Abstract
Vessel sealing devices effectively produce hemostatic seals with minimal thermal damage, but the strength of seals decreases as vessel diameter increases. Because vessels sealed at an angle to the vessel require a greater functional seal diameter than those sealed perpendicularly to the vessel, it was hypothesized that perpendicular seals would have comparably higher burst pressures. Ex vivo, porcine carotid arteries of nominal diameters of 5, 6, and 7 mm were sealed perpendicularly to and at a 45° angle to the longitudinal axis of the vessels, and burst pressures of the sealed vessels were measured. Overall burst pressures were 51% greater for perpendicular seals than for angled seals (P<.001). Mean burst pressures for the 5-mm angled and 7-mm perpendicular groups, which have similar seal lengths, were not significantly different (P=.959). Analysis using the functional diameter as a covariate indicated that the seal length is the primary variable in determining burst pressure, and not some other inherent characteristic of angled versus perpendicular sealing. These results suggest that at least for vessels ≥5 mm in diameter, surgeons should approach vessels perpendicularly and not at an angle, for the highest possible seal strength. The development of articulated sealing and cutting devices would provide greater seal strength, in addition to improved maneuverability, especially in laparoscopic surgery, where angles of approach may be limited by the fixed location of surface cannulas.
Introduction
Methods for sealing blood vessels strive to follow Halsted's principles1 by producing immaculate hemostasis with minimal tissue damage. Modern commercial devices2 can effectively and efficiently seal vessels using the mechanisms elucidated by Sigel and Dunn3 of compression, heat, and time. A critical parameter of vessel sealing has always been strength. When sealing blood vessels, it is desirable to produce seals with a strength that is supraphysiological (i.e., substantially greater than 120 mm Hg). Ex vivo burst pressure is commonly used as a surrogate for seal strength. The greater the experimentally determined burst pressure, the less likely the chance of failure under physiological conditions. Ex vivo studies in laboratories, however, generally examine burst strength by evaluating seals made perpendicularly to the blood vessel under controlled conditions.
Unfortunately, the clinical environment is not one that always allows for perpendicular seals, especially in laparoscopic surgery, where angles are hampered by the fixed nature of the abdominal wall cannulas and the historical absence of adequate articulating hemostatic tools. New laparoscopic instruments with the ability to articulate their end effectors are now available, including bipolar energy instruments used for coagulating vessels. Because strong vessel seals are important for adequate homeostasis, the value of an articulating vessel sealing device may primarily reside in its ability to maneuver around corners and behind structures, as well as allowing a perpendicular approach to vessels or bundles.
It is well recognized that burst pressures decrease with increasing vessel diameter,4,5 currently limiting the usability of energized sealing devices to vessel diameters of 7 mm or less. Although there are several studies showing an inverse correlation between burst pressure and vessel diameter, there is little discussion in the literature on the effect of sealing vessels at an angle rather than perpendicularly to the longitudinal axis of the vessel. As the functional diameter of a vessel can be expected to increase when the sealing device is applied at a non-perpendicular angle to the longitudinal axis of the blood vessel, it may be anticipated that perpendicular vessel seals will be stronger and display higher burst pressures than those sealed at an angle.
With any surgical technology, optimal results often depend upon the method of use, and in the case of vessel sealing, it was hypothesized that the strength of a seal may depend upon the angle at which the sealing device is applied. The purpose of this study was to quantitatively determine whether there are differences in strength between vessels of similar nominal outer diameter that are sealed perpendicularly to the blood vessel and those sealed at a 45° angle. We theorized that for vessels of similar size, seals created at a 45° angle would have a greater functional diameter and hence would exhibit lower burst pressures than those sealed perpendicularly to the longitudinal axis of the blood vessel.
