Abstract
Purpose
To evaluate the correlation of the distance Krimsky test and the alternate prism cover test (APCT) for the distance deviation in patients with horizontal strabismus.
Methods
Forty patients with horizontal strabismus (20 esotropia and 20 exotropia) were included in this study. Patients with a variable angle of deviation, vertical angle over 5 prism diopters, impaired binocular vision, or poor cooperation were excluded. We instructed the patient to look a target 6 meters away, and applied a prism over the patient's dominant eye while flashing a light source 33 centimeters from the middle of both eyebrows. When the corneal light reflexes were located on the center of each cornea, we measured the angle of deviation. We defined this method as 'distance Krimsky test,' and the angle measured by this method was compared with the conventional Krimsky test and APCT at distance. We analyzed the accuracy and intra- and inter-observer reliability.
Results
The angle of strabismus measured by the distance Krimsky test showed a significant agreement and correlation with the deviation angle measured by the APCT. We elicited the correlation gradient between the angle measured by the distance Krimsky test and the APCT. In addition, the distance Krimsky test showed significant intra- and inter-observer reliabilities.
Conclusions
The distance Krimsky test is expected to be more useful than the Krimsky test in measuring the distance angle of deviation for patients with strabismus in whom it is difficult to measure the angle of deviation using the APCT. The distance Krimsky test can be an accurate and useful test through the improvement of proficiency of examiners and the establishment of individualized normative data.
Keywords: Distance Krimsky test, Esotropia, Exotropia, Strabismus
The alternate prism cover test (APCT) is the most frequently used method to measure the angle of deviation in patients with strabismus, but it can only be used when both eyes have sufficient vision for fixation. In cases of sensory strabismus, severe amblyopia, and infantile strabismus, it is difficult to take measurements with the APCT due to insufficient vision or poor cooperation in these patients [1,2]. In such cases, the Hirschberg test or Krimsky test, which use corneal reflection for measuring the strabismic angle, are commonly used. Although these methods are useful in measuring the near angle of deviation, their accuracy for the distance angle of deviation is undefined because these methods use a near fixation-point [2,3]. When the difference between the near and the distance angle of strabismus is substantial, a serious error may occur if strabismic surgery is conducted only on the basis of the near angle of deviation. In addition, infantile esotropia patients require surgery before the age of 2 in order to acquire single binocular vision [4-7]. It is not easy to measure the distance angle of deviation at this age, and there is a problem in the accuracy of the measurements when using the near deviation angle measured with the corneal reflection method. In spite of these problems, there are no reliable data regarding the accuracy or reproducibility of the corneal reflection method at distance. Therefore, in this study, we aimed to examine the usefulness and accuracy of the distance Krimsky test, and the correlation with other tests such as the conventional Krimsky test and the APCT by comparing the angle of deviation.
Materials and Methods
Twenty patients with exotropia and 20 patients with esotropia, who visited our clinic from March 2009 to June 2010 were enrolled in this study along with 5 orthophoric patients as the control group.
The inclusion criteria were patients over 5 years old with good cooperation, the best corrected visual acuity over 0.1 logarithm of minimum angle resolution in both eyes, no change in strabismic angle at near and distance for more than 3 months, and constant strabismus.
The exclusion criteria were as follows: 1) patients with a variable angle of deviation such as heterophoria, intermittent strabismus, accommodative strabismus, incomitant strabismus, and strabismus with a vertical angle more than 5 prism diopters (PD). 2) Patients with poor binocular vision such as amblyopia. 3) Uncooperative patients such as infants and toddlers. 4) Patients with abnormal findings in the other ophthalmic exams.
We instructed each patient to focus on a target 6 meters away and applied a prism over the patient's dominant eye with a light source from 33 centimeters away at the middle of both eyebrows. When the corneal light reflections were located on the center of each cornea, we measured the angle of deviation. We defined this method as the 'distance Krimsky test'. The conventional Krimsky test was conducted in such a way that both the fixation target and the light source were 33 centimeters from the middle of both eyebrows. In our study, the APCT was conducted at a distance and was considered as the standard method of measuring the distance angle of deviation. In the case of an accompanying vertical strabismic angle, the vertical deviation measured by the APCT at distance was corrected with prism before measuring the horizontal strabismic angle in the distance Krimsky test.
