health department's PHLD to manage the PHL. The PHLD agreed to visit the Mendocino County PHL once a month and provide supervision through telecommunication. Table 3 summarizes the county demographics and PHL profiles pre- and post-closure of the Mendocino County PHL.
Table 3.
Number of personnel, specimens tested, and population served at the Sonoma and Mendocino County PHLs pre- and post-closure of the Mendocino County PHL: California, 2007–2011
aPersonnel includes technical and clerical categories denoted in full-time equivalents.
PHL = public health laboratory
NA = not applicable
During this period, the Mendocino County PHL was supported by a laboratory manager and two public health microbiologists (PHMs). During the first year, one PHM retired, leaving one microbiologist and the laboratory manager to handle the workload for the laboratory. When the laboratory manager retired and the health department could not successfully recruit a qualified applicant, sustaining the PHL became problematic. Under federal and state requirements, PHLs may employ a part-time PHLD if there is a full-time supervising PHM working in the laboratory. After having difficulty recruiting for both the PHLD and supervising PHM positions, the Mendocino County health officer decided that the $250,000 needed to maintain the PHL should be directed to other programs. In 2009, Mendocino County health department administrators and boards of supervisors decided to close the PHL and outsource laboratory testing. Laboratory samples were sent to clinical laboratories in hospitals around Mendocino County, and specimens of public health concern (e.g., rabies and Mycobacterium tuberculosis) were sent to the Sonoma County PHL, which was located approximately 63 miles away. A fee-for-service contractual agreement was established.
Points of improvement.
A fee-for-service contract does not foster the same level of mutual reliance and commitment for the PHL that a JPA requires. According to Sonoma County laboratory personnel, the fee-for service arrangement does not contribute to the overhead cost of supporting a PHL or the costs of maintaining a federally qualified PHLD. In spring 2010, a different contractual model was proposed by the Sonoma County PHLD and health department administrators. The revised contract establishes a partnership similar to the JPA that requires the Mendocino County health department to increase its share of financial support for the laboratory. Monetary support will be scaled up during a three-year period. The Mendocino County health department will cover one-third of the cost in the first year, two-thirds of the cost in the second year, and the full cost in the third year. This support plan allows the Mendocino County health department to increase its budget for laboratory services during a three-year cycle. This contract was established in the 2011–2012 fiscal year. Both health department administrators agreed that there are minimal governance issues and decided to continue with a contractual agreement rather than use a more formalized JPA. After three years, both counties will reevaluate the contract and adjust to future needs.
LESSONS LEARNED
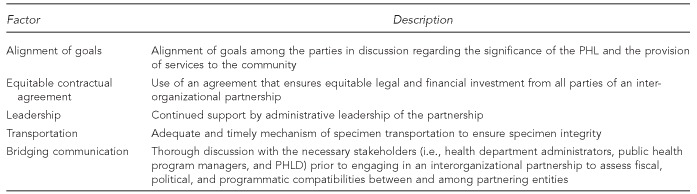
Due to the decentralized manner in which LPHLs in California function, a one-size-fits-all model will not work due to political, legal, financial, and structural differences among health departments. In the case of the Napa-Solano County PHL consolidation, a JPA was selected to allow for equal governance of the joint laboratory. The Mendocino County and Sonoma County health department administrators decided to use a contract rather than a JPA due to minimal governance issues. Health department administrators and the PHLD must work together and analyze factors that are important and pertinent to their specific needs and circumstances. In addition, the alignment of goals, open communication, and continued support of leaders is imperative to ensure a successful long-term relationship, as exemplified in the consolidation of the Napa County and Solano County PHLs. A -summary of the factors discussed in the case studies that are integral in a successful long-term partnership is shown in the Figure.
Figure.
Summary of factors that are integral for a successful PHL partnership
PHL = public health laboratory
PHLD = public health laboratory director
The LPHL system in California is the largest network of LPHLs in the U.S., with 35 LPHLs serving 61 health jurisdictions. Multiple factors are impacting LPHLs today, including shifts in federal regulations, competition from clinical and commercial laboratories, and local and national economic pressures. To cope with resource limitations, health department administrators and PHLDs may be forced to assess different strategies to address these constraints. Provision of public health services (e.g., PHLs) may benefit from assessing the feasibility of engaging in interorganizational forms of cooperation.
