Abstract
Purpose
To compare the foveal thickness (FT) parameters measured by Stratus optical coherence tomography (OCT) and Spectralis OCT in various retinal diseases and to construct conversion formulas between the two types of OCT devices.
Methods
We examined 366 consecutive patients (475 eyes) with retinal diseases and 13 normal controls (13 eyes). The patients were categorized into eight retinal disease groups. The mean amount and distribution of foveal thickness differences (FTD) measured by Stratus and Spectralis OCT were determined, and conversion formulas were constructed for Stratus OCT FT from Spectralis OCT FT for each retinal disease group.
Results
Among retinal diseases, the mean FTD was significantly larger in exudative age-related macular degeneration (AMD) patients (mean ± SD, 94.0 ± 55.0 µm) compared to normal subjects (66.2 ± 11.7 µm; p < 0.0001). The proportion of eyes with a mean FTD outside 1.96 standard deviations of normal subject FTD was greatest in the exudative AMD (50.0%) group and smallest in the macular hole (18.2%) group. The predicted FTs obtained through the conversion formulas showed lower variance than the actual FTD values, especially in the exudative AMD group. The prediction line for exudative AMD deviated most from that of normal subjects.
Conclusions
FTD shows diverse values and variances among various retinal diseases, especially in exudative AMD, which indicates that Stratus OCT FT cannot be predicted from Spectralis OCT FT by FTD value alone. We constructed statistically significant conversion formulas, which provided more reliable methods to predict Stratus OCT-measured FT from Spectralis OCT measurements for different retinal disease groups.
Keywords: Foveal thickness, Optical coherence tomography, Prediction, Spectral-domain, Time-domain
Optical coherence tomography (OCT) is the most common imaging tool used to examine the macula, as it is the only instrument that provides direct visualization of the in vivo retinal structure [1]. The traditional OCT technique involves time-domain OCT (TD-OCT) [2-5], where retinal depth information is obtained with a reference arm after longitudinal translation over time [6]. Good reproducibility of retinal thickness measurements by Stratus OCT (Carl Zeiss Meditec, Dublin, CA, USA) has been demonstrated [7,8]. However, since the time-domain method samples only one point at a time, a relatively long period of time is needed to obtain A- and B-scan images, resulting in lower image resolution compared to spectral domain-OCT (SD-OCT) [9].
Newer SD-OCT offers improved image resolution of less than 5 to 7 µm, dramatically faster acquisition speeds (18,000 to 40,000 A-scans/second), and detailed views of the intraretinal microstructures as well as three-dimensional images of the retina [8,10-12]. In SD-OCT, light beams returning from the sample and reference paths are combined at the detector, and then a spectrometer resolves the interference signals throughout the depth of each A-scan without varying the length of the reference path [9]. This allows the acquisition of retinal images approximately 50 times faster with SD-OCT than with TD-OCT [13] and results in improved resolution of the B-scan images and better delineation of the retinal layers, including the retinal pigment epithelium (RPE)-Bruch's membrane choriocapillaris complex [14,15].
Numerous studies and clinical trials have used foveal thickness (FT) values that are measured by Stratus OCT for the determination of macular lesions, such as those in exudative age-related macular degeneration (AMD) and macular edema, and for the assessment of treatment response and guidelines for retreatment [16-18]. In order to use the known treatment and follow-up guidelines that are proposed in numerous clinical studies, it is essential to match the thickness parameters of different OCT devices, especially between TD-OCT and SD-OCT. A recent study on normal subjects demonstrated that Spectralis OCT (Heidelberg Engineering Inc., Heidelberg, Germany) obtained retinal thickness measurements that were increased by approximately 65 to 70 µm compared to Stratus OCT measurements [19].
However, studies have reported discrepancies in FT values measured by TD-OCT and SD-OCT in eyes with various retinal diseases [20-23]. Stratus OCT defines retinal thickness from the internal limiting membrane (ILM) to the complex of the inner and outer segments (IS/OS) of the photoreceptor junction and RPE layer, while Spectralis OCT selects images from the ILM to the RPE-Bruch's membrane choriocapillaris complex [12]. Because the segmentation algorithm for each OCT instrument is different, the measured FT should also be different for each. One study using Stratus and Spectralis OCT reported that the mean foveal thickness differences (FTD) in eyes with choroidal neovascularization (CNV) and AMD were significantly greater than those in normal eyes and in other retinal diseases [20]. Conversion equations and their application to TD-OCT and SD-OCT for the examination of eyes with diabetic macular edema [22] and with AMD [23] have been previously reported. However, no studies have compared the distribution of FTDs in various retinal diseases or constructed conversion formulas that predict TD-OCT-measured FT on the basis of SD-OCT-measured FT across different retinal diseases. In addition, the association between the amount of FTD and the disease severity indicated by FT has not yet been investigated.
The purpose of this study was to compare the measurement values obtained using TD-OCT (Stratus) and SD-OCT (Spectralis) devices in normal and diseased retinas in order to construct conversion formulas in normal eyes and eyes with various retinal diseases. These conversion formulas must be as accurate as possible in order to predict the FT provided by Stratus OCT on the basis of data obtained using Spectralis OCT. The accuracy of these formulas must also be verified to ensure minimal errors in clinical application.
Materials and Methods
This was a retrospective cross-sectional study comparing measurement values between TD-OCT and SD-OCT devices in normal and diseased retinas. This study was approved by the Institutional Review Board of Seoul National University Bundang Hospital, and the tenets of the Declaration of Helsinki were followed throughout the study.