To analyze the accuracy of the distance Krimsky test, we compared the deviation angles measured by the distance Krimsky test and the APCT and calculated the extent of concordance. These results were compared with the extent of concordance between the conventional Krimsky test and the APCT.
For analysis of the reliability of distance Krimsky test, two observers (KSJ and KH) measured the same patient with the distance Krimsky test, and inter-observer agreements were analyzed. Intra-observer agreements were analyzed by having the same observer repeat the measurement. Intra- and inter-observer agreements for the conventional Krimsky test and the APCT were analyzed in the same manner to compare each of the three tests.
To minimize bias, each observer tested on the same day without any information of the horizontal strabismic angles that were measured by each method. To correct the angle kappa, we presumed that angle kappa of both eyes to be the same and measured the deviation angles when the position of corneal reflection in the non-fixating eye was the same as that in the fixating eye instead of the accurate corneal center.
We used a 22-piece loose prism set in which prisms of more than 20 PD were divided by an interval of 5 PD. For this reason, when we could not measure the correct angle with a single prism such as 23 or 32 PD, we measured by placing another prism on the fixating eye and non-fixating eye simultaneously, and the total deviation angle was computed using a conversion table [8].
The Mann-Whitey U-test in SPSS ver. 16 (SPSS Inc., Chicago, IL, USA) was used for statistical analysis. A p-value <0.001 was considered to be statistically significant. Correlation between each test was examined through the Pearson correlation coefficient by means of a simple linear regression analysis. Standard deviation, coefficient of variation, and intraclass correlation coefficient were computed and compared in order to assess the intra-observer agreement. Bland and Altman plots were used for analysis for the evaluation of inter-observer agreement.
Results
Sixteen males and 24 females were included in this study. The average ages of the patients with exotropia and esotropia were 20.7 ± 12.4 years and 18.3 ± 8.7 years, respectively (Table 1). Patients' refractive errors ranged from +3.50 to -8.00 Dsph. Angles of exodeviation and esodeviation ranged from a minimum of 10 PD to a maximum of 40 PD under the APCT with an average of 22.5 ± 10.2 and 19.4 ± 6.7 PD, respectively. Among these, a total of 6 patients had vertical strabismus, and the average vertical strabismus in these patients was 2.2 ± 1.2 PD, which fell well within 5 PD.
Table 1.
Demographic characteristics of the study groups
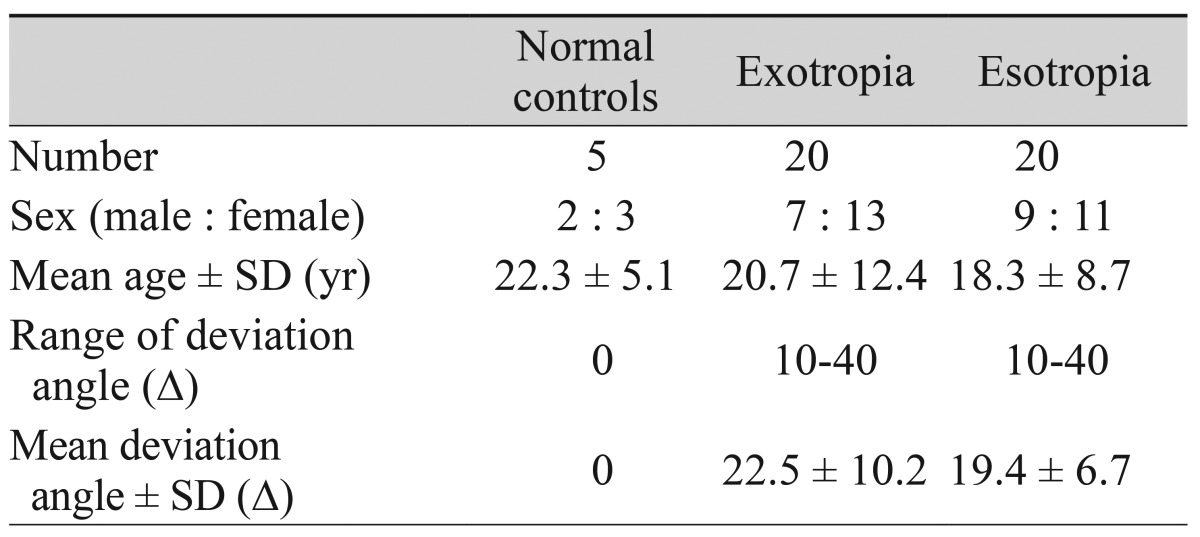
SD = standard deviation; Δ = prism diopters.
