Abstract
Objective
The purpose of this report is to describe the management of a patient with advanced trapeziometacarpal (TMC) osteoarthritis (OA) using mobilization with movement technique in combination with kinesiology tape to decrease pain and improve range of motion.
Clinical Features
A 52-year-old female seamstress (a career of 35 years’ duration) presented to a physiotherapy clinic with pain in the dorsal aspect of the thumb carpometacarpal region of the right (dominant) hand. Examination revealed reduced ability to abduct the right thumb, significant loss of web space, weakness of pinch grip, and deterioration of hand function. Radiographs demonstrated OA of the TMC stage IV according to the Eaton-Littler-Burton classification, with instability and subluxation of the joint.
Intervention and Outcome
A combined treatment protocol of mobilization with movement and kinesiology tape at the TMC joint for 12 weekly sessions was performed. Outcome measures were assessed at baseline, immediately upon completion of treatment, and at 2-month follow-up and included numeric pain rating scale, range of motion, pressure pain threshold, and tip pinch strength at the TMC joint. Treatment interventions were applied for 12 sessions over a period of 2 months. Outcome measures indicated significant reduction of the patient’s subjective pain reports and considerable improvement in functional and occupational tasks. A follow-up visit at 4 months (2 months after last treatment) showed that the improvement was maintained.
Conclusion
A combined program of mobilization with movement and kinesiology tape reduced pain, increased range of motion, and increased tip pinch strength in a patient with severe functional impairment related to dominant TMC OA.
Key indexing terms: Thumb, Osteoarthritis, Manual therapy, Hand strength
Introduction
Trapeziometacarpal osteoarthritis (TMC OA) is a degenerative alteration of the thumb carpometacarpal joint, characterized by progressive deterioration of joint surfaces and newly forming bone, presenting as pain at the base of the thumb and dysfunction.1 In Europe and the United States, the prevalence of TMC OA has been reported as high as 30% to 40% of postmenopausal women and between 8% and 12% in the general population.2-4 Trapeziometacarpal OA frequently induces pain at the base of the thumb and often progressive closure of the first web, which in turn causes an alteration of the thumb-index pinch and limitation in hand function.5
Evidence-based recommendations of TMC OA include activity modifications, rest, nonsteroidal anti-inflammatory drugs, and thenar intrinsic and extrinsic muscle strengthening exercises.6 Nonpharmacological manual interventions have only recently begun to be specifically researched in advanced-stage TMC OA: recent studies investigating hypoalgesic mechanical effects of manual therapies in TMC OA have focused on different passive mobilization techniques (ie, median nerve mobilization by sliding technique7) and passive and accessory joint mobilizations.8-10 A randomized controlled trial analyzing changes in pressure sensitivity after treatment with Kaltenborn mobilization9 or radial nerve mobilization1 in patients with TMC OA reported that unilateral mobilization applied on the symptomatic hand increased pressure pain thresholds over the TMC joint immediately and at follow-up periods.9 Typically, in clinical situations, manual therapy interventions combine several treatment strategies for TMC OA; however, to our knowledge, the benefits of kinesiology taping and Mobilization With Movement (MWM)11 have not yet been studied in patients with TMC OA. Because patients often report significant pain relief and functional improvements from these techniques in other conditions,12 it was decided to investigate this approach in a patient who was not responsive to conventional therapy for TMC OA.
It is hypothesized that positional faults of joints can occur following injuries or because of physiological changes secondary to degenerative conditions.13 Mobilization With Movement is a manual force technique applied to promote restoration of normal joint alignment and arthrokinematics, rather than the stretching of tightened tissues.13 The technique includes sustained manual correction of subtle joint malalignment, with active movement immediately superimposed on the corrected joint position.12 The active movement chosen is one that previously produced pain but, when superimposed on improved joint alignment, occurs pain-free.14 It has been suggested that MWM can help with immediate pain relief and improve function.15 Kinesiology taping is the application of thin, elastic tape to painful structures, with the goal of reducing pain, improving joint alignment, and improving proprioception.16 The proposed benefits of taping may occur because of the increased circulation created by increasing the interstitial space between skin and underlying connective tissues, thereby improving venous and lymphatic flow, and by stimulation of cutaneous mechanoreceptors, reducing pain.16
At present, there are no published case reports that describe the management of TMC OA using MWM and kinesiology taping. Therefore, the purpose of this report is to describe the management of a patient with advanced TMC OA using MWM technique in combination with kinesiology tape to decrease pain and improve range of movement.