Consecutive patients who visited the retina clinic of Seoul National University Bundang Hospital and who were examined with both Stratus and Spectralis OCT between September 2009 and October 2009 were included in this study. Because the new Spectralis OCT was first introduced to our hospital in September 2009, there was no information regarding the FT of the new SD-OCT machine. Therefore, all subjects who visited the retina clinic during this period and who were indicated for OCT examination underwent both Stratus and Spectralis OCT examinations of a dilated pupil on the same day by two well-trained OCT technicians. The medical records and OCT data of 366 consecutive patients (475 eyes) and 13 normal controls (13 eyes) were retrospectively reviewed. Ocular disorder diagnoses were obtained from a computerized database of electronic medical records. Thirteen eyes of 13 subjects who visited the retina clinic during the study period without posterior segment pathology and with definite normal features on OCT scanning were categorized as normal.
Eyes with retinal pathology were categorized into eight retinal disease groups: epiretinal membrane (ERM, n = 68), macular hole (MH, n = 22), diabetic retinopathy (DR, n = 127), retinal vein occlusion (RVO, n = 53), exudative AMD (n = 80), nonexudative AMD (n = 25), central serous chorioretinopathy (CSC, n = 26), and others (rhegmatogenous retinal detachment, n = 18; normal tension glaucoma, n = 15; uveitis, n = 19; and senile retinoschisis, n = 9). Retinal diseases with pathological changes that were mostly confined within the inner retina, including ERM, MH, DR, and RVO, were defined as the inner-retinal disease group.
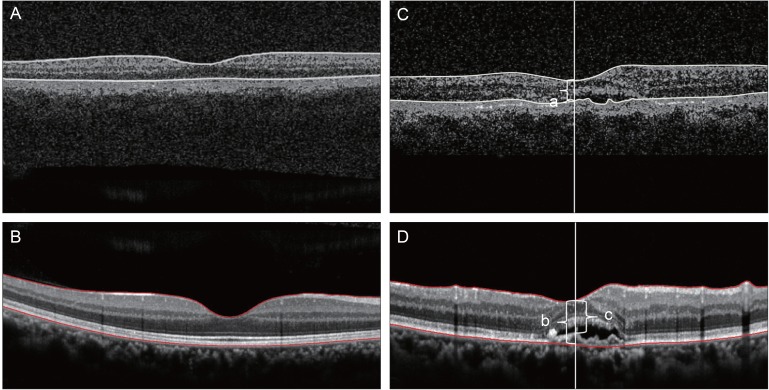
When measuring FT with Stratus OCT, we used a 6-mm linear cross-hair pattern that was centered on the fovea (512 A-scans; scan length, 6.0 mm) and a fast macular thickness map pattern. The automated analysis package of the Stratus OCT defines retinal thickness as the distance between the ILM and the complex of the photoreceptor junction of the IS/OS layer (Fig. 1A) [1,24].
Fig. 1.
Representative cross-sections taken by Stratus (A) and Spectralis (B) optical coherence tomography (OCT) in normal controls, and the measurement of foveal thickness (FT) by Stratus OCT (C) and Spectralis OCT (D) in exudative age-related macular degeneration (AMD). The borders of retinas in normal controls measured by Stratus OCT are outlined as white lines, (A) and those measured by Spectralis OCT are outlined as red lines (B). Meanwhile, the FT of Stratus OCT in exudative AMD, which did not include choroidal neovascularization (CNV) thickness (white lines), is indicated by 'a' (C). However, the FT of Spectralis OCT in exudative AMD included CNV thickness (red lines), and the FT measured by Spectralis OCT before and after considering CNV thickness is indicated by 'b' and 'c', respectively (D).
The axial resolution of Spectralis OCT is less than 7 µm with a data-acquisition speed of 40,000 A-scans/second [24]. Scans were obtained with the automated averaging system (automatic real time mean = 10) activated in order to amplify the signals and to reduce the noise in the images [24]. Retinal thickness was defined as the distance between the ILM to the bottom of the RPE-Bruch's membrane choriocapillaris complex by automatic segmentation algorithms of the Spectralis software (Fig. 1B) [1,24]. The average retinal thickness within a 1-mm radius of the central fovea on the Early Treatment Diabetic Retinopathy Study grid, as measured using Stratus and Spectralis OCT, was defined as FT in normal subjects and subjects with any form of retinal disease, including macular hole [1].
For each scan, the color thickness maps and horizontal line scans of the Stratus and Spectralis OCTs were reviewed for image artifacts due to failure of identification of the inner or outer retinal boundaries or to segmentation algorithm failure, that is, when segmentation lines of the OCT images were not properly placed. All comparisons and analyses of FT were performed after the exclusion of artifacts on OCT scans.
The FTD was defined as the difference between the FT values that were measured by Stratus and Spectralis OCT in the same patient. The mean value of the FTDs of each retinal disease group was compared to that of the normal group. The proportion of eyes that had FTDs that were 1.96 standard deviations (SD) from the mean FTD of normal eyes was compared between disease groups, and the coefficients of variation of the FTDs were calculated in order to analyze the degree of relative dispersion of the FTDs in each disease category.