The intraclass correlation coefficients of exotropia / esotropia were 0.92 / 0.95 in the conventional Krimsky test, 0.91 / 0.90 in the distance Krimsky test, and 0.97 / 0.98 in the APCT, illustrating that the intra-observer agreement of the APCT was the highest and the agreements were also high for both the distance Krimsky test and the conventional Krimsky test (Table 2). The intra-observer agreements of each test were statistically significant (p < 0.001 for all).
Table 2.
The intra-observer agreements and their significance of the conventional Krimsky test, APCT, and distance Krimsky test
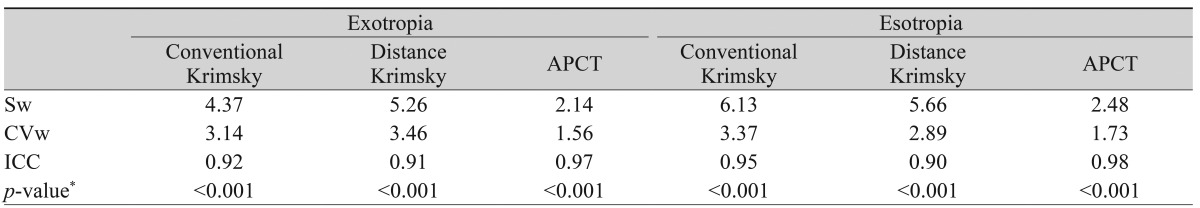
APCT = alternate prism cover test; Sw = within-subject standard deviation; CVw = coefficient of variation; ICC = intraclass correlation coefficient.
*Comparison of within-subject variances between each method.
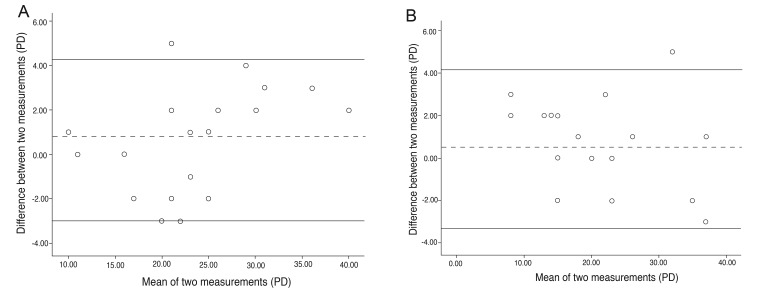
In the Bland & Altman table, the 95% limits of agreement between the two measurements by different observers using the distance Krimsky test were ±4.5 PD for exotropia, and ±5.6 PD for esotropia. Differences between the two measurements were included in the standard deviation of ±1.96. The mean differences were near zero in each exotropia and esotropia, illustrating significant inter-observer agreement (Fig. 1).
Fig. 1.
Inter-observer reproducibility of the distance Krimsky test in exotropia (A) and esotropia (B). The mean angle of deviation and the difference of the measurements of two observers are showed using the Bland and Altman method. The bias between the two measurements was assessed statistically as the mean of the differences compared to zero. The 95% limits of agreement between the two measurements were ±4.5 prism diopters (PD) for exotropia, and ±5.6 PD for esotropia. Differences between the two measurements were included in the standard deviation of ±1.96, and the mean differences are near zero for each exotropia and esotropia, illustrating good inter-observer agreement.
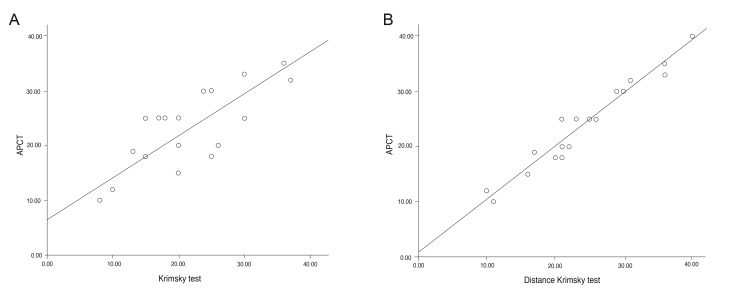
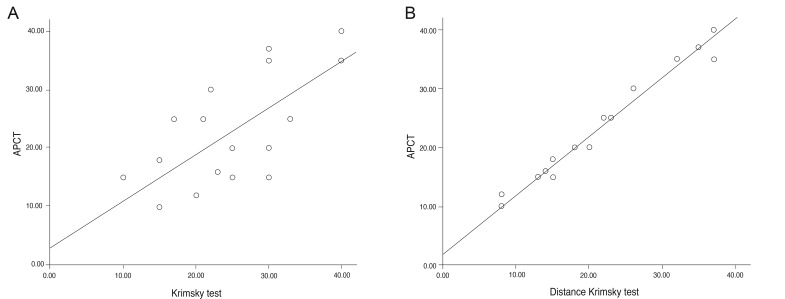
The Pearson correlation coefficient for examining the correlation between the strabismic angles measured by each of the methods demonstrated the correlation between the APCT and the distance Krimsky test to be highest for both exotropia and esotropia (p < 0.001) (Table 3). The Pearson correlation coefficient displayed the slope of the linear regression analysis graph that illustrates the correlation between each test. In the case of exotropia, the correlation between the conventional Krimsky test and the APCT at distance was close to Y = 0.738X (X, PD measured with the conventional Krimsky test; Y, PD measured with the APCT); in the case of esotropia, it was close to Y = 0.651X. The correlation coefficients between the distance Krimsky test and the APCT were 0.981 and 0.919 for exotropia and esotropia, respectively, illustrating that the extent of concordance between the distance Krimsky test and the APCT was higher than the concordance between the conventional Krimsky test and the APCT (Figs. 2 and 3).
Table 3.
The extent of concordance between three methods for measurement of the strabismic angle
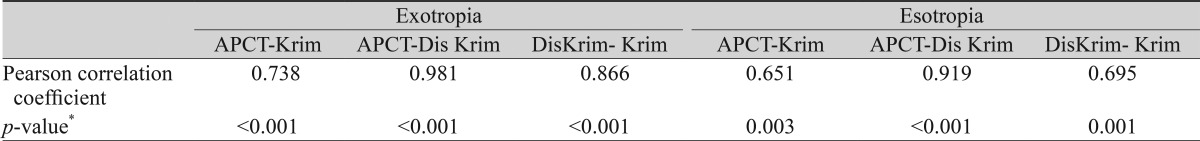
APCT = alternate prism cover test; Krim = conventional Krimsky test; DisKrim = distance Krimsky test.
*Pearson's correlation coefficient between each exam.
Fig. 2.
Correlation between the corneal reflection test and the alternate prism cover test (APCT) at distance for the strabismic angle in exotropia. (A) The correlation between the conventional Krimsky test and the APCT was close to Y = 0.738X (X, prism diopter measured with the conventional Krimsky test; Y, prism diopter measured with the APCT). (B) The correlation of the distance Krimsky test and the APCT was found to be Y = 0.981X (X, prism diopter measured with the distance Krimsky test; Y, prism diopter measured with the APCT). The extent of the concordance between the distance Krimsky test and the APCT was higher than that of the conventional Krimsky test and the APCT in exotropia.
Fig. 3.
The correlation between the corneal reflection test and the alternate prism cover test (APCT) at distance for the strabismic angle in esotropia. (A) The correlation between the conventional Krimsky test and the APCT was Y = 0.651X (X, prism diopter measured with the conventional Krimsky test; Y, prism diopter measured with the APCT). (B) The correlation of the distance Krimsky test and the APCT was found to be Y = 0.919X (X, prism diopter measured with the distance Krimsky test; Y, prism diopter measured with the APCT). This illustrates the extent of concordance between the distance Krimsky test and the APCT; it was higher than the concordance between the conventional Krimsky test and the APCT in esotropia.
Discussion
For the accurate evaluation and surgery of strabismus, both near and distance angles of deviation need to be taken. The conventional Krimsky test is conducted for patients who are unable to cooperate, have sensory strabismus, or have vision worse than 20 / 400. This test is mainly used to measure the angle of deviation at a near fixation point. Until now, there have been no reports about measuring the distance deviation using corneal reflection.
The main reason for errors when measuring the strabismic angle by means of the APCT is poor control of accommodation, particularly in cases of near range measurements [9]. The conventional Krimsky test can also induce changes in the strabismic angle due to accommodative or non-accommodative convergence due to near range measuring [1]. Even for sensory strabismus, non-accommodative convergence such as proximal convergence can occur. Accordingly, the conventional Krimsky test has the possibility of errors in measuring strabismic angles using near point fixation, which can induce accommodation and convergence of the eyes. In cases with differences between the near and distance strabismic angles, serious errors may occur if the surgical procedures are carried out only on the basis of the results of the conventional Krimsky test.
In this study, the extent of the concordance between the distance Krimsky test and the APCT at distance was higher than that of the conventional Krimsky test and the APCT at distance showing that the distance Krimsky test can decrease accommodative error and be more accurate in measuring the distance angle of deviation than the conventional Krimsky test. Therefore, we have to consider not only the conventional Krimsky test but also the distance Krimsky test when using the corneal reflection method.
In the current study, we found that the extent of concordance between the distance Krimsky test and the APCT in exodeviation was higher than that in esodeviation. This may be due to the fact that esodeviations involve accommodation or convergence more frequently.
The method of measuring the deviation angle between the corneal reflection point and the central axis of the pupil through photographic imaging as a modification of the conventional Krimsky test has been used for quite some time. According to the thesis by Lee and Lee [2], if the strabismic angle is Y (PD) and the relative ratio of the right eye to the left eye about difference (mm) between the corneal reflection point and central axis of pupil in each eye is X (%), the correlation is Y = 1.67X - 14.3 (R2 = 0.94, p = 0.006) when corneal reflections and photograph are used, along with illustration of good correlation. Although statistical accuracy can be increased through such a measurement, it has limitations in that it would generate additional costs due to the need for a special computational program and devices depending on the situation and it takes a long time. In addition, fixation at the near range rather than at distance has been used in the majority of previous studies using photographic imaging [2,10]. The distance Krimsky test in our study is a useful test with a high level of reproducibility and accuracy as well as with a high extent of concordance to the APCT. It can also be easily performed on an outpatient basis without the need for additional devices or techniques.
There are several considerations when measuring the strabismic angle with either the distance Krimsky test or the conventional Krimsky test. Firstly, when the corneal reflection is outside the center, causes other than strabismus must be considered. One such cause is a large angle kappa. In general, the average angle kappa is up to 5° in the random population [1]. If there is large positive angle kappa, a small quantity of esodeviation may be overlooked, and orthophoria or esotropia may be misdiagnosed with exotropia (pseudoexotropia). In addition, if there is large negative angle kappa, exodeviation may be overlooked, and orthoporia or exotropia may be misdiagnosed with esotropia (pseudoesotropia). In this study, under the presumption that the angle kappa of both eyes was the same, the angle kappa was compensated in a way that measuring the angle of deviation when the position of the corneal reflection in the non-fixating eye was the same as that in the fixating eye, instead of the correct center of the cornea.
