Abstract
Aspergillosis in the central nervous system (CNS) is a very rare disease in immune-competent patients. There was a case of a healthy man without a history of immune-compromised disease who had invasive aspergillosis with unusual radiologic findings. A 48-year-old healthy man with diabetes mellitus, presented with complaints of blurred vision that persisted for one month. Brain magnetic resonance imaging (MRI) showed multiple nodular enhancing lesions on the right cerebral hemisphere. The diffusion image appeared in a high-signal intensity in these areas. Cerebrospinal fluid examination did not show any infection signs. An open biopsy was done and intraoperative findings showed grayish inflammatory and necrotic tissue without a definitive mass lesion. The pathologic result was a brain abscess caused by fungal infection, morphologically aspergillus. Antifungal agents (Amphotericin B, Ambisome and Voriconazole) were used for treatment for 3 months. The visual symptoms improved. There was no recurrence or abscess pocket, but the remaining focal enhanced lesions were visible in the right temporal and occipital area at a one year follow-up MRI. This immune-competent patient showed multiple enhancing CNS aspergillosis in the cerebral hemisphere, which had a good outcome with antifungal agents.
Keywords: Aspergillosis, Cerebral, Enhancement, Immune-competent, Multiple
INTRODUCTION
Aspergillosis of the central nervous system (CNS) is a very rare disease in immune-competent patients11). Aspergillosis of the CNS could cause an altered mental status, seizures, and focal neurologic symptoms7,23). It can present as aseptic meningitis, solitary or multiple CNS abscess and cerebral infarction1,5,6). The main route of infection is the inhalation of spores into the lungs which is the primary site of infection leading to the hematogenous spread to other organs6,22). The mortality rate of this infection is very high, and early diagnosis and rapid treatment are crucial25,26).
We report the case of a healthy man without a history of immune-compromised disease who presented with multiple nodular enhancing aspergillosis in the right cerebral hemisphere and had the good clinical outcome after adequate conservative treatment after biopsy.
CASE REPORT
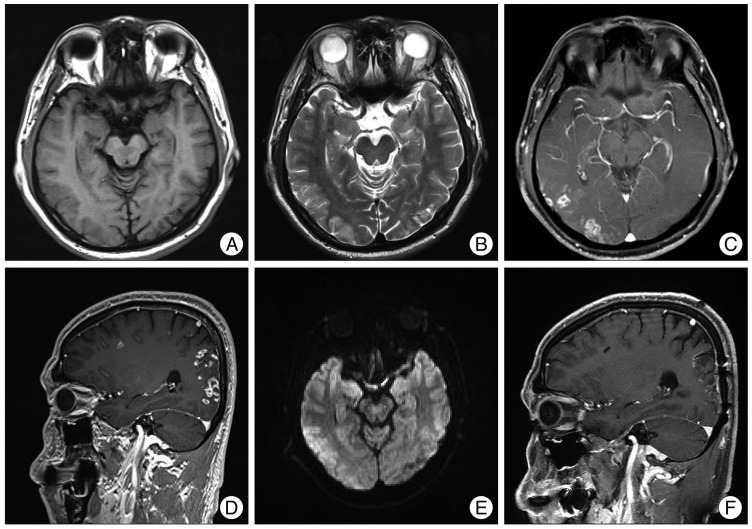
A 48-year-old man with diabetes mellitus, presented to the department of ophthalmology with the complaints of blurred vision that persisted for one month. There was defected visual accuracy in the left eye about 18 years ago. In ophthalmologic examination, there was no new lesion in the both eyes. The laboratory examinations were within normal range. The random blood glucose was 164 mmol/L and the glycosylated hemoglobin was 8.1%. Upon further evaluation, magnetic resonance imaging (MRI) of the brain showed a low-signal intensity on T1-wighted images and a high-signal intensity on T2-weighed images (Fig. 1A, B). After gadolinium enhancement, multiple nodular enhancing lesions with or without a focal necrotic area were shown in the right frontotemporoparietal cortex and white matter (Fig. 1C, D). The diffusion image appeared with high-signal intensity in these areas (Fig. 1E). The magnetic resonance spectroscopy obtained from the right occipital region showed elevated lactate/lipid peaks, with mild decreased N-acetylaspartate and no elevation of choline, which suggested necrotic conditions. The lumbar-puncture examination cerebrospinal fluid did not show any infection signs. The body fluid parasite and anti-human immunodeficiency virus levels in the cerebrospinal fluid were negative.
Fig. 1.