Because the thickness of the CNV was included in the FT that was measured by Spectralis OCT (Fig. 1D), but not in the Stratus OCT-measured FT (Fig. 1C), each OCT image of the exudative AMD group was reviewed to measure the CNV thickness using the Heidelberg Explorer ver. 4.0 software package (Heidelberg Engineering Inc.). Erroneous outer segmentation lines in OCT images obtained for patients with exudative AMD, including CNV thickness, were repositioned manually into the RPE-Bruch's membrane junction. CNV thickness was then subtracted from the original FT measured using Spectralis OCT and was defined as a Modified Spectralis OCT FT. In addition, the FTD between the FT of Stratus OCT and modified Spectralis OCT FT was defined as Modified FTD. Finally, an additional conversion formula was constructed from the FT value measured by Stratus and Spectralis OCT and CNV thickness using generalized estimating equations (GEE).
Statistical analysis was performed with SAS ver. 9.1 (SAS Institute Inc., Cary, NC, USA). Comparisons of the differences in FTDs of patients with different retinal disorders measured by Stratus and Spectralis OCT were performed using GEE to adjust for the inclusion of bilateral eyes of individuals. The working correlation structure was assumed to be exchangeable or independent. The mean FTDs of the disease groups and the proportions of eyes that had an FTD that was 1.96 SD from the mean FTD of normal eyes were compared to those of normal controls using GEE. Formulas based on GEE were constructed to estimate the Stratus OCT FT from Spectralis OCT FT, and the discrepancies between the predicted and actual OCT FT were presented and compared among groups. The associations between FT and FTD were analyzed, and formulas based on the GEE were constructed for the normal, inner-retinal disease, and exudative AMD groups. A p-value less than 0.05 was considered statistically significant.
Results
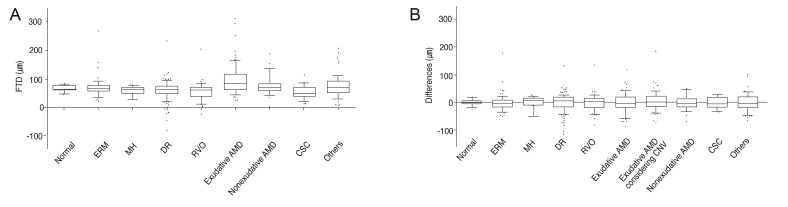
The mean age of each group and the number of eyes examined in each group are shown in Table 1. The mean age ± SD of all subjects was 61.5 ± 13.1 years (range, 14 to 88 years). The mean FTD was largest in the exudative AMD group (94.0 ± 55.0 µm), followed by the nonexudative AMD group (75.2 ± 36.2 µm), others (73.9 ± 41.1 µm), ERM (69.2 ± 34.5 µm), normal (66.2 ± 11.7 µm), DR (60.5 ± 37.6 µm), MH (57.2 ± 20.7 µm), RVO (54.5 ± 33.2 µm), and CSC (53.2 ± 23.6 µm) groups (Fig. 2A and Table 2). The mean FTD was greater in the exudative AMD group than in normal controls (p < 0.0001, GEE), but there were no significant differences between the mean FTD of the other retinal diseases and that of the normal group. The coefficient of variation of FTD was largest in the DR group (62.2%) and smallest in the normal group (17.6%) (Table 2).
Table 1.
Demographic data of normal subjects and patients with one of eight retinal diseases
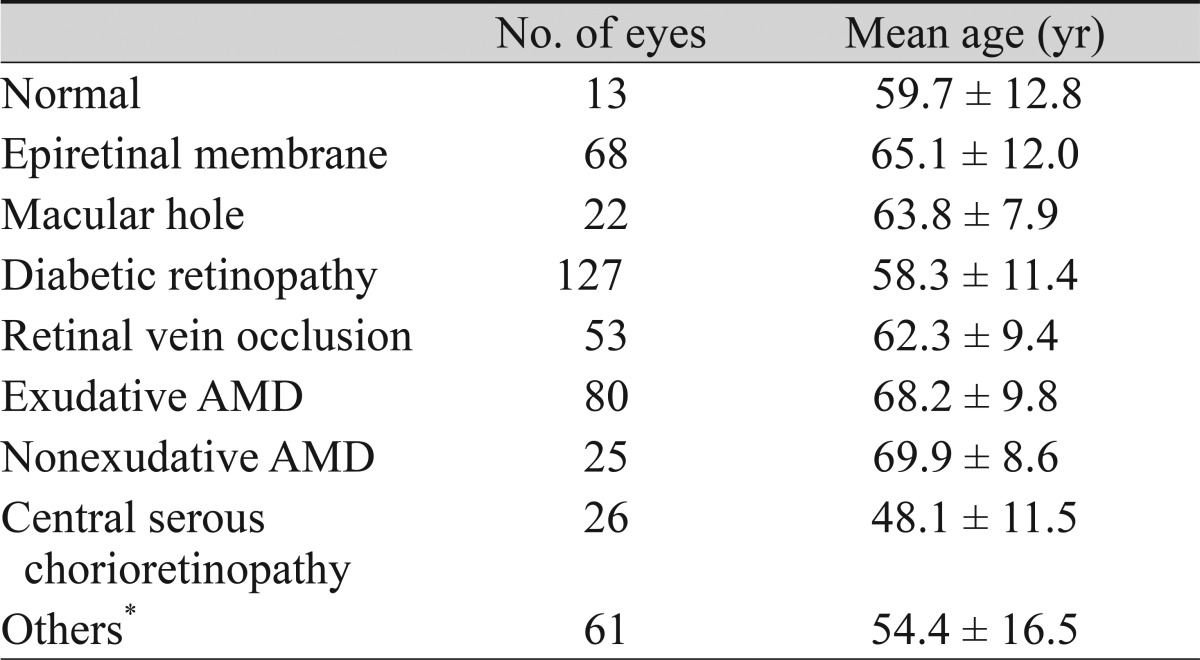
Values are presented as number or mean ± standard deviation.