Case report
Background
A 52-year-old female seamstress was referred to the physical therapy clinic for treatment because of increasing pain and functional limitations in her right (dominant) hand. She presented with a 14-year history of insidious and increasing pain, with progressive lack of grip and pinch strength in her right hand. A diagnosis of right hand stage IV TMC OA, with instability and dorsal subluxation of the joint (Eaton-Littler-Burton classification17), was confirmed by radiograph and physical examination18,19 (Fig. 1).
Fig. 1.

Stage IV TMC OA of the right hand.
Health history
At the time of assessment, the patient was not taking medications and had no other reported medical conditions. Before initiation of treatment, the patient had been experiencing a rapid progression of her right hand symptoms. She had consulted with her general medical practitioner 8 months previously, who confirmed the diagnosis of TMC OA. He prescribed a course of oral nonsteroidal anti-inflammatory medication in combination with a short-arm thumb orthotic, immobilizing the wrist in neutral and the painful thumb in abduction. In addition, the general medical practitioner had advised work modification, including stopping work for 1 week, and a trial of 6 sessions of physical therapy (laser and ultrasonographic therapy). The patient reported no benefit from this medical or physical therapy management and had discontinued treatment 6 weeks before presentation at our facility.
Pain was located along the dorsal aspect of the TMC joint and was described as a “constant achy feeling,” with occasional “sharp” pain with specific movements, particularly thumb abduction and flexion, and graded at 7 of 10 on a numeric pain scale (NPS).
The patient’s subjective reports indicated increased severity of symptoms associated with her occupational tasks, particularly cutting with scissors, such that she was experiencing difficulty performing her occupational tasks. Acetaminophen and rest provided little relief, whereas repetitive use (eg, gripping) aggravated the pain. She reported that pinching (between the thumb and her first finger), cutting with scissors, turning door keys, writing, and holding cutlery utensils all aggravated her pain, with difficulty lifting even small amounts of weight with the affected hand. Because of her recent exacerbation of pain, she was no longer able to maintain her occupational tasks as a seamstress.
Physical examination
The patient held the right first metacarpal in adduction and flexion, with a zig-zag collapse deformity, commonly seen in advanced stages of TMC OA20,21: The right first dorsal interosseus muscle and thenar musculature showed evidence of atrophy compared with the left hand. The first metacarpal base was prominent dorsally.
Neck, shoulder, and elbow range of motion (ROM) was within normal limits bilaterally.
Pretreatment goniometric evaluation of the right hand indicated reduced active and passive ROM of the TMC joint in both palmar and radial abduction of the right thumb, that is, 35° and 42°, respectively (compared with 57° and 58° on the asymptomatic left thumb), with painful active and resisted opposition, adduction, and flexion.
The patient reported tenderness to palpation of the right TMC and scapholunate joints, with maximal tenderness located on the TMC joint line dorsally. The result of the right TMC axial compression test for OA (grind test) was positive.22
The right (dominant) TMC joint was noted by a radiologist to have grade IV OA according to the Eaton-Littler classification.17 Asymptomatic TMC OA was also noted in the same joint on the left (nondominant) hand.
Results of laboratory blood tests were unremarkable for metabolic, inflammatory, or infectious joint disease. Results of both Durkin and Tinel tests for carpal tunnel were negative,23 and result of Finkelstein test for tenosynovitis of the first dorsal compartment was negative bilaterally.24 A confirmation of a diagnosis of TMC OA stage IV complicated by TMC joint laxity was noted.
Treatment interventions
Before initiation of treatment, the patient was advised about the potential benefits of physiotherapy treatment as well as its potential adverse effects; and written informed consent for treatment was obtained. During the 12 intervention sessions over the course of 2 months, the patient received MWM techniques to promote pain-free thumb mobility13; and Kinesiology tape was applied immediately posttreatment and worn for 5 days to assist with joint repositioning posttreatment.25
The primary treatment interventions are outlined in detail below.