Radiologic findings. A and B : In brain MRI, there are low-signal intensity on T1-wighted axial images and high-signal intensities in the T2-weighed axial image on right occipital cortex. C and D : Multiple enhancing nodules with necrotic change are shown in right frontotemporoparietal cortex and white matter. E : In diffusion MRI, the high-signal intensity lesions are shown in right frontotemporoparietal cortex and white matter. F : The recurrence does not appear in the right temporal and occipital area with remaining focal enhanced lesions.
An occipital craniotomy and biopsy was performed using the guidance of neuronavigation. In the operative field, there was a reddish color change of the cortex and the thickened arachnoid membrane had a yellowish color change (Fig. 2A). There was no definitive mass lesion. By using grasping forcep, the biopsy was done in the yellowish white matter. The biopsy showed many inflammatory cells containing some hyphae with the positive periodic acid-shiff stain (Fig. 2B). The pathology result showed a brain abscess caused by fungal infection that had the morphologically of aspergillus. Amphotericin B (50 mg/day) therapy was immediately started after the biopsy confirmation, but there were swelling, and skin eruptions at injection site, and fever. On the 3rd day of treatment, the antifungal agent was changed to ambisome (3 mg/kg/day). After 6 days, the serum creatinine level became elevated to 1.9 mg/dL and the antifungal agent was changed with voriconazole (400 mg/day). Voriconazole therapy was maintained for 3 months. The subjective visual symptom improved. There was no recurrence noted at the one year follow up MRI, but the remaining focal enhanced lesions were visible in the right temporal and occipital area (Fig. 1F).
Fig. 2.
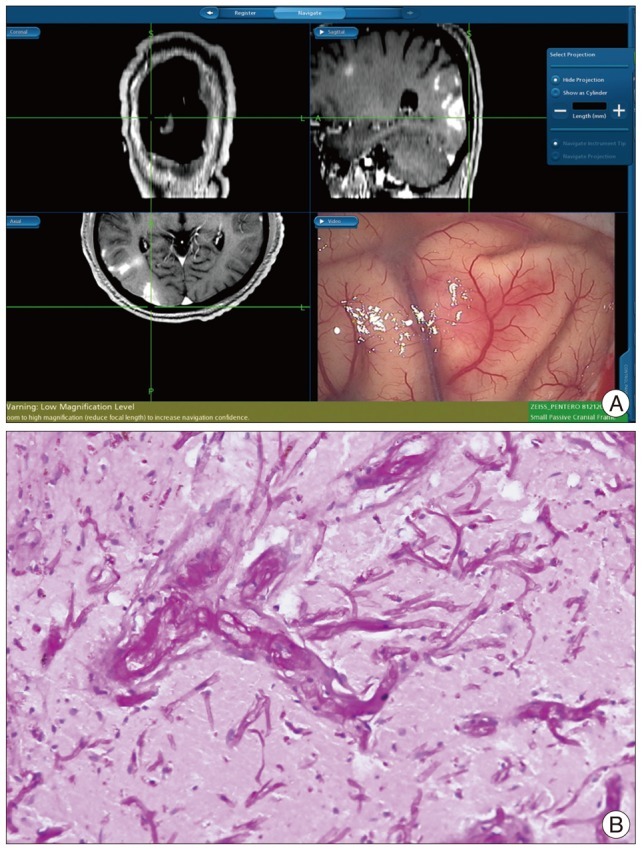
Operative and pathologic findings. A : There was no definitive mass lesion, but reddish tissues of the cortex and the thickened yellowish arachnoid membrane are shown. B : In the biopsy, there are shown the hyphaes with the positive periodic acid-shiff staining (original magnification ×200).
DISCUSSION
Central nervous system aspergillosis is a rare disease in immuno-competent patients but there is a poor prognosis and a very high mortality (88-99%)7,16,22). The stress of surgery may be a risk factor for fungal infection15,16). Broad-spectrum antibiotics over a 3 month period could be a predisposing factor for CNS aspergillosis4,18). The abuse of antibiotics may be a predisposing factor for CNS aspergillosis. This patient did not have any immuno-compromized disease other than those linked with diabetes mellitus.