AMD = age-related macular degeneration.
*Others group includes retinal diseases such as rhegmatogenous retinal detachment, normal tension glaucoma, uveitis, and senile retinoschisis.
Fig. 2.
(A) The mean foveal thickness difference (FTD) of normal subjects and subjects with retinal diseases. The mean FTD was greatest in the exudative age-related macular degeneration (AMD) group, and it was greater than that of normal controls (p < 0.0001, generalized estimating equations [GEE]). (B) The means and standard deviations (SD) of the differences between the virtual foveal thickness (FT) of Stratus optical coherence tomography (OCT) calculated by the conversion formulas and the actual FT measured by Stratus OCT in each group. The SD was decreased by applying conversion formulas, especially in the exudative AMD group. The horizontal lines within the white boxes indicate medians, the upper and lower limits of the white boxes indicate 75th and 25th percentiles, respectively, the upper and lower limits of the whiskers indicate 90th and 10th percentiles, and the dots over and under the whiskers indicate the values outside the 90th and 10th percentiles. ERM = epiretinal membrane; MH = macular hole; DR = diabetic retinopathy; RVO = retinal vein occlusion; CSC = central serous chorioretinopathy; CNV = choroidal neovascularization.
Table 2.
Comparison of the mean FT ± SD measured by Stratus and Spectralis OCTs and the mean FTD ± SD in subjects with different retinal disorders
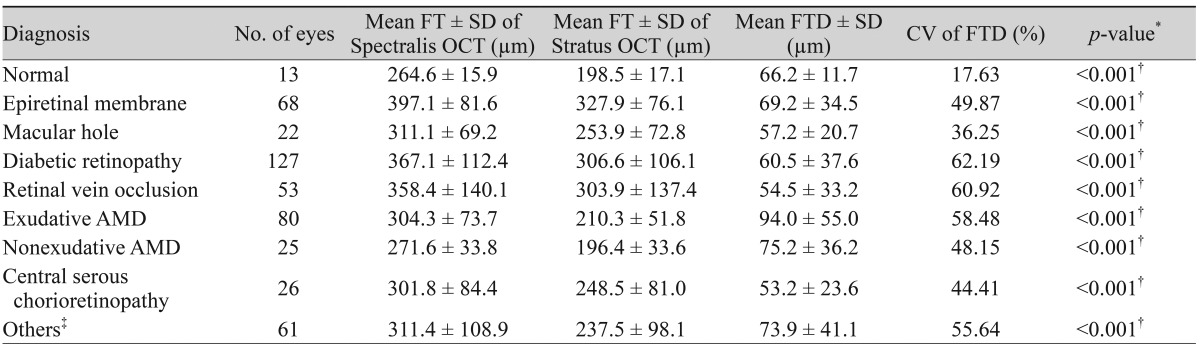
FT = foveal thickness; SD = standard deviation; OCT = optical coherence tomography; FTD = foveal thickness difference; CV = coefficient of variation; AMD = age-related macular degeneration.
*From paired t-tests of the differences between Stratus OCT-measured FT and Spectralis OCT-measured FT in normal controls and each retinal disease group; †<0.05 and statistically significant; ‡Others group includes retinal diseases such as rhegmatogenous retinal detachment, normal tension glaucoma, uveitis, and senile retinoschisis.
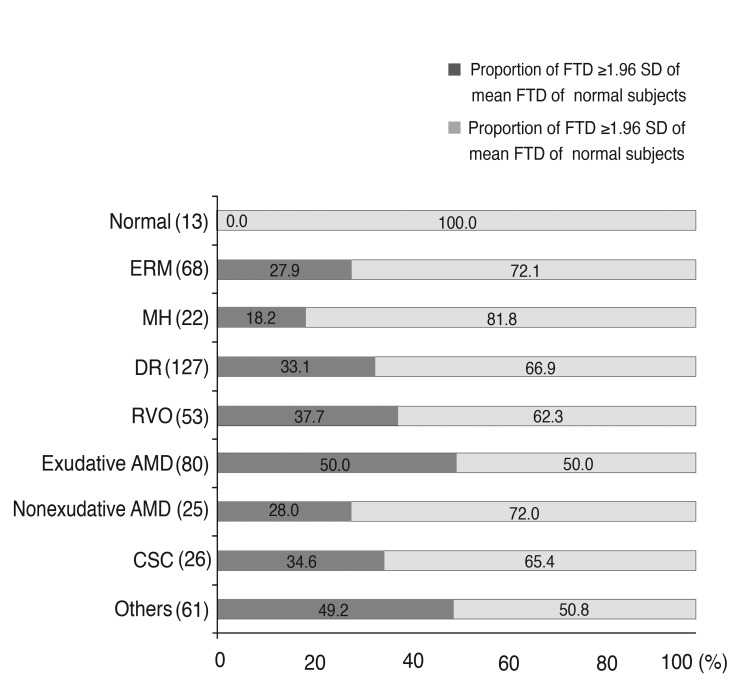
The proportion of eyes showing FTD values outside of 1.96 SD of the normal control values (FTD >89.0 or <43.3 µm) was greatest in the exudative AMD group (50.0%) and smallest in the macular hole group (18.2%) (Fig. 3). However, no statistically significant difference was found when comparing the proportions among disease groups.
Fig. 3.
The proportions of eyes with different retinal disorders with a mean foveal thickness difference (FTD) that was 1.96 standard deviations (SDs) outside the mean FTD of normal subjects. The proportion was greatest in the exudative age-related macular degeneration (AMD) group. The numbers in parentheses indicate the number of patients in each group. ERM = epiretinal membrane; MH = macular hole; DR = diabetic retinopathy; RVO = retinal vein occlusion; CSC = central serous chorioretinopathy.
In normal subjects, there were no correlations between FTD and Stratus OCT-measured FT (FTStratus, p = 0.13, GEE) or between FTD and Spectralis OCT-measured FT (FTSpectralis, p = 0.39, GEE). In the inner-retinal disease group, there was no significant correlation between FTD and FTStratus (p = 0.81, GEE), but a statistically significant positive correlation was observed between FTD and FTSpectralis (p = 0.0004, GEE, FTD = 0.10 × FTSpectralis + 25.76). In the exudative AMD group, the correlations of FTD and Modified FTD with FT measured by Stratus and Spectralis OCT were analyzed. There was a statistically significant positive correlation between FTSpectralis and FTD (p < 0.0001, GEE, FTD = 0.53 × FTSpectralis - 67.61), but no significant correlation between FTStratus and FTD (p = 0.59, GEE), between FTStratus and modified FTD (p = 0.26, GEE), or between modified FTSpectralis and modified FTD (p = 0.63, GEE).
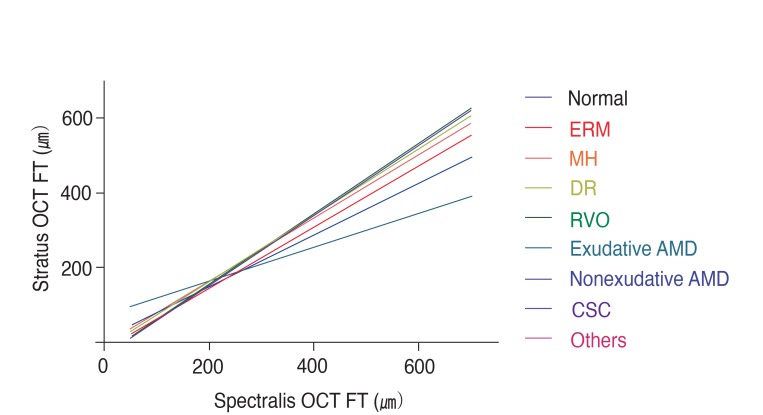
Finally, the conversion formulas of FTStratus from FTSpectralis shown in Table 3 and Fig. 4 were statistically significant, except in the nonexudative AMD group. In Fig. 4, the prediction lines of the inner-retinal disease groups were close to that of the normal group, while the exudative AMD group showed a prediction line that deviated most from that of normal subjects and, thus, had the lowest correlation coefficient (0.47). For the exudative AMD group, an additional formula was constructed that considered CNV thickness, which resulted in a correlation coefficient for FTSpectralis (0.79) that was closer to 1.0 than that of the original formula. Fig. 2B shows the averages and SDs of the differences between the FTStratus values calculated by the conversion formulas and the actual FTStratus in each group. The SD was largest in the exudative AMD group (38.6 µm) and lowest in the normal subjects (11.3 µm). The SDs of the differences between predicted FTStratus and actual FTStratus (the right column of Table 3) were smaller than the SDs of the differences in FTDs (Table 2) in each group, except for the MH group. The SD was dramatically decreased by applying the conversion formulas in the exudative AMD group (38.6 µm from 55.0 µm). Furthermore, in the exudative AMD group, the additional conversion formula that considered CNV thicknesses was also applied, and the SD after considering CNV thicknesses (37.2 µm) was slightly smaller than that before considering CNV thicknesses (38.6 µm).
Table 3.
The conversion formulas between the FT measured by Stratus OCT and Spectralis OCT in normal subjects and subjects with various retinal diseases
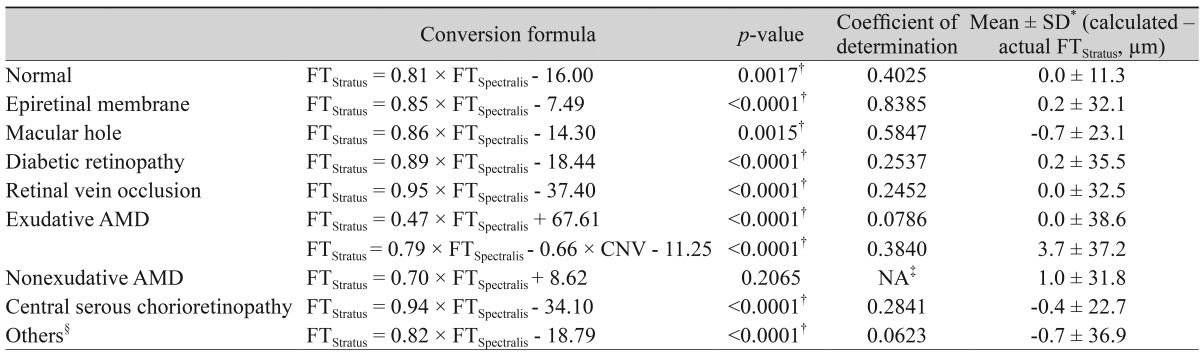
FT = foveal thickness; OCT = optical coherence tomography; FTStratus = FT measured by Stratus OCT; FTSpectralis = FT measured by Spectralis OCT; AMD = age-related macular degeneration; CNV = choroidal neovascularization; NA = not available.
*Standard deviations of the differences between FTStratus calculated by the conversion formulas and actual FTStratus; †p-value with an asterisk is <0.05 and statistically significant; ‡The conversion formula for eyes with nonexudative AMD was not statistically significant, so the coefficient of determination was not available; §Others group includes retinal diseases such as rhegmatogenous retinal detachment, normal tension glaucoma, uveitis, and senile retinoschisis.
Fig. 4.
The graphs of the conversion formulas between the foveal thickness (FT) measured by Stratus optical coherence tomography (OCT) and Spectralis OCT in normal subjects and subjects with various retinal diseases. ERM = epiretinal membrane; MH = macular hole; DR = diabetic retinopathy; RVO = retinal vein occlusion; AMD = age-related macular degeneration; CSC = central serous chorioretinopathy.
Discussion
OCT imaging currently has a large role in the diagnosis and management of exudative AMD, and it has a significant impact on the management of patients, especially with regard to treatment with anti-vascular endothelial growth factor agents [25]. Despite its use, there is some variation among different OCT systems in how images are captured, quantified, and displayed to the clinician, and these factors may have a significant impact on how OCT data is interpreted, which subsequently affects management decisions [25].
It is well known that Stratus OCT defines the outer retinal border as the complex of the photoreceptor IS/OS junction layer and RPE, while Spectralis OCT selects the Bruch's membrane [12,21]. In patients with exudative AMD, the retinal outer structure can be disturbed by CNV, RPE detachment, subretinal fluid accumulation, intraretinal edema, or fibrotic scars [26]. These retinal morphological changes may make the differentiation of retinal layers by the OCT software more difficult. This may explain why the mean FTD and the proportion of patients with a mean FTD that was 1.96 SDs outside of the mean FTD of normal subjects were greatest in patients with exudative AMD. Likewise, the revised conversion formula for FTStratus for exudative AMD using CNV thickness (Table 3) was well-matched to our expectations of low SDs and higher correlation coefficients, and this can be interpreted to mean that the FTStratus is equivalent to FTSpectralis less the CNV thickness (equivalent to the modified FTSpectralis).
There was a statistically significant positive correlation between FTSpectralis and FTD in the exudative AMD group. However, there was no significant correlation between FTStratus and FTD in that disease group. The higher resolution and accuracy of Spectralis OCT may be the main reasons why this has been shown in previous reports [27,28]. Another explanation is that Spectralis OCT includes CNV during the measurement of FT, and the included CNV thickness should be larger in eyes with large FTSpectralis, which leads to increased FTD with increasing FTSpectralis. This explanation is also supported by the fact that there was no correlation between FTSpectralis and modified FTD (p = 0.63, GEE). Using the Modified FTD formulation, therefore, the FTD can be controlled in the accepted range even in eyes with large FT values. In Fig. 4, the prediction line for exudative AMD shows increasing discrepancy in FTStratus values from the line of normal subjects. This could also be explained by the increasing thickness of CNV in exudative AMD eyes with increasing FTSpectralis.
However, the FTD values of eyes in the inner-retinal disease group were associated with FTSpectralis but not with FTStratus. The better accuracy of Spectralis OCT in delineating retinal borders in eyes with inner-retinal pathology, as well as outer-retinal diseases, may support the positive correlation between FTD and FTSpectralis. The use of the eye tracker when scanning the retina with Spectralis OCT results in a better localization of the fovea and a lower incidence of artifacts than when using Stratus OCT. In summary, FTD values are expected to be greater in eyes with either inner-retinal disease or exudative AMD showing large FT on Spectralis OCT than in eyes with small FT.
In previous studies on diabetic macular edema [21,22], the mean FTDs between the FTs measured by Stratus and Spectralis OCTs were 77.7 and 76 µm, respectively, whereas that of the patients with DR in this study was 60.5 µm. In another study that included eyes with various retinal diseases [20], the mean FTD between the FTs measured by Stratus and Spectralis OCTs was largest (97.1 µm) in CNV (n = 9), followed by 65.3 µm in DR (n = 12), 84.5 µm in ERM (n = 10), and 60.7 µm in RVO (n = 7), which generally corresponded to our results (94.0 µm in Exudative AMD [n = 80], 60.5 µm in DR [n = 127], 69.2 µm in ERM [n = 68], and 54.5 µm in RVO [n = 53]).
In the present study, we constructed conversion formulas that predicted FTStratus from FTSpectralis for each retinal disease group (Fig. 4 and Table 3). The conversion formulas were different among the disease groups and statistically significant, except for eyes with nonexudative AMD. It should be noted that the SDs of the differences between actual FTStratus and predicted FTStratus calculated from FTSpectralis using the conversion formulas (Table 3) were smaller than the SDs of FTD (Table 2). Thus, these formulas can be useful when calculating FTStratus from FTSpectralis according to the corresponding retinal disease, and they may be more precise than considering mean FTD alone, irrespective of the disease diagnosis.