CONCLUSIONS
The economic climate locally and nationally has had a detrimental impact on the public health system during the past several years. Laboratories in California and across the nation have had to downsize their staff, outsource and/or eliminate services, and close laboratories to cope with economic and regulatory pressures.14 As economic conditions continue to worsen, health department administrators need to assess different options to maximize the use of resources for public health services such as PHLs. One option to improve efficiency and maintain access to quality PHL testing and services is engagement in partnerships to leverage resources and obtain economies of scale. By partnering with other laboratories, costs are shared, and expertise and testing services are expanded. This partnership can ensure that a robust PHL network continues to support public health efforts to detect, identify, and monitor emerging and reemerging public health threats and emergencies.15
Footnotes
This article was made possible by contributions from state, local, and city health department administrators and public health laboratory directors. Sincerest gratitude is extended to those individuals who took the time to share their experiences regarding interorganizational partnerships from among their public health laboratories.
REFERENCES
- 1.Census Bureau (US) State and county quickfacts: California, 2012. [cited 2012 Jul 15]. Available from: URL: http://quickfacts.census.gov/qfd/states/06000.html.
- 2.Census Bureau (US) State and county quickfacts: Florida, 2012. [cited 2012 Jul 15]. Available from: URL: http://quickfacts.census.gov/qfd/states/12000.html.
- 3.Census Bureau (US) State and county quickfacts: New York, 2012. [cited 2012 Jul 15]. Available from: URL: http://quickfacts.census.gov/qfd/states/36000.html.
- 4.Census Bureau (US) State and county quickfacts: Texas, 2012. [cited 2012 Jul 15]. Available from: URL: http://quickfacts.census.gov/qfd/states/48000.html.
- 5.Hsieh K. California's public health laboratories: inter-organizational cooperation models to bolster laboratory capacity. 2011. [cited 2012 Jul 15]. Available from: URL: http://digitalassets.lib.berkeley.edu/etd/ucb/text/Hsieh_berkeley_0028E_11865.pdf.
- 6.Ahn R, Gaylin DS, Keiller A, Mendelson DN, Moiduddin A, Rubin RJ. Public health laboratories and health system change. Rockville (MD): Department of Health and Human Services (US); 1997. [cited 2009 Jul 15]. Also available from: URL: http://aspe.hhs.gov/health/Reports/phlabs/front.htm. [Google Scholar]
- 7.Hill EG. Overview of the governor's budget. Sacramento (CA): Legislative Analyst's Office; 2003. [cited 2011 Jan 19]. Also available from: URL: http://www.lao.ca.gov/2003/budget_overview/03-04_budget_overview.pdf. [Google Scholar]
- 8.Soman LA. California's state budget for fiscal year 2010–2011: another long budget year. Los Angeles: UCLA Center for Healthier Children, Families and Communities; 2010. [cited 2013 Mar 31]. Also available from: URL: http://www.uscucedd.org/downloads/products_publications/professional_publications/periodicals/cacshcnews/CAState_Budget_Report072310.pdf. [Google Scholar]
- 9.Centers for Disease Control and Prevention (US) Subpart M: personnel for non-waived testing. [cited 2012 Jul 15]. Available from: URL: http://wwwn.cdc.gov/clia/regs/subpart_m.aspx#493.1405.
- 10.Child J, Faulkner D. Strategies of co-operation: managing alliances, networks, and joint ventures. New York: Oxford University Press; 1998. [Google Scholar]
- 11.Gulati R. Does familiarity breed trust? The implications of repeated ties for contractual choice in alliances. Acad Manag J. 1995;38:85–112. [Google Scholar]
- 12.Stake RE. Multiple case study analysis. New York: The Guilford Press; 2005. [Google Scholar]
- 13.Yin RK. Case study research: design and methods. 4th ed. Thousand Oaks (CA): Sage Publications, Inc.; 2009. [Google Scholar]
- 14.Centers for Disease Control and Prevention (US) and Association of Public Health Laboratories. A practical guide to assessing and planning implementation of public health laboratory service changes. 2012. [cited 2013 Mar 31]. Available from: URL: http://stacks.cdc.gov/view/cdc/11883.
- 15.Institute of Medicine. The future of the public's health in the 21st century. Washington: National Academies Press; 2002. [PubMed] [Google Scholar]