Systemic aspergillus can be a risk factor of CNS aspergillosis22). Aspergillus invasion of the CNS usually occurs by the hematogenous spread from primary sources (such as the lungs or gastrointestinal tract)6,22). This case did not show the systemic aspergillosis. Because of its ability to digest elastin in the vessel walls, the fungus makes a highly virulent and angioinvasive organism6,22). Hyphal elements may also grow through the vessel wall, compromising the structural integrity of the vessel wall and constructing aneurysms6,7,10,16,22), so larger arteries could be ruptured and lead to hemorrhage. In addition, hyphal elements may occlude the lumen of the vessels completely, leading to ischemic stroke. Aspergillosis tends to occlude perforating arteries, so ischemic lesions may appear in sites that are rarely affected by other infectious organisms, such as the basal nuclei, thalami, corpus callosum, and brainstem1,3,28).
Neuroimaging is useful in the diagnosis of CNS aspergillosis. In a brain computed tomography, the lesions have low attenuation and may be accompanied by hemorrhagic change6,16,22). This case showed a low dense lesion without hemorrhage. Aspergillus abscesses generally appear as hypointense on non-enhanced T1-weighted MR images, but in some cases, high signal intensity lesions may be seen. The shortened T1 relaxation times may be related with the presence of iron, manganese, or methemoglobin in aspergillosis abscesses. In addition to abscess formation, CNS aspergillosis can rarely associated with mycotic aneurysm1,8). Hemorrhagic lesions occur in 25% of cases1,28). Dependent on the level of the inflammatory reaction, enhancement appears with variable features, with the stage of the infection and the immunity of the patient1,6). On T2-weighted MR images, the lesions of low signal intensity at the periphery correspond to hemorrhage and can be seen on gradient-echo T2-weighted images1,27). Zinreich et al.30) demonstrated that the areas of low signal intensity on T2-weighted images were traced to the presence of iron, manganese, and magnesium in the fungal structures. Aspergillus abscesses have a dense population of hyphal elements peripherally, with a relative small lesions of fungal elements centrally, a feature that contributes to the distinct peripheral low signal intensity on T2-weighted images1,5). On diffusion-weighted images, most CNS fungal abscesses appear in high signal intensity central areas, caused by the restricted diffusion of water in the presence of coagulative necrosis and polymorphonuclear cells, and the rim of the abscess may appear hypointense, caused by hemorrhagic or iron products1,20,24). The ring enhancement lesions, especially in patients without known immunodeficiencies, can be solitary or multiple lesions21,26,28). The ependymal and leptomeningeal enhancements are rare lesions, but dural enhancement may be visible6,16,22). In immune-compromised patients, multiple ring enhancing lesions should distinguish lymphoma, metastatic disease, and multiple abscesses20,23).
In this case, the MRI showed low-signal intensity on T1-wighted images and high-signal intensity on T2-weighed images with multiple nodular enhancing lesions in the right cerebral cortex and white matter. Also there was diffuse diffusion restriction in these areas. It was difficult to get the provisional diagnosis of fungal infection because the patient was immuno-competent with multiple enhancing lesions.
The definitive diagnosis is made with special staining and histopathological tests19). Hyphae with 45 degrees branches is a typical and specific finding for aspergillosis11,14). As a routine procedure, a surgical biopsy may help for the early diagnosis and subsequently early intervention4,13). In unusual neuro-imaging appearances, even in patients that are immune-competent, treatment and evaluation about the fungal infection should be started as soon as possible with the hope for a better outcome. A search for the evidence of coexisting pulmonary or sinus infections should occur when evaluating this disease1,23).
In CNS aspergillosis, a main cause of poor prognosis is the delay in diagnosis and the low penetration of antifungal agents into the CNS25,26). The standard treatments of aspergillosis are the intravenous injection of amphotericin B or flucytocine and the oral medication of itraconazole17). Recently, a voriconazole is recommended for CNS aspergillus infection. But, this agent is expensive, so the actual medication is restricted. Even with high dose antifungal agents, the fatality rates range from 28% and 86%. The other fungal agents are, posakonasole and caspofungin. Amphotericin-B is a very useful antifungal agent, but has adverse effects (renal and hepatic toxicity, anemia, fever and electrolyte abnormalities), therefore therapeutic use is limited2,11). A study by Herbrecht et al.9) compared voriconazole and amphotericin B in invasive aspergillus, and the success rate of treatment was high for voriconazole. In invasive aspergillus, many reports accepted that the efficacy and survival rate is higher with voriconazole than amphotericin B9,11). A total or subtotal resection may be effective in a focal CNS aspergillosis lesion and one study showed that mortality can be reduced from 64% to 39%4,29). Treatment of an antifungal agent alone has revealed a mortality of >90% in most series4,12). However, this case showed a good prognosis. This patient had been treated for 3 months and showed a complete radiologic response.