The exudative AMD group showed the most dramatic decrease in the SD of the discrepancy, from 55.0 to 38.6 µm, which indicates that the conversion formula was more accurate in eyes with exudative AMD (Fig. 2B and Table 3). In the exudative AMD group, when CNV thickness was included in the model, the conversion formula showed a correlation coefficient that was closer to 1.0 (0.79) and a smaller SD (37.2 µm) compared to the conversion formula that included FT alone (0.47 and 38.6 µm), which implies that the prediction was more firm after accounting for CNV thickness.
There are several limitations to the present study. Because we included consecutive patients who visited our hospital during the study period, the number of patients and the severity of retinal diseases were not well controlled, which might have influenced the results and statistical significance. Another limitation is that we did not measure the FT of the same eyes with two different SD-OCT devices, and therefore our results cannot be applied to other types of SD-OCT devices. However, from our results, it is expected that the inclusion of CNV in the outer retinal boundary is the most important determining factor for measured FT of eyes with CNV. The segmentation algorithms of OCT devices should be tested when the prediction of FTStratus is required, and there may be less variance in FTD when using OCT devices with segmentation algorithms that are similar to those of Stratus OCT, such as Cirrus HD OCT (Carl Zeiss Meditec).
In conclusion, the differences in the measured FTs between Stratus and Spectralis OCT were not uniform among retinal disease groups and showed large inter-individual variations compared to eyes with normal retinal anatomies, especially in eyes with exudative AMD. Thus, simple adjustments of mean FTD between two OCT devices can lead to incorrect results. Statistically significant conversion formulas could be constructed for different retinal disease groups, and these can be used when predictions of Stratus OCT-measured FT from Spectralis OCT-measured FT are required.
Acknowledgements
We thank the Medical Research Collaboration Center of Seoul National University Bundang Hospital for assistance in statistical analysis. This study was supported by the Translational Research Program (A111161) funded by the Korea Health Technology R&D Project, Ministry of Health and Welfare, Korea.
Footnotes
This study was previously presented in part at the Symposium and Congress of Korean Ophthalmological Society, Busan, Korea, April 2010.
No potential conflict of interest relevant to this article was reported.
References
- 1.Leung CK, Cheung CY, Weinreb RN, et al. Comparison of macular thickness measurements between time domain and spectral domain optical coherence tomography. Invest Ophthalmol Vis Sci. 2008;49:4893–4897. doi: 10.1167/iovs.07-1326. [DOI] [PubMed] [Google Scholar]
- 2.Huang D, Swanson EA, Lin CP, et al. Optical coherence tomography. Science. 1991;254:1178–1181. doi: 10.1126/science.1957169. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Hee MR, Izatt JA, Swanson EA, et al. Optical coherence tomography of the human retina. Arch Ophthalmol. 1995;113:325–332. doi: 10.1001/archopht.1995.01100030081025. [DOI] [PubMed] [Google Scholar]
- 4.Puliafito CA, Hee MR, Lin CP, et al. Imaging of macular diseases with optical coherence tomography. Ophthalmology. 1995;102:217–229. doi: 10.1016/s0161-6420(95)31032-9. [DOI] [PubMed] [Google Scholar]
- 5.Thomas D, Duguid G. Optical coherence tomography: a review of the principles and contemporary uses in retinal investigation. Eye (Lond) 2004;18:561–570. doi: 10.1038/sj.eye.6700729. [DOI] [PubMed] [Google Scholar]
- 6.Forte R, Cennamo GL, Finelli ML, de Crecchio G. Comparison of time domain Stratus OCT and spectral domain SLO/OCT for assessment of macular thickness and volume. Eye (Lond) 2009;23:2071–2078. doi: 10.1038/eye.2008.363. [DOI] [PubMed] [Google Scholar]
- 7.Paunescu LA, Schuman JS, Price LL, et al. Reproducibility of nerve fiber thickness, macular thickness, and optic nerve head measurements using Stratus OCT. Invest Ophthalmol Vis Sci. 2004;45:1716–1724. doi: 10.1167/iovs.03-0514. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Gurses-Ozden R, Teng C, Vessani R, et al. Macular and retinal nerve fiber layer thickness measurement reproducibility using optical coherence tomography (OCT-3) J Glaucoma. 2004;13:238–244. doi: 10.1097/00061198-200406000-00012. [DOI] [PubMed] [Google Scholar]
- 9.Kakinoki M, Sawada O, Sawada T, et al. Comparison of macular thickness between Cirrus HD-OCT and Stratus OCT. Ophthalmic Surg Lasers Imaging. 2009;40:135–140. doi: 10.3928/15428877-20090301-09. [DOI] [PubMed] [Google Scholar]
- 10.Joeres S, Tsong JW, Updike PG, et al. Reproducibility of quantitative optical coherence tomography subanalysis in neovascular age-related macular degeneration. Invest Ophthalmol Vis Sci. 2007;48:4300–4307. doi: 10.1167/iovs.07-0179. [DOI] [PubMed] [Google Scholar]
- 11.Drexler W, Sattmann H, Hermann B, et al. Enhanced visualization of macular pathology with the use of ultrahigh-resolution optical coherence tomography. Arch Ophthalmol. 2003;121:695–706. doi: 10.1001/archopht.121.5.695. [DOI] [PubMed] [Google Scholar]
- 12.Sayanagi K, Sharma S, Kaiser PK. Comparison of retinal thickness measurements between three-dimensional and radial scans on spectral-domain optical coherence tomography. Am J Ophthalmol. 2009;148:431–438. doi: 10.1016/j.ajo.2009.04.008. [DOI] [PubMed] [Google Scholar]
- 13.Wojtkowski M, Bajraszewski T, Targowski P, Kowalczyk A. Real-time in vivo imaging by high-speed spectral optical coherence tomography. Opt Lett. 2003;28:1745–1747. doi: 10.1364/ol.28.001745. [DOI] [PubMed] [Google Scholar]
- 14.Alam S, Zawadzki RJ, Choi S, et al. Clinical application of rapid serial fourier-domain optical coherence tomography for macular imaging. Ophthalmology. 2006;113:1425–1431. doi: 10.1016/j.ophtha.2006.03.020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Srinivasan VJ, Wojtkowski M, Witkin AJ, et al. High-definition and 3-dimensional imaging of macular pathologies with high-speed ultrahigh-resolution optical coherence tomography. Ophthalmology. 2006;113:2054.e1–2054.e14. doi: 10.1016/j.ophtha.2006.05.046. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Lalwani GA, Rosenfeld PJ, Fung AE, et al. A variable-dosing regimen with intravitreal ranibizumab for neovascular age-related macular degeneration: year 2 of the PrONTO Study. Am J Ophthalmol. 2009;148:43–58.e1. doi: 10.1016/j.ajo.2009.01.024. [DOI] [PubMed] [Google Scholar]
- 17.Shimura M, Nakazawa T, Yasuda K, et al. Comparative therapy evaluation of intravitreal bevacizumab and triamcinolone acetonide on persistent diffuse diabetic macular edema. Am J Ophthalmol. 2008;145:854–861. doi: 10.1016/j.ajo.2007.12.031. [DOI] [PubMed] [Google Scholar]
- 18.Soheilian M, Ramezani A, Obudi A, et al. Randomized trial of intravitreal bevacizumab alone or combined with triamcinolone versus macular photocoagulation in diabetic macular edema. Ophthalmology. 2009;116:1142–1150. doi: 10.1016/j.ophtha.2009.01.011. [DOI] [PubMed] [Google Scholar]
- 19.Grover S, Murthy RK, Brar VS, Chalam KV. Comparison of retinal thickness in normal eyes using Stratus and Spectralis optical coherence tomography. Invest Ophthalmol Vis Sci. 2010;51:2644–2647. doi: 10.1167/iovs.09-4774. [DOI] [PubMed] [Google Scholar]
- 20.Han IC, Jaffe GJ. Comparison of spectral- and time-domain optical coherence tomography for retinal thickness measurements in healthy and diseased eyes. Am J Ophthalmol. 2009;147:847–858. 858.e1. doi: 10.1016/j.ajo.2008.11.019. [DOI] [PubMed] [Google Scholar]
- 21.Lammer J, Scholda C, Prunte C, et al. Retinal thickness and volume measurements in diabetic macular edema: a comparison of four optical coherence tomography systems. Retina. 2011;31:48–55. doi: 10.1097/IAE.0b013e3181e095a4. [DOI] [PubMed] [Google Scholar]
- 22.Ibrahim MA, Sepah YJ, Symons RC, et al. Spectral- and time-domain optical coherence tomography measurements of macular thickness in normal eyes and in eyes with diabetic macular edema. Eye (Lond) 2012;26:454–462. doi: 10.1038/eye.2011.293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Krebs I, Hagen S, Smretschnig E, et al. Conversion of Stratus optical coherence tomography (OCT) retinal thickness to Cirrus OCT values in age-related macular degeneration. Br J Ophthalmol. 2011;95:1552–1554. doi: 10.1136/bjo.2010.194670. [DOI] [PubMed] [Google Scholar]
- 24.Sayanagi K, Sharma S, Yamamoto T, Kaiser PK. Comparison of spectral-domain versus time-domain optical coherence tomography in management of age-related macular degeneration with ranibizumab. Ophthalmology. 2009;116:947–955. doi: 10.1016/j.ophtha.2008.11.002. [DOI] [PubMed] [Google Scholar]
- 25.Cukras C, Wang YD, Meyerle CB, et al. Optical coherence tomography-based decision making in exudative age-related macular degeneration: comparison of time- vs spectral-domain devices. Eye (Lond) 2010;24:775–783. doi: 10.1038/eye.2009.211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Menke MN, Dabov S, Knecht P, Sturm V. Reproducibility of retinal thickness measurements in patients with age-related macular degeneration using 3D Fourier-domain optical coherence tomography (OCT) (Topcon 3D-OCT 1000) Acta Ophthalmol. 2011;89:346–351. doi: 10.1111/j.1755-3768.2009.01692.x. [DOI] [PubMed] [Google Scholar]
- 27.Ray R, Stinnett SS, Jaffe GJ. Evaluation of image artifact produced by optical coherence tomography of retinal pathology. Am J Ophthalmol. 2005;139:18–29. doi: 10.1016/j.ajo.2004.07.050. [DOI] [PubMed] [Google Scholar]
- 28.Leung CK, Chan WM, Chong KK, et al. Alignment artifacts in optical coherence tomography analyzed images. Ophthalmology. 2007;114:263–270. doi: 10.1016/j.ophtha.2006.06.059. [DOI] [PubMed] [Google Scholar]