Abstract
Background:
Cardiac syndrome X is a relatively common disorder, and still not much is known about the causative factors or its pathophysiology, which makes it difficult to cure. Due to its chronic nature and debilitating symptoms, many patients have significantly reduced quality of life (QOL).The purpose of this study was to assess the impact of phase III cardiac rehabilitation (CR) and relaxation on the QOL of patients.
Materials and Methods:
This research is a randomized clinical trial study. Forty eligible and consenting women (age 30-65 years) were randomly assigned to four groups. In the first group (n = 11), progressive muscle relaxation (PMR); in the second group (n = 11), phase III CR; and in the third group (n = 11), PMR along with phase III CR were performed for 8 weeks at home. The fourth group (n = 7) was used as the control group. Short form of QOL questionnaire (SF-36) was used for data gathering. Data analysis was performed using χ2, Kruskal-Wallis, and rank sum difference tests.
Results:
After phase III CR, relaxation, and combination of CR and relaxation, patients demonstrated improved QOL (P < 0.001). The results of post-test multiple comparisons showed that there were statistically significant differences between control and all intervention groups (P < 0.05). There was also statistically significant difference between relaxation and combination of phase III CR and relaxation groups (P < 0.5).
Conclusions:
An 8-week phase III CR program together with relaxation improved QOL of patients with cardiac syndrome X. We suggest phase III CR program together with relaxation as an effective treatment in these patients.
Keywords: Cardiac syndrome X, Iran, muscle relaxation, quality of life
INTRODUCTION
Kemp introduced the term “cardiac syndrome X” (CSX) in 1973 to describe patients with the triad of angina pectoris, positive exercise test, and normal coronary angiogram.[1] Although there is no accurate statistics about the prevalence of this syndrome, approximately 10-30% of patients with angina pectoris symptoms undergoing coronary angiography have normal or near-normal coronary arteries and are considered to be suffering from CSX.[2,3] CSX is more common in women than men, so 70% of patients with CSX are at the perimenopausal age.[4] Limited studies have been conducted on the CSX in Iran and its prevalence has been reported to range between 16.4% and 26.3%.[5–7]
Chest pain is an important symptom of CSX that causes patients to refer to a physician and hospital, and is frequently indistinguishable from the symptoms of acute myocardial infarction.[8] Chest pain may be debilitating, so about 50% of patients have functional limitations in activities of daily living, 50% lose their jobs, and 75% frequently go to physician for refractory chest pain.[9] Severity and frequency of chest pain has a direct impact on the quality of life of patients with CSX.[10] Due to its unknown etiology, treatment of CSX is a major challenge for both patients and physicians. Therefore, decreasing the symptoms and improving the quality of life are the important treating goals in these patients.[3]
During recent decades, interest in evaluating and improving the quality of life of patients with chronic illness has considerably increased, so it is vital to improve daily life activities and quality of life in patients with chronic illness.[11] Clinical trial results showed that quality of life can be an indicator of quality of health care, that is considered as a part of treatment program. In addition, its measurement can be a useful guide for improving care in chronic illness. Awareness about the quality of life of patients will help nurses, as a member of health care team, to deliver nursing care in order to improve patients’ quality of life.[12]
Preliminary studies have suggested that aerobic exercises, especially if applied with relaxation techniques, may have a positive effect on subjective symptoms, dyspnea, duration of pain, and quality of life of patients with CSX.[13,14] However, patients with CSX may refrain from doing physical activities because of fear of onset of chest pain or its aggravation. This reduced level of activity may result in loss of body fitness and functional limitations, which may produce a vicious cycle of pain and inactivity. Since the beneficial effects of exercise have been demonstrated both in healthy individuals and in different groups of patients, it is possible that exercise breaks the cycle of pain and inactivity in patients with CSX.[15]
Nowadays psychological methods are used either singly or in combination with other methods in treatment of chronic pain. The beneficial effect of relaxation are reduction of heart rate; decreased anxiety and angina pectoris; increased return to work; and lower mortality rate in patients with myocardial infarction.[16] It is possible that psychological treatments can be useful in patients with CSX, particularly if these interventions are initiated shortly after diagnosis.[17]
Nowadays great emphasis is laid on the use of complementary therapies in health systems. The use of easy and cost-effective, non-pharmacological methods for pain management and quality of life improvement in patients with CSX may have positive social, economic, and personal outcomes. Thus, the purpose of this study was to determine the effects of cardiac rehabilitation and relaxation on the quality of life of patients with CSX.
MATERIALS AND METHODS
This study was a randomized clinical trial. The study population comprised all women with CSX. In this study, women with chest pain, positive exercise test, or positive myocardial perfusion imaging for ischemia, and normal coronary angiogram were considered as CSX. Other inclusion criteria were: Age 30-65 years; absence of myocardial disease, left ventricular hypertrophy, and valvular disease; ejection fraction more than 50%; not smoking before entering the study; no history of psychiatric illness, any musculoskeletal or psychological condition for which exercise is contraindicated; non-participation in any exercise relaxation or meditation programs during the past 6 months.
Initially 114 eligible samples were selected from hospitalized patients who underwent coronary angiography from April 2010 to October 2012 in Sayyed-o-Shohada and Talegani hospitals, Urmia, Iran. Forty of those patients were willing to participate in this study, who were randomly assigned to four groups [7 patient in the control group, 11 patients in cardiac rehabilitation (CR) group, 11 patients in the progressive muscle relaxation (PMR) group, and 11 patients in the group in which CR and PMR are combined (CR and PMR)].
The study was approved by local ethics committee. Written informed consents were obtained from all patients. Coded questionnaires were distributed to all subjects. Current treatment of patients continued under the supervision of a cardiologist. After completion of the study, an optional training session was held for the participants of the control group.
One or two face-to-face training sessions were held for patients of intervention groups, and each session lasted 60-90 min. Jacobson’s progressive muscle relaxation method (16-muscle groups’ relaxation) was taught to patients in PMR, and CR and PMR groups. Jacobson’s 16 different muscle groups relaxation technique is one of the progressive muscle relaxation techniques which have been described carefully by Bernstein and Borkovec in 1973. Muscles of the body were divided into 16 groups as follows: Dominant hand and forearm; dominant upper arm; non-dominant hand and forearm; non-dominant upper arm; forehead; upper cheeks and nose; lower face; neck; chest, shoulders, upper back; abdomen; dominant upper leg; dominant calf; dominant foot; non-dominant upper leg; non-dominant calf; and non-dominant foot.[18] The researcher gave training on how to perform the relaxation. Then, the patients were asked to demonstrate the technique to the researcher. PMR group and CR and PMR group performed progressive muscle relaxation program based on Jacobson’s method, 15 min daily at home. Educational pamphlet and audio CDs were given to the patients for better learning and effective implementation of the relaxation techniques at home.
Aerobic exercise (according to phase III cardiac rehabilitation) was taught to patients in CR group and CR and PMR group. Training sessions included stretching exercises, walking (including education of the frequency, duration, and intensity of walking), pulse controls in allowable range, and some points on benefits of walking. Each exercise session consisted of three parts: Warm-up, walking at the intensity of 60-65% of allowable maximum heart rate, and cool down. Duration of exercise sessions began from 25 min and at the end of 8 weeks was increased to 40 min at every turn. CR group and CR and PMR group performed phase III CR exercise program, three times per week. Heart rate monitoring was performed using a heart rate monitor (Beurer PM45). At the end of training sessions, a pamphlet and a CD of stretching exercises were provided to patients. The patients in intervention groups did the training given for 8 weeks. During this period, the patients were followed up weekly by telephone calls, and phone number of the researcher was given to the patients to conta ct in emergency. All subjects completed the data-collecting questionnaire before and after the intervention.
Data were gathered through short form of quality of life (QOL) (SF-36) questionnaire and a demographic questionnaire. SF-36 includes 36 questions and eight dimensions as follows: General health (6 items), physical functioning (10 items), physical role limitation (4 items), pain (2 items), emotional role limitation (3 items), social functioning (2 items), vitality (4 items), and mental health (5 items). All questions are scored on a scale from 0 to 100, with 100 representing the highest level of functioning possible. The scores from those questions that address each specific area of functional health status are then averaged together, for a final score within each of eight dimensions measured.
SF-36 is a standardized questionnaire, which has been used in numero us studies in Iran and its reliability and validity for Iranian population approved by Montazeri et al. (2005). A known group comparison and convergent validity were used to ensure validity. Reliability of the questionnaire was confirmed by internal consistency (Cronbach’s alpha 0.71-0.90).[19]
Statistical analysis was performed using SPSS 16 software. The data were analyzed using Kruskall-Wallis test to compare groups. Then the rank sum difference test was used for multiple comparisons to determine the difference between groups. Comparisons of qualitative data were performed using χ2 test. The significance was set at the level of 5% (P < 0.05).
RESULTS
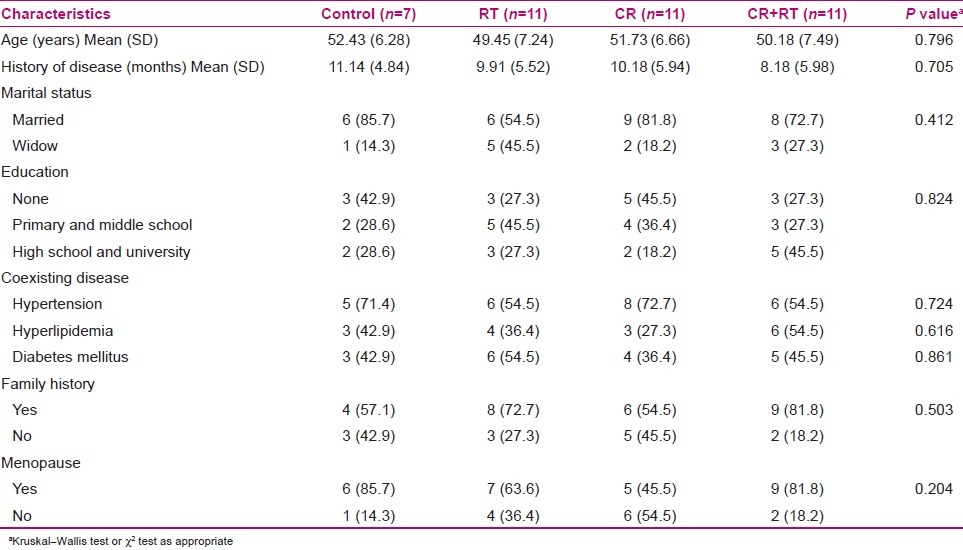
Out of 40 individuals studied, 27 (67.5%) were menopausal at the study time. The mean (SD) age of patients in control, PMR, CR, and CR and PMR groups were 52.43 (6.28), 49.45 (7.24), 51.73 (6.66), and 50.18 (7.49), respectively [Table 1].
Table 1.
Comparison of demographic characteristics of study patients in the four groups
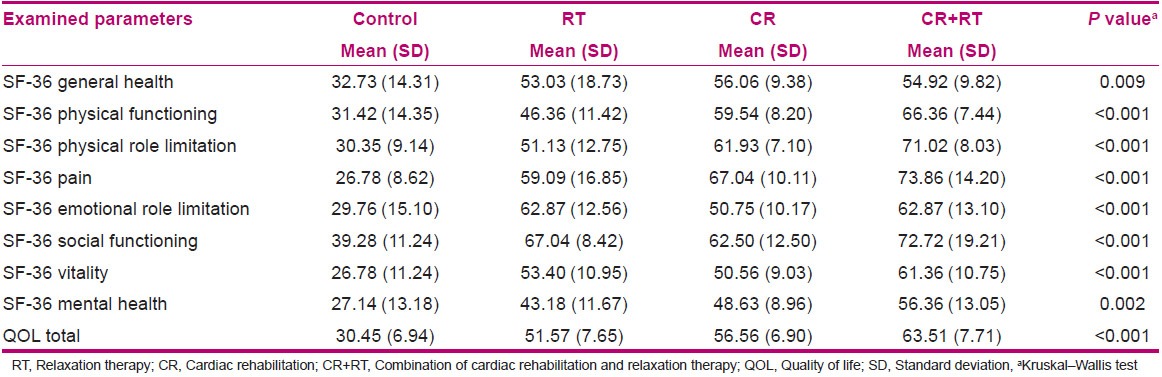
Kruskal-Wallis test results showed that there were no significant differences between the four groups in terms of general health, physical functioning, physical role limitation, pain, emotional role limitation, social functioning, vitality, and mental health before the intervention (P < 0.05) [Table 2]. But after the intervention, there were significant differences in scores between the four groups (P < 0.001) [Table 3]. The rank sum difference test was used for multiple comparisons to determine the difference within and between groups.
Table 2.
Comparison of quality of life of dimensions and total score before intervention in the four groups
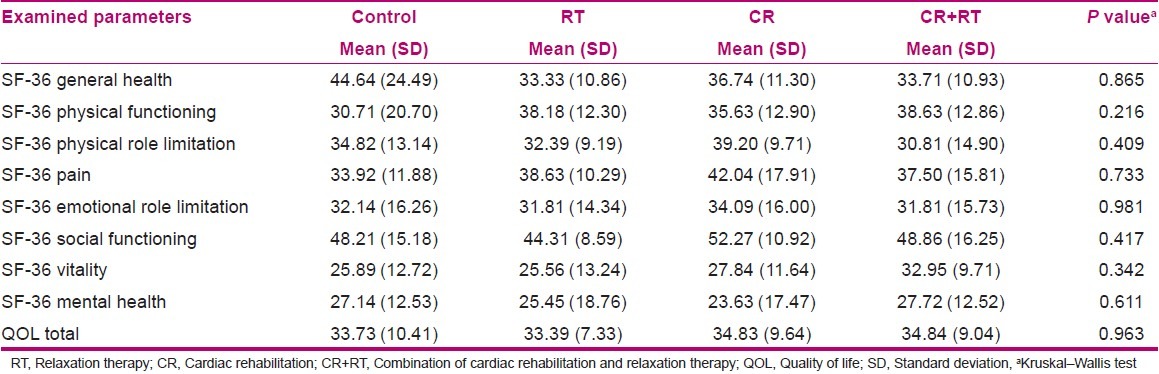
Table 3.
Comparison of quality of life of dimensions and total score after intervention in the four groups
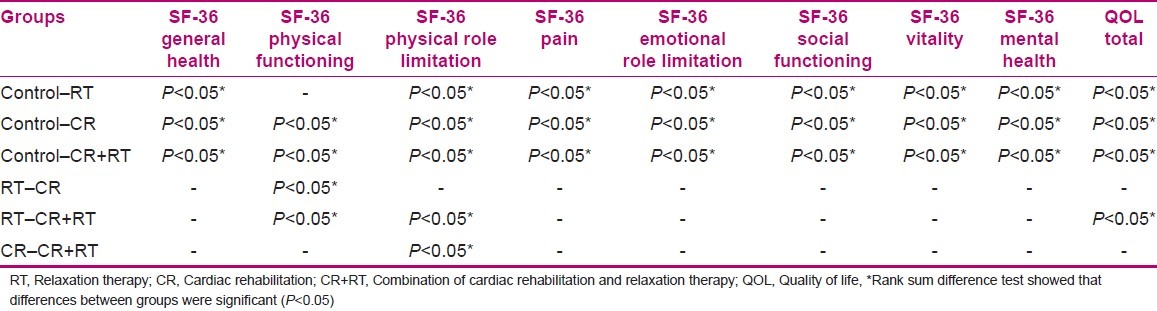
After the intervention, the results showed that there were significant differences between the three intervention groups and the control group in all dimensions of QOL except physical functioning (P < 0.05). There were no significant differences between PMR group and control group in terms of physical functioning (P > 0.05). There were no significant differences among the three intervention groups in terms of general health, pain, emotional role limitation, social functioning, vitality, and mental health (P > 0.05). There were significant differences in physical functioning in the PMR group as compared with the CR group and CR and PMR group (P < 0.05). There were also significant differences in physical role limitation in CR and PMR group as compared with CR group and PMR group (P < 0.05) [Table 4].
Table 4.
Multiple comparisons difference pre-test of post-test quality of life of dimensions and total score between the four groups
Kruskal-Wallis test results showed that there were no significant differences between the four groups in terms of QOL total scores before the intervention (P = 0.963) [Table 2]. But after the intervention, there were significant differences in scores between the four groups (P < 0.001) [Table 3]. The rank sum difference test was used for multiple comparisons to determine the difference within and between groups.
The results showed that after the intervention, there were significant differences between the three intervention groups and the control group. Moreover, there were significant differences between PMR group and CR and PMR group in QOL total scores (P < 0.05) [Table 4].
DISCUSSION
Results of the present study showed that progressive muscle relaxation improved the total QOL and all tits dimensions except physical functioning in the PMR group as compared to the control group. This is in agreement with the study by Asbury et al. (2009) in which it was found that autogenic training (one method of relaxation) may improve the QOL and psychological well-being in women with CSX.[20] Tyni-lenne et al. (2002) investigated the effects of physical training and relaxation therapy on the QOL and exercise capacity in women with CSX and found that the relaxation improved health-related QOL in the relaxation group.[21] Cunningam et al. (2000) also showed that after the intervention, transcendental meditation increased QOL of patients with CSX.[22]
The results of the present study showed that cardiac rehabilitation improved the QOL and all its dimensions in the CR group as compared with the control group.
Tyni-lenne et al. (2002) in their study demonstrated that the exercise improved health-related QOL in the exercise group.[21] Asbury et al. (2008) in their study evaluated the impact of phase III CR exercise program on QOL in women with CSX and showed that CR improved QOL in intervention group as compared with the control group. But unlike the results of this study, CR only improved four dimensions of QOL, including general health, physical functioning, pain, and vitality, in the intervention group.[23] This difference may be a result of more exercise sessions (three times per week) in our study. On the other hand, this difference may be due to complex, multidimensional, and dynamic structure, and subjective nature of QOL. Findings of a review study showed that the effects of exercise-based rehabilitation programs in terms of overall reduction in adverse clinical outcomes are similar to those of comprehensive cardiac rehabilitation programs after myocardial infarction.[24]
Results of the present study showed that cardiac rehabilitation along with relaxation improved the QOL and all its dimensions in the CR group as compared with the control group. We could not find any studies that investigated the effect of CR along with relaxation on QOL in patients with CSX. However, Asbury et al. (2011), in their study regarding the impact of group support on QOL in women with CSX, showed that participation in a support group (exercise training, relaxation, diet, and meditation) only improved the vitality demission of QOL and had no effect on the total QOL score in the intervention group as compared with the control group.[25]
Difference between the intervention groups in terms of QOL and its dimensions analyzed using the method of multiple comparisons showed that there were no statistically significant differences between the three intervention groups in six dimensions of QOL, including general health, pain, emotional role limitation, social functioning, vitality, and mental health. In the dimension of physical functioning, the results showed that cardiac rehabilitation and cardiac rehabilitation along with relaxation significantly improved the QOL, as compared with relaxation. In addition, results showed that cardiac rehabilitation along with relaxation significantly improved physical role limitations, as compared with relaxation and cardiac rehabilitation alone.
Multiple comparison results showed a significant improvement of QOL in the three intervention groups as compared with control group, but cardiac rehabilitation along with relaxation improved the QOL better than relaxation and cardiac rehabilitation alone. In addition, this difference was statistically significant between CR and PMR group and PMR group.
Tyni-lenne et al. (2002) found that exercise and relaxation improved the QOL as compared to control group, but there was no significant difference between the two interventions. These findings are consistent with the results of this study.[21]
Based on aforementioned findings, we can say that although all three methods of PMR, CR, and CR along with PMR improved the QOL and its dimensions, CR along with PMR improved the QOL of women with CSX better. More extensive studies should be conducted with larger sample size to reach decisive conclusions. Looking at the results, we found that relaxation training on psychological dimensions and exercise on physical dimensions of QOL have a greater effect, although the effects of relaxation training on physical dimensions and exercise on psychological dimensions of QOL are also highlighted.
Two limitations need to be addressed regarding the present study. The first limitation concerned the small sample size and the second limitation was the lack of direct observation of the techniques taught to the intervention groups at home. However, considering that the subjects participated voluntarily in the study and had a high level of motivation to control their symptoms, we expected that they performed the taught techniques. The findings of this study also confirm our conclusion.
CONCLUSION
Although in some instances, there were no statistically significant differences among groups on the measured variables (QOL and its dimensions), in general, CR along with relaxation improved QOL of women with CSX. Improvement of QOL of patients with CSX may reduce morbidity and physical, psychological, and social limitations, and strengthen their coping with the disease. According to the results of this study, health care providers can use interventions such as exercise and relaxation in the management of CXS.
Nurses, because of great experience and skill in providing care and educating the patients, can help them to follow their activities such as exercise and relaxation programs.
On the other hand, the home-based rehabilitation is a part of community-based rehabilitation programs which may resolve some barriers (rehabilitation centers being far from patient’s house and high costs of the programs) of patients’ compliance with the programs.
Finally, we recommend further studies to evaluate the effect of exercise with varying severity and frequency and different kinds of relaxation techniques on the QOL of patients with CSX.
ACKNOWLEDGMENTS
The authors acknowledge the Vice-Chancellery of Research and Technology, Urmia University of Medical Sciences, which approved and financially supported this project, and thank all staffs and directors in Sayyed-o-Shohada and Talegani hospitals and also would like to thank all the patients who participated in this study for their sincere cooperation.
Footnotes
Source of Support: Urmia University of Medical Sciences
Conflict of Interest: None.
REFERENCES
- 1.Merz C, Etiba W, Pepine CJ, Jabnson BD, Shaw LJ, Kelsey SF. Cardiac syndrome X: Relation to microvascular angina and other conditions. Curr Cardiovasc Risk Rep. 2007;1:167–75. [Google Scholar]
- 2.Lanza G. Cardiac syndrome X: A critical overview and future perspectives. Heart. 2007;93:159–66. doi: 10.1136/hrt.2005.067330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Slobody PR. Cardiac syndrome x: A brief overview for nurses. Dimens Crit Care Nurs. 2008;27:209–12. doi: 10.1097/01.DCC.0000325076.47670.50. [DOI] [PubMed] [Google Scholar]
- 4.Singh M, Singh S, Arora R, Khosla S. Cardiac syndrome X: Current concepts. Int J Clin Pract. 2010;142:113–9. doi: 10.1016/j.ijcard.2009.11.021. [DOI] [PubMed] [Google Scholar]
- 5.Rafiei M, Sadr S, Mirjalili M, Nayebzadeh M, Namayandeh S. The study of X syndrome, Afshar Hospital-Yazd. TUMJ. 2004;62:55–61. [Google Scholar]
- 6.Shoalehvar M, Sanatkar M. Evaluation of patients with angina pectoris and normal coronary angiography. J Isfahan Med Sch. 2002;19:4–8. [Google Scholar]
- 7.Taghizade B. A survey to determine the prevalence of cardiac syndromexand associated coronary risk factors among the patients referred for angiography in taleghani of urmia [Medical thesis] Urmia: Urmia University of Medical Science; 2008. [Google Scholar]
- 8.Bugiardini R, Merz C. Angina with “normal” coronary arteries. JAMA. 2005;293:477–84. doi: 10.1001/jama.293.4.477. [DOI] [PubMed] [Google Scholar]
- 9.Larsen W, Mandleco B. Chest pain with angiographic clear coronary arteries: A provider’s approach to cardiac syndrome X. J Am Acad Nurse Pract. 2009;21:371–6. doi: 10.1111/j.1745-7599.2009.00425.x. [DOI] [PubMed] [Google Scholar]
- 10.Asbury EA, Creed F, Collins P. Distinct psychosocial differences between women with coronary heart disease and cardiac syndrome X. Eur Heart J. 2004;25:1695–701. doi: 10.1016/j.ehj.2004.07.035. [DOI] [PubMed] [Google Scholar]
- 11.Isikhan V, Guner P, Komurcu S, Ozet A, Arpaci F, Ozturk B. The relationship between disease features and quality of life in patients with cancer-I. Cancer Nurs. 2001;24:490–5. doi: 10.1097/00002820-200112000-00012. [DOI] [PubMed] [Google Scholar]
- 12.Testa MA, Simonton DC. Assessment of quality of life outcome. NEJM. 2003;3:835–84. doi: 10.1056/NEJM199603283341306. [DOI] [PubMed] [Google Scholar]
- 13.Eriksson BE, Tyni-Lenne R, Svedenhag J. Physical training in syndrome X: Physical training counteracts deconditioning and pain in syndrome X. J Am Coll Cardiol. 2000;36:1619–25. doi: 10.1016/s0735-1097(00)00931-1. [DOI] [PubMed] [Google Scholar]
- 14.Leaf DA, Goldhaber J. Effects of physical exercise training in syndrome X. Clin Cardiol. 1993;16:65–6. doi: 10.1002/clc.4960160114. [DOI] [PubMed] [Google Scholar]
- 15.Asbury EA, Collins P. Psychosocial factors associated with non cardiac chest pain and syndrome X. Herz. 2005;30:55–60. doi: 10.1007/s00059-005-2649-x. [DOI] [PubMed] [Google Scholar]
- 16.van Dixhoorn J, White A. Relaxation therapy for rehabilitation and prevention in ischaemic heart disease. Eur J Cardiovasc Prev Rehabil. 2005;12:193–202. doi: 10.1097/00149831-200506000-00002. [DOI] [PubMed] [Google Scholar]
- 17.Jadhav S, Ferrell W, Greer IA, Petrie JR, Cobbe SM, Sattar N. Effects of metformin on microvascular function and exercise tolerance in women with angina and normal coronary arteries: A randomized, double-blind, placebo-controlled study. J Am Coll Cardiol. 2006;48:956–63. doi: 10.1016/j.jacc.2006.04.088. [DOI] [PubMed] [Google Scholar]
- 18.Dehdari T. Design and evaluation of theory-based educational program for reducing patients anexiety after CABG [Phd thesis] Tehran: Tarbiat Modares University; 2007. [Google Scholar]
- 19.Montazeri A, Goshtasebi A, Vahdaninia M, Gandek B. The short form health survey (SF-36): Translation and validation study of the Iranian version. Qual Life Res. 2005;14:857–82. doi: 10.1007/s11136-004-1014-5. [DOI] [PubMed] [Google Scholar]
- 20.Asbury EA, Kanji N, Ernst E, Barbir M, Collins P. Autogenic training to manage symptomology in women with chest pain and normal coronary arteries. Menopause. 2009;16:60–5. doi: 10.1097/GME.0b013e318184762e. [DOI] [PubMed] [Google Scholar]
- 21.Tyni-lenne R, Stryjan S, Eriksson B, Berglund M, Sylven C. Benifical therapeutic effects of physical training and relaxation therapy in women with coronary syndrome x. Physiother Res Int. 2002;7:35–43. doi: 10.1002/pri.239. [DOI] [PubMed] [Google Scholar]
- 22.Cunningam C, Brown S, Kaski J. Effects of transcendental meditation on symptoms and electrocardiographic changes in patients with cardiac syndrome X. Am J Cardiol. 2000;85:653–5. doi: 10.1016/s0002-9149(99)00828-0. [DOI] [PubMed] [Google Scholar]
- 23.Asbury EA, Slattery C, Grant A, Evans L, Barbir M, Collins P. Cardiac rehabilitation for the treatment of women with chest pain and normal coronary arteries. Menopause. 2008;15:454–60. doi: 10.1097/gme.0b013e31815982eb. [DOI] [PubMed] [Google Scholar]
- 24.Stephens MB. Cardiac rehabilitation. Am Fam Physician. 2009;80:955–9. [PubMed] [Google Scholar]
- 25.Asbury EA, Webb CM, Collins P. Group support to improve psychosocial well-being and primary-care demands among women with cardiac syndrome X. Climacteric. 2011;14:100–4. doi: 10.3109/13697137.2010.499181. [DOI] [PubMed] [Google Scholar]