Method of application of MWM13
At initial assessment, active motions (TMC radial and palmar abduction and adduction) of the thumb were limited by pain. To find the position that best allowed for pain-free motion, an iterative process was used. The therapist had to experiment with and fine-tune the direction and pressure of the imposed carpal glide using feedback from the patient. As the first metacarpal was positioned toward neutral, reducing the subluxation using manual gliding pressure, the patient’s ability to move into previously painful ranges with pain-free ranges was noted. When the proper position, direction, and force of the thumb mobilization were established, the patient performed 3 sets of 10 repetitions of each of the previously painful thumb motions: TMC radial and palmar abduction and adduction (Fig. 2).
Fig. 2.
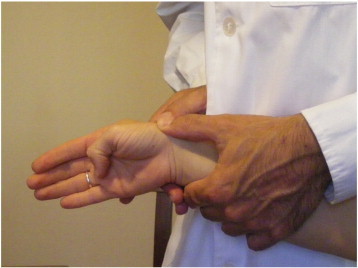
Mobilization with movement. Active thumb motion performed with reduction of the TMC joint.
Kinesiology tape
The Kinesiology tape was placed without tension for a relaxation effect25 (Fig. 3). The goals of application of tape were also to facilitate proprioceptive feedback to the involved joint,26 to assist with circulation, and to diminish nociceptive input to the nervous system to prolong the effects of manual interventions.16
Fig. 3.
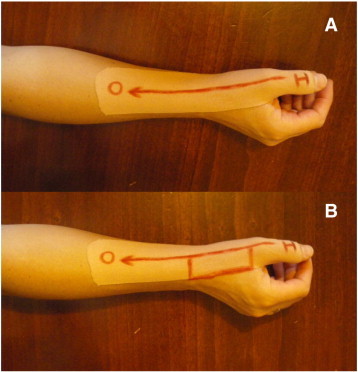
Kinesiology tape for TMC joint (tendons). Tape is placed without tension for a relaxation effect from the insertion (I) to the origin (O). Without (A) and with (B) a corrective strip over the snuff box and parallel to tendons.
Outcome measures
Outcome measures were performed at baseline, at the conclusion of treatment, and again at 2-month follow-up.
The primary outcome measure was pain intensity of first TMC joint, which was assessed with the NPS. The NPS is a 10-cm line anchored with a numeric “0” at one end representing no pain and “10” at the other end representing the worst pain imaginable, and sequential numbers in between.27 Pain was assessed as the participant performed tip pinch between the thumb and the index finger. The NPS was selected as the primary outcome measure based on the ability to detect minimally important clinically important differences, noted to be 2.0 cm in this instrument.28 The Hospital Anxiety and Depression Scale (HADS) was used to capture psychosocial adjustment.29,30 Goniometric evaluations of the thumb were taken according to the American Society of Surgery of the Hand guidelines.31 To avoid measurement error, the same examiner performed all ROM measurements. Pressure pain threshold (PPT) was evaluated: this is a quantitative sensory test of tissue sensitivity and is defined as the minimal amount of pressure that produces pain, measured via a pressure algometer.32 Measurements were performed with a Mechanical Pressure Algometer (Wagner Instruments, Greenwich, CT). The validity and reproducibility of algometry have been described, with higher PPT indicating lower pain sensitivity.33 The patient was instructed to indicate as soon as the sensation changed from pressure to pain, according to established protocols for measuring algometry.34 The PPT was measured contralaterally over the TMC joint at the anatomical snuffbox. The pressure applied was increased by approximately 0.1 kg/cm2 each second until the onset of pain. Three measurements were obtained from each point, and the mean was used for statistical analysis. A 1-min rest period was allowed between each measurement. The PPT was measured in kilograms per square centimeter at baseline, immediately after treatment, and 2 months after the treatment period. Motor performance was assessed by analyzing tip pinch strength measured by mechanical pinch gauge (Baseline, Irvington, NY) in the sitting position with the shoulder adducted and neutrally rotated and the elbow flexed at 90°.9,35 The reliability of pinch strength has been found to be high (intraclass correlation coefficient = 0.93).36 The treatment produced clinically significant improvements in pain and function. The NPS decreased by 3 points during the treatment, a clinically significant effect,37 which was maintained at 2-month follow-up.
Goniometric measurements are listed in Table 1. The ROM measures also improved: at commencement of treatment, first carpometacarpal palmar abduction/radial abduction TMC joint ROM measured 35° and 42°, respectively. Immediately upon completion of treatment (2 months), ROM of the affected joint measured 47° palmar abduction and 50° radial abduction, maintained at follow-up at 2 months in 50° and 50° palmar and radial abduction, an improvement of 42.9%/19.1%, respectively. The PPT increased from 2.18 to 3.75 kg/cm2 at the completion of treatment, which was maintained at 2-month follow-up, with PPT levels measured at 3.9 kg/cm2, an improvement of 78.9%.