Materials and Methods
Carotid arteries harvested from a porcine model were obtained from Animal Biotech Industries (Danboro, PA). The vessel outer diameters were measured visually and sorted into three groups: 5 mm (4.5 mm to <5.5 mm), 6 mm (5.5 mm to <6.5 mm), and 7 mm (6.5–7.5 mm). Each vessel was randomly assigned to be sealed and transected with the device shaft either perpendicular to the vessel (90°) or at a 45° angle (Fig. 1). Vessels were sealed using one of six 14-cm ENSEAL® ETRIO314H tissue sealers (Ethicon Endo-Surgery, Cincinnati OH) by the method provided in the manufacturer's instructions for use.6 This vessel sealer is an advanced bipolar device intended for use during open or laparoscopic surgery to transect and dissect tissue. Sealing of a vessel is effected by application of controlled radiofrequency energy while the vessel is compressed, and the vessel is cut via movement of a knife under a consistent shear. The device is cleared for use in sealing vessels up to and including 7 mm in diameter.
FIG. 1.
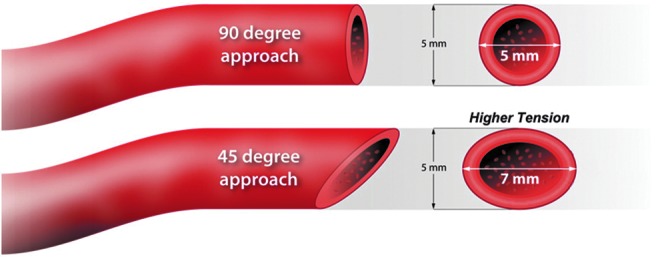
Angled versus perpendicular orientation comparison.
The orientation of transections was carried out by visual alignment using a right-angled triangle drawn on the procedure table for reference. All perpendicular orientations were completed with the device shaft perpendicular to the vessel, whereas all angled orientations were made with the device shaft at a 45° angle to the vessel. The functional diameter was established as the length of the seal required to completely seal the vessel irrespective of the nominal diameter of the vessel.
Burst pressure testing was conducted on the left and right side seals of each transected vessel. The pressure system consisted of a computer-controlled syringe pump (Harvard Apparatus, Holliston, MA) with an inline pressure transducer. Physiologic saline was used as an infusion medium at a flow rate of 47 mL/minute. Intraluminal pressure data acquisition during testing was performed using the LabView® system design software (National Instruments Corp., Austin, TX), including the maximal pressure at failure.
In all analyses, the minimum bursting pressure of either the left or right side of the transection was used. Burst pressure differences between vessel groups were compared via t test, and overall burst pressures were modeled via analysis of variance with factors of vessel size, instrument, and orientation. An additional comparison was performed between the group of 5-mm angled seals and the group of 7-mm perpendicular seals.
Supplementary analysis was performed to understand the relationship between functional vessel diameter and burst pressure. Vessels sealed at a 45° angle have a functional diameter greater than their nominal diameter by a factor of √2 (1.414…). Analysis of covariance was performed on the minimum of the left and right burst pressures using device and orientation as categorical factors, the inverse of the functional diameter as a covariate (mm−1), and the interaction between orientation and the inverse of the functional diameter. The functional diameter of perpendicular applications was taken as the nominal diameter, and the functional diameter of angled applications was calculated as the product of the nominal diameter and √2. Minitab® software (Minitab Inc., State College, PA) was used in the analysis of all data.
Results
A typical set of sealed vessels is shown in Figure 2. In total, 87 perpendicular and 89 angled vessels were sealed (Table 1). There were no significant differences between the mean vessel diameters of perpendicular and angled applications for any of the three vessel groups or overall. The vast majority of vessel bursts were observed at the seal. The few vessels that leaked at the adventitia or at a branch were excluded from the analysis, as these leaks were attributed to potential vessel damage as a result of harvesting. Sealing angle did not appear to affect the small number of bursts that did not occur at the seal.
FIG. 2.

Porcine carotid arteries sealed (left) perpendicularly and (right) at an angle. The scale below is 1 mm per line.
Table 1.
Summary of Vessel Diameters and Burst Pressures for Groups and Overall
| Group, measure | Perpendicular | Angled | P value |
|---|---|---|---|
| 5 mm | |||
| n | 39 | 44 | — |
| Mean diameter (mm) | 4.9±0.2 | 5.0±0.3 | .573 |
| Burst pressure (mm Hg) | 809±368 | 498±295 | <.001 |
| 6 mm | |||
| n | 25 | 25 | — |
| Mean diameter (mm) | 5.9±0.3 | 5.8±0.3 | .759 |
| Burst pressure (mm Hg) | 676±323 | 451±285 | .012 |
| 7 mm | |||
| n | 23 | 20 | — |
| Mean diameter (mm) | 7.0±0.3 | 7.0±0.3 | .996 |
| Burst pressure (mm Hg) | 484±289 | 367±207 | .139 |
| All | |||
| n | 87 | 89 | — |
| Mean diameter (mm) | 5.7±0.9 | 5.7±0.9 | .551 |
| Burst pressure (mm Hg) | 685±358 | 455±276 | <.001 |
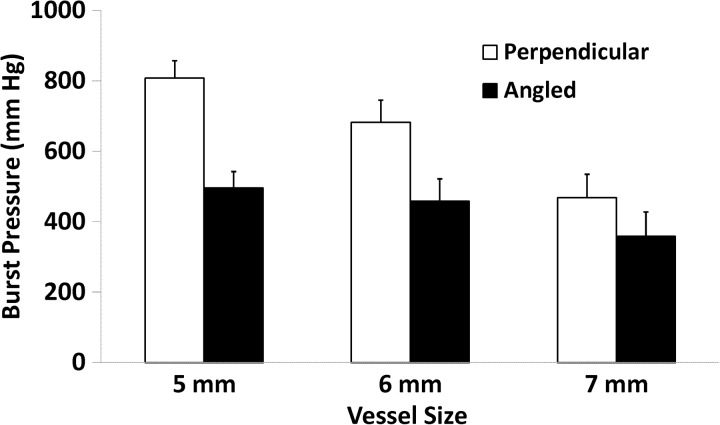
The perpendicular applications showed significantly higher burst pressures than the angled applications for both the 5-mm (P<.001) and 6-mm (P=.012) groups. Analysis of variance on all vessels showed significant differences in burst pressure among the vessel size groups (P<.001) and orientation (P<.001). The interaction between size and orientation was not significant (P=.225). Overall, the mean burst pressure was 51% higher in perpendicular (685±358 mm Hg) than angled (455±276 mm Hg) transections, with larger diameter vessels having lower burst pressures (Fig. 3). The mean burst pressure in 5-mm vessels sealed at a 45° angle was not different from that in 7-mm vessels sealed perpendicularly (498±295 and 484±289 mm Hg, respectively; P=.859).
FIG. 3.
Mean burst pressures for vessel diameter group and transection orientation. Error bars represent the standard error.
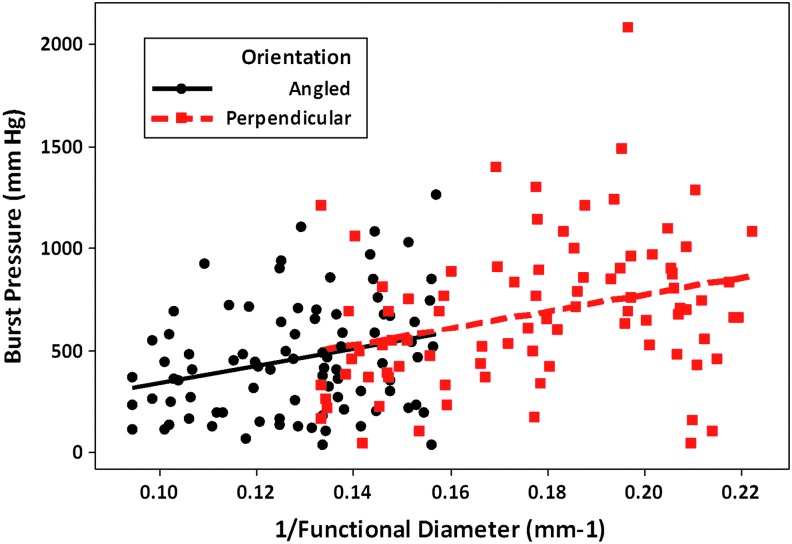
Analysis of covariance, as described in Materials and Methods, showed that the only significant factor was the inverse of the functional diameter (P<.001). Using the functional diameter instead of the nominal diameter, the orientation was not significant (P=.966), nor was there a significant interaction between the slope of the inverse of the functional diameter and the orientation (P=.997).
Discussion
According to LaPlace's law,7 the tension (T) of a blood vessel is proportional to the product of pressure (P) and radius (R): T∝P×R. Hence, vessels of larger diameter will be subjected to higher tensions at similar pressures and should be more likely to fail. This effect is commonly seen when sealing similar types of vessels of differing diameters. In a study of seven different arterial vessel sealing devices in pigs,2 the mean burst pressures declined from 846 mm Hg for 2–3-mm-diameter vessels to 764 mm Hg for 4–5-mm-diameter ones and 521 mm Hg for 6–7-mm-diameter ones. A similar study of four devices using both arteries and veins3 showed that burst pressures declined monotonically with vessel diameter: 466, 408, 307, and 38 mm Hg for vessel diameters of >0–3, >3–5, >5–7, and >7 mm, respectively.
When a vessel is sealed at an angle, the functional diameter is unintentionally increased (Fig. 1). An angled cross-section of a cylinder is an ellipse, the length of whose major axis is given by the nominal vessel diameter divided by the cosine of the cross-sectional angle. Because this axis will be greater than the nominal diameter of the vessel, per Laplace's Law, it will experience the highest tension and be most likely the point of failure. Hence, one may expect that vessels sealed at an angle will have lower bursting pressures than those sealed perpendicularly to the vessel's axis.
Ex vivo burst pressure testing is a common industry practice to demonstrate sealing effectiveness accepted by the Food and Drug Administration for regulatory submissions. Given that the pressures we observed are beyond those that can be induced in animal models, no direct correlation can be demonstrated between in vivo and ex vivo burst pressures. However, we believe the relationship between sealing angle and strength observed ex vivo will be similar to what occurs in vivo.
In this study, we confirmed that seal strength (i.e., burst pressure) decreases with increasing vessel diameter and that this decrease is observed irrespective of angle of seal. Mean burst pressures for both perpendicular and angled seals decreased as the vessel diameter of the groups increased from 5 mm to 6 mm and then 7 mm. What is novel in this study is the finding that vessels sealed perpendicularly are stronger than those sealed at a 45° angle to the blood vessel for similar diameters. For both the 5-mm and 6-mm groups, as well as overall, the perpendicular seals had significantly higher burst pressures than the angled seals.
The importance of this difference is demonstrated by comparison of burst pressures for a 7-mm perpendicular seal and a 5-mm angled seal. For a 45° angle, the increase in functional diameter is approximately 41%, so a 5-mm angled seal has a functional diameter of 7.07 mm. In fact, the burst pressures of 7-mm perpendicular and 5-mm angled seals were similar, indicating seal strength is substantially compromised by sealing at an angle rather than perpendicularly to the blood vessel.
The key factor in the difference in vessel strength between perpendicular and angled applications appears to be solely the functional diameter. As shown by the analysis of covariance, adjusting the burst pressure results by using the inverse of the functional diameter as a covariate completely explains the difference between orientations, and not some other inherent characteristic of angled versus perpendicular vessel sealing. The trend lines of the regression of burst pressure with the inverse of the functional diameter are similar for both perpendicular and angled applications (Fig. 4), indicating that the phenomenon regulating burst pressure is the same for both over a wide range of diameters (4.5–10.6 mm).
FIG. 4.
Burst pressure as a function of the inverse of the functional diameter with trend lines for angled and perpendicular applications.
Because the length of a perpendicular seal is the shortest possible for a given diameter vessel, these results suggest that the ideal approach is at a right angle to the vessel in order to optimize seal strength, at least for vessels 5 mm in diameter or greater. There are other important benefits to sealing vessels perpendicularly. Because the functional diameter is smallest for a perpendicular seal, it is easier to capture the vessel with a single purchase, leading to improved efficiency. The area exposed in a perpendicular seal is minimized in comparison with one at an angle, so sealing devices that impart heat should produce less collateral thermal damage. Finally, depending upon how compression is applied by the sealing device, reduction in the functional diameter of the vessel may result in more uniform compression and hence a higher-quality seal.
In vivo, a perpendicular approach to vessel sealing and transection is often not possible. This is especially true in laparoscopic or robotic procedures, where factors such as limited surgical space, difficult anatomical geography, and limited visibility of the device's end effector may prevent sealing at a right angle to the blood vessel. Technological improvements, such as articulation of the end effector, may provide the surgeon with the ability to form perpendicular seals of inherently higher strength in areas of difficult access. Currently available laparoscopic articulating devices have been successfully used in robotic applications but are hampered by their large size (8 mm in diameter) and lack of a cutting blade.8 For laparoscopic applications in general, articulation of an end effector could provide improved geometric access to blood vessels, ensuring the highest possible seal strength and quality.
In conclusion, blood vessels with diameters of 5 mm or greater sealed at an angle have significantly lower burst strength than those sealed perpendicularly to the vessel. This effect is explained by the larger functional diameter of angled applications compared with that of perpendicular ones. Articulation of the end effector, by enabling perpendicular application, may provide vessel sealing of higher strength, especially in laparoscopic procedures.
Acknowledgments
The study was funded by Ethicon Endo-Surgery, Inc., the manufacturer of the bipolar device tested.
Disclosure Statement
All authors are employees of Ethicon Endo-Surgery, Inc., a Johnson & Johnson Company.
References
- 1.Osborne MP. William Stewart Halsted; his life and contributions to surgery. Lancet Oncol. 2007;8:256–265. doi: 10.1016/S1470-2045(07)70076-1. [DOI] [PubMed] [Google Scholar]
- 2.Overhaus M. Schaefer N. Walgenbach K. Hirner A. Szyrach MN. Tolba RH. Efficiency and safety of bipolar vessel and tissue sealing in visceral surgery. Minim Invasive Ther Allied Technol. 2012;21:396–401. doi: 10.3109/13645706.2011.651145. [DOI] [PubMed] [Google Scholar]
- 3.Sigel B. Dunn MR. The mechanism of blood vessel closure by high frequency electrocoagulation. Surg Gynecol Obstet. 1965;121:823–831. [PubMed] [Google Scholar]
- 4.Newcomb WL. Hope WW. Schmelzer TM. Heath JJ. Norton HJ. Lincourt AE. Heniford BT. Iannitti DA. Comparison of blood vessel sealing among new electrosurgical and ultrasonic devices. Surg Endosc. 2009;23:90–96. doi: 10.1007/s00464-008-9932-x. [DOI] [PubMed] [Google Scholar]
- 5.Hruby GW. Marruffo FC. Durak E. Collins SM. Pierorazio P. Humphrey PA. Mansukhani MM. Landman J. Evaluation of surgical energy devices for vessel sealing and peripheral energy spread in a porcine model. J Urol. 2007;178:2689–2693. doi: 10.1016/j.juro.2007.07.121. [DOI] [PubMed] [Google Scholar]
- 6.ENSEAL® Instructions for Use. Cincinnati, OH: Ethicon Endo-Surgery, Inc.; 2011. [Google Scholar]
- 7.Schmidt-Nielsen K. Cambridge, UK: Cambridge University Press; 1990. Animal Physiology: Adaptation and Environment. [Google Scholar]
- 8.Meehan JJ. The robotic Gyrus PK: A new articulating thermal sealing device and a preliminary series report. J Laparoendosc Adv Surg Tech A. 2008;18:183–185. doi: 10.1089/lap.2007.0179. [DOI] [PubMed] [Google Scholar]