Abstract
Background:
Evidence-based practice (EBP) is one of the main professional competencies for health care professionals and a priority for medicine and nursing curriculum as well. EBP leads to improve effective and efficient care and patient outcomes. Nurse educators have responsibility to teach the future nurses, and an opportunity to promote patient outcomes. Therefore, the aim of this study was to describe nurse educators’ knowledge and attitude on EBP.
Materials and Methods:
This was a descriptive study conducted in nursing faculties of two major universities of medical sciences affiliated to Ministry of Health and Medical Sciences in Tehran, Iran. Data were gathered using a three-section questionnaire. Content and face validity was further enhanced by submitting it to nursing research and education experts. Statistical analysis was carried out using SPSS 11 software.
Results:
According the results, nursing faculties’ knowledge of EBP was mainly moderate (47.1%). Significant statistical relationship was found between the level of knowledge with education and teaching experience in different nursing programs. Nurses generally held positive attitudes toward EBP (88.6%) and there was no statistical significant relationship with demographic variables.
Conclusion:
Nursing educators are in a position to influence nursing research in clinical practice in the future. Therefore, it is critical to achieve implementation of EBP and be a change agent for a paradigm shift toward EBP.
Keywords: Attitude, evidence-based practice, Iran, knowledge
INTRODUCTION
Evidence-based practice (EBP) constitutes one of the professional qualities of healthcare personnel and is among the priorities of medical education programs, including nursing education.[1] In order to expedite the transfer of research findings to clinical practice, it is essential for nurses to acquire sufficient knowledge and skill and have strong faith in the crucial role of EBP in clinical settings. According to the results of a qualitative research in Iran, nurses have a positive attitude about the use of scientific evidence to guide practice.[2] However, nursing care system in Iran does not provide the incentive for nurses to engage in research and EBP.[3] EBP results in professional development of nurses’ capabilities and creates a new paradigm in nursing education. According to Melynk and Fineout-Overholt (2005), EBP provides a solution for reducing uncertainty in the sophisticated health care system and improves the quality of healthcare.[4] Estrabrooks et al. stated that this approach fills the gap between the evidences discovered by research and their application in clinics, thus enabling healthcare providers to offer quality services for patients and their families.[5] Grol (2000) believes that evidence-based nursing omits inefficient practices and implements effective approaches which eventually results in an appropriate and efficient care with an improved outcome for patients.[6]
Krugman (2003) states that establishing the culture of EBP is an essential plan for human resource development and believes that starting evidence-based activities would serve as a pioneer for shifting the culture to that end. According to her, changing the attitude and enhancing the knowledge of nurses is the first step toward establishment of EBP.[7] According to Melynk et al. acquiring knowledge about research methods, having the skill to evaluate research reports with a critic’s eye, and having a positive attitude toward evidence-based nursing are among methods that may enable overcome the obstacles hindering the application of research findings and thus will lead to improvement of healthcare quality.[8] McCleary and Brown (2002) conducted a study on 528 graduate nurses working in educational pediatric hospitals of Ontario, Canada, concerning the relationship between training of nurses for research and the implementation of evidence-based nursing, and they reported that the nurses’ knowledge of EBP and their positive attitude toward it will contribute to its implementation in healthcare system.[9] In Iran, the positive attitude toward EBP has been reported in clinical nurses[2,3] as well. However, none of them considered both the knowledge and attitude of EBP together.
Nursing faculties are in charge for training the future nurses, so their participation in integrating the EBP into clinical education will improve healthcare outcomes.[10] Therefore, they must involve themselves in clinical issues and approximate clinical, educational, and research activities through teaching EBP to students and nurses. It is evident that this requires instructors to have sufficient knowledge and positive attitude before involvement in this sophisticated practice.
Considering the novelty of the idea of EBP in Iranian medical and particularly nursing education, and few studies conducted about this issue, and it is mentionable that educators need to be committed to the principles of EBP, provide resources, and create a supportive environment for its implementation,[11] this study was conducted to investigate the Iranian nursing faculties’ knowledge and attitude on EBP.
MATERIALS AND METHODS
Design
This was a descriptive study conducted in two main nursing faculties in Tehran University of Medical Sciences, Tehran, Iran.
Participants
The study population were all nursing faculties providing clinical nursing education in two main nursing faculties in Tehran (N = 90). Finally, 70 questionnaires were completed, reflecting a response rate of 78%.
Data collection
A review of the literature recognized scales measuring knowledge and attitudes on EBP, developed for use in the health professions and staff nurses,[12] but not explicitly for nursing faculties. The research team developed a self-report questionnaire based on the researchers in the United States of America (USA).[13,14]
The questionnaire consisted of demographics and professional profile and two subscales. The demographics and professional profile included 10 questions. The knowledge of EBP subscale consists of 15 multiple choice and 10 matching questions. The attitudes toward EBP subscale comprised 17 items; however, there is some variation in the structure of the subscale responses.
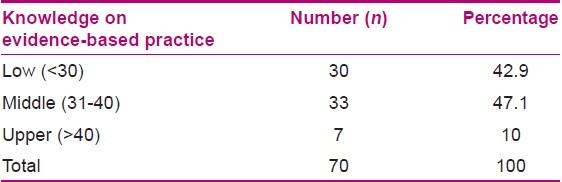
For measuring the knowledge of EBP subscale, each right and wrong answer was scored 2 and 0, respectively. The maximum score that could be obtained was 50. A total score of less than 30 was classified as low, 31-40 as moderate, and more than 40 as high [Table 1].
Table 1.
Nursing faculties’ knowledge on Evidence-based practice
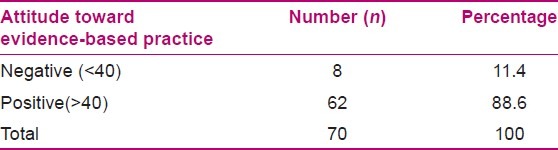
For measuring the attitude of EBP subscale, each item was prepared in a Likert’s scale from agree, no opinion to disagree. So, the greatest score that could be acquired was 51. A total score of less than 40 was classified as negative and more than 40 as positive.
Face and content validity for the tool was obtained by gathering the view points of 10 experts in the field. Test and retest was done for reliability purpose and a correlation coefficient of 0.76 was achieved. Koronbakh Alpha showed an internal consistency of 0.89.
Ethical considerations
Ethics committee of Tehran University of Medical Sciences approved the research proposal. Participants were informed regarding the study aims, confidentiality of the data, and the freedom to withdrawal and oral consent was obtained.
Data analysis
For data analysis, each section of the questionnaire was graded separately. The range of grades for the second section of the questionnaire (knowledge) was defined as high (75% or higher of questionnaire grades), moderate (50%-74% of questionnaire grades), and low (50% or less of questionnaire grades). Higher grades indicated higher knowledge. The grades obtained in the second section was categorized as less than 30 (low knowledge), 31-40 (moderate knowledge), and more than 40 (high knowledge).
None of the participants had chosen “No idea” for any question of the third section, the range of grading for the third section (Attitude) was divided in two groups: Grades of 40 and higher were defined as positive attitude and grades lower than 40 were defined as negative attitude.
After merging the average and high levels due to their low frequency, the Fisher’s exact test was used to analyze the relationship between demographic features of the units under study and the level of knowledge of the faculties regarding EBP.
RESULTS
Nurse faculties were predominantly female (82.9%) with M.Sc. degree (91.4%). PhD degrees were held by 8.6% of the sample, and none had a B.Sc. degree. Their ages ranged between 30 and 55 years with a mean of 46.44 years [standard deviation (SD) 4.45]. Years of work experience as a faculty ranged from 11 to 20 (mean 15, SD 5.8). Nurse faculties that were teaching in B.Sc. level (20%), in both B.Sc. and M.Sc. levels (71.4%). Only 8.6% of the participants had teaching experiences in PhD level. According to the responses, approximately 87.1% indicated that they were not teaching EBP and more than one half of the respondents (51.6%) had never been trained in EBP workshops or through continuing education programs.
Knowledge and Evidence-based practice
The majority of respondents (60%) were partially aware of EBP and just a few numbers (N = 5) had not previously heard this term. More than half of the respondents (61.4%) were unaware of Cochrane collaboration as a source of information about EBP. The respondents felt that they were knowledgeable about the research strategies (71.4%). More than 80% of their knowledge about the terms such as “relative risks,” “odds ratio,” “confidence interval,” and “systematic bias” was in a low level. Participants scored themselves low on the ability to present a correct definition of EBP as well. In general, the majority of the nurse faculties were in a moderate level of knowledge toward EBP [Table 1]. Table 2 outlines the results of statistical tests for the relationship between nurse faculties’ demographic features and their knowledge to EBP.
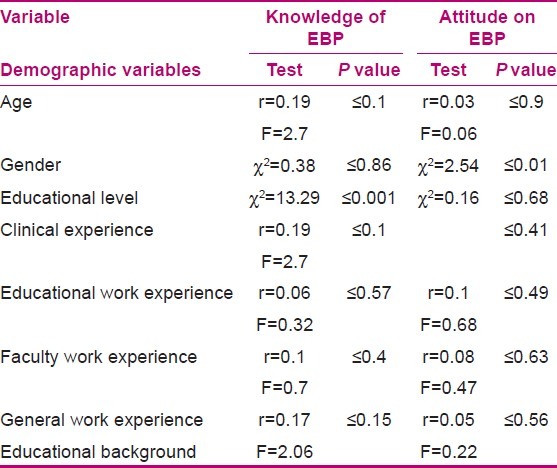
Table 2.
Nursing faculties attitude toward Evidence-based practice
The findings indicated a significant statistical relationship between the knowledge of nursing faculty members and such variables as level of education (χ2 = 13.29, P ≤ 0.001) and educational background in different levels of nursing (χ2 = 22.41, P ≤ 0.001). However, no significant statistical relationship was observed for age, work experience, participation in research paper criticism sessions, and participation and teaching in EBP workshops [Table 2].
Attitude and Evidence-based practice
As for the attitude of faculty members toward EBP, the findings indicate that 80% of members believed EBP is helpful in making clinical decisions, and 81.4% were inclined to implement EBP in their clinical education. Nonetheless, 57.1% believed that EBP is not consistent with the present facts of Iranian nursing community and thus not feasible to implement. The general outline of the findings indicates a positive attitude of the majority of participants (88.6%) toward EBP [Table 2]. The mean grade of attitude towards EBP is 45.79 with a SD of 5.39, having 32 as minimum and 51 as maximum grade.
Our data analysis indicated no significant statistical relationship between the most of demographic features of the participants and their attitude toward EBP [Table 3].
Table 3.
Relationship between demographic features and nursing faculties’ knowledge and attitude on Evidence-based practice
DISCUSSION
Despite having positive attitude the majority of nursing faculties had an average level of knowledge. Moreover, 60% stated that they are aware of the concept of EBP only “to some extent,” whereas nursing teachers (who have at least a Master’s degree in the field, have been trained about research methodology and are probably teachers of research methods) are expected to be sufficiently aware of this concept and to have acquired appropriate skills. This finding reflects the not-so-strong provision of EBP approach in faculty members. Considering the fact that more than 70% of participants were familiar with techniques of searching literature, it appears that they had no difficulty in accessing research methods and results, while the McColl et al. study (1998) reported only 16% of physicians in England to have received official education regarding literature search techniques.[15] Similarly, our findings indicate that the nurse faculties are not familiar with technical terms used in evaluation of research articles, such as odds ratio, relative risk, and confidence interval. Other studies have corroborated this lack of knowledge regarding technical terms of research, as well.[16] Furthermore, only about half of the respondents in this study had acquired their knowledge of EBP through participating in activities such as workshops, seminars, and conferences. Since Jette et al., depicted that educational sessions of EBP and teaching literature search techniques improve the knowledge of physiotherapists,[16] it appears that supporting these sessions and educational programs would be essential in improving the methods of using resources and databases for acquiring up-to-date knowledge.
The findings of our study indicated that a great number of participants were familiar with the techniques of literature search; however, they did not use the Cochrane database and systematic review articles as sources of evidence. These findings are in line with those of Melynk et al. reporting 68% of nurses not to use the Cochrane database.[17] In contrast, Kamwendok (2002) reported most Swedish rehabilitation specialists (70%) to use up-to-date sources and databases in their clinical practice.[18] Considering the availability of internet and databases in most nursing universities, nursing teachers of any rank and professional status are expected to show greater attention to this issue, as Thomas (1998) believes nursing teachers to be responsible for educating nurses who are going to perform EBP.[19] These teachers should serve as a role model for nursing students during both theoretical and practical education and must establish the base of EBP. Ciliska (2005) stated that unless instructors teach EBP, the students and consequently nurses will never manage to base their services on evidences.[20]
Our findings also indicated a significant relationship between the level of knowledge of nursing faculty members concerning the EBP and variables such as level of education and experience of teaching in different levels of nursing education, while it was not observed to be significantly related to other personal features. These are not consistent with those of Jette et al., who stated that participating in educational sessions, whether during practical training or in ongoing educational programs, is related to the participants’ knowledge of technical terms and the concept of EBP.[16] However, they reported that knowledge and skills of retrieving information critically are related to the level of education, which is similar to our findings. Comparing the findings of these two studies indicates that nursing educational programs highlighting EBP have not been conducted in Iran during the recent years.
Most respondents in our study had a positive attitude toward EBP, which is similar to the results of other studies conducted on the attitude of nurses and other healthcare personnel toward this issue.[21,22] Our participants believed that EBP is essential for both nursing clinical practice and education, because EBP using the up-to-date scientific findings will improve the quality of care for patients. Similarly, Mc Ewen (2002) stated that nursing teachers and students believe that EBP fills the gap between research, theory, and practice.[23] Furthermore, this finding is consistent with similar studies conducted on physicians, rehab specialists, and clinical nurses.[3,16,24,25] 94% of American pediatricians strongly believed that using guidelines of clinical practice will motivate them for improving patient care[28] and 70% of Iranian nurses in hospitals of Tehran University of Medical Sciences had a positive attitude toward using research evidences in clinical practice.[3]
Participants in our study were not sure whether the current research evidences will aid them in clinical decision making for patient care (37.1%). According to them, EBP may impose some limitations on education and practice and is not feasible in the present status of Iranian nursing community (57.1%). Similarly, statements of British physicians in a qualitative study[26] and clinical nurses in Iran[3] indicated that they doubted the application of current clinical guidelines and research evidences to clinical practice and believed research findings to be unrelated to some patients. The participants in our study probably believe that research studies are not compatible with clinical situations. In addition, our participants had a broad range of beliefs from approval to disapproval concerning the existence of research evidences to confirm the interventions they perform for patient care. These mixed responses combining agreement and disapproval for EBP reinforce this idea that implementing EBP requires researches to be better focused on clinical activities and answering clinical questions.
Most participants in our study believed that EBP can improve the quality of patient care and declared that they are inclined to learn and develop skills necessary for implementing EBP in their clinical education. This is in line with previous studies.[21,22] In another study by McColl et al., most physicians had responded positively to EBP, and they used clinical guidelines and standard cares in their clinical activities.[19] In another qualitative study,[29] many statements indicated that inclination toward EBP is related to implementing it in practice. In that study, expressions such as “stress,” “difficult and demanding,” “dangers and risks,” and “nuisance” were used by participants to describe EBP; the authors stated that despite using the above expressions, the participating physicians were inclined to use evidence-based interventions.[25]
Lack of significant relationship between the demographic features of participants and their attitude toward EBP is not in line with the findings of Jette et al. (2003), who reported that the attitude of younger practitioners with less work experience is more positive compared to older participants with longer years of experience.[16] As for the level of education, a study by Olade (2003) indicated Finnish nurses with higher levels of education to have a more positive attitude toward using research evidences in practice.[27] Ultimately, more focused interventions are required to reinforce the attitude of nurses in order to enhance their motivation and desire to learn and commit to EBP. Thus, it appears that the positive mentality of Iranian nurses, particularly those in the nursing education systems, has provided a suitable opportunity for “evidence-based practice” to be included in nursing practices.
Using convenience sampling with limited number of samples is the main limitation of our study, so more extensive studies are needed in order to generalize the findings.
CONCLUSION
Respondents established that the use of evidence in practice was essential, and they had a positive attitude toward EBP. They believed that quality of patient care was improved when evidence was used in practice. Nursing faculties were interested in improving the skills necessary to implement EBP. Despite of their low-level knowledge, they declared that they needed to increase the use of evidence in their daily practice.
Considering their positive attitude on EBP, it seems that nursing faculties are emotionally prepared for capturing the required knowledge toward EBP. This leads nursing education policy makers to use this opportunity and move toward promoting EBP paradigm.
ACKNOWLEDGEMENTS
The authors would like to thank the Center for Nursing Care Research (CNCR), Tehran University of Medical Sciences, for funding this research project
Footnotes
Source of Support: Tehran University of medical Sciences, Center for Nursing Care Research
Conflict of Interest: None.
REFERENCES
- 1.Greiner A, Knebel E. Health professions education: A bridge to quality. Washington, DC: National Academies Press; 2003. [PubMed] [Google Scholar]
- 2.Adib-Hajbaghery M. Evidence-based practice: Iranian nurses’ perceptions. Worldviews Evid Based Nurs. 2009;6:93–101. doi: 10.1111/j.1741-6787.2009.00149.x. [DOI] [PubMed] [Google Scholar]
- 3.Mehrdad N, Salsali M, Kazemnejad A. The spectrum of barriers to and facilitators of research utilization in Iranian nursing. J Clin Nurs. 2008;17:2194–202. doi: 10.1111/j.1365-2702.2007.02040.x. [DOI] [PubMed] [Google Scholar]
- 4.Melynk B, Fineout-Overholt E. Evidence-based practice in nursing and health care: A guide to best practice. Philadelphia, PA: Lippincott, Williams and Wilkins; 2005. [Google Scholar]
- 5.Estrabrooks CA, Wallin L, Milner M. Measuring Knowledge Utilization in Health Care. Int J Policy Evaluation Manag. 2003;1:3–36. [Google Scholar]
- 6.Grol R. Between evidence based practice and total quality management: The implement of cost-effective care. Int J Qual health care. 2000;12:297–304. doi: 10.1093/intqhc/12.4.297. [DOI] [PubMed] [Google Scholar]
- 7.Krugman M. Evidence-based practice: The role of Staff Development. J Nurses Staff Dev. 2003;19:279–85. doi: 10.1097/00124645-200311000-00003. [DOI] [PubMed] [Google Scholar]
- 8.Melynk B, Fineout-Overholt E, Stone P, Ackerman M. Evidence-Based Practice: The past, the present and Recommendations for the Millennium. Pediatr Nurs. 2000;26:77–80. [PubMed] [Google Scholar]
- 9.McCleary L, Brown T. Research utilization among pediatric health professionals. Nurs Health Sci. 2002;4:163–71. doi: 10.1046/j.1442-2018.2002.00124.x. [DOI] [PubMed] [Google Scholar]
- 10.Penz KL, Bassendowski SL. Evidence-Based Nursing in Clinical Practice: Implication for Nurse Educators. J Cont Educ Nurs. 2006:37. doi: 10.3928/00220124-20061101-03. [DOI] [PubMed] [Google Scholar]
- 11.Adib-Hajbaghery M. Factors facilitating and inhibiting evidence-based nursing in Iran. J Adv Nurs. 2007;58:566–75. doi: 10.1111/j.1365-2648.2007.04253.x. [DOI] [PubMed] [Google Scholar]
- 12.Melnyk BM, Fineout-Overholt E, Mays MZ. The evidence-based practice beliefs and implementation scales: Psychometric properties of two new instruments. Worldviews Evid Based Nurs. 2008;4:208–16. doi: 10.1111/j.1741-6787.2008.00126.x. [DOI] [PubMed] [Google Scholar]
- 13.Upton D, Upton P. Development of an evidence-based practice questionnaire for nurses. J Adv Nurs. 2006;54:454–8. doi: 10.1111/j.1365-2648.2006.03739.x. [DOI] [PubMed] [Google Scholar]
- 14.Aarons GA. Mental health provider attitudes toward adoption of evidence based practice: The evidence-based practice attitude scale (EBPAS) Ment Health Serv Res. 2004;6:61–74. doi: 10.1023/b:mhsr.0000024351.12294.65. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.McColl A, Smith H, White P, Field J. General practitioners perception of the route to evidence-based medicine: A questionnaire survey. Br Med J. 1998;316:361–5. doi: 10.1136/bmj.316.7128.361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Jette DU, Bacon K, Batty C, Carlson M, Ferland A, Hemingway RD, et al. Evidence-based practice: Beliefs, attitudes, knowledge, and behaviors of physical therapists. J Am Phys Ther. 2003;83:786–805. [PubMed] [Google Scholar]
- 17.Melynk Bernadette M, Overholt Ellen F, Feinstein Nancy F, Hong Li, Small L, Wilcox L, et al. Nurses’ Perceived Knowledge, Beliefs, Skills and Need Regarding Evidence-Based Practice: Implications for Accelerating the Paradigm Shift. Worldviews Evid Based Nurs. 2004:185–193. doi: 10.1111/j.1524-475X.2004.04024.x. [DOI] [PubMed] [Google Scholar]
- 18.Kamwendo K. What does Swedish physiotherapist feel about research. A survey of perceptions, attitudes, intentions and engagement? Physiother Res Int. 2002;7:23–34. doi: 10.1002/pri.238. [DOI] [PubMed] [Google Scholar]
- 19.Thomas E. The role of nurse lecturers in the utilization of research findings in practice. Development of professional practice research training fellowships: Occasional papers. Health Professional Wales, University of Wales College of Medicine. 1998 [Google Scholar]
- 20.Ciliska D. Education for Evidence-Based Practice. J Prof Nurs. 2005;21:345–50. doi: 10.1016/j.profnurs.2005.10.008. [DOI] [PubMed] [Google Scholar]
- 21.Stevenson K, Lewis M, Hay E. Do physiotherapists’ attitudes toward evidence-based practice change as a result of an educational program? J Eval Clin Pract. 2004;10:207–17. doi: 10.1111/j.1365-2753.2003.00479.x. [DOI] [PubMed] [Google Scholar]
- 22.Metcalfe C. Barriers to implementing the evidence base in four NHS therapies (Dietitian, Occupational therapist, and Physiotherapist, Speech and language therapist) Physiotherapy. 2001;87:433–41. [Google Scholar]
- 23.McEwen M. Application of theory in nursing practice. In: McEwen M, Wills EM, editors. Theoretical basis for nursing. Philadelphia: Lippincott, Williams and Wilkins; 2002. pp. 347–67. [Google Scholar]
- 24.Flores G, Lee M, Bauchner H, Kastner B. Pediatricians’ attitudes, beliefs and practices regarding clinical practice guidelines: A national survey. Pediatr. 2000;105:496–501. doi: 10.1542/peds.105.3.496. [DOI] [PubMed] [Google Scholar]
- 25.Freeman AC, Sweeney K. Why general practitioners do not implement evidence: Qualitative study. Br Med J. 2001;323:1100–2. doi: 10.1136/bmj.323.7321.1100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Cranney M, Warren E, Barton S. Why do GPs not implement evidence-based guidelines? A descriptive study. Fam Practitionaire. 2001;18:359–63. doi: 10.1093/fampra/18.4.359. [DOI] [PubMed] [Google Scholar]
- 27.Olade R. Attitudes and factors affecting research utilization. Nurs Forum. 2003:5–15. doi: 10.1111/j.0029-6473.2003.00005.x. [DOI] [PubMed] [Google Scholar]


