Abstract
Background:
Herpes genitalis is one of the commonest sexually transmitted infections in the world caused by herpes simplex virus (HSV) 1 and 2. All herpes viruses show latency. Herpes genitalis caused by HSV-1 and HSV-2 is recurrent in 55 and 90% of case respectively.
Aims:
To comparatively evaluate the therapeutic efficacy of topical zinc sulfate (ZnSO4) in varying concentrations in herpes genitalis.
Materials and Methods:
Ninety patients clinically diagnosed as herpes genitalis and confirmed by Tzanck test were taken up for study and divided into 3 groups of 30 patients each which were applied topical ZnSO4 in concentrations of 1%, 2% and 4% respectively for 3 months. Ten patients of herpes genitalis were kept as control in whom only distilled water was applied. Patients were followed up for a total period of 6 months for any recurrences.
Results:
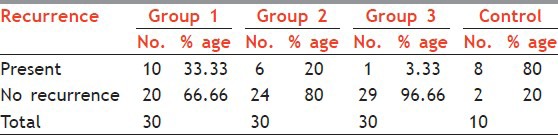
Ten patients of group 1 (1% ZnSO4) showed recurrence, 6 patients in group 2 (2% ZnSO4) and only one patient in group 3 (4% ZnSO4) showed recurrence. In the control group, 8 out of 10 patients showed recurrence. No serious side effects were seen in all 3 groups.
Conclusion:
Topical ZnSO4 has been found to be an effective therapeutic modality not only for treatment but also for prolonging remissions in herpes genitalis. Topical 4% ZnSO4 has been found to be most efficacious out of the three concentrations, without any side effects.
Keywords: Herpes genitalis, new approach, zinc sulfate
INTRODUCTION
Herpes genitalis is one of the commonest diseases in both developing as well as in developed countries. It is now the most common cause of genital ulceration in the developed world.[1] It is caused by herpes simplex virus (HSV) 1 and 2, a deoxyribonucleic acid virus. Most cases are due to HSV-2 virus. The disease is known since antiquity (derived from the Greek word which means “to creep”). It is characterized by small, grouped, painful vesicles or pustules on an erythematous base, which break and form ulcers in 2-4 days. One of the important characteristics of all herpes viruses is latency.[2] Herpes genitalis caused by HSV-2 is recurrent in 90% of cases. In herpes genitalis caused by HSV-1, 55% patients report recurrent episodes.[3] A number of drugs are used in the treatment of primary as well as recurrent herpes genitalis including acyclovir, famciclovir, valacyclovir, ganciclovir, idoxuridine, trifluridine, foscarnet, cidofovir. But it should be noted that to date, there is no evidence that any antiviral drug can affect the natural history of herpes genitalis in humans and curtail the recurrent nature of the disease.[2] A number of studies have showed the efficacy of Zn2 + in inhibiting herpes viruses in vitro.[4] This study was being undertaken to evaluate the therapeutic efficacy of topical zinc sulfate (ZnSO4) in varying concentrations in herpes genitalis.
MATERIALS AND METHODS
A total of 100 patients attending the sexually transmitted infection clinic, GGS Medical College, Faridkot, over a period of 1 year, from April 2008 to April 2009 and clinically diagnosed as herpes genitalis with a positive Tzanck smear were included in the study, which were further divided in 3 groups of 30 patients each for topical application of three different concentration of ZnSO4 (i.e., 1%, 2% and 4%) respectively and 10 patients kept as control in whom only distilled water was applied. Patients who were venereal disease research laboratory (VDRL) test reactive or human immunodeficiency virus positive were not included in the study.
ZnSO4 solution was prepared fresh by dissolving measured amounts of ZnSO4 powder (commercially available as 100% crystalline powder) in distilled water to make three concentrations, i.e., 1%, 2% and 4%. After cleaning the lesions with distilled water, an ear bud soaked in ZnSO4 solution was applied on lesions for 5 min and then lesions again cleaned with distilled water.
The protocol was to apply topical ZnSO4 on the first visit, then after every 5 days for 1 month, followed by every 10 days for 2 months and then after every 15 days for 3 months for the total period of 6 month.
The patients were advised to follow-up after 24 h of the first application to see any side-effects like a burning sensation, increased erythema, severe pain or new lesions. Next follow-up visit was on every 5 days for 1 month, then after every 10 days for 2 months and then for every 15 days for 3 months. At every follow-up visit, response of treatment was recorded and graded both objectively as well as photographically both by the researcher and analyzer.
G0: No improvement
G1: 25-50% improvement
G2: 51-75% improvement
G3: 76-99% improvement
G4: Complete recovery
RESULTS
A total of 100 patients aged between 20 years and 70 years were enrolled for study. Majority of them were between 30 years and 50 years age group (sexually active) [Table 1]. History of extra/premarital contact was present in the majority of patients [Table 2]. In all 3 groups, majority of patients had lesions on both prepuce and glans penis. During a follow-up of 6 months, 10 (33.33%) patients of group 1 [Figure 1a and b] showed recurrence, 6 (20%) patients in group 2 [Figure 2a and b] and only 1 (03.33%) patient in group 3 [Figure 3a–d] showed recurrence. In the control group 8 (80%) out of 10 patients showed recurrence. No serious side effects were seen in all 3 groups, although minor side effects were most common in group 3. Out of all the 3 groups, 4% topical ZnSO4 was found to be most efficacious [Table 3].
Table 1.
Distribution of patients according to age

Table 2.
Distribution of patients according to sexual behavior

Figure 1.
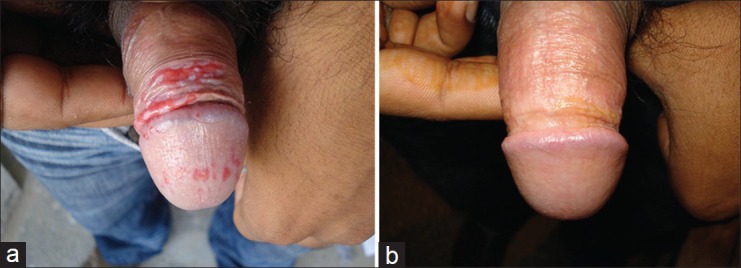
(a) Group 1: Superficial erosions present on under the surface of the prepuce before treatment with topical 1% zinc sulfate, (b) Group 1: Same patient at 6 months follow-up with complete resolution of lesions after treatment with topical 1% zinc sulfate without any recurrence in 6 months follow-up period
Figure 2.
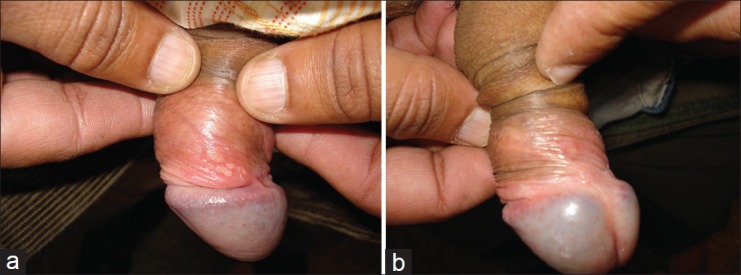
(a) Group 2: Vesicular erosions present on the under surface of the prepuce before treatment with topical 2% zinc sulfate, (b) Group 2: Complete resolution of lesions after treatment with topical 2% zinc sulfate at 6 months follow-up period without any recurrences
Figure 3.

(a) Group 3: Superficial erosions present on glans before treatment with topical 4% zinc sulfate, (b) Group 3: Same patient at 5 days of follow-up periods after treatment with topical 4% zinc sulfate showing partial resolution of lesions, (c) Group 3: Same patient after 10 days of treatment with topical 4% zinc sulfate, showing almost complete resolution of lesions, (d) Group 3: Same patient after treatment with topical 4% zinc sulfate at 6 months follow-up period without any recurrences
Table 3.
Distribution of patients according to recurrence
DISCUSSION
Herpes genitalis once considered being a minor sexually transmitted disease, is rapidly gaining importance in present day scenario, as an increase of two fold has been reported from North India in recent years.[5] Even immune-competent people with HSV people can have frequent, painful and recurrent genital lesions.[2] Gupta and Kumar observed that the prevalence of HSV-2 rises with initiation of sexual activity in adolescence and steadily increases through adulthood.[2] In our study also majority of the patients were between 30 years and 50 years of age group (52.2%). A study carried out by Brody showed that daily application of low concentrations (0.025-0.05%) of ZnSO4 is effective in recurrent herpes at skin site and also prevents relapse of post-herpetic erythema multiforme.[6] Maintenance treatment was once a week for 1 month and then twice a month for 2 year observation period. He used low concentration to prevent any side effects. In our study, much higher concentration was used, but no serious side effects were seen, and were also more effective. Randomized double blind placebo controlled clinical trial of two strengths (0.025 and 0.05%) of topical ZnSO4 against recurrent herpes simplex was done by Iraji and Faghihi, which showed that 0.05% topical ZnSO4 is an effective therapeutic modality against recurrent herpes simplex infection as compared to lower concentration or placebo.[7] Again it was lower concentration of topical ZnSO4 (0.25%), which Finnerty used for herpes genitalis. He applied this solution 6-8 times a day which resulted in healing of lesions in 8-10 days.[8] We used topical ZnSO4 at a longer interval but still no recurrence was seen. In another study carried out by Wahba, 4% ZnSO4 in water applied topically was found to be effective in recurrent herpes simplex. Eighteen patients were treated with 4% ZnSO4 in water. In all patients, pain, tingling and burning stopped entirely within first 24 h of ZnSO4 application. Crusting occurred in 1-3 days. Time needed for complete healing ranged between 6 days and 12 days (mean 9.5 days).[9] In our study, improvement was seen a little later but healing occurred in almost in 1-2 weeks.
CONCLUSION
Topical ZnSO4 has been found to be an effective therapeutic modality not only for treatment but also for preventing recurrences of herpes genitalis, with 4% topical ZnSO4 found to be most efficacious out of the three concentrations, without any side effects.
Footnotes
Source of Support: Nil.
Conflict of Interest: None declared.
REFERENCES
- 1.Mindel A. Genital herpes - How much of a public-health problem? Lancet. 1998;351(Suppl 3):16–8. doi: 10.1016/s0140-6736(98)90005-8. [DOI] [PubMed] [Google Scholar]
- 2.Gupta S, Kumar B. Sexually Transmitted Infections. 1st ed. New Delhi: Elsvier; 2005. Herpes genitalis simplex infections; pp. 191–214. [Google Scholar]
- 3.Scoular A, Norrie J, Gillespie G, Mir N, Carman WF. Longitudinal study of genital infection by herpes simplex virus type 1 in Western Scotland over 15 years. BMJ. 2002;324:1366–7. doi: 10.1136/bmj.324.7350.1366. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kümel G, Schrader S, Zentgraf H, Brendel M. Therapy of banal HSV lesions: Molecular mechanisms of the antiviral activity of zinc sulfate. Hautarzt. 1991;42:439–45. [PubMed] [Google Scholar]
- 5.Kumar B, Sahoo B, Gupta S, Jain R. Rising incidence of genital herpes over two decades in a sexually transmitted disease clinic in north India. J Dermatol. 2002;29:74–8. doi: 10.1111/j.1346-8138.2002.tb00169.x. [DOI] [PubMed] [Google Scholar]
- 6.Brody I. Topical treatment of recurrent herpes simplex and post-herpetic erythema multiforme with low concentrations of zinc sulphate solution. Br J Dermatol. 1981;104:191–4. doi: 10.1111/j.1365-2133.1981.tb00044.x. [DOI] [PubMed] [Google Scholar]
- 7.Iraji F, Faghihi G. A randomized double blind placebo – Controlled clinical trial of two strengths of topical zinc sulfate solution against recurrent herpes simplex. Arch Iran Med. 2003;6:13–5. [Google Scholar]
- 8.Finnerty EF. Topical zinc in the treatment of herpes simplex. Cutis. 1986;37:130–1. [PubMed] [Google Scholar]
- 9.Wahba A. Topical application of zinc-solutions: A new treatment for herpes simplex infections of the skin? Acta Derm Venereol. 1980;60:175–77. [PubMed] [Google Scholar]