CONCLUSION
This immune-competent patient showed the multiple enhancing CNS aspergillosis on the cerebral hemisphere, which showed a good outcome with antifungal agents. Although there was no history of immunodeficiency, early diagnosis and treatments are necessary a good outcome for the patient.
References
- 1.Almutairi BM, Nguyen TB, Jansen GH, Asseri AH. Invasive aspergillosis of the brain : radiologic-pathologic correlation. Radiographics. 2009;29:375–379. doi: 10.1148/rg.292075143. [DOI] [PubMed] [Google Scholar]
- 2.Alobid I, Bernal M, Calvo C, Vilaseca I, Berenguer J, Alos L. Treatment of rhinocerebral mucormycosis by combination of endoscopic sinus debridement and amphotericin B. Am J Rhinol. 2001;15:327–331. [PubMed] [Google Scholar]
- 3.Ashdown BC, Tien RD, Felsberg GJ. Aspergillosis of the brain and paranasal sinuses in immunocompromised patients : CT and MR imaging findings. AJR Am J Roentgenol. 1994;162:155–159. doi: 10.2214/ajr.162.1.8273655. [DOI] [PubMed] [Google Scholar]
- 4.Chen S, Pu JL, Yu J, Zhang JM. Multiple Aspergillus cerebellar abscesses in a middle-aged female : case report and literature review. Int J Med Sci. 2011;8:635–639. doi: 10.7150/ijms.8.635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Cox J, Murtagh FR, Wilfong A, Brenner J. Cerebral aspergillosis : MR imaging and histopathologic correlation. AJNR Am J Neuroradiol. 1992;13:1489–1492. [PMC free article] [PubMed] [Google Scholar]
- 6.DeLone DR, Goldstein RA, Petermann G, Salamat MS, Miles JM, Knechtle SJ, et al. Disseminated aspergillosis involving the brain : distribution and imaging characteristics. AJNR Am J Neuroradiol. 1999;20:1597–1604. [PMC free article] [PubMed] [Google Scholar]
- 7.Denning DW. Invasive aspergillosis. Clin Infect Dis. 1998;26:781–803. doi: 10.1086/513943. quiz 804-805. [DOI] [PubMed] [Google Scholar]
- 8.Harris DE, Enterline DS. Neuroimaging of AIDS. I. Fungal infections of the central nervous system. Neuroimaging Clin N Am. 1997;7:187–198. [PubMed] [Google Scholar]
- 9.Herbrecht R, Denning DW, Patterson TF, Bennett JE, Greene RE, Oestmann JW, et al. Voriconazole versus amphotericin B for primary therapy of invasive aspergillosis. N Engl J Med. 2002;347:408–415. doi: 10.1056/NEJMoa020191. [DOI] [PubMed] [Google Scholar]
- 10.Klein HJ, Richter HP, Schachenmayr W. Intracerebral aspergillus abscess : case report. Neurosurgery. 1983;13:306–309. doi: 10.1227/00006123-198309000-00016. [DOI] [PubMed] [Google Scholar]
- 11.Köse S, Cavdar G, Senger SS, Akkoçlu G. Central nervous system aspergillosis in an immunocompetent patient. J Infect Dev Ctries. 2011;5:313–315. doi: 10.3855/jidc.1461. [DOI] [PubMed] [Google Scholar]
- 12.Lin SJ, Schranz J, Teutsch SM. Aspergillosis case-fatality rate : systematic review of the literature. Clin Infect Dis. 2001;32:358–366. doi: 10.1086/318483. [DOI] [PubMed] [Google Scholar]
- 13.Liu W, Chen H, Cai B, Li G, You C, Li H. Successful treatment of sellar aspergillus abscess. J Clin Neurosci. 2010;17:1587–1589. doi: 10.1016/j.jocn.2010.03.040. [DOI] [PubMed] [Google Scholar]
- 14.Maiorano E, Favia G, Capodiferro S, Montagna MT, Lo Muzio L. Combined mucormycosis and aspergillosis of the oro-sinonasal region in a patient affected by Castleman disease. Virchows Arch. 2005;446:28–33. doi: 10.1007/s00428-004-1126-x. [DOI] [PubMed] [Google Scholar]
- 15.Merseburger AS, Oelke M, Hartmann J, Stenzl A, Kuczyk MA. Intracranial aspergillosis in a non-immunocompromised patient treated for muscle-invasive bladder cancer. Int J Urol. 2004;11:666–668. doi: 10.1111/j.1442-2042.2004.00850.x. [DOI] [PubMed] [Google Scholar]
