Abstract
Objective
The purpose of this case report is to describe chiropractic management of a patient with arm and hand numbness and who was suspected to have ulnar nerve compression.
Clinical Features
A 41-year-old woman presented with hand weakness and numbness along the medial aspect of her right forearm and the 3 most medial fingers. The onset of symptoms presented suddenly, 3 weeks prior, when she woke up in the morning and assumed she had “slept wrong.” The patient’s posture showed protracted shoulders and moderate forward head carriage. Orthopedic assessment revealed symptomatic right elevated arm stress test, grip strength asymmetry, and a Tinel sign at the right cubital tunnel.
Intervention and Outcome
The patient was treated using chiropractic care, which consisted of manipulative therapy, myofascial therapy, and elastic therapeutic taping. Active home care included performing postural exercises and education about workstation ergonomics. She demonstrated immediate subjective improvement of her numbness and weakness after the first treatment. Over a series of 11 treatments, her symptoms resolved completely; and she was able to perform work tasks without dysfunction.
Conclusion
Chiropractic treatment consisting of manipulation, soft tissue mobilizations, exercise, and education of workstation ergonomics appeared to reduce the symptoms of ulnar nerve compression symptoms for this patient.
Key indexing terms: Nerve compression syndrome, Thoracic outlet, Cubital tunnel syndrome, Chiropractic
Introduction
Compression neuropathy is a common problem in the upper limb and is often the result of a compressed nerve at various points over its course in the upper limb.1 Compression syndromes can result in dysfunction and, if left to become a chronic problem, may lead to irreversible morbidity.1 Clinically, most patients may effectively be managed with conservative measures.2 Therefore, it is important to be able to identify, clinically diagnose, and treat these compression syndrome as early as possible.
The chiropractic profession offers several theories as to the cause of nerve compression complexes. As early as 1910, Palmer3 suggested that spinal “subluxation” interfered with normal transmission of nerve energy, which could lead to dysfunction. Other theories suggest that nerves are not very susceptible to altered electrical function with bone on nerve compression, but hypothesize that axoplasmic flow may be altered or deranged when the nerve is compressed. 4
Upton and McComas5 first suggested the term double crush syndrome (DCS). They described that compression of an axon at one location makes it more sensitive to the effects of compression at another location, resulting from impaired axoplasmic flow.5 Therefore, the DCS theory suggests that 2 lesions along the same axon with little or no independent clinical ramifications, when combined, lead to appearance or magnification of symptoms.6 It is theorized that DCS can involve 2 compression sites along a peripheral nerve or 1 compression site on the peripheral nerve and 1 compression site at its corresponding spinal nerve root(s) level. There is some evidence to support the DCS theory.7,8 However, Golovchinsky9 stated that the exact neurophysiological and cellular mechanisms of this phenomenon have not been clearly established or accepted. Because of the unknown mechanisms of a DCS, its existence has been a matter of debate.9
There is little literature on chiropractic management of ulnar compression disorders or DCS.10 Therefore, the purpose of this case report is to describe the management of a patient with ulnar compression symptoms with suspected DCS.
Case report
A 41-year-old white woman presented to a chiropractic clinic with right hand weakness, and right medial sided forearm and hand numbness. The onset of symptoms presented suddenly, 3 weeks prior, when she woke up in the morning and assumed she had “slept wrong.” She denied any trauma. The symptoms were described by the patient as being “heavy and tight.” The severity of numbness was measured as 6.4 cm (a number derived from the average numbness in the hand and forearm) on a visual analog scale (VAS). The VAS used a horizontal line that measured 10 cm in length. For this particular patient’s complain of numbness, a measurement of 0 cm meant there was no numbness; and a measurement of 10 cm represented complete numbness. She worked full-time as an academic counselor. She described sitting “hunched” over during the work day. She claimed to spend most of her time typing on the keyboard and talking on the phone. She had an earpiece for the phone. The patient noticed that, once the numbness began, she had difficulties with most work duties and activities of daily living. In particular, she complained of an inability to type and write with the right hand. She would only stretch and get up to use the restroom or go for lunch. When asked about associated symptoms, she stated that, occasionally, her right 3 medial fingers “blanched.” She was unable describe more details with respect to the blanching. The patient denied anything that made the symptoms better or worse. The patient denied her hands feeling cold or clammy or having swelling. The patient was self-medicating with over-the-counter ibuprofen daily because she thought it would help with the numbness. She claimed that the ibuprofen did not help the symptoms. In addition, she was taking birth control (Kariva, manufactured by Teva Pharmaceuticals) for over 10 years.
Inspection of posture revealed moderate forward head carriage, with severe bilaterally protracted shoulders. Palpation of the cervical musculature was nonremarkable for muscle spasm or tenderness. Cervical spine active ranges of motion were full and pain-free. Assessment of joint play of the cervical and thoracic intervertebral joints was restricted in several areas in the lower cervical spine and upper thoracic spine. Palpation of the right triceps surae and common wrist flexors was hypertonic and produced a mild discomfort for the patient. Orthopedic testing revealed that the elevated arm stress test (EAST) was positive for numbness and “a cold feeling” on her symptomatic side within 2 minutes of performing the test. The EAST maneuver was performed by having the patient lift both arms to 90° of abduction with full shoulder external rotation and close and open their fists for several minutes or until symptoms appeared. 11,12 Radial pulses did not diminish or lose patency on the affected side. The results of the following tests were negative: Valsalva, cervical compression, and distraction. Range of motion of both wrists and elbows was full and pain-free. Tinel sign, at the right cubital tunnel, reproduced the patient's symptoms of numbness into her right hand along the 3 medial fingers. The results of the following orthopedic tests were negative without significant findings: Allen test, Phalen maneuver, reverse Phalen maneuver, Tinel sign at the carpal tunnel, and Tinel sign at the tunnel of Guyon. Grip strength was tested using a blood pressure cuff. An average of 240 mm Hg was noted on the right and 260 mm Hg on the left. Weakness was found in the right biceps, triceps, brachioradialis, and the medial two fingers. All other upper extremity motor testing was unremarkable. Reflexes in the upper extremities were 2 + bilaterally. The patient indicated an inability to discriminate between sharp and dull sensations along the thenar region in the symptomatic right hand.
The working diagnosis was subacute mild right ulnar nerve pathology with associated thoracic and cervical intersegmental dysfunction. It was suspected that there was compression of the ulnar nerve at the thoracic outlet and cubital tunnel.
Treatment consisted of diversified chiropractic manipulative therapy to the restricted segments of the cervicothoracic and thoracic spine. Because of the positive Tinel finding over the cubital tunnel, elastic therapeutic tape was applied using a “lifting” technique over the right cubital tunnel. This technique involves having the patient flex her right elbow and then placing a 4” × 2” piece of elastic tape on top of the skin with a tape stretch of approximately 25% to 50% (Fig 1). Another piece of elastic tape was used to reduce the muscle tone of the right common wrist flexors. This tape was placed starting at the right ulnar styloid with a 25% to 50% stretch and ending at the right medial epicondyle. Additional passive modalities included a myofascial release to the right triceps, common wrist and elbow flexors, cubital tunnel, and lumbricals. To address the postural findings, the patient was given active care that consisted of performance of a postural exercises every hour during waking hours. The following are the instructions that were given to the patient to perform the postural exercises (Fig 2 and Fig 3.) Wall push-ups were given in which the patient was instructed to perform 3 sets of 50 twice a week. In addition, the patient received directions to have her employer’s ergonomic specialist help rearrange her office.
Fig 1.
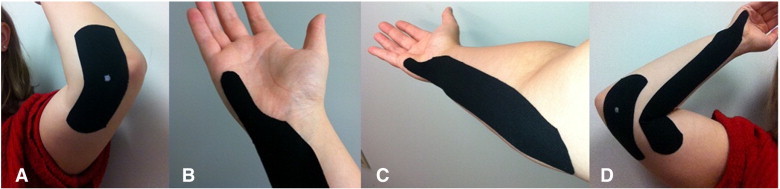
Elastic therapeutic taping technique. A, A “lifting” technique placed over the cubital tunnel (white dot is where the center of the patient’s cubital tunnel is located) with 25% to 50% of tension applied to the tape. B, Reducing the hypertonicity of the common wrist flexor group by applying elastic tape from the ulnar styloid up to the medial epicondyle with approximately 25% to 50% of tension in the tape. C, Completed tapings shown together.
Fig 3.
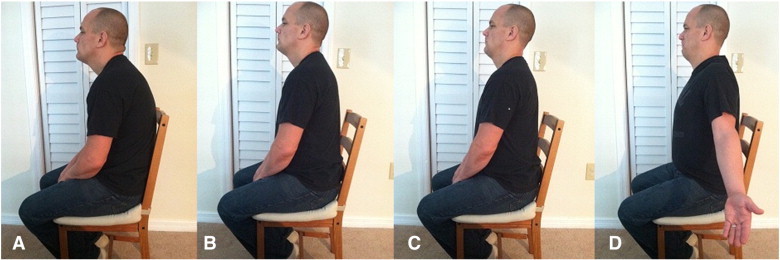
Postural exercises. A, Normal posture (before exercise). B, Patient is instructed to lift chest superiorly and anteriorly while also creating an anterior pelvic tilt. C, Patient is asked to breath normally and tuck the chin into retraction toward his neck without inducing neck flexion. D, Patient will then attempt to bring his shoulder blades together by externally rotating arms and placing them into extension (special focus on not activating the upper trapezius muscles).
Fig 2.
Instructions for postural exercises
| 1. Sit at the edge of a chair. |
| 2. Rock the pelvis forward bringing your low back into extension. |
| 3. Tuck the chin slightly toward the neck. |
| 4. With the hands turned forward and the elbow straight bring, bring the arms backward attempting to pull the shoulder blades together. |
| 5. Hold this position for 15 s breathing normally. |
| 6. Release this position. |
A total of 11 treatments were rendered in this patient’s care. After 8 visits, approximately 4 weeks after initiation of care, the reevaluation was performed. Results of both the Tinel sign at the right elbow and EAST were negative. Her posture had reduced forward head carriage, and her shoulders were not internally rotated. At this time, she had no numbness in her right hand and no signs of upper extremity dysfunction. The decision was made for the patient to return to care once biweekly for up another 4 weeks; and if she continued to have no subjective discomfort or numbness, she would be released from care. Overall, the patient’s severity of numbness, as measured by VAS, went from 6.4 to 0 cm within 6 visits. Full function returned within 5 visits, and no exacerbation of pain continued until she was released. At the 11th and final visit, she had no symptoms, was able to return to regular work duties without any dysfunction, and was released from care.
Discussion
The authors hypothesize that patient symptoms were the result of compression of the ulnar nerve resulting from muscular imbalances, restricted motion, and fascial restrictions. This reasoning was based on the reduction of patient’s symptoms with myofascial mobilizations and correction of muscular imbalances through exercises. It was suspected that there was distal entrapment at the cubital tunnel and that the proximal entrapment site was at the thoracic outlet.
Several authors have suggested that thoracic outlet syndrome (TOS) may be a possible element in DCS and peripheral nerve compressions.13 Peet14 used the term TOS to refer to compression of the neurovascular structures in the area just above the first rib and behind the clavicle. There are 3 categories of TOS: arterial, venous, and neurogenic (nTOS).15 In this care, it was theorized that the patient had a case of nTOS because of the neurological symptomatology of an ulnar nerve compression and a positive EAST sign. Thoracic outlet syndrome may present with a large constellation of symptoms clinically due to the compression or entrapment of the whole or part of the brachial neurovascular bundle. It is typically characterized by pain, paresthesias, and weakness in the upper extremity.15 The fourth and fifth fingers are most affected with paresthesias, and the severity of these symptoms tends to become worse at the end of the day or during sleep.15 The diagnosis of TOS can be made by history, physical examination, orthopedic tests, ultrasonography, radiological evaluation, and electrodiagnostic studies (EDS).11 Electrodiagnostic studies were not taken on this patient. It was determined by the physician that EDS were not needed at this time; however, they may be implemented in the future if conservative care was not helping.
Provocative orthopedic tests, such as Adson test, are nonspecific.11,12 However, the EAST sign is a provocative maneuver that may have some general predictive value in screening11,12 and may assist in the diagnosis of nTOS.16 However, the literature shows a high false-positive rate for these tests in healthy subjects.16 According to Nord et al,16 the sensitivity and specificity of these tests for nTOS have not been established; and provocative testing is not a replacement for EDS.
It is possible that the cause of the symptoms in this patient’s case were from mechanical dysfunction in the form of poor posture. The authors hypothesize that the poor posture was amplified because of the patient’s ergonomically incorrect workstation. Poor workplace ergonomics can create musculoskeletal disorders that can happen from manual or repetitive work that puts strains on the body systems.17 A variety of repetitive hand intensive work may contribute to soft tissue injuries of the upper extremities.17 Repetitive tasks in the employment field have been considered in analyses of compression syndromes.18 The patient in this case spent approximately 8 hours a day typing and making phone calls. She claimed that her wrists always held in an extended position and that she had a “hunched back.” During the physical examination, it was noted that she had increased forward head carriage and internally rotated shoulders. This type of abnormal posture could possibly lead to symptoms associated with TOS.19 Generalized muscle imbalance of the cervical spine and shoulder girdle may lead to fascial thickening and fibrosis of some muscle with resultant constriction of the thoracic outlet.20 Poor posture with a forward head carriage and internally rotated shoulders could possibly decrease the costoclavicular space and, over time, lead to shortening of the scalenes and pectoralis minor muscle. This may form a vicious cycle21-23 and possible compression of the brachial neurovascular complex (Fig 4). In the early 1990s, a theory based on muscle engram developed.24 During this period, Liebenson25 theorized that because the maintenance of the muscle imbalance was potentially caused more by muscle hypertonicity than hypotonicity, more emphasis should be placed on relaxing the hypercontracted muscles and less on strengthening the shoulder girdle muscles. A postural exercise was prescribed for the patient based on these findings. Pavlu et al26 describe Brügger’s work for postural correction exercises used in this case.
Fig 4.
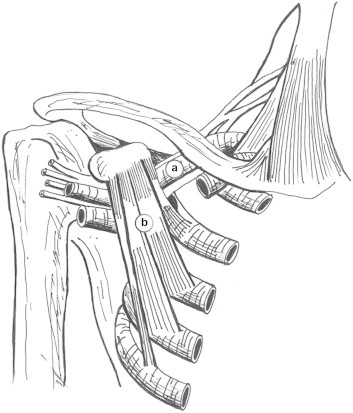
Thoracic outlet: compression of the brachial neurovascular bundle (A) due to the pectoralis minor muscle (B).
The second suspected compression site was thought to be at the cubital tunnel because of a positive Tinel sign at the elbow. Cubital tunnel syndrome is a condition brought on by an increase in the pressure exerted upon the ulnar nerve at the cubital tunnel and is the most common entrapment condition involving the ulnar nerve.27,28 It is second only to carpal tunnel syndrome in compressive neuropathologies of the upper extremities.27,28 Repetitive overhead activities, such as throwing, are a primary cause of this condition. The ulnar nerve is the terminal branch of the medial cord of the brachial plexus and contains fibers from the C8 and T1 spinal nerve roots.29 It traverses the cubital tunnel to enter the forearm where it passes between the 2 heads of the flexor carpi ulnaris muscle. Fig 5 demonstrates the 5 areas of common entrapments for the ulnar nerve at the elbow. The unusual anatomy of the cubital tunnel and the increase in intraneural pressure associated with elbow flexion are believed to be key issues in the pathogenesis of cubital tunnel syndrome.28
Fig 5.
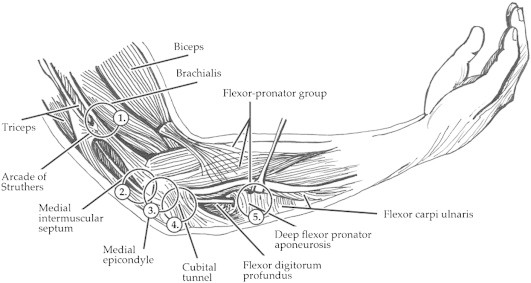
Cubital tunnel syndrome: the 5 common areas of entrapment of the ulnar nerve. (1) arcade of Struthers, (2) medial intermuscular septum, (3) medial epicondyle, (4) cubital tunnel, and (5) flexor-pronator group.
The classic clinical symptomatology of those with cubital tunnel syndrome is having paresthesias over the small and ring fingers.1,30 Typically, these sensory deficits are seen first in the disease, followed by motor dysfunction as the compression of the nerve becomes chronic in nature.1 Graham et al31 have published the theorized most important symptoms to diagnose CTS:
-
1.
Numbness and tingling in the median nerve distribution
-
2.
Nocturnal numbness
-
3.
Weakness and/or atrophy of the thenar musculature
-
4.
Tinel sign
-
5.
Phalen test
-
6.
Loss of 2-point discrimination
The suspicion of cubital tunnel syndrome was based upon the patient’s symptoms and a positive Tinel sign at the cubital tunnel reproducing these symptoms.
It was hypothesized that the patient’s poor posture combined with poor work ergonomics (ie, her workstation chair is too low with a high desk that promoted extended elbow flexion with wrist extension). In the authors’ opinion, it is believed that these chronic issues can lead to an ischemic compression to the ulnar nerve at the sites of the entrapment. Active treatment using myofascial release techniques and elastic therapeutic taping were used during each treatment. In myofascial therapies, it has been suggested that subjective and objective improvements should be observed in the first to third treatments.32-34 In the case of this patient, she had an immediate symptomatic improvement after the first treatment.
The authors hypothesized that the main clinical use of elastic therapeutic taping is to normalize muscle tone. The patient in this case received treatment to her right forearm wrist flexors, in theory to reduce the compression along the ulnar’s nerve path. It is believed that when the tape is applied to the skin with a light to moderate amount of tension (approximately 25%-50% of the tape’s total resting length), the recoil effect of the elasticity of the tape lifts the skin to create a shearing force to the underlying fascia.35 The exact mechanism by which elastic therapeutic tape can influence different tissues and functions is unknown. It is claimed that the tape can improve blood and lymphatic flow and decrease pain through affecting nerve signals 36; however, no research has been published to support these claims. There has been some preliminary research that demonstrates elastic taping techniques may increase the range of motion of the neck and increase bioelectric activity of the vastus medialis muscle and lower trapezius.37,38 In the case presented, it is believed that the elastic tape increased lymphatic flow that may have aided in decreasing an ischemic compression to the ulnar nerve because the tape was placed over an entrapment site of the ulnar nerve at the cubital tunnel. In addition, it is hypothesized that the tape aided in a process of mechanotransduction that, over an unknown period, helped with superficial and deep fascial release. The clinical efficacy of manual therapy for mild to moderate peripheral nerve entrapments is lacking sufficient evidence.
Manual therapies that involve soft tissue mobilization are intended to release fascial adhesions,39 stimulate mechanoreceptors,40 and increase lymphatic fluid flow.41 These outcomes are used to increase ranges of motion and thereby function. It is intended that this mechanically can allow for decreased compression at the site of nerve entrapment. In addition, the increase ranges of motion may allow for decreased ischemia of the vasa nervorum of the nerve by increasing circulation to the area.42
Limitations
Advanced studies, such as electromyographic testing, were not used to confirm diagnosis of neuropathy; thus, a definitive diagnosis could not be confirmed. Electrophysiological studies are essential for the diagnosis and management of entrapment neuropathies.43 In this case, the diagnoses were made based upon the subjective symptomatology of the patient and orthopedic findings. Orthopedic examination testing may be of value; but on average, specificity is 53% and sensitivity is 72%.44 It was believed that this patient possibly had DCS, but it cannot be confirmed without electromyographic testing. The patient may have had additional conditions that mimicked or overlapped the primary condition, which may have confounded the results (eg, trigger points or other musculoskeletal conditions). The treatment provided was multimodal, so it is unknown if any particular component was more effective than another. As well, the patient may have improved because of other reasons such as other activities or because of the natural course of the disorder; thus, we cannot say for certain that improvements were solely the results of the chiropractic management of this case.
Conclusions
The patient in this case appeared to benefit from a course of chiropractic conservative and multimodal management of her symptoms. Within the span of 11 visits, her symptoms resolved; and she was able to return to full function and work duties.
Funding sources and potential conflicts of interest
No funding sources or conflicts of interest were reported for this study. This case report is submitted as partial fulfillment of the requirements for the degree of Master of Science in Advanced Clinical Practice in the Lincoln College of Postprofessional, Graduate, and Continuing Education at the National University of Health Sciences.
Acknowledgment
The authors thank Robert Hansen for the anatomical illustrations in this article.
References
- 1.Mukund R., Mansukhani T., Mansukhani K. Compressive neuropathy in the upper limb. Indian J Plast Surg. 2011;44(2):283–297. doi: 10.4103/0970-0358.85350. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Arle J., Zager E. Surgical treatment of common entrapment neuropathies in the upper limbs. Muscle Nerve. 2000;23:1160–1174. doi: 10.1002/1097-4598(200008)23:8<1160::aid-mus2>3.0.co;2-4. [DOI] [PubMed] [Google Scholar]
- 3.Palmer D.D. Portland Printing House; Portland, OR: 1910. The science, art and philosophy of chiropractic. [Google Scholar]
- 4.Leach R. 2nd ed. Williams and Wilkins; Baltimore: 1986. The chiropractic theories: a synopsis of scientific research. 49–70. [DOI] [PubMed] [Google Scholar]
- 5.Upton A.R.M., McComas A.J. The double crush in nerve entrapment syndromes. Lancet. 1973;2:359–362. doi: 10.1016/s0140-6736(73)93196-6. [DOI] [PubMed] [Google Scholar]
- 6.Swenson R.S. Double crush syndrome: what is the evidence? J Neuromusculoskeletal System. 1993;1:23–29. [Google Scholar]
- 7.Massey E.W., Riley T.L., Pleet A.B. Coexistent carpal tunnel syndrome and cervical radiculopathy (double crush syndrome) South Med J. 1981;74:957–959. doi: 10.1097/00007611-198108000-00018. [DOI] [PubMed] [Google Scholar]
- 8.Hurst L.C., Weissberg D., Carroll R.E. The relationship of the double crush to carpal tunnel syndrome (an analysis of 1,000 cases of carpal tunnel syndrome) J Hand Surg [Br] 1985;10:202–204. doi: 10.1016/0266-7681(85)90018-x. [DOI] [PubMed] [Google Scholar]
- 9.Golovchinsky V. Kluwer; Norwell, MA: 2000. Double crush syndrome. [Google Scholar]
- 10.Russell B.S. A suspected case of ulnar tunnel syndrome relieved by chiropractic extremity adjustment methods. J Manipulative Physiol Ther. 2003;26(9):602–607. doi: 10.1016/j.jmpt.2003.08.005. [DOI] [PubMed] [Google Scholar]
- 11.Roos D.B. Thoracic outlet syndrome is underdiagnosed. Muscle Nerve. 1999;22(1):126–129. doi: 10.1002/(sici)1097-4598(199901)22:1<126::aid-mus21>3.0.co;2-s. [DOI] [PubMed] [Google Scholar]
- 12.Gillard J., Perez-Cousin M., Hachulla E., Remy J., Hurtevent J.F., Vinckier L. Diagnosing thoracic outlet syndrome: contribution of provocative tests, ultrasonography, electrophysiology, and helical computed tomography in 48 patients. Joint Bone Spine. 2001;68(5):416–424. doi: 10.1016/s1297-319x(01)00298-6. [DOI] [PubMed] [Google Scholar]
- 13.Narakas A.O. The role of thoracic outlet syndrome in the double crush syndrome. Ann Hand Surg. 1990;9(5):331–340. doi: 10.1016/s0753-9053(05)80506-x. [DOI] [PubMed] [Google Scholar]
- 14.Peet R.M., Henriksen J.D., Anderson T.D., Martin G.M. Thoracic outlet syndrome: evaluation of a therapeutic exercise program. Proc Mayo Clin. 1956;131:281–287. [PubMed] [Google Scholar]
- 15.Brantigan C.O., Roos D.B. Diagnosing thoracic outlet syndrome. Hand Clin. 2004;20:27–36. doi: 10.1016/s0749-0712(03)00080-5. [DOI] [PubMed] [Google Scholar]
- 16.Nord K.M., Kapoor P., Fisher J., Thomas G., Sundaram A., Scott K. False positive rate of thoracic outlet syndrome diagnostic maneuvers. Electromyogr Clin Neurophysiol. 2008;48(2):67–74. [PubMed] [Google Scholar]
- 17.Biswas R., Sachdev V., Jindal V., Ralhan S. Musculoskeletal disorders and ergonomic risk factors in dental practice. Indian J Dent Sci. 2012;4(1):70–74. [Google Scholar]
- 18.Gerr F., Letz R., Landrigan P.J. Upper extremity muscluoskeletal disorders of occupational origin. Annu Rev Publ Health. 1991;12:543–566. doi: 10.1146/annurev.pu.12.050191.002551. [DOI] [PubMed] [Google Scholar]
- 19.Nicholas A. The thoracic outlet syndrome in athletes. J Am Board Fam Pract. 1996;9(5):346–355. [PubMed] [Google Scholar]
- 20.Vanti C., Natalini L., Romeo A., Tosarelli D., Pillastrini P. Conservative treatment of thoracic outlet syndrome. A review of the literature. Eura Medicophys. 2007;43(1):55–70. [PubMed] [Google Scholar]
- 21.Mackinnon S.E., Novak C.B. Clinical commentary: pathogenesis of cumulative trauma disorder. J Hand Surg (Am) 1994;19:873–883. doi: 10.1016/0363-5023(94)90205-4. [DOI] [PubMed] [Google Scholar]
- 22.Sucher B.M. Thoracic outlet syndrome. A myofascial variant: part 1. Pathology and diagnosis. J Am Osteopath Assoc. 1990;90(686–96):703–704. [PubMed] [Google Scholar]
- 23.Sucher B.M., Heath D.M. Thoracic outlet syndrome. A myofascial variant: part 3. Structural and postural considerations. J Am Osteopath Assoc. 1990;93(334):340–345. [PubMed] [Google Scholar]
- 24.Sucher B.M., Heath D.M. Thoracic outlet syndrome. A myofascial variant: part 2. Treatment. J Am Osteopath Assoc. 1990;90(810–2):817–823. [PubMed] [Google Scholar]
- 25.Liebenson C. Thoracic outlet syndrome: diagnosis and conservative management. J Manipulative Physio Ther. 1988;11:493–499. [PubMed] [Google Scholar]
- 26.Pavlu D., Petak-Kruegger S., Janda V. Rehabilitation of the spine: Brügger methods for postural correction. C. Lippincott Williams and Wilkins; Philadelphia, PA: 2007. pp. 352–369. [Google Scholar]
- 27.Bednar M.S., Blair S.J., Light T.R. Complications of the treatment of cubital tunnel syndrome. Hand Clin. 1994;10:83–92. [PubMed] [Google Scholar]
- 28.Norkus S.A., Meyers M.C. Ulnar neuropathy of the elbow. Sports Med. 1994;17:189–199. doi: 10.2165/00007256-199417030-00005. [DOI] [PubMed] [Google Scholar]
- 29.Cutts S. Cubital tunnel syndrome. Postgrad Med J. 2007;83(975):28–31. doi: 10.1136/pgmj.2006.047456. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Elhassan B., Steinmann S.P. Entrapment neuropathy of the ulnar nerve. J Am Acad Orthop Surg. 2007;15:672–681. doi: 10.5435/00124635-200711000-00006. [DOI] [PubMed] [Google Scholar]
- 31.Graham B., Regehr G., Naglie G., Wright J.G. Development and validation of diagnostic criteria for carpal tunnel syndrome. J Hand Surg. 2006;31A:919–924. [PubMed] [Google Scholar]
- 32.Leahy P.M., Mock L.E. Myofascial release technique and mechanical compromise of peripheral nerves of the upper extremity. Chiropract Sports Med. 1992;6:139–150. [Google Scholar]
- 33.Buchberger D.J. Use of active release techniques in postoperative shoulder: a case report. J Sports Chiropr Rehabil. 1999;13:60–65. [Google Scholar]
- 34.Pajaczkowski J.A. Mimicking turf-toe: myofasopathy of the first dorsal interosseous muscle treated with ART. J Can Chiropr Assoc. 2003;47:28–32. [Google Scholar]
- 35.Gonzalez-Iglesias J., Fernandez-de-Las-Penas C., Cleland J.A., Huijbregts P., Del Rosario Gutierrez-Vega M. Short-term effects of cervical Kinesio taping on pain and cervical range of motion in patients with acute whiplash injury: a randomized clinical trial. J Orthop Sports Phys Ther. 2009;39:515–521. doi: 10.2519/jospt.2009.3072. [DOI] [PubMed] [Google Scholar]
- 36.Kase K., Tatsuyuki H., Tomoki O. Kinesio Taping Association; Tokyo: 1998. Kinesio taping perfect manual. [Google Scholar]
- 37.Yoshida A., Kahanov L. The effect of Kinesio taping on lower trunk range of motions. Res Sports Med. 2007;15:103–112. doi: 10.1080/15438620701405206. [DOI] [PubMed] [Google Scholar]
- 38.Slupik A., Dwornik M., Bialoszewski D., Zych E. Effect of the Kinesio taping on bioelectrical activity of vastus medialis muscle: preliminary report. Ortop Traumatol Rehabil. 2007;9:644–651. [PubMed] [Google Scholar]
- 39.Hammer W. Integrative fascial release and functional testing. Australas Chiropr Osteopathy. 2000;9(1):13–16. [PMC free article] [PubMed] [Google Scholar]
- 40.Schleip R. Fascial plasticity: a new neurobiological explanation. J Bodywork Mov Ther. 2003;7(1):11–19. [Google Scholar]
- 41.Giampietro V., Sayers J., McBrier N., Buckley W. Systematic review of efficacy for manual lymphatic drainage techniques in sports medicine and rehabilitation: an evidence-based approach. J Man Manip Ther. 2009;17(3):e80–e89. doi: 10.1179/jmt.2009.17.3.80E. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Smith D.R., Kobrine A.I., Rizzoli H.V. Blood flow in peripheral nerves: normal and post severance flow rates. J Neurol Sci. 1977;33:341–346. doi: 10.1016/0022-510x(77)90131-9. [DOI] [PubMed] [Google Scholar]
- 43.David C., Preston D.C., Barbara E., Shapiro B.E. Elsevier; Philadelphia: 1998. Electromyography and neuromuscular disorders. Clinical-electrophysiologic correlations. 2nd ed. [Google Scholar]
- 44.Gillard J., Perez-Cousin M., Hachulla E., Remy J., Hurtevent J.F., Vinckier L. Diagnosis thoracic outlet syndrome: contribution of provocative test, ultrasonography, electrophysiology, and helical computed tomography in 48 patient. Joint Bone Spine. 2001;68:416–424. doi: 10.1016/s1297-319x(01)00298-6. [DOI] [PubMed] [Google Scholar]