Table 1.
Outcome measures
| Pretreatment Left |
Pretreatment Right |
Posttreatment Right, 2 mo after initial presentation, 12 visits |
Follow-up, 4 mo after initial presentation Right |
|
|---|---|---|---|---|
| HADS | ||||
| AS | 2 | 2 | 1 | |
| DS | 2 | 2 | 1 | |
| NPS | ||||
| 1 | 7 | 3 | 3 | |
| ROM (°) | ||||
| 1st TMC palmar abduction | 57 | 35 | 47 | 50 |
| 1st TMC radial abduction | 58 | 42 | 50 | 50 |
| PPT (kg/cm2) | ||||
| TMC joint | 4.45 | 2.18 | 3.75 | 3.9 |
| Pinch strength (kg) | ||||
| Tip pinch | 3.7 | 2.14 | 2.5 | 2.63 |
AS, anxiety; DS, depression; HADS, hospital anxiety and depression scale; NPS, numeric pain rating scale; PPT, pressure pain threshold; ROM, range of motion; TMC, Trapeziometacarpal.
Tip pinch strength increased by 2.5 kg and was maintained until first follow-up, an improvement of 22.9%. Outcomes are summarized in Table 1.
A follow-up visit 2 months after treatment completion confirmed that the patient had improved. The NPS, ROM, PPT, and tip pinch improved 57.1%, 30%, 78.9%, and 22.9%, respectively. The HADS scores for anxiety and depression were maintained at 1 and 1, respectively, at 2-month follow-up. The patient maintained full treatment compliance throughout the course of the study, with no reported adverse effects.
Discussion
This patient presented with TMC OA stage IV17 complicated by TMC joint laxity and a radiological positional abnormality, a clinical presentation commonly seen in OA of the TMC joint.38 Following 12 treatments of MWM over a period of 8 weeks, the involved TMC joint pain severity, ROM, and function improved in this patient despite the long-standing mechanical structural change and chronicity of pain. Mobilization With Movement as a manual therapy technique has been described in managing pain reduction and improved function in a number of preliminary studies and case reports for both traumatic and nontraumatic joint disorders.14,39-44
The technique involves a comprehensive physical examination of the patient’s active, resistive, passive, and accessory movements at the involved joint, as well as isolated overpressure tests to determine the appropriate manual mobilization direction.44 This iterative process is important to establish the appropriate therapeutic accessory movement to use for maximum pain relief and improved ROM, following which 3 sets of 10 mobilizations are typically performed symptom-free, with support from kinesiology tape often applied following treatment to sustain the joint repositioning.44
The mechanism by which MWM is able to rapidly reduce pain remains speculative; however, several theories exist.12 It has been surmised that manual correction of a positional fault can give rise to hypoalgesia by changing the mechanics of the joint and reducing the dysfunction.44 However, an interesting study by Hsieh et al (2002),15 in a case of thumb trauma, has illustrated that the positional fault theory, although perhaps initially responsible for the immediate marked hypoalgesic effect, may not be entirely responsible for sustained pain relief. These authors identified in their case study via magnetic resonance imaging that the patient’s thumb metacarpal identified positional fault initially had an immediate improvement in bony alignment following application of MWM, but the original fault had reoccurred at follow-up despite the patient remaining asymptomatic. This finding led the authors to conclude that MWM may produce its beneficial effects via stimulating alternative antinociceptive and motor mechanisms, rather than solely due to long-term correction of the mechanical positional fault alone.15 Mulligan’s11 MWM technique may be particularly applicable to patients with TMC OA because of the pathological processes in OA that lead to changes in the shape of articular surfaces at this joint, which are amenable to manual correction to induce pain-free movement. Other mechanisms, including hypoalgesic effects, may be involved in the pain relief process.45
The role of kinesiology tape in the management of musculoskeletal disorders has been described in a recent meta-analysis.16 Proposed mechanisms of pain relief from application of kinesiology tape include improvement in circulation of both venous and lymphatic fluid by increasing the interstitial space between the skin and underlying tissues, improving joint and muscle alignment, and reducing subcutaneous nociceptive input to the central nervous system.16 Interestingly, a recent study has also determined that the application of kinesiology tape to the forearm muscles significantly improves grip strength in healthy participants46; however, improvements in strength for individuals with OA have not been determined. We anticipate that the improvements in tip pinch muscle strength in our study may be due to a combination of factors.
The notion that manual therapy interventions can beneficially influence the central nervous system for pain control is becoming increasingly recognized,47 perhaps by reducing spinal segmental sensitivity47,48 or by enhancing endogenous cortical descending pain-relieving pathways.49 The exact mechanisms of pain relief afforded by MWM and the application of kinesiology tape, however, remain hypothetical and may be interesting topics for exploration in subsequent clinical trials.
Limitations
As in all case studies, limitations exist: this case report would have been enhanced by additional outcome measures such as the inclusion of a standardized self-reported functional outcome measure, such as the Disabilities of the Arm, Shoulder, and Hand50; and it is our intention to include functional outcomes in further randomized controlled trials. Considering the nature of this study, a cause-effect relationship cannot be established, thus limiting the generalizability of findings. There is also a paucity of literature showing the effectiveness of MWM and kinesiology tape in the treatment of hand OA; thus, our treatment approach is novel. Although this patient showed relief from pain and improved ROM and tip pinch strength, we cannot generalize the beneficial effects of this case; nor can it be implied that the patient would not have improved following the normal course of the disorder. As is customary in physical therapy, several interventions were applied during the same treatment session, making it more difficult to ascertain the “active ingredients”51 of the intervention. These considerations will generate hypotheses for future trials.
The techniques used in this case study may require additional training for competent application but are worthwhile adjuncts for clinical practice12 and may enhance the clinical approach to hand OA. The exact mechanisms of pain relief remain theoretical, but it is hypothesized that they may be due to a combination of improved mechanics combined with a change in the processing of pain in the central nervous system.11,12 The results of this case report are promising and justify further clinical controlled studies to confirm the current results and investigate further the mechanisms of pain reduction.
Conclusion
The current case report demonstrated that MWM and Kinesiology tape induced hypoalgesia and improved ROM and tip pinch strength in a patient with stage IV right TMC OA. Clinical improvements in functional and occupational demands demonstrate the potential clinical utility of this treatment protocol for chronic pain and restriction of TMC ROM due to long-standing OA.
Funding sources and potential conflicts of interest
No funding sources or conflicts of interest were reported for this study.
Contributor Information
Jorge Hugo Villafañe, Email: mail@villafane.it.
Dolores Langford, Email: doloreslangford93@gmail.com.
Isabel Maria Alguacil-Diego, Email: Isabel.alguacil@urjc.es.
Josué Fernández-Carnero, Email: josuefernandezcarnero@gmail.com.
References
- 1.Villafane J.H., Silva G.B., Bishop M.D., Fernandez-Carnero J. Radial nerve mobilization decreases pain sensitivity and improves motor performance in patients with thumb carpometacarpal osteoarthritis: a randomized controlled trial. Arch Phys Med Rehabil. 2012;93(3):396–403. doi: 10.1016/j.apmr.2011.08.045. [DOI] [PubMed] [Google Scholar]
- 2.Pellegrini V.D., Jr. Osteoarthritis of the trapeziometacarpal joint: the pathophysiology of articular cartilage degeneration I. Anatomy and pathology of the aging joint. J Hand Surg Am. 1991;16(6):967–974. doi: 10.1016/s0363-5023(10)80054-1. [DOI] [PubMed] [Google Scholar]
- 3.Weilby A. Tendon interposition arthroplasty of the first carpo-metacarpal joint. J Hand Surg Br. 1988;13(4):421–425. doi: 10.1016/0266-7681_88_90171-4. [DOI] [PubMed] [Google Scholar]
- 4.Haara M.M., Heliovaara M., Kroger H. Osteoarthritis in the carpometacarpal joint of the thumb. Prevalence and associations with disability and mortality. J Bone Joint Surg Am. 2004;86-A(7):1452–1457. doi: 10.2106/00004623-200407000-00013. [DOI] [PubMed] [Google Scholar]
- 5.Poole J.U., Pellegrini V.D., Jr. Arthritis of the thumb basal joint complex. J Hand Ther. 2000;13(2):91–107. doi: 10.1016/s0894-1130(00)80034-4. [DOI] [PubMed] [Google Scholar]
- 6.Hochberg M.C., Altman R.D., April K.T. American College of Rheumatology 2012 recommendations for the use of nonpharmacologic and pharmacologic therapies in osteoarthritis of the hand, hip, and knee. Arthritis Care Res. 2012;64(4):465–474. doi: 10.1002/acr.21596. [DOI] [PubMed] [Google Scholar]
- 7.Villafane J.H., Silva G.B., Fernandez-Carnero J. Short-term effects of neurodynamic mobilization in 15 patients with secondary thumb carpometacarpal osteoarthritis. J Manipulative Physiol Ther. 2011;34(7):449–456. doi: 10.1016/j.jmpt.2011.05.016. [DOI] [PubMed] [Google Scholar]
- 8.Villafañe J.H., Silva G.B., Chiarotto A. Passive joint mobilization of arm joints on secondary carpometacarpal osteoarthritis. Increased strength and reduced pain: a case series. J Manipulative Physiol Ther. 2012;35:735–742. doi: 10.1016/j.jmpt.2012.10.012. [DOI] [PubMed] [Google Scholar]
- 9.Villafane J.H., Silva G.B., Diaz-Parreno S.A., Fernandez-Carnero J. Hypoalgesic and motor effects of kaltenborn mobilization on elderly patients with secondary thumb carpometacarpal osteoarthritis: a randomized controlled trial. J Manipulative Physiol Ther. 2011;34(8):547–556. doi: 10.1016/j.jmpt.2011.08.005. [DOI] [PubMed] [Google Scholar]
- 10.Villafane J.H., Silva G.B., Fernandez-Carnero J. Effect of thumb joint mobilization on pressure pain threshold in elderly patients with thumb carpometacarpal osteoarthritis. J Manipulative Physiol Ther. 2012;35(2):110–120. doi: 10.1016/j.jmpt.2011.12.002. [DOI] [PubMed] [Google Scholar]
- 11.Mulligan. Manual therapy, NAGS, SNAGS, MWMs. 4th ed. Wellington New Zealand 1999.
- 12.Vicenzino B., Paungmali A., Teys P. Mulligan's mobilization-with-movement, positional faults and pain relief: current concepts from a critical review of literature. Man Ther. 2007;12(2):98–108. doi: 10.1016/j.math.2006.07.012. [DOI] [PubMed] [Google Scholar]
- 13.Backstrom K.M. Mobilization with movement as an adjunct intervention in a patient with complicated de Quervain's tenosynovitis: a case report. J Orthop Sports Phys Ther. 2002;32(3):86–94. doi: 10.2519/jospt.2002.32.3.86. [discussion 94–87] [DOI] [PubMed] [Google Scholar]
- 14.Exelby L. Peripheral mobilisations with movement. Man Ther. 1996;1(3):118–126. doi: 10.1054/math.1996.0259. [DOI] [PubMed] [Google Scholar]
- 15.Hsieh C.Y., Vicenzino B., Yang C.H., Hu M.H., Yang C. Mulligan's mobilization with movement for the thumb: a single case report using magnetic resonance imaging to evaluate the positional fault hypothesis. Man Ther. 2002;7(1):44–49. doi: 10.1054/math.2001.0434. [DOI] [PubMed] [Google Scholar]
- 16.Williams S., Whatman C., Hume P.A., Sheerin K. Kinesio taping in treatment and prevention of sports injuries: a meta-analysis of the evidence for its effectiveness. Sports Med. 2012;42(2):153–164. doi: 10.2165/11594960-000000000-00000. [DOI] [PubMed] [Google Scholar]
- 17.Eaton R.G., Littler J.W. A study of the basal joint of the thumb. Treatment of its disabilities by fusion. J Bone Joint Surg Am. 1969;51(4):661–668. [PubMed] [Google Scholar]
- 18.Batra A., Kanvinde R. Osteoarthritis of the thumb trapeziometacarpal joint. Curr Orthop. 2007;21:135–144. [Google Scholar]
- 19.Jaggi R., Morris S. Practice tips. Rule of thumb: update on first carpometacarpal joint osteoarthritis. Can Fam Physician. 2007;53(8):1309–1310. [PMC free article] [PubMed] [Google Scholar]
- 20.Batra R.K. Osteoarthritis of the trapeziometacarpal joint. Curr Orthop. 2007;21:135–144. [Google Scholar]
- 21.Van Heest A.E., Kallemeier P. Thumb carpal metacarpal arthritis. J Am Acad Orthop Surg. 2008;16(3):140–151. doi: 10.5435/00124635-200803000-00005. [DOI] [PubMed] [Google Scholar]
- 22.Merritt M.M., Roddey T.S., Costello C., Olson S. Diagnostic value of clinical grind test for carpometacarpal osteoarthritis of the thumb. J Hand Ther. 2010;23(3):261–268. doi: 10.1016/j.jht.2010.02.001. [DOI] [PubMed] [Google Scholar]
- 23.Novak C.B., Mackinnon S.E., Brownlee R., Kelly L. Provocative sensory testing in carpal tunnel syndrome. J Hand Surg Br. 1992;17(2):204–208. doi: 10.1016/0266-7681(92)90090-o. [DOI] [PubMed] [Google Scholar]
- 24.Batteson R., Hammond A., Burke F., Sinha S. The de Quervain's screening tool: validity and reliability of a measure to support clinical diagnosis and management. Musculoskeletal Care. 2008;6(3):168–180. doi: 10.1002/msc.129. [DOI] [PubMed] [Google Scholar]
- 25.Howell E.R. Conservative care of De Quervain's tenosynovitis/ tendinopathy in a warehouse worker and recreational cyclist: a case report. J Can Chiropr Assoc. 2012;56(2):121–127. [PMC free article] [PubMed] [Google Scholar]
- 26.Chang H.Y., Chou K.Y., Lin J.J., Lin C.F., Wang C.H. Immediate effect of forearm Kinesio taping on maximal grip strength and force sense in healthy collegiate athletes. Phys Ther Sport. 2010;11(4):122–127. doi: 10.1016/j.ptsp.2010.06.007. [DOI] [PubMed] [Google Scholar]
- 27.Jensen M.P., Karoly P., Braver S. The measurement of clinical pain intensity: a comparison of six methods. Pain. 1986;27(1):117–126. doi: 10.1016/0304-3959(86)90228-9. [DOI] [PubMed] [Google Scholar]
- 28.Emshoff R., Bertram S., Emshoff I. Clinically important difference thresholds of the visual analog scale: a conceptual model for identifying meaningful intraindividual changes for pain intensity. Pain. 2011;152(10):2277–2282. doi: 10.1016/j.pain.2011.06.003. [DOI] [PubMed] [Google Scholar]
- 29.Mykletun A., Stordal E., Dahl A.A. Hospital Anxiety and Depression (HAD) Scale: factor structure, item analyses and internal consistency in a large population. Br J Psychiatry. 2001;179:540–544. doi: 10.1192/bjp.179.6.540. [DOI] [PubMed] [Google Scholar]
- 30.Snaith R.P. The Hospital Anxiety And Depression Scale. Health Qual Life Outcomes. 2003;1:29. doi: 10.1186/1477-7525-1-29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.ASfSot Hand. The hand: examination and diagnosis. 1990. New York: Churchill Livingstone. [Google Scholar]
- 32.Ylinen J. Pressure algometry. Aust J Physiother. 2007;53(3):207. doi: 10.1016/s0004-9514(07)70032-6. [DOI] [PubMed] [Google Scholar]
- 33.Fischer A.A. Pressure algometry over normal muscles. Standard values, validity and reproducibility of pressure threshold. Pain. 1987;30(1):115–126. doi: 10.1016/0304-3959(87)90089-3. [DOI] [PubMed] [Google Scholar]
- 34.Ylinen J., Nykanen M., Kautiainen H., Hakkinen A. Evaluation of repeatability of pressure algometry on the neck muscles for clinical use. Man Ther. 2007;12(2):192–197. doi: 10.1016/j.math.2006.06.010. [DOI] [PubMed] [Google Scholar]
- 35.Mathiowetz V., Weber K., Volland G., Kashman N. Reliability and validity of grip and pinch strength evaluations. J Hand Surg Am. 1984;9(2):222–226. doi: 10.1016/s0363-5023(84)80146-x. [DOI] [PubMed] [Google Scholar]
- 36.Schreuders T.A., Roebroeck M.E., Goumans J., van Nieuwenhuijzen J.F., Stijnen T.H., Stam H.J. Measurement error in grip and pinch force measurements in patients with hand injuries. Phys Ther Sep. 2003;83(9):806–815. [PubMed] [Google Scholar]
- 37.Salaffi F., Stancati A., Silvestri C.A., Ciapetti A., Grassi W. Minimal clinically important changes in chronic musculoskeletal pain intensity measured on a numerical rating scale. Eur J Pain. 2004;8(4):283–291. doi: 10.1016/j.ejpain.2003.09.004. [DOI] [PubMed] [Google Scholar]
- 38.Polatsch D.B., Paksima N. Basal joint arthritis: diagnosis and treatment. Bull NYU Hosp Jt Dis. 2006;64(3–4):178–184. [PubMed] [Google Scholar]
- 39.Vicenzino B., Wright A. Effects of a novel manipulative physiotherapy technique on tennis elbow: a single case study. Man Ther. 1995;1(1):30–35. doi: 10.1054/math.1995.0247. [DOI] [PubMed] [Google Scholar]
- 40.Wilson E. Central facilitation and remote effects: treating both ends of the system. Man Ther. 1997;2(3):165–168. doi: 10.1054/math.1997.0297. [DOI] [PubMed] [Google Scholar]
- 41.Kavanagh J. Is there a positional fault at the inferior tibiofibular joint in patients with acute or chronic ankle sprains compared to normals? Man Ther. 1999;4(1):19–24. doi: 10.1016/s1356-689x(99)80005-8. [DOI] [PubMed] [Google Scholar]
- 42.Vicenzino B., Paungmali A., Buratowski S., Wright A. Specific manipulative therapy treatment for chronic lateral epicondylalgia produces uniquely characteristic hypoalgesia. Man Ther. 2001;6(4):205–212. doi: 10.1054/math.2001.0411. [DOI] [PubMed] [Google Scholar]
- 43.Collins N., Teys P., Vicenzino B. The initial effects of a Mulligan's mobilization with movement technique on dorsiflexion and pain in subacute ankle sprains. Man Ther. 2004;9(2):77–82. doi: 10.1016/S1356-689X(03)00101-2. [DOI] [PubMed] [Google Scholar]
- 44.Folk B. Traumatic thumb injury management using mobilization with movement. Man Ther. 2001;6(3):178–182. doi: 10.1054/math.2001.0414. [DOI] [PubMed] [Google Scholar]
- 45.Paungmali A., O'Leary S., Souvlis T., Vicenzino B. Hypoalgesic and sympathoexcitatory effects of mobilization with movement for lateral epicondylalgia. Phys Ther. 2003;83(4):374–383. [PubMed] [Google Scholar]
- 46.Lee J.H.Y.W., Lee K.S. Effects of head-neck rotatio and Kinesio taping of the flexor muscles on dominant hand grip strength. J Phys Ther Sci. 2010;22(3):285–289. [Google Scholar]
- 47.Bialosky J.E., Bishop M.D., Price D.D., Robinson M.E., George S.Z. The mechanisms of manual therapy in the treatment of musculoskeletal pain: a comprehensive model. Man Ther. 2009;14(5):531–538. doi: 10.1016/j.math.2008.09.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Imamura M., Imamura S.T., Kaziyama H.H. Impact of nervous system hyperalgesia on pain, disability, and quality of life in patients with knee osteoarthritis: a controlled analysis. Arthritis Rheum. 2008;59(10):1424–1431. doi: 10.1002/art.24120. [DOI] [PubMed] [Google Scholar]
- 49.Ossipov M.H., Dussor G.O., Porreca F. Central modulation of pain. J Clin Invest. 2010;120(11):3779–3787. doi: 10.1172/JCI43766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Beaton D.E., Katz J.N., Fossel A.H., Wright J.G., Tarasuk V., Bombardier C. Measuring the whole or the parts? Validity, reliability, and responsiveness of the Disabilities of the Arm, Shoulder and Hand outcome measure in different regions of the upper extremity. J Hand Ther. 2001;14(2):128–146. [PubMed] [Google Scholar]
- 51.Straus S.E., Tetroe J., Graham I.D., Zwarenstein M., Bhattacharyya O., Shepperd S. Monitoring use of knowledge and evaluating outcomes. CMAJ. 2010;182(2):E94–E98. doi: 10.1503/cmaj.081335. [DOI] [PMC free article] [PubMed] [Google Scholar]