- 16.Miaux Y, Ribaud P, Williams M, Guermazi A, Gluckman E, Brocheriou C, et al. MR of cerebral aspergillosis in patients who have had bone marrow transplantation. AJNR Am J Neuroradiol. 1995;16:555–562. [PMC free article] [PubMed] [Google Scholar]
- 17.Joung MK, Kong DS, Song JH, Peck KR. Concurrent nocardia related brain abscess and semi-invasive pulmonary aspergillosis in an immunocompetent patient. J Korean Neurosurg Soc. 2011;49:305–307. doi: 10.3340/jkns.2011.49.5.305. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Mylonakis E, Paliou M, Sax PE, Skolnik PR, Baron MJ, Rich JD. Central nervous system aspergillosis in patients with human immunodeficiency virus infection. Report of 6 cases and review. Medicine (Baltimore) 2000;79:269–280. doi: 10.1097/00005792-200007000-00008. [DOI] [PubMed] [Google Scholar]
- 19.Norlinah MI, Ngow HA, Hamidon BB. Angioinvasive cerebral aspergillosis presenting as acute ischaemic stroke in a patient with diabetes mellitus. Singapore Med J. 2007;48:e1–e4. [PubMed] [Google Scholar]
- 20.Oner AY, Celik H, Akpek S, Tokgoz N. Central nervous system aspergillosis : magnetic resonance imaging, diffusion-weighted imaging, and magnetic resonance spectroscopy features. Acta Radiol. 2006;47:408–412. doi: 10.1080/02841850600580325. [DOI] [PubMed] [Google Scholar]
- 21.Phuttharak W, Hesselink JR, Wixom C. MR features of cerebral aspergillosis in an immunocompetent patient : correlation with histology and elemental analysis. AJNR Am J Neuroradiol. 2005;26:835–838. [PMC free article] [PubMed] [Google Scholar]
- 22.Pollack E, Bhaya A, Law M. Differentiating intracranial aspergillosis from a high grade glioma using MRI and MR spectroscopic imaging. J Neuroimaging. 2007;17:361–366. doi: 10.1111/j.1552-6569.2007.00105.x. [DOI] [PubMed] [Google Scholar]
- 23.Ruhnke M, Kofla G, Otto K, Schwartz S. CNS aspergillosis : recognition, diagnosis and management. CNS Drugs. 2007;21:659–676. doi: 10.2165/00023210-200721080-00004. [DOI] [PubMed] [Google Scholar]
- 24.Schaefer PW, Grant PE, Gonzalez RG. Diffusion-weighted MR imaging of the brain. Radiology. 2000;217:331–345. doi: 10.1148/radiology.217.2.r00nv24331. [DOI] [PubMed] [Google Scholar]
- 25.Schwartz S, Thiel E. Update on the treatment of cerebral aspergillosis. Ann Hematol. 2004;83(Suppl 1):S42–S44. doi: 10.1007/s00277-004-0849-8. [DOI] [PubMed] [Google Scholar]
- 26.Siddiqui K, Douglas M, Carey M, Benamer H. A case of invasive aspergillosis in a patient with no identifiable immunodeficiencies. Libyan J Med. 2008;3:49–51. doi: 10.4176/071011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Tempkin AD, Sobonya RE, Seeger JF, Oh ES. Cerebral aspergillosis : radiologic and pathologic findings. Radiographics. 2006;26:1239–1242. doi: 10.1148/rg.264055152. [DOI] [PubMed] [Google Scholar]
- 28.Yamada K, Shrier DA, Rubio A, Shan Y, Zoarski GH, Yoshiura T, et al. Imaging findings in intracranial aspergillosis. Acad Radiol. 2002;9:163–171. doi: 10.1016/s1076-6332(03)80166-6. [DOI] [PubMed] [Google Scholar]
- 29.Young RF, Gade G, Grinnell V. Surgical treatment for fungal infections in the central nervous system. J Neurosurg. 1985;63:371–381. doi: 10.3171/jns.1985.63.3.0371. [DOI] [PubMed] [Google Scholar]
- 30.Zinreich SJ, Kennedy DW, Malat J, Curtin HD, Epstein JI, Huff LC, et al. Fungal sinusitis : diagnosis with CT and MR imaging. Radiology. 1988;169:439–444. doi: 10.1148/radiology.169.2.3174990. [DOI] [PubMed] [Google Scholar]