Secondly, the distance Krimsky test and the conventional Krimsky test should be used sparingly in cases of ectopic macula or eccentric fixation in amblyopia. According to reports, approximately 44% of strabismic amblyopia patients perform eccentric fixation [11]. If we perform surgery with the strabismic angle measured with the distance Krimsky test without considering eccentric fixation or ectopic macula, some patients may suffer postoperative problems such as visual discomfort, abnormal head posture, or increase in the strabismic angle.
Limitations of this study include the small number of subjects and the possibility of different results in measurements in accordance with the proficiency of the examiners. However, in consideration of the fact that the same problems also exist for the APCT, the difference between the results of the examiners can be overcome through enhancement of proficiency of the examiners. For this purpose, it is necessary to establish individualized normative data for each of the examiners for the distance Krimsky test along with improvements in repetitive proficiency and accumulation of more data on the distance Krimsky test.
In conclusion, the distance Krimsky test has a high level of intra- and inter-observer agreement and displays significant correlation with the APCT at distance. It is expected to be more useful than the conventional Krimsky test for measuring the distance angle of deviation in infants or low vision patients who are difficult to measure with the APCT. Through improvement in the proficiency of the examiners and establishment of individualized normative data, the distance Krimsky test can be useful for the accurate evaluation of strabismus.
Footnotes
No potential conflict of interest relevant to this article was reported.
References
- 1.Von Noorden GK, Campos EC. Examination of patient-II: motor signs in heterophoria and heterotropia. In: Von Noorden GK, Campos EC, editors. Binocular vision and ocular motility: theory and management of strabismus. 6th ed. St. Louis: Mosby; 2002. pp. 85–100.pp. 168–210. [Google Scholar]
- 2.Lee JA, Lee HY. New method for measurement of strabismic angle using corneal reflex and photograph. J Korean Ophthalmol Soc. 2002;43:1988–1992. [Google Scholar]
- 3.Choi RY, Kushner BJ. The accuracy of experienced strabismologists using the Hirschberg and Krimsky tests. Ophthalmology. 1998;105:1301–1306. doi: 10.1016/S0161-6420(98)97037-3. [DOI] [PubMed] [Google Scholar]
- 4.Cho YA, Roh KH. Early surgery for infantile esotropia. J Korean Ophthalmol Soc. 1993;34:1251–1256. [Google Scholar]
- 5.Parks MM. Symposium: infantile esotropia: summary and conclusions. Am Orthopt J. 1968;18:19–22. [PubMed] [Google Scholar]
- 6.Ing MR. Early surgical alignment for congenital esotropia. Ophthalmology. 1983;90:132–135. doi: 10.1016/s0161-6420(83)34586-3. [DOI] [PubMed] [Google Scholar]
- 7.Zak TA, Morin JD. Early surgery for infantile esotropia: results and influence of age upon results. Can J Ophthalmol. 1982;17:213–218. [PubMed] [Google Scholar]
- 8.Thompson JT, Guyton DL. Ophthalmic prisms: measurement errors and how to minimize them. Ophthalmology. 1983;90:204–210. doi: 10.1016/s0161-6420(83)34572-3. [DOI] [PubMed] [Google Scholar]
- 9.Wright KW. The ocular motor examination. In: Wright KW, Spiegel PH, editors. Pediatric ophthalmology and strabismus. 2nd ed. New York: Springer; 2003. pp. 189–203. [Google Scholar]
- 10.Yang HK, Han SB, Hwang JM, et al. Assessment of binocular alignment using the three-dimensional Strabismus Photo Analyzer. Br J Ophthalmol. 2012;96:78–82. doi: 10.1136/bjophthalmol-2011-300305. [DOI] [PubMed] [Google Scholar]
- 11.Von Noorden GK, Helveston EM. Decentered corneal light reflex. In: Von Noorden GK, Helveston EM, editors. Strabismus: a decision making approach. St. Louis: Mosby; 1994. pp. 26–27. [Google Scholar